Abstract
Thailand is experiencing a development-associated health-risk transition with increasing prominence of chronic diseases. We aim to determine the risk factors for cardiovascular disease (CVD) deaths in Thailand. We conducted longitudinal analyses of deaths in the nationwide Thai Cohort Study from 2005 to 2010 (n=86866) using national vital registration data. Multivariate logistic regression models were used to calculate mutually adjusted estimates of association between dying from CVD and various risk factors measured at baseline in 2005. For three important risks, population attributable fractions were calculated. There were 78 CVD deaths. The probability of dying from CVD for males was 0.15% and for females was 0.04%. Multivariate modelling showed that current smoking (OR=4.01, CI=2.02-7.93), hypertension (OR=1.91, CI=0.95-3.85), and diabetes (OR=2.51, CI=1.01-6.25) are major risk factors of CVD deaths. For males, 54% of CVD deaths can be attributed to smoking. Females are protected by very low rates of smoking. Ischaemic heart disease (OR=6.85, CI=2.47-19.01) is also a strong predictor of CVD deaths. As CVD is a top cause of death, reducing CVD mortality by controlling smoking, hypertension, and hyperglycaemia will substantially improve life expectancy in Thailand today. The low smoking rates among females need to be actively maintained and confer great benefit.
Keywords: cardiovascular diseases, mortality, Thai Cohort study, cardiovascular risk factors, smoking
1. Introduction
In Thailand, in response to better nutrition, sanitation and health services over the last 20-40 years, deaths due to infectious disease, maternal mortality and child mortality have fallen (Sleigh, Seubsman, & Bain, 2008). Now, with changing lifestyles, diet and physical activity chronic diseases are rising. National vital statistics, corrected by verbal autopsy, now show cardiovascular disease (CVD) has become a leading cause of death for both men and women (Porapakkham et al., 2005; Kosulwat, 2002). For planning policy responses to such a profound health transition it is best to use national data on relevant risk patterns and associated local cause-specific mortality (Carmichael, 2011). Indeed, national level public health policy and practice are most effective when they respond to local data (Mahapatra et al., 2007). For example, trends in the developed world reveal continued problems with high rates of smoking among females, but in Thailand the female smoking rate remains negligible; evidently, local perspective needs to drive local responses to smoking.
There is limited published information on risk factors for CVD mortality in Thailand. However, two geographically restricted cohort studies (Electricity Generating Authority in Bangkok and the Khon Kaen Cohort Study) have reported that hypertension, diabetes, smoking, cholesterol and male sex are associated with CVD death (Sritara et al., 2003; Kamsa-Ard et al., 2013). National surveys also indicate that some internationally established risk factors for CVD (e.g. overweight and diabetes) have increased significantly in Thailand (Deerochanawong et al., 2013; Ministry of Public Health, 2011).
Since 2005, we have studied a cohort made up of over 85,000 Thai adults residing nationwide, the Thai Cohort Study (TCS). There were 78 CVD deaths in the cohort over the period 2005-2010, enough to provide an early picture of local risks and trends for this mortality category of emerging importance in transitional Thailand. The risks assessed include social, occupational, geographic, economic, environmental, dietary, psychological and behavioural factors, as well as physical activity and medical history. Here we present the risk metrics for those TCS members who died from CVD compared to those who survived over the period from 2005 to 2010. This information provides the detailed nationwide risk-mortality data needed to plan a response. It is the first report on CVD death from the TCS.
2. Methods
2.1 Baseline Information
We use exposure data (see below) from our Thai Cohort Study (TCS) baseline in 2005. TCS is a large longitudinal study (n=86,866) of the health consequences of socioeconomic development in a country experiencing a rapid transition to chronic diseases (Sleigh, Seubsman & Bain, 2008; Seubsman et al., 2011; Seubsman et al., 2012). Cohort participants resided nationwide and were initially aged 18-87 years with most in the 25-35 year age range. All were distance-learning students enrolled at Sukhothai Thammathirat Open University (STOU) and they provided detailed health-risk information by mailed questionnaire, a reliable technique with such well-educated informants used to mail based information exchange. Cohort members are employed in their local communities and most are of modest means, the constraints that led them to Open University. They represent well the STOU student body and the Thai population for field of study, ethnicity, religion, wealth and geographic residence (Seubsman et al., 2012).
Risk factor (‘exposure’) information gathered included sex, birth year, family history, income, civil status, health service access, the quality of health insurance coverage, cardiometabolic disease (doctor diagnosis of ischemic heart disease, hypertension, hyperlipidaemia, or diabetes), smoking, drinking, physical activity, emotional health problems, height and weight. In other studies we have re-measured self-reported height, weight, diabetes and hypertension all of which were of adequate accuracy for epidemiologic validity (Thawornchaisit et al., 2013; Lim, Seubsman, & Sleigh, 2009).
Reported monthly personal income in Thai Baht (1 US dollar = 35 Baht) was analysed in 4 categories (‘<=3000’, ‘3001−20000’, or ‘20001 and above’). We classified civil status as living with partner or not. Health service access was measured by a question that “in the past 12 months, have you personally used any of the following health services”; answers were “only use public services”, “used private services (at least once)”, and “others–neither public nor private”. We recorded health insurance coverage: “30 Baht scheme” (universal coverage available to all Thais since 2001, initially with a small co-payment of 30 baht or $US0.86), “civil servant benefit scheme”, and “others”. The family history variable, recorded in 2005, noted if mother or father had died from CVD (high blood pressure, heart disease, or stroke).
Health behaviours reported include smoking, alcohol consumption, and physical activities. Smoking was classified as ‘never’, ‘ex-smoker’, or ‘current smoker’. Alcohol consumption was classified as ‘occasional social drinker’, ‘never’, ‘current regular drinker’ or ‘now stopped’. Information on exercise-related weekly physical activity (PA) was obtained by asking: “during a typical week (7-day period) how many times on average do you do each of these physical activities”: ‘walking continuously for at least 10 minutes’; ‘mild exercise for more than 20 minutes’; ‘moderate physical activities for more than 20 minutes’; ‘vigorous physical actives for more than 20 minutes’. Metabolically-adjusted exercise-related PA (number of sessions) was calculated as ‘walking + mild + moderate physical activities + 2*vigorous physical activities’; finally, PA was recoded as ‘less than 7 sessions’ or ‘7 sessions or more’. This derived measure of PA was based on the International Physical Activity Questionnaire and the Active Australia Survey (Banks et al., 2011).
Emotional health problems were measured by the seventh question of the Short Form 8 Health Survey1: “during the past 4 weeks, how much have you been bothered by emotional problems (such as feeling anxious, depressed or irritable)?” The responses were categorized into not at all/very little/somewhat versus quite a lot/extremely. Body size was based on height and weight, evaluated as Body Mass Index (BMI). The BMI categories used Asian standards: underweight (less than 18.5), normal (18.5 to <23), at risk (23 to <25), obese I (25 to <30), and obese II (>=30) (Banks et al., 2011; Okubo et al., 2007).
2.2 Mortality Data
Death data come from the national Vital Registration with the Ministry of Interior and Minster of Public Health in Thailand. The 2005 TCS baseline data were linked to the mortality files using the citizen identification number which is unique for every Thai person. From 2005 to 2010, 580 deaths of cohort members were reported to the Ministry of Interior. Cause of death data were added by the Ministry of Public Health. The completeness of registration of adult deaths in Thailand was 86% from 1950-2000 (Mathers el al., 2005), but over the last decade coverage is thought to have improved to 95% (Prasutkul & Vapattanawong, 2006). For the study we report here, the vital statistics office at the Ministry of Public Health investigated cause of death for almost all those whose deaths were ill-defined by investigating hospital records and performing verbal autopsies. After this adjustment, ill-defined deaths were only 8.4% (N=49) of total deaths and there were 78 deaths from CVD.
2.3 Statistical Analysis
We used logistic regression to investigate associations between baseline exposures measured in 2005 and risk of dying from cardiovascular disease over the period 2005-2010. Exposures tested include smoking, drinking, physical activity, hypertension, hyperlipidaemia, diabetes, ischaemic heart disease, abnormal weight, and emotional problems. We also tested sex, birth year (five large subgroups – equivalent to 5 age groups), civil status, income, family history of CVD, health service use, and health insurance. We progressively introduced exposure variables into the model if their coefficients or likelihood ratio tests were statistically significant (p<0.05). Incoming variables were also included if they altered the estimates for other variables by changing their odds ratios by 10% or more. The Hosmer-Lemeshow test was used to confirm that the model was adequately fitted. In the final model, correlations between explanatory variables did not show significant multi-collinearity and the mean variance inflation factor value was 1.24. Individuals with missing data or dying from non-cardiovascular causes were excluded from the multivariate model of cardiovascular mortality, leaving 80585 for final analyses.
For the final statistical analyses, we calculate population attributable fractions (PAF) to estimate the proportion of CVD deaths in the population that would be avoided if certain important risk factors were removed. The formula used and sources of data are given with Table 3, along with the PAFs for smoking, hypertension, and diabetes.
Table 1.
Demographic characteristics of Thai Cohort study members who died of cardiovascular diseases, 2005-2010
| Cardiovascular Deaths n (%) | Other causes of death n (%) | Survived n (%) | Total n (%) | |||||
|---|---|---|---|---|---|---|---|---|
| Sex | ||||||||
| Males | 61 | (0.15%) | 338 | (0.86%) | 38998 | (98.99%) | 39397 | (100%) |
| Females | 17 | (0.04%) | 164 | (0.35%) | 47288 | (99.62%) | 47469 | (100%) |
| Birth year | ||||||||
| <1960 | 24 | (0.45%) | 88 | (1.63%) | 5273 | (97.92%) | 5385 | (100%) |
| 1960-1969 | 22 | (0.12%) | 121 | (0.67%) | 17894 | (99.21%) | 18037 | (100%) |
| 1970-1974 | 9 | (0.06%) | 81 | (0.53%) | 15184 | (99.41%) | 15274 | (100%) |
| 1975-1979 | 11 | (0.05%) | 97 | (0.44%) | 21901 | (99.51%) | 22009 | (100%) |
| 1980-1986 | 12 | (0.05%) | 115 | (0.44%) | 26034 | (99.51%) | 26161 | (100%) |
Table 2.
Risk factors for cardiovascular mortality, Thai Cohort Study (2005-2010)*
| Risk factors | Number of CVD deaths | Number Surviving** | Adjust OR (95%) | |
|---|---|---|---|---|
| Sex | ||||
| Males | 61 | 38998 | ref | |
| Females | 17 | 47288 | 0.43 | 0.21-0.87 |
| Birth cohort | ||||
| <1960 | 24 | 5273 | ref | |
| 1960-1969 | 22 | 17894 | 0.42 | 0.22-0.82 |
| 1970-1974 | 9 | 15184 | 0.19 | 0.08-0.47 |
| 1975-1979 | 11 | 21901 | 0.16 | 0.06-0.38 |
| 1980-1986 | 12 | 26034 | 0.17 | 0.07-0.41 |
| Civil status | ||||
| Not living with a partner | 34 | 44,975 | ref | |
| Living with partner | 42 | 38,789 | 0.52 | 0.29-0.94 |
| Drinking | ||||
| Occasional social drinker | 41 | 50972 | ref | |
| No, never | 16 | 22429 | 1.82 | 0.92-3.60 |
| Current regular drinker | 4 | 4116 | 0.58 | 0.20-1.67 |
| Used to drink before now stopped | 16 | 7617 | 1.64 | 0.86-3.15 |
| Smoking | ||||
| Never | 31 | 60612 | ref | |
| Ex-smoker | 20 | 14540 | 1.55 | 0.75-3.19 |
| Current Smoker | 25 | 8603 | 4.01 | 2.02-7.93 |
| BMI | ||||
| Normal | 34 | 46,372 | ref | |
| Underweight | 5 | 12,517 | 0.86 | 0.33-2.24 |
| At risk | 12 | 12,864 | 0.59 | 0.28-1.26 |
| Obese I | 17 | 11,201 | 0.96 | 0.51-1.83 |
| Obese II | 6 | 2,207 | 1.72 | 0.68-4.34 |
| Hypertension | ||||
| No | 62 | 82379 | ref | |
| Yes | 16 | 3907 | 1.91 | 0.95-3.85 |
| Diabetes | ||||
| No | 69 | 85419 | ref | |
| Yes | 9 | 867 | 2.51 | 1.01-6.25 |
| Ischaemic heart disease | ||||
| No | 72 | 85936 | ref | |
| Yes | 5 | 350 | 6.85 | 2.47-19.01 |
All odds ratios mutually adjusted
Deaths from other causes excluded.
Table 3.
Odds ratio (OR), risk factor prevalence and population-attributable risk (PAF)* of major risk factors for CVD deaths in Thai population
| Risk Factors | OR | Prevalence of Risk Factors (%)** | PAF (%) | |||
|---|---|---|---|---|---|---|
| Total | Males | Total | Males | Total | Males | |
| Current Smoking | 4.0 | 3.9 | 20.7 | 40.4 | 38.4 | 53.9 |
| Hypertension | 1.9 | 1.8 | 21.5 | 23.0 | 16.4 | 14.9 |
| Diabetes | 2.5 | 3.0 | 7.5 | 6.6 | 10.2 | 11.8 |
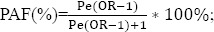 Pe is the prevalence of the risk factor in the Thai population (Webb & Bain 2011);
Pe is the prevalence of the risk factor in the Thai population (Webb & Bain 2011);
Prevalence in National Health Examination Survey, 2009 (Minister of Public Health 2011).
3. Results
Of 86866 cohort members analysed, 78 members died from CVD over the 5 years following the 2005 baseline survey (Table 1). The probability of dying from CVD for males (0.15%) was higher than for females (0.04%). The oldest group (born before 1960) had the highest probability of dying from CVD (0.45%) and the youngest birth cohorts (born from 1975 to 1986) had the lowest probability.
The multivariate odds ratios for each explanatory variable in the final model of CVD deaths are shown in Table 2. The estimates were mutually adjusted and the model fit the data well (Hosmer-Lemeshow test, p=0.73). Males had higher mortality odds and risk increased with age. Living with a partner lowered mortality significantly. Compared to never smokers, current smokers were at much higher risk of dying (OR=4.01, CI=2.02-7.93). Ex-smokers also had a higher risk of dying from CVD (OR=1.55, CI=0.75-3.19) but the risk was less than for current smokers. Over the observed time period (5 years) drinking categories were not significantly associated with dying from CVD.
Self-reported ischaemic heart disease was a very strong predictor of CVD death (OR=6.85, CI=2.47-19.01). In addition, people who reported having hypertension (OR=1.91, CI=0.95-3.85) or diabetes (OR=2.51, CI= 1.01-6.25) in 2005 had a greater risk of dying from CVD within five years and this increased risk was statistically significantly for diabetes and nearly significant for hypertension. There was an increased risk (OR=1.72, CI=0.68-4.34) of dying for obese people (BMI>=30), but this association was not significant in our time frame. However, if hypertension and diabetes were excluded in the model, the risk of dying for obese II people would increase to 2.26 (CI=0.92-5.51).
We also tested income, family history of dying from CVD, health services access, quality of health insurance, physical activity, emotional problems, and hyperlipidaemia. No significant relationship between these factors and dying from CVD within the five years was observed.
Table 3 summarises the population effects of smoking, hypertension, and diabetes. For these important risk factors, the table brings together the relative odds of CVD mortality estimated from our Thai Cohort Study, the population prevalence of these risk factors for adults reported by a recent national survey and the estimated population-attributable fractions (PAF%). As there were few (17) female deaths in our cohort we did not calculate the odds ratio or the fractions for females because estimates were too imprecise. We calculated our results for the whole population and then repeated the calculations restricted to males. The estimates for males used odds ratios from a male-only model of CVD deaths that included all the variables shown in Table 2. Odds ratios used for the whole population are listed in Table 2.
Our calculations show that hypertension accounts for 16% and diabetes for 10% of deaths from CVD in the Thai adult population. Current smoking is an even bigger problem as it caused 38% of CVD deaths in the Thai population and 54% of CVD deaths in the male portion of the population. This is indicates the current importance of smoking among Thai males. Also important are the data (not shown) for smoking rates among Thai females which remained very low both in the cohort (1%) and the general population (2%).
4. Discussion
Although the deaths in this relatively young nationwide Thai cohort are not yet numerous the associated risk factors cohere well to the pattern reported in developed countries around the world. This implies that CVD in Thailand is going to pose a substantial burden in the next 20-30 years. Our most important cohort-based observation was that among Thai males 54% of future CVD deaths could be avoided by prevention of smoking uptake. Also noteworthy is the related benefit conferred on Thai females by the very low smoking rates in that half of the population; maintenance of such low rates should be a fundamental public health goal for Thailand.
We also demonstrated that hypertension and diabetes are major current risk factors for deaths from CVD for Thais. In the whole population, PAF analyses reveals that 16% of CVD deaths are due to hypertension, and 10% are due to diabetes. As the prevalence of diabetes is rapidly increasing in Thailand (Deerochanawong et al., 2013), it can be expected that this disease will play a bigger role for CVD deaths in the future. Self-reported ischaemic heart disease is also a strong predictor of CVD deaths. BMI >=30 was also associated with dying from CVD, but this effect was not statistically significant in the relatively short time period monitored. Living with a partner halves the risk of dying from CVD. Social drinking was protective with a non-significant decrease in CVD mortality compared with those who never drank or those who stopped drinking.
Similar effects on CVD for smoking have been reported in other Asian populations (Asia Pacific Cohort Studies Collaboration, 2005). For example, in China, smoking is one of the most important contributors to the development of coronary heart disease (Zhang, Lu, & Liu, 2008). Our analyses also suggested that risk of dying from CVD attenuated when people stopped smoking. This is consistent with previous research showing that there is a substantial decrease in CVD mortality for former smokers compared with continuing smokers (Ockene & Miller, 1997; Critchley & Capewell, 2003). So prevention of smoking uptake is the most powerful intervention but cessation of smoking is also very effective for preventing CVD deaths.
In previous research, mostly focused on European populations, obesity has been associated with diabetes, hypertension, stroke, and ischaemic heart disease (Haslam & James, 2005). Recently, Zheng et al. (2011) have pooled the results for 120,700 deaths in 19 Asian cohort studies and showed that deaths from CVD increased when BMI exceeded 27.5. One other study in Thailand reported a weak increase in risk of all-cause mortality associated with BMI >= 35 among older men (Vapattanawong et al., 2010). In our study, the increased risk of deaths was unequivocal once BMI reached 30. But we note our cohort is still young and there were relatively few deaths observed over the relative short 5 year period. Also, much of the obesity effect on CVD mortality may operate through a causal pathway that includes diabetes and hypertension. When diabetes and hypertension were excluded in our model, the obesity-related risk of CVD death increased, approaching statistical significance.
The relationship between marital status and mortality has been repeatedly demonstrated in a large number of countries (Hu & Goldman, 1990). Married individuals have higher emotional and social support and lower stress (Lipowicz & Lopuszanska, 2005). Although psychological problems were controlled in our analyses, the protective effect of living with a partner remained significant. It is possible that social support may reduce CVD mortality not only through psychological factors but also through health care as well as through first-aid of CVD.
This study is one of the first attempts to link a large longitudinal study on multiple health risk factors with official CVD mortality data in South East Asia. National cause-of-death data in Thailand ten years ago had a high proportion of ill-defined deaths and inaccurate information (Porapakkham et al., 2005). However, in our study, after investigations by Ministry of Public Health, ill-defined deaths were reduced to 8.4% of total deaths and this decreased a major source of error. However, there may have been some other errors when measuring exposure variables in 2005.
In addition, our logistic regression may suffer from the problem of rare events data as there are only 78 CVD deaths over the five years (King & Zeng, 2001). To respond to this possibility, we re-tested the risk factor estimates of our models using both Exact Logistics Regression and Rare Events Logistic Regression, and the results varied by less than 10% to those we obtained from standard logistics regression. Furthermore we repeated the model underlying Table 2 using survival analysis and Poisson regression and the resulting Hazard Ratios and Incident Risk Ratios for each variable were virtually identical to the Logistic Regression estimates.
5. Conclusion
Cardiovascular disease is the top cause of death in Thailand, accounting for 27% of the mortality burden (Institute for Health Metrics and Evaluation, 2013). Mortality from CVD due to smoking, hypertension and diabetes is playing an important role in overall mortality with high population attributable fractions (38%─smoking, 16%─hypertension; 10%─diabetes). Given the high population prevalence of these three key risk factors, reducing CVD mortality by controlling smoking, hypertension, and hyperglycaemia will substantially improve life expectancy in Thailand today. Also important is the need for Thais to be conscious of preserving their culturally conferred population health advantage and ensure that the female half of population continues to avoid smoking.
References
- Asia Pacific Cohort Studies Collaboration. Smoking, quitting, and the risk of cardiovascular disease among women and men in the Asia-Pacific region. International Journal of Epidemiology. 2005;34(5):1036–45. doi: 10.1093/ije/dyi104. http://dx.doi.org/10.1093/ije/dyi104 . [DOI] [PubMed] [Google Scholar]
- Banks E, Lim L, Seubsman S, Bain C, Sleigh A. Relationship of obesity to physical activity, domestic activities, and sedentary behaviours:Cross-sectional findings from a national cohort of over 70,000 Thai adults. BMC Public Health. 2011;11(1):762. doi: 10.1186/1471-2458-11-762. http://dx.doi.org/10.1186/1471-2458-11-762 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmichael G. A. Exploring Thailand’s mortality transition with the aid of life tables. Asia Pacific Viewpoint. 2011;52(1):85–105. doi: 10.1111/j.1467-8373.2010.01436.x. http://dx.doi.org/10.1111/j.1467-8373.2010.01436.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Critchley J. A, Capewell S. Mortality risk reduction associated with smoking cessation in patients with coronary heart disease. Journal of the American Medical Association. 2003;290(1):86–97. doi: 10.1001/jama.290.1.86. http://dx.doi.org/10.1001/jama.290.1.86 . [DOI] [PubMed] [Google Scholar]
- Deerochanawong C, Ferrario A. Diabetes management in Thailand:A literature review of the burden, costs, and outcomes. Globalization and Health. 2013;9(1):11. doi: 10.1186/1744-8603-9-11. http://dx.doi.org/10.1186/1744-8603-9-11 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslam D. W, James W. P. T. Obesity. Lancet. 2005;366(9492):1197–209. doi: 10.1016/S0140-6736(05)67483-1. http://dx.doi.org/10.1016/S0140-6736(05)67483-1 . [DOI] [PubMed] [Google Scholar]
- Hu Y, Goldman N. Mortality differentials by marital status:an international comparison. Demography. 1990;27(2):233–50. http://dx.doi.org/10.2307/2061451 . [PubMed] [Google Scholar]
- Institute for Health Metrics and Evaluation. GBD Compare. 2013. Retrieved December 30, 2013, from http://viz.healthmetricsandevaluation.org/gbd-compare .
- Kamsa-Ard S, Promthet S, Lewington S, Burrett J. A, Sherliker P, Kamsa-Ard S, Wiangnon S, Parkin D. M. Association between smoking and mortality:Khon Kaen Cohort Study, Thailand. Asian Pacific Journal of Cancer Prevention. 2013;14(4):2643–7. doi: 10.7314/apjcp.2013.14.4.2643. http://dx.doi.org/10.7314/APJCP.2013.14.4.2643 . [DOI] [PubMed] [Google Scholar]
- King G, Zeng L. Logistic regression in rare events data. Political analysis. 2001;9(2):137–63. http://dx.doi.org/10.1093/oxfordjournals.pan.a004868 . [Google Scholar]
- Kosulwat V. The nutrition and health transition in Thailand. Public Health Nutrition. 2002;5(1a):183–89. doi: 10.1079/PHN2001292. http://dx.doi.org/10.1079/PHN2001292 . [DOI] [PubMed] [Google Scholar]
- Lim L, Seubsman S, Sleigh A. Validity of self-reported weight, height and body mass index among university students in Thailand:implications for population studies of obesity in developing countries. Population Health Metrics. 2009;7(15) doi: 10.1186/1478-7954-7-15. http://dx.doi.org/10.1186/1478-7954-7-15 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipowicz A, Lopuszanska M. Marital differences in blood pressure and the risk of hypertension among Polish men. European Journal of Epidemiology. 2005;20(5):421–27. doi: 10.1007/s10654-005-1752-x. http://dx.doi.org/10.1007/s10654-005-1752-x . [DOI] [PubMed] [Google Scholar]
- Mahapatra P, Shibuya K, Lopez A. D, Coullare F, Notzon F. C, Rao C, Szreter S. Civil registration systems and vital statistics:successes and missed opportunities. Lancet. 2007;370(9599):1653–1663. doi: 10.1016/S0140-6736(07)61308-7. http://dx.doi.org/10.1016/S0140-6736(07)61308-7 . [DOI] [PubMed] [Google Scholar]
- Mathers C. D, Fat D. M, Inoue M, Rao C, Lopez A. D. Counting the dead and what they died from:an assessment of the global status of cause of death data. Bulletin of the World Health Organization. 2005;83(3):171–177. [PMC free article] [PubMed] [Google Scholar]
- Ministry of Public Health. Thailand Health Profile Report 2008-2010. Bangkok: The War Veterans Organizations of Thailand; 2011. [Google Scholar]
- Ockene I. S, Miller N. H. For the American Heart Association Task force on risk reduction. cigarette smoking, cardiovascular disease, and stroke:a statement for healthcare professionals from the American Heart Association. Circulation. 1997;96(9):3243–47. doi: 10.1161/01.cir.96.9.3243. http://dx.doi.org/10.1161/01.CIR.96.9.3243 . [DOI] [PubMed] [Google Scholar]
- Okubo H, Sasaki S, Murakami K, Kim M. K, Takahashi Y, Hosoi Y, Itabashi M. Three major dietary patterns are all independently related to the risk of obesity among 3760 Japanese women aged 18–20 years. International Journal of Obesity. 2007;32(3):541–549. doi: 10.1038/sj.ijo.0803737. http://dx.doi.org/10.1038/sj.ijo.0803737 . [DOI] [PubMed] [Google Scholar]
- Porapakkham Y, Rao C, Pattaraarchachai J, Polprasert W, Vos T, Adair T, Lopez A. D. Estimated causes of death, Thailand 2005:implications for health policy. Population Health Metrics. 2010;8(14) doi: 10.1186/1478-7954-8-14. http://dx.doi.org/10.1186/1478-7954-8-14 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasartkul P, Vapattanawong P. The completeness of death registration in Thailand:evidence from demographic surveillance system of the Kanchanaburi Project. World Health and Population. 2006;8:43–51. doi: 10.12927/whp.2006.18054. http://dx.doi.org/10.12927/whp.2006.18054 . [DOI] [PubMed] [Google Scholar]
- Seubsman S, Kelly M, Sleigh A, Peungson J, Chokkanapitak J, Vilainerun D the Thai Cohort Study Team. Methods used for successful follow-up in a large scale national cohort study in Thailand. BMC Research Notes. 2011;4(1):166. doi: 10.1186/1756-0500-4-166. http://dx.doi.org/10.1186/1756-0500-4-166 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seubsman S, Yiengprugsawan V, Sleigh A. C. A large national Thai Cohort Study of the health-risk transition based on Sukhothai Thammathirat Open University students. ASEAN Journal of Open and Distance Learning. 2012;4(1) [PMC free article] [PubMed] [Google Scholar]
- Sleigh A. C, Seubsman S. A, Bain C. Cohort profile:the Thai cohort of 87 134 Open University students. International Journal of Epidemiology. 2008;37(2):266–72. doi: 10.1093/ije/dym161. http://dx.doi.org/10.1093/ije/dym161 . [DOI] [PubMed] [Google Scholar]
- Sritara P, Cheepudomwit S, Chapman N, Woodward M, Kositchaiwat C, Tunlayadechanont S, Yipintsoi T. Twelve year changes in vascular risk factors and their associations with mortality in a cohort of 3499 Thais:The Electricity Generating authority of Thailand study. International Journal of Epidmiology. 2003;32(3):461–468. doi: 10.1093/ije/dyg105. http://dx.doi.org/10.1093/ije/dyg105 . [DOI] [PubMed] [Google Scholar]
- Thawornchaisit P, De Looze F, Reid C. M, Seubsman S, Sleigh A. C. Validity of self-reported hypertension:Findings from the Thai Cohort Study compared to physician telephone interview. Global Journal of Health Science. 2013;6(2):1–11. doi: 10.5539/gjhs.v6n2p1. http://dx.doi.org/10.5539/gjhs.v6n2p1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vapattanawong P, Aekplakorn W, Rakchanyaban U, Prasartjul P, Porapakkham Y. Obesity and mortality among older Thais:A four year follow up study. BMC Public Health. 2010;10(1):604. doi: 10.1186/1471-2458-10-604. http://dx.doi.org/10.1186/1471-2458-10-604 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb P, Bain C. Essential Epidemiology:An Introduction for Students and Health Professional’s. Cambridge: Cambridge University Press; 2011. [Google Scholar]
- Zhang X. H, Lu Z. L, Liu L. Coronary heart disease in China. Heart. 2008;94(9):1126–31. doi: 10.1136/hrt.2007.132423. http://dx.doi.org/10.1136/hrt.2007.132423 . [DOI] [PubMed] [Google Scholar]
- Zheng W, McLerran D. F, Rolland B, Zhang X, Inoue M, Matsuo K, Potter J. D. Association between body-mass index and risk of death in more than 1 million Asians. New England Journal of Medicine. 2011;364(8):719–29. doi: 10.1056/NEJMoa1010679. http://dx.doi.org/10.1056/NEJMoa1010679 . [DOI] [PMC free article] [PubMed] [Google Scholar]


