Abstract
Introduction and Aims
Alcohol use disorders are highly prevalent among men who have sex with men (MSM) in Peru where the HIV epidemic is concentrated 100-fold greater among MSM, than in the general population. Drinking expectancies have been associated with the intent to drink and engage in high-risk behaviors. Assessing them in this population may uncover attractive intervention targets that in turn can be used to reduce problematic drinking and risky sexual behaviors. The drinking expectancy questionnaire for MSM (DEQ-MSM) was developed to accurately measure drinking expectancies, specifically among MSM. This study aimed to validate this instrument for the first time in Spanish, in South America and among MSM in Peru.
Design and Methods
To validate the DEQ-MSM among Spanish-speaking MSM in Peru, we used exploratory and confirmatory factor analysis in a sample of 5,148 MSM, including 700 transgender women (TGW).
Results
Exploratory factor analysis showed a 2-factor structure to the Spanish version of the DEQ-MSM (DEQ-MSM-S), which was similar for MSM and TGW. The reliability of the translated DEQ-MSM was excellent (α=0.91).
Discussion and Conclusions
The DEQ-MSM-S was shown to be highly reliable in a large population of Peruvian MSM and TGW. This short instrument can be effectively integrated into research or clinical practice, in order to identify alcohol-consuming, high-risk MSM, who can then be directed for further screening and/or intervention. Future research should aim to associate the Spanish version of the DEQ-MSM with risky sexual behaviors among this population, in order to identify potential intervention targets.
Keywords: alcohol expectancies, alcohol use disorders, men who have sex with men, MSM
Introduction
Alcohol consumption is a common social and recreational activity that differs globally within multiple cultures and contextually (1), but it is also known that it can lead to major health problems, addiction and even death (1). Problematic use of alcohol and other drugs is highly prevalent among men who have sex with men (MSM) (2). Multiple studies in different global settings, have associated hazardous/harmful use of alcohol with sexual risk behaviors, among MSM and other at-risk populations (3–9), that can lead to HV infection, an epidemic that greatly affects the MSM population globally (10). Among people living with HIV/AIDS (PLH), alcohol use disorders (AUDs) negatively impact the HIV continuum of care (9), including delays in HIV diagnosis (11), being unaware of HIV positive status (12), delayed linkage to HIV care (13, 14), decreased antiretroviral therapy (ART) adherence (15) and other HIV-related treatment outcomes (16).
Similar to North America, more than half of new HIV infections in Latin America are due to unprotected sex between men (17). In Peru, a middle-income country where overall HIV prevalence is only 0.2% (18), HIV prevalence among MSM in Lima is 18–22% (19, 20), or 100-fold greater. A recent nationwide biosurveillance of Peruvian MSM found that AUDs exceeded 60%, and were associated with increased HIV risk-taking behaviors that increased with AUD severity (8). While a causal relationship between alcohol consumption and HIV risk among MSM has yet to be unequivocally established (21), numerous studies document a high correlation between problematic alcohol consumption, risky sexual behaviors and HIV infection. Moreover, factors contributing to alcohol consumption are often complex and studies that further elaborate pathways leading to heavy consumption and ultimately HIV risk behaviors and adverse consequences along the HIV continuum of care are crucial for development of targeted interventions that target the individual before alcohol is ingested.
Drinking expectancies refer to beliefs held by the individual about what will happen for him/her after drinking. They include positive and negative feelings, such as the positive expectation to relax and enjoy a social function, as well as the negative expectation that too much drinking may affect one’s judgment or cause a headache the day after drinking. To measure alcohol expectancies, researchers have used questionnaires, such as the 90-item Alcohol Expectancy Questionnaire (22). Recently an abbreviated alcohol expectancies questionnaire was developed and validated specifically for MSM: the 10-item drinking expectancy questionnaire for MSM (DEQ-MSM) (23). This measure helps ensure that the specific issues pertinent to alcohol use among MSM will be accurately captured. Adapting a validated instrument developed for a specific population in another setting or cultural context (including a new language) that shares some common characteristics but may have cultural differences is necessary, to ensure validity. It is therefore important to accurately translate and validate such measures in new populations to ensure both validity and reliability. The DEQ-MSM has so far been validated only among MSM in Australia (23), a high-income country where MSM culture and behaviors may be distinct from MSM in Peru, where AUDs are highly prevalent and homosexuality is more stigmatized.
Here, we aim to accurately translate, validate and test the reliability of the DEQ-MSM questionnaire (23) among a large sample of Peruvian MSM. This represents the first cross-cultural use of the DEQ-MSM instrument since its initial publication, as well as its first use in the Spanish language.
Methods
Participants
Between May and October 2011, a bio-behavioral survey of 5,575 MSM was conducted by the Peruvian NGO Associación Civil Impacta Salud y Educación (Impacta). Participants were eligible if they were 18 years or older, could provide informed consent, were born male (transgender women [TGW] were included and comprised 14% of the sample) and reported sex with another male in the last 12 months. Using a modified snowball recruitment strategy (24), participants were recruited in the capital, Lima, as well as in the provincial cities of Ica, Piura, Pucallpa and Iquitos. Computer-assisted interviews were overseen by trained research assistants and conducted in private locations, within participating research organizations, NGOs and healthcare facilities. Survey completion was 92.3%, resulting in 5,148 participants included in the final analytic sample. Participants were paid 10 Nuevos Soles ($3.70 USD) for their time and the study was approved by Institutional Review Boards of Yale University and Impacta.
Questionnaire
The original 10-item DEQ-MSM questionnaire, developed in 2011 by Mullens et al. (23), assesses different types of drinking expectancies using a 5-point Likert scale (response options range from “strongly disagree” to “strongly agree”). The survey was first translated into Spanish and then back-translated into English (25), in order to ensure accuracy (Table 1). In a group setting with two facilitators fluent in English and Spanish, each item was read aloud in Spanish and presented on paper to a group of 8 MSM, where feedback was provided to ensure proper terminology and understanding of each question. After translation procedures were completed, it was tested by research assistants, incorporated into the larger survey that assessed AUDs and HIV risk behaviors and then administered to participants using CASI.
Table 1.
The Drinking Expectancies Questionnaire for Men who have Sex with Men (DEQ-MSM) in English and in Spanish translation.
| Item | Original DEQ-MSM | Spanish DEQ-MSM |
|---|---|---|
| 1 | I'm less able to ask for/discuss condoms during sex when drinking | Yo soy menos hábil de pedir o discutir el uso de condones durante el sexo cuando he tomado |
| 2 | When I drink my body is more physically sensitive | Cuando tomo mi cuerpo es físicamente más sensible |
| 3 | I become less rational when I'm drinking | Me convierto en menos racional cuando tomo |
| 4 | When I'm drinking I'm more forward with possible sexual partners | Cuando estoy tomando soy más propositivo con posibles parejas sexuales |
| 5 | Drinking makes it difficult for me to concentrate | Tomar dificulta concentrarme |
| 6 | Drinking makes my sexual performance better | Tomar me mejora la performance sexual |
| 7 | Sex is better when I've been drinking | El sexo es mejor cuando tomo |
| 8 | I feel more stimulation during sex when I'm drinking | Me siento más estimulado en el sexo cuando tomo |
| 9 | My mood is better when I've been drinking | Mi humor es mejor cuando tomo |
| 10 | I feel more connected with other people when I drink | Me siento conectado con la gente cuando tomo |
Analyses
Factor analysis was conducted for each survey item (23). Reliability was measured using Cronbach’s alpha. Analyses were independently conducted exclusively with both MSM (4,448) and TGW (700). Because the findings were similar for MSM and TGW, the sample was combined for presentation here. All analyses were performed using IBM SPSS (version 22).
Results
The 10 items of the DEQ-MSM-S (S for Spanish) were loaded into a principal axis factor analysis. Oblique rotation was used to account for correlation between items. The rotation converged in seven iterations and resulted in a two-factor solution, accounting for 59.5% of the total variance. Factor loadings for the ten items and two factors are shown in Table 2.
Table 2.
Principal axis factor matrix for DEQ-MSM, including Mean and Standard Deviation values for each item and two composite factor scores.
| Factor 1 | Factor 2 | Mean, SD | |
|---|---|---|---|
| Factor 1: Affect | |||
| Item 8: I feel more stimulation during sex when I’m drinking | 0.959 | −0.098 | 1.54, 1.21 |
| Item 7: Sex is better when I’ve been drinking | 0.893 | −0.052 | 1.43, 1.19 |
| Item 9: My mood is better when I’ve been drinking | 0.744 | 0.051 | 1.72, 1.25 |
| Item 6: Drinking makes my sexual performance better | 0.679 | 0.102 | 1.50, 1.18 |
| Item 10: I feel more connected with other people when I drink | 0.613 | 0.223 | 1.80, 1.24 |
| Factor 2: Cognition | |||
| Item 3: I become less rational when I’m drinking | −0.036 | 0.838 | 1.41, 1.20 |
| Item 2: When I drink my body is more physically sensitive | 0.010 | 0.748 | 1.64, 1.27 |
| Item 4: When I’m drinking I’m more forward with possible sexual partners | 0.106 | 0.621 | 1.62, 1.24 |
| Item 5: Drinking makes it difficult for me to concentrate | −0.048 | 0.607 | 1.55, 1.22 |
| Item 1: I am less able to ask for/ discuss condoms during sex when drinking | 0.270 | 0.542 | 1.39, 1.29 |
| Factor 1: Affect | 1.60, 1.03 | ||
| Factor 2: Cognition | 1.52, 0.97 |
Factor 1 contained five items that address the perceived impact of alcohol consumption on mood (e.g., “My mood is better when I’ve been drinking”) and interpersonal connectedness (e.g., I feel more connected with other people when I drink). As such, Factor 1 was termed “Affect.” Factor 2 contained 5 items that address the impact of alcohol consumption on decision-making processes (e.g., I am less able to ask for / discuss condoms during sex when drinking”). Factor 2 was termed “Cognition.”
Reliability
Internal consistency for the 10-item DEQ-MSM-S was strong (α=0.91). Reliabilities for the Affect (α=0.90) and Cognition (α=0.84) subscales ranged from strong to excellent.
Convergent Validity
Validity of the two-factor structure of the DEQ-MSM-S was further evaluated by comparing factor scores between individuals who met screening criteria for having an AUD as measured by the World Health Organization’s Alcohol Use Disorders Identification Test (AUDIT) (26). In the present sample, 63.2% (N=3233) met criteria for an AUD with a score of 8 or greater. Independent samples t tests indicated participants with an AUD had significantly higher mean scores on both the Affect (M=1.88, SD=0.97) and Cognition (M=1.76, SD=0.91) factors of the DEQ-MSM-S, compared to participants with no AUD (Affect: M=1.11, SD=0.96; Cognition: M=1.12, SD=0.93), taffect (5115)=−27.69, p<0.0001, tcognition (5115)= −24.24, p<0.0001.
Predictive Validity
Predictive validity was assessed by testing for an association between the two factor scores and AUDIT scores, measured continuously. The AUDIT score was regressed onto the affect and cognition composite scores in two separate linear regression equations. Results show a significant effect for both affect (β=3.30, p<0.0001, R2=0.174; F[1,5115]=1076.76, p<0.0001) and cognition (β=3.31, p<0.0001, R2=0.154; F[1,5115]=930.21, p<0.0001) on continuous AUDIT scores, indicating a strong positive correlation.
Correlations
To minimize item-specific error, the average response across items was calculated and used to generate a mean score for each of the two factors. These two composite factor-scores were then loaded into a correlation matrix with mean scores for the 10 items of the DEQ-MSM-S. Each of the 10 items correlated strongest with their respective composite factor (see Table 3)
Table 3.
Pearson Correlations between the 10-item DEQ-MSM and Affect and Cognition Subscales
| Item 8 | Item 7 | Item 9 | Item 6 | Item 10 |
Item 3 | Item 2 | Item 4 | Item 5 | Item 1 | Affect | Cognition | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Item 8: I feel more stimulation during sex when I’m drinking | 1 | |||||||||||
| Item 7: Sex is better when I’ve been drinking | .828** | 1 | ||||||||||
| Item 9: My mood is better when I’ve been drinking | .659** | .613** | 1 | |||||||||
| Item 6: Drinking makes my sexual performance better | .676** | .696** | .563** | 1 | ||||||||
| Item 10: I feel more connected with other people when I drink | .622** | .576** | .752** | .547** | 1 | |||||||
| Item 3: I become less rational when I’m drinking | .444** | .456** | .445** | .492** | .449** | 1 | ||||||
| Item 2: When I drink my body is more physically sensitive | .440** | .423** | .437** | .476** | .450** | .613** | 1 | |||||
| Item 4: When I’m drinking I’m more forward with possible sexual partners | .545** | .539** | .490** | .599** | .498** | .588** | .550** | 1 | ||||
| Item 5: Drinking makes it difficult for me to concentrate | .432** | .433** | .431** | .508** | .435** | .583** | .484** | .548** | 1 | |||
| Item 1: I am less able to ask for / discuss condoms during sex when drinking | .314** | .311** | .302** | .358** | .294** | .460** | .482** | .374** | .384** | 1 | ||
| Affect (Factor 1) | .889** | .871** | .847** | .816** | .826** | .537** | .524** | .628** | .527** | .371** | 1 | |
| Cognition (Factor 2) | .559** | .555** | .540** | .624** | .546** | .830** | .807** | .786** | .767** | .701** | .664** | 1 |
p<.001
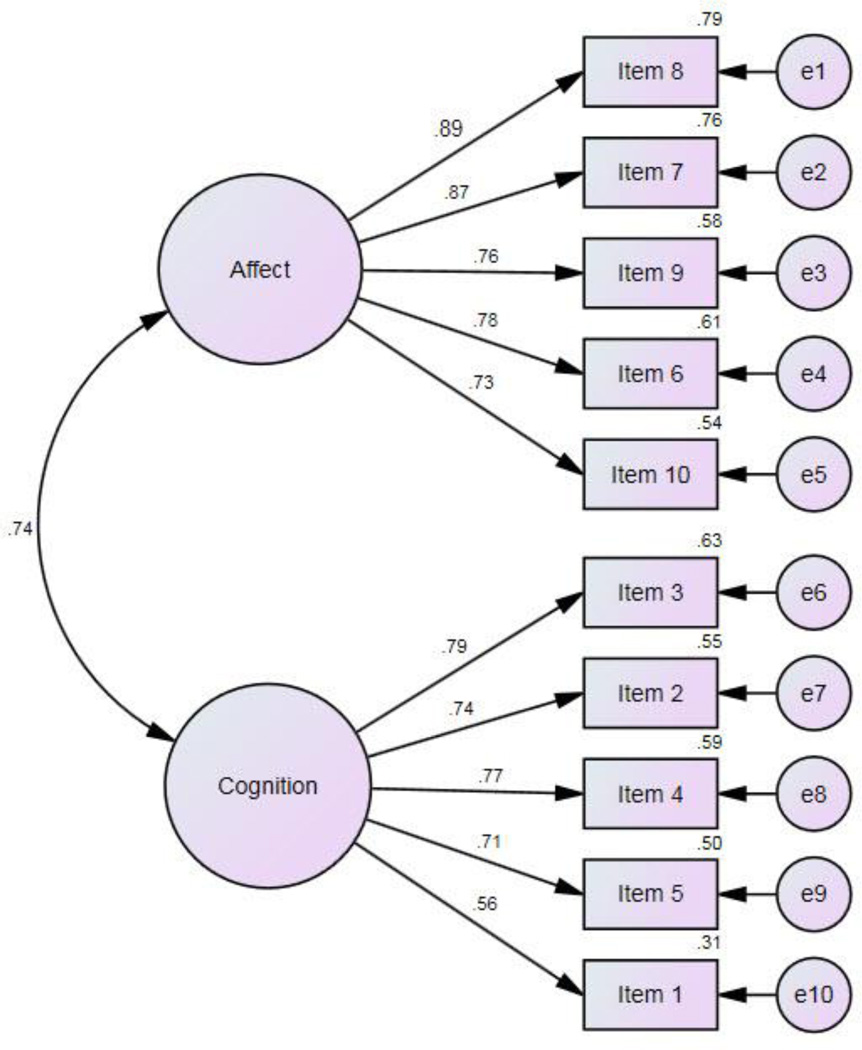
Confirmatory Factor Analysis
A confirmatory factor analysis (CFA) was conducted on the 2-factor structure of the DEQ-MSM-S, using AMOS Version 22 (IBM SPSS Version 22) with maximum likelihood estimation. Figure 1 illustrates the hypothesized model and standardized beta weights. The root mean square error of approximation (RMSEA=0.121) indicated a poor fit with a highly significant chi-square (χ2=2614.4, df=655, p<0.001), but is likely a result of RMSEA’s sensitivity to large samples (27). Other fit indices not sensitive to sample size, however, indicate a good model fit: CFI=0.916, NFI=0.915, TLI=0.964, IFI=0.916 (values >0.95 suggest a good fit; values between 0.90–0.95 indicate an adequate fit). Beta values for each item indicate strong loadings to each factor, confirming results from the Exploratory Factor Analysis. Item 1, however, had a lower beta weight (β=0.56) compared to other items loading onto the cognition factor. These analyses were repeated in the sub-sample of 700 TGW and the results indicated the factor structure of the DEQ-MSM-S for TGW was identical, although as expected factor loadings varied slightly across items.
Figure 1.
Confirmatory Factor Analysis (CFA) of DEQ-MSM
Discussion
Alcohol expectancies are associated with intent to drink, drinking and post-drinking behavior. Although a number of instruments designed to measure such expectancies exist, there is a lack of instruments developed for specific populations (e.g., MSM and TGW), particularly those who speak languages other than English or live in diverse cultural contexts where reasons for alcohol consumption may differ. The DEQ-MSM questionnaire (23) is the first instrument specifically designed to measure drinking expectancies among MSM. This instrument was developed and validated in a sample of Australian MSM, in English. While MSM globally may share many similar characteristics, there are also distinct differences in local cultures, as well as differences between high-income countries, like Australia, and middle-income ones, like Peru. These differences may be due to different levels of acceptability of homosexuality, stigma against homosexuality, perceptions of male culture (e.g. machoism) and the different role of religion, around the world.
The aim of this study was to administer a Spanish translation of the DEQ-MSM (named DEQ-MSM-S) to a large sample of Peruvian MSM and subsequently validate it for use among Spanish-speaking populations. During initial development of the DEQ-MSM, the researchers identified three domains of perceived reinforcement: ‘cognitive impairment’, ‘sexual activity’ and ‘social and emotional facilitation’ (23). Our own factor analysis revealed some similarities and some differences between the original instrument and our Spanish translation, used in a bio-behavioral survey of more than 5,000 Peruvian MSM, including TGW. Our analysis showed that in spite of potential cultural differences between MSM in different countries, the questionnaire’s items loaded to two factors with similarities to the ones in the original study. Our two factors related only to ‘affect’ and ‘cognition’. Four out of five items in the ‘cognition’ factor corresponded to the original study’s ‘cognitive impairment’ factor. While the other items load to somewhat different factors than in the original study, the strong correlations suggest that this is a robust instrument that can be used in this population. Although the original DEQ-MSM had a three-factor solution, the third factor contained only two items, which can indicate a weak factor in that the loss of one of these items would reveal a single-item factor. Second, that factor does not appear to be fully conceptually distinct from the first factor (of the original DEQ-MSM). The substantially larger sample size used in this analysis may have contributed to a more parsimonious, two-factor solution. Nevertheless, it is also possible that the structure differences between the DEQ-MSM and the DEQ-MSM-S could be attributed to cultural differences.
Our analyses show that the DEQ-MSM-S has been successfully translated and used in a large sample of Peruvian MSM. Its reliability indicates that this instrument can now be used in future research among this population and other Spanish speaking MSM communities, to identify associations between drinking expectancies and sexual risk behaviors. An understanding of such associations could aid in the development of targeted interventions to reduce problematic drinking in this population.
Given its brevity, ease of administration, and straightforward interpretation, the DEQ-MSM-S may serve as a useful instrument to both public health authorities targeting alcohol consumption and clinicians working with Spanish-speaking MSM clients who consume alcohol. Administration of the questionnaire in the context of clinical practice could illuminate expectancies that contribute to a given client’s drinking behavior. Elevated scores on one or both factors of the DEQ-MSM-S could guide clinicians in terms of where to direct efforts for cognitive interventions if needed and which techniques might be most effective.
A high score on the “affect” factor may indicate that the client possesses positive but somewhat inaccurate expectancies about alcohol’s impact on sexual functioning. For example, in contrast to the statements “Drinking makes my sexual performance better” and “I feel more stimulation during sex when I’m drinking,” previous research suggests that a high level of alcohol consumption has a null or attenuating effect on men’s physiological sexual arousal (4, 28). Thus, the clinician could support the client in critically evaluating existing expectancies in light of contradictory evidence and highlight the potential sexual benefit of abstaining from heavy drinking. On the other hand, expectancies around alcohol enhancing subjective sexual experience (“Sex is better when I’ve been drinking”), which are cultivated and reinforced by dominant culture, can become self-fulfilling prophecies (4, 29) and may therefore be resistant to change. In such cases, intervening with the client about the concomitant vulnerabilities to sexual risk-taking behaviors (e.g. not using condoms) that alcohol may confer through increased psychological sexual arousal, reduced self-awareness, and/or lower concern about risk (29, 30) is important. Further, if participants report improved mood or social connectedness expectancies related to alcohol use (“My mood is better when I’ve been drinking” or “I feel more connected with other people when I drink”), the clinician could probe factors contributing to a client’s experience of poorer mood and feelings of disconnectedness when sober, and help the client find safer and more effective alternative strategies to boost mood, reduce social anxieties, and/or strengthen relationships. Altogether, such information may also help guide primary and secondary HIV prevention strategies that target behavioral change among MSM who consume alcohol.
Whereas a client’s agreement with items on the “affect” factor would reflect positive and potentially inaccurate drinking expectancies, a client’s agreement with most items on the “cognition” factor would reflect predominantly negative and potentially accurate expectancies (e.g., “Drinking makes it more difficult to concentrate”). Thus, a high score on the cognition factor may indicate existing recognition of the problematic effects of drinking on decision-making and other thought processes and could serve as a launching point for discussion about the link between cognitive impairment, risk behavior, and adverse health consequences. In addition to encouraging a client who is engaging in risk behaviors while drinking to reduce his level of alcohol consumption, clinicians could help the client identify strategies that could be implemented in advance of planned alcohol use to maximize his safety during periods of consumption (e.g., carrying condoms in his wallet if he reports that he is “less able to ask for/discuss condoms during sex when drinking” or “more forward with possible sexual partners”).
Administration of a paper-and-pencil, self-report measure to clients to help identify cognitions contributing to sexual risk-taking — and thus, targets for cognitive intervention — is a technique that has been used previously in the context of HIV risk reduction counseling among MSM (31–34). Acceptability of a single-session personalized cognitive counseling program implementing this strategy among substance-using MSM in particular has been reported previously (31). Specifically, men were asked to select from a list of self-justifications (i.e. rationalizing statements) that they employed during a recent risky event in which they knowingly engaged in risky behaviors with another man. Subsequently within the session, the men explored strategies to avoid repeating such behaviors, including reframing the specific self-justifications used. This intervention yielded promising results for alcohol use reduction, but not alcohol-associated sexual risk reduction (32). The DEQ-MSM-S may function as a useful alternative or adjunct screening measure to capture more global (versus event-specific) cognitions contributing to alcohol use and alcohol-associated sexual risk among Spanish-speaking MSM clientele.
Administration of the DEQ-MSM-S could be beneficial in the context of alcohol treatment among men (or TGW) diagnosed with AUDs, but could also yield valuable insights in other settings attended by men who do not meet diagnostic criteria for an AUD (e.g., binge drinking) and/or are unlikely to seek treatment for an AUD, but whose alcohol use nonetheless heightens their risk for acquiring HIV and other sexually transmitted infections. Importantly, while the DEQ-MSM-S may provide useful information about the alcohol expectancies of a given client, the clinician would need to conduct a more thorough, individualized assessment to determine the extent to which these expectancies contribute to sexual risk or otherwise threaten the wellbeing of the client and therefore necessitate intervention. In the Peruvian setting, the Ministry of Health has created a few new clinical settings specializing in testing and treating STIs, where incorporating the DEQ-MSM-S in clinical practice could provide a useful additional tool to screen for problematic alcohol drinking. Further research is warranted to establish the acceptability of the DEQ-MSM-S among clinicians and clients and its utility in clinical practice.
Limitations
Item 1 had a lower beta weight compared to other items loading onto the cognition factor. The Spanish-language translation of the item was considered accurate by native speakers and was unlikely to be the cause of the weaker loading. In future evaluations of the DEQ-MSM-S, this item may be considered for removal, if this specific result is replicated in other Spanish-speaking cultural settings.
Although item 2 loaded strongly on the Cognition factor, the content of the item is noticeably distinct from the other Cognition items. The translation was double-checked and considered accurate. The participants may have interpreted this item as relating to the emotional response of touching. Future studies evaluating the factor structure of the DEQ-MSM-S may further explore this item by either adding additional items to further measure the discrete constructs of Cognition and Affect, or by rephrasing this item.
Conclusion
The DEQ-MSM-S has been successfully validated among a population of Peruvian MSM, including TGW. This instrument may now provide a useful tool for clinicians and researchers, in order to identify high-risk drinking MSM and provide targeted interventions.
Acknowledgments
Funding: This research was funded by the U.S. National Institute on Drug Abuse (NIDA) and the National Institute of Mental Health (NIMH) through research (R01 DA032106) and career development awards (K24 DA017072 to FLA, K01 DA038529 to JAW and K01 MH103080 to SKC) and the Global Fund to Fight AIDS, Tuberculosis and Malaria grants PER-506-G03-H and PER-607-G05-H awarded to CARE PERU. Unrestricted discretionary core funds from Associación Civil Impacta Salud y Educación were also provided. The funding sources played no role in study design, data collection, data analysis, data interpretation, writing of the manuscript or the decision to submit the paper for publication.
REFERENCES
- 1.World Health Organization. Geneva: 2011. Global Status Report on Alcohol and Health. [Google Scholar]
- 2.Ostrow DG, Stall R. Alcohol, tobacco, and drug use among gay and bisexual men. In: Wolitski RJ, Stall R, Valdiserri RO, editors. Unequal opportunity: Health disparities affecting gay and bisexual men in the United States. New York: Oxford University Press; 2008. [Google Scholar]
- 3.Fisher JC, Bang H, Kapiga SH. The association between HIV infection and alcohol use: a systematic review and meta-analysis of African studies. Sex Transm Dis. 2007;34(18049422):856–863. doi: 10.1097/OLQ.0b013e318067b4fd. [DOI] [PubMed] [Google Scholar]
- 4.George WH, Stoner SA. Understanding acute alcohol effects on sexual behavior. Annu Rev Sex Res. 2000;11(11351836) 92-9124. [PubMed] [Google Scholar]
- 5.Heath J, Lanoye A, Maisto SA. The role of alcohol and substance use in risky sexual behavior among older men who have sex with men: a review and critique of the current literature. AIDS Behav. 2012;16(3):578–589. doi: 10.1007/s10461-011-9921-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prev Sci. 2007;8(2):141–151. doi: 10.1007/s11121-006-0061-2. [DOI] [PubMed] [Google Scholar]
- 7.Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV. Issues in methodology, interpretation, and prevention. The American psychologist. 1993;48(10):1035–1045. doi: 10.1037//0003-066x.48.10.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ludford KT, Vagenas P, Lama JR, Peinado J, Gonzales P, Leiva R, et al. Screening for drug and alcohol use disorders and their association with HIV-related sexual risk behaviors among men who have sex with men in Peru. PLoS One. 2013;8(8):e69966. doi: 10.1371/journal.pone.0069966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care utilization. Drug Alcohol Depend. 2010;112:178–193. doi: 10.1016/j.drugalcdep.2010.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beyrer C, Wirtz AL, Walker D, Johns B, Sifakis F, Baral SD. The Global HIV Epidemics among Men Who Have Sex with Men. Washington, D.C.: The World Bank; 2011. [Google Scholar]
- 11.Samet JH, Mulvey KP, Zaremba N, Plough A. HIV testing in substance abusers. Am J Drug Alcohol Abuse. 1999;25(2):269–280. doi: 10.1081/ada-100101860. [DOI] [PubMed] [Google Scholar]
- 12.Vagenas P, Ludford KT, Gonzales P, Peinado J, Cabezas C, Gonzales F, et al. Being Unaware of Being HIV-Infected is Associated with Alcohol Use Disorders and High Risk Sexual Behaviors Among Men Who Have Sex with Men in Peru. AIDS Behav. 2013 doi: 10.1007/s10461-013-0504-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Samet JH, Larson MJ, Horton NJ, Doyle K, Winter M, Saitz R. Linking alcohol- and drug-dependent adults to primary medical care: a randomized controlled trial of a multi-disciplinary health intervention in a detoxification unit. Addiction. 2003;98(4):509–516. doi: 10.1046/j.1360-0443.2003.00328.x. [DOI] [PubMed] [Google Scholar]
- 14.Samet JH, Freedberg KA, Savetsky JB, Sullivan LM, Padmanabhan L, Stein MD. Discontinuation from HIV medical care: squandering treatment opportunities. J Health Care Poor Underserved. 2003;14(2):244–255. doi: 10.1353/hpu.2010.0798. [DOI] [PubMed] [Google Scholar]
- 15.Ferro EG, Weikum D, Vagenas P, Copenhaver MM, Gonzales P, Peinado J, et al. Alcohol Use Disorders Negatively Influence Antiretroviral Medication Adherence Among Men Who Have Sex with Men in Peru. AIDS Care. 2015;27(1):93–103. doi: 10.1080/09540121.2014.963013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care utilization. Drug Alcohol Depend. 2010;112(3):178–193. doi: 10.1016/j.drugalcdep.2010.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Griensven F, de Lind van Wijngaarden JW, Baral S, Grulich A. The global epidemic of HIV infection among men who have sex with men. Curr Opin HIV AIDS. 2009;4(4):300–307. doi: 10.1097/COH.0b013e32832c3bb3. [DOI] [PubMed] [Google Scholar]
- 18.Garcia PJ, Holmes KK, Carcamo CP, Garnett GP, Hughes JP, Campos PE, et al. Prevention of sexually transmitted infections in urban communities (Peru PREVEN): a multicomponent community-randomised controlled trial. Lancet. 2012;379(9821):1120–1128. doi: 10.1016/S0140-6736(11)61846-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sanchez J, Lama JR, Kusunoki L, Manrique H, Goicochea P, Lucchetti A, et al. HIV-1, sexually transmitted infections, and sexual behavior trends among men who have sex with men in Lima, Peru. J Acquir Immune Defic Syndr. 2007;44(5):578–585. doi: 10.1097/QAI.0b013e318033ff82. [DOI] [PubMed] [Google Scholar]
- 20.Tabet S, Sanchez J, Lama J, Goicochea P, Campos P, Rouillon M, et al. HIV, syphilis and heterosexual bridging among Peruvian men who have sex with men. AIDS. 2002;16(9):1271–1277. doi: 10.1097/00002030-200206140-00010. [DOI] [PubMed] [Google Scholar]
- 21.Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behav. 2012;16(6):1394–1410. doi: 10.1007/s10461-011-0131-8. [DOI] [PubMed] [Google Scholar]
- 22.Brown SA, Goldman MS, Inn A, LR A. Expectancies of reinforcement from alcohol: Their domain and relation to drinking patterns. J Consult Clin Psychol. 1980;48:419–426. doi: 10.1037//0022-006x.48.4.419. [DOI] [PubMed] [Google Scholar]
- 23.Mullens AB, Young RM, Dunne MP, Norton G. The Drinking Expectancy Questionnaire for Men who have Sex with Men (DEQ-MSM): a measure of substance-related beliefs. Drug and alcohol review. 2011;30(4):372–380. doi: 10.1111/j.1465-3362.2010.00225.x. [DOI] [PubMed] [Google Scholar]
- 24.Goodman LA. Snowball sampling. Ann Math Stat. 1961;32(1):148–170. [Google Scholar]
- 25.Brislin RW. Back-Translation for Cross-Cultural Research. J Cross-Cultural Psych. 1970;1:185–216. [Google Scholar]
- 26.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: The Alcohol Use Disorders Identification Test. Geneva, Switzerland: World Health Organization (W.H.O.); 2001. [Google Scholar]
- 27.MacCallum RC, Widaman KF, Zhang S, Hong S. Sample size in factor analysis. Psychological Methods. 1999;4(1):84–99. [Google Scholar]
- 28.George WH, Davis KC, Norris J, Heiman JR, Schacht RL, Stoner SA, et al. Alcohol and erectile response: the effects of high dosage in the context of demands to maximize sexual arousal. Experimental and clinical psychopharmacology. 2006;14(4):461–470. doi: 10.1037/1064-1297.14.4.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mutchler MG, McDavitt B, Gordon KK. "Becoming bold": alcohol use and sexual exploration among Black and Latino young men who have sex with men (YMSM) J Sex Res. 2014;51(6):696–710. doi: 10.1080/00224499.2013.772086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.George WH, Davis KC, Norris J, Heiman JR, Stoner SA, Schacht RL, et al. Indirect effects of acute alcohol intoxication on sexual risk-taking: The roles of subjective and physiological sexual arousal. Arch Sex Behav. 2009;38(4):498–513. doi: 10.1007/s10508-008-9346-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Knight KR, Das M, DeMicco E, Raiford JL, Matheson T, Shook A, et al. A roadmap for adapting an evidence-based HIV prevention intervention: personal cognitive counseling (PCC) for episodic substance-using men who have sex with men. Prev Sci. 2014;15(3):364–375. doi: 10.1007/s11121-013-0364-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Santos GM, Coffin PO, Vittinghoff E, DeMicco E, Das M, Matheson T, et al. Substance use and drinking outcomes in Personalized Cognitive Counseling randomized trial for episodic substance-using men who have sex with men. Drug Alcohol Depend. 2014;138:234–239. doi: 10.1016/j.drugalcdep.2014.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dilley JW, Woods WJ, Loeb L, Nelson K, Sheon N, Mullan J, et al. Brief cognitive counseling with HIV testing to reduce sexual risk among men who have sex with men: results from a randomized controlled trial using paraprofessional counselors. J Acquir Immune Defic Syndr. 2007;44(5):569–577. doi: 10.1097/QAI.0b013e318033ffbd. [DOI] [PubMed] [Google Scholar]
- 34.Dilley JW, Woods WJ, Sabatino J, Lihatsh T, Adler B, Casey S, et al. Changing sexual behavior among gay male repeat testers for HIV: a randomized, controlled trial of a single-session intervention. J Acquir Immune Defic Syndr. 2002;30(2):177–186. doi: 10.1097/00042560-200206010-00006. [DOI] [PubMed] [Google Scholar]