Abstract
Palmer devised a classification system to guide treatment of triangular fibrocartilage complex tears in 1989. The main division is between traumatic Type I and atraumatic Type II tears. The wrist arthroscopy makes diagnosis and treatment of ulnar impaction syndrome possible in a less invasive way. Arthroscopy is the most valuable tool for diagnosis and treatment of acute scapholunate and lunotriquetral dissociation. Arthroscopic grading of Kienböck's disease better describes articular damage compared with plain radiographs and can help surgical treatment. The wrist arthroscopy generally makes it possible to make the diagnosis of the chondral lesion before they are visible by the usual imaging.
Abbreviations: TFCC, triangular fibrocartilage complex; DRUJ, distal radio ulnar joint; 6R, 6 radial portal (radial to extensor carpi ulnaris); SLIL, scapholunate interosseous ligament; LTILl, unotriquetral interosseous ligament; DRCL, dorsal radiocarpal ligament tear
Keywords: Wrist arthroscopy, Arthroscopic grading, TFCC
1. Introduction
Wrist arthroscopy has steadily grown from a mostly diagnostic tool to a valuable adjunctive procedure in the treatment of myriad wrist disorders, and the number of conditions that are amenable to arthroscopic treatment continues to grow.1
Through wrist arthroscopy, triangular fibrocartilage complex (TFCC) injury diagnosis, classification, and treatment can be performed arthroscopically, including distal ulna resection (wafer procedure). Also, direct visualization of the articular damage compared with plain radiographs in Kienböck's disease can help guide surgical treatment options. Arthroscopic assessment of intercarpal ligament injuries and instability is now considered the gold standard by many authors. Arthroscopy can also aid us in the management of post-traumatic capsular contraction, resection of ganglia, and the relatively rare isolated ulna styloid impaction.2
Although wrist arthroscopy can identify an anatomic abnormality, it cannot be used to differentiate between asymptomatic degenerative conditions versus a pathologic lesion that is the cause of wrist pain. A thorough wrist examination is still integral to any arthroscopic assessment.1
2. Triangular fibrocartilage complex
One of the most common uses for wrist arthroscopy is the diagnosis and treatment of disorders of the TFCC. TFCC provides stability to the DRUJ and acts as a load-bearing structure.3, 4, 5 As patients may have asymptomatic tears of the TFCC, the history and physical examination are of paramount importance.3
Palmer's classification of TFCC injuries can be used to help guide treatment (Table 1).6 This divides lesions into Type 1 (traumatic) and Type 2 (degenerative).2
Table 1.
Classification and treatment of TFCC tears.3
| Type of tear | Location of tear | Treatment recommendation |
|---|---|---|
| Traumatic | ||
| 1A | Tear in horizontal or central portion | Debridement |
| 1B | Tear from distal ulna insertion ± ulnar styloid fracture | Repair |
| 1C | Tear with ulnocarpal ligaments disrupted Tear of ulnolunate and ulnotriquetral ligaments |
Controversial, open repair or reconstruction |
| 1D | Tear from insertion at radius | Repair or debridement |
| Degenerative | ||
| IIA | TFCC wear but no perforation | Scope to confirm that the TFCC is intact, then ulnar shortening |
| IIB | TFCC wear but no perforation; chondromalacia of lunate or ulnar head | Scope to confirm that the TFCC is intact, then ulnar shortening |
| IIC | Central perforation of TFCC Chondromalacia of lunate or ulnar head |
Debridement of the TFCC and wafer procedure Alternative ulnar shortening |
| IID | Central perforation of TFCC; chondromalacia of lunate or ulnar head; perforation of LT ligament | Debridement of the TFCC and LTL, chondroplasty, possibly arthroscopic reduction and internal fixation of LT interval if unstable and/or ulnar shortening |
| IIE | Central perforation of TFCC; perforation of LT ligament; ulnocarpal arthritis | Debridement of joint or open salvage |
The classification of Type 1 TFCC injuries is based on the location of the tear (Fig. 1). Class 1A lesions involve the central or horizontal part of the TFCC. Class 1B lesions represent an avulsion of the peripheral aspect of the TFCC from its insertion onto the ulna (Fig. 1). Class 1C lesions occur when the ulnocarpal ligaments are disrupted. Class 1D lesions occur when the radial attachment of the TFCC is avulsed.7, 8
Fig. 1.

Type 1B TFCC tear.
Class 2 tears are staged according to the severity of degenerative changes involving the TFCC, ulnar head, ulnocarpal bones, and lunotriquetral ligament.6
All patients should have a trial of activity modification, splinting, and anti-inflammatory medication before embarking on surgical treatment. When non-operative treatment has been unsuccessful, wrist arthroscopy is indicated for the evaluation and treatment of TFCC injuries. On the basis of the location and size of the lesion, the surgeon may opt to either debride or repair the tear.3
Studies of the vascularity of the TFCC have shown that the central and radial aspects of the TFCC are relatively avascular.9 Class 1A lesions are routinely debrided and have little effect on forearm axial-load transmission or DRUJ kinematics.10, 11
Peripheral TFCC tears are often associated with DRUJ instability that requires repair (Fig. 2: arthroscopic outside in repair of Type 1A TFCC tear). Fortunately, it is the peripheral aspect of the TFCC that has sufficient blood supply to make repair feasible.3
Fig. 2.
Arthroscopic repair of the Type 1B TFCC tear.
Jantea et al.5 and Trumble et al.12 have suggested that class 1C and 1D tears of the TFCC may also be repaired.
Although the Palmer's classification system remains useful,13 it does not clarify the most critical issue: the presence or absence of DRUJ instability.14 In particular, the term “class 1B injury” is now being used to describe two distinct entities: a lesion that is fully stable at the DRUJ (i.e., central fibrocartilage disk separation from the dorsal wrist capsule) and a lesion that produces DRUJ instability (i.e., radioulnar ligament avulsion from the ulnar fovea). A great confusion has been generated in both the evaluation and management of class 1B injuries. The critical distinction is in differentiating injuries that produce instability of the distal radioulnar joint (DRUJ) from those that do not.14
Atzei and coworkers had developed a new classification attending to this important issue (Table 2). Based on the arthroscopic findings, five classes of TFCC peripheral tears are recognized, and guidelines for specific treatment can be considered.15
Table 2.
Atzei's TFCC complex peripheral tears classification.15
| Class | DRUJ instability | Affected TFCC part | TFCC healing | DRUJ cartilage | Treatment |
|---|---|---|---|---|---|
| 1 | None/slight | Distal | Good | Good | Suture |
| 2 | Mild/severe | Distal + proximal | Good | Good | Foveal reattachment |
| 3 | Mild/severe | Proximal | Good | Good | Foveal reattachment |
| 4 | Severe | Proximal | Poor | Good | Reconstruction |
| 5 | Mild/severe | – | – | Poor | Salvage |
In degenerative lesions, the positive ulnar variance must be addressed in addition to debridement of the TFCC tear. Impaction syndrome may be treated surgically by an extra-articular ulna shortening or a wafer procedure.3
Because of the efficacy of the open wafer distal ulna resection as a treatment for ulnar impaction syndrome, several authors have communicated good results with an arthroscopic wafer procedure for ulnocarpal abutment.16
Arthroscopic wafer resection is performed through the 3–4 and 6R portals (Fig. 3: arthroscopic wafer procedure). The central disk is excised using a basket forceps or a radiofrequency probe, it being mandatory that the dorsal and volar radioulnar ligaments are preserved. Once the ulnar head is visualized, a shaver is used to remove the remaining cartilage from the ulnar head. Afterwards, a 2.9 mm burr is advanced through the 6R portal and a 3 mm bony resection is affected.14
Fig. 3.
Arthroscopic wafer procedure.
2.1. Carpal instability
Disruption of the scapholunate interosseous ligament (SLIL) or lunotriquetral interosseous ligament (LTIL) may occur in isolation or as part of a more extensive perilunate wrist dislocation.17 Arthroscopy has become the gold standard for diagnosis of SLIL injuries, allowing direct vision of both intrinsic and extrinsic ligaments. The articular cartilage state can be checked under static condition as well as during the dynamic mode. We believe that all suspected injuries of the SLIL should undergo arthroscopy.14
Scapholunate instability without radiocarpal arthritis has been classified into pre-dynamic, dynamic, and static.18 Nowadays, there is a wide variety of arthroscopic classifications of this instability. Geissler and co-workers have proposed one which is the most widely used arthroscopic classification.19 Depending on the findings at the radiocarpal (Fig. 4) and midcarpal (Fig. 5) arthroscopy, it provides four degrees of injury (Table 3).14
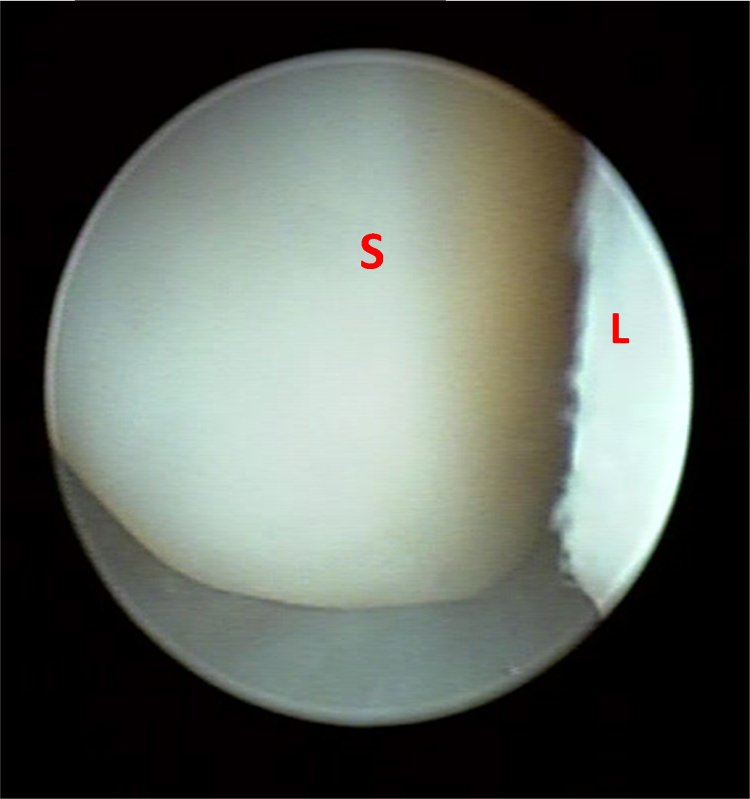
Fig. 4.
Radio carpal view of Gissler 4 SLL tear.
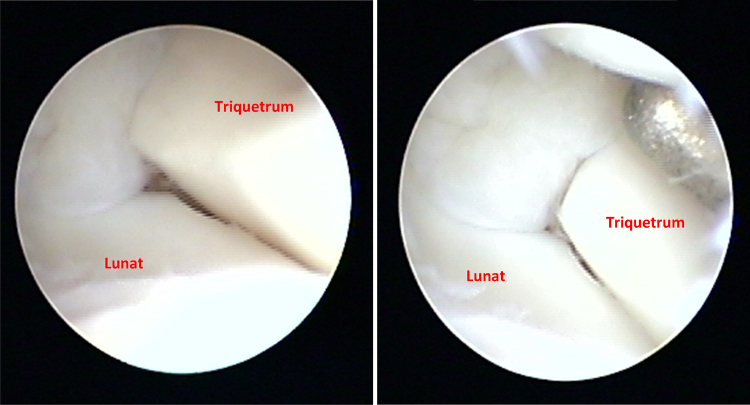
Fig. 5.
Midcarpal view of Gissler 2 LTL tear.
Table 3.
Geissler's interosseous ligament injury classification.18
| Grade | Radiocarpal Joint | Midcarpal view | Carpal bone gap |
|---|---|---|---|
| 1 | Attenuation/Hemorrhage of interosseous ligament | No incongruence/step off | None |
| 2 | Attenuation/Hemorrhage of interosseous ligament | Incongruence/step off of the carpal alignment | Less than the width of the probe |
| 3 | Incongruence/step off of the carpal alignment | Incongruence/step off of the carpal alignment | Probe passes between the carpal bones |
| 4 | Incongruence/step off of the carpal alignment | Incongruence/step off of the carpal alignment | 2.7 mm arthroscope passes between the carpal bone |
Many of the SLIL injuries can be managed arthroscopically. Partial SLIL tears, without evidence of instability (pre-dynamic stage) can be addressed by means of debridement of the damaged tissue using a basket forceps or a radiofrequency probe.14
Grading the severity of injury is perhaps the most important step in the entire procedure of arthroscopic treatment of SLIL and LTIL. Grading the degree of LTIL disruption is done using a dynamic stress examination (Table 4). The scope and probe portals are reversed for grading the SLIL disruption.17
Table 4.
Arthroscopic classification and treatment of intrinsic ligament instability.17
| Grade | Diastasis | Average of three midcarpal stress shift tests: distraction, translation, rotation | Treatment |
|---|---|---|---|
| I | Volar opening of 2.3 mm, no dorsal opening | Less than 10% shift | Partial tear does not require pin stabilization |
| II | 2.3 mm or greater diastasis, both dorsally and volarly | Shifts between 10% and 25%: A: radiocarpal view, ligament reduced to normal bed B: radiocarpal view, ligament free edge not reduced |
A: arthroscopic repair with early mobilization B: limited open direct anchor repair of ligament edge |
| III | 2.5 mm or greater diastasis | Shifts > 25%: A: radiocarpal view, ligament reduced to normal bed B: radiocarpal view, ligament free edge not reduced |
A: arthroscopic repair, no early mobilization owing to damaged secondary stabilizing ligaments B: limited open direct repair of ligament edge |
Mild forms of lunotriquetral instability can be treated with ulnocarpal ligament shrinkage. This procedure takes advantage of the anatomy of the ulnotriquetral and ulnolunate ligaments and these ligaments form a “V” as they diverge from their origin on the palmar distal radioulnar ligament and insert on the palmar aspect of the lunate or triquetrum.1
In cases where instability is seen (dynamic stage), debridement alone is not sufficient. There is a current controversy regarding the best treatment for these injuries. Some studies are reporting good results with arthroscopic debridement and thermal shrinkage.20, 21 When faced with a reducible static scapholunate instability, Villanova and Del Pino14 recommended an arthroscopic reduction of the scaphoid-lunate articulation, that has been described by Hausman et al.22
2.2. Dorsal radiocarpal ligament tear (DRCL)
In most series, the DRCL is overlooked during the standard arthroscopic examination because it is difficult to visualize through the standard dorsal portals. The DRCL is best viewed through the volar radial portal due to the straight line of sight. Isolated DRCL tears respond favorably to repair. Repairs may also be considered in cases in which the associated interosseous ligament tear or TFCC tear can be treated arthroscopically. A classification scheme for DRCL tears and its treatment is presented in Table 5.1, 23
Table 5.
| Stage | Description | Treatment |
|---|---|---|
| 1 | Isolated DRCL tear | Arthroscopic DRCL repair |
| 2 | DRCL with associated SLIL or LTIL (Geissler I/II) or TFCC tear or midcarpal instability | Arthroscopic DRCL repair, SLIL or LTIL debridement ± shrinkage, TFCC repair/debridement ± wafer |
| 3A | DRCL tear with associated SLIL and/or LTIL (Geissler III) and/or TFCC tear | Arthroscopic DRCL repair, SLIL/LTIL shrinkage ± pinning, TFCC repair/debridement ± wafer |
| 3B | DRCL tear with SLIL and/or LTIL (Geissler IV) and/or TFCC tear | Open SLIL repair/reconstruction ± capsulodesis, LTIL repair/reconstruction, TFC repair/debridement ± wafer |
| 4 | DRCL with chondromalacia or widespread degenerative changes | Partial carpal fusion versus PRC |
2.3. Kienböck's disease
Historically, the radiologic classification of Kienböck's disease of Lichtman et al.24 has been used to assess the condition, although its reliability has been shown to be poor.25 Arthroscopy provides direct visualization and assessment of the pathology in the radiocarpal and midcarpal joints. The disparity between radiographic assessment and arthroscopic assessment has been highlighted by Ribak,26 who reported that plain radiographs were poorly correlated with arthroscopic findings.2
Wrist arthroscopy has become a valuable assessment and a primary treatment tool for Kienböck's disease. It allows identification of the nonfunctional joints and tailoring of the surgical reconstructions depending on the anatomic findings.14
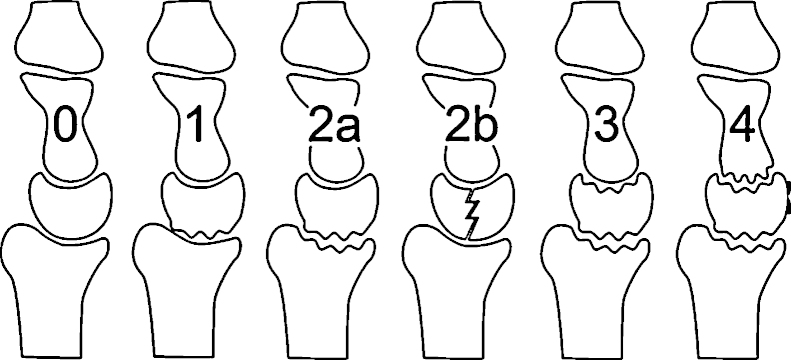
Bain and Begg described an arthroscopic classification for Kienböck's disease based on the number of articular surfaces involved (Fig. 6).27 In Grade 0, all articular surfaces are normal; hence, an extra-articular unloading procedure may be indicated. Grade 1 consists of 1 nonfunctional proximal lunate surface, which can be treated with a proximal row carpectomy, radioscapholunate arthrodesis, or lunate excision and scaphocapitate arthrodesis. In Grade 2, the proximal and distal lunate surfaces are nonfunctional, which requires a proximal row carpectomy or scaphocapitate arthrodesis. Grade 3 consists of nonfunctional articular surfaces of the proximal and distal lunate facet and the lunate facet of the radius. In Grade 4, all 4 articular facets are nonfunctional; hence, both require total wrist arthrodesis or arthroplasty (Table 6).28
Fig. 6.
Arthroscopic classification of Kienböck's disease adopted from Bain GI, Begg M. Arthroscopic assessment and classification of Kienbock's disease. Tech Hand Up Extrem Surg 2006;10:8–13.
Table 6.
Arthroscopic classification and treatment of Kienböck's disease.26
| Grade | Articular surfaces involved | Treatment |
|---|---|---|
| 0 | Non | Extra-articular unloading |
| 1 | Proximal lunate surface | PRC, RSL arthrodesis or lunate excision and SC arthrodesis |
| 2 | The proximal + distal lunate surfaces | PRC, or SC arthrodesis |
| 3 | Proximal and distal lunate facet + the lunate facet of the radius | Total wrist arthrodesis or arthroplasty |
| 4 | All 4 articular facets are nonfunctional | Total wrist arthrodesis or arthroplasty |
2.4. Chondroplasty and loose bodies
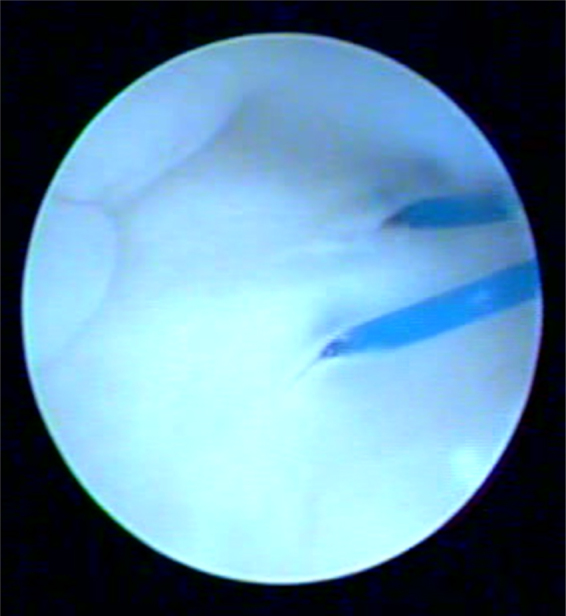
Articular cartilage damage is a common cause of wrist pain; it may result from osteochondral fractures, chronic carpal instability, or chondromatosis, or it may occur idiopathically. Loose bodies are common sequelae of osteoarthritis. They may also be seen in avascular necrosis due to sloughing of a cartilage defect. Loose bodies give rise to pain and locking (Fig. 7: loose body in the radiocarpal joint), which is relieved following arthroscopic removal.1
Fig. 7.

Loose body.
Wrist arthroscopy is the best way to assess chondral defects. When non-operative therapy has failed to provide relief of symptoms caused by a cartilaginous lesion, arthroscopic management can relieve the discomfort, synovitis, and crepitation. Chondroplasty and removal of loose bodies may assist in the reduction of wrist pain. As the wrist is a non-weight-bearing joint, the results are often better than those obtained with knee arthroscopy.3
Culp et al.28 have provided a modified Outerbridge classification for chondral lesions in the wrist (Table 7) in which Grade I represents softening of the hyaline surface, Grade II consists of fibrillation and fissuring, Grade III represents a fibrillated lesion of varying depth in the articular surface, and Grade IV has a full-thickness defect down to bone. Grades I–III lesions are treated with debridement and localized synovectomy. Localized Grade IV lesions can be treated with abrasion chondroplasty and subchondral drilling.1
Table 7.
Modified Outerbridge classification and treatment of chondral lesions in the wrist.1
| Grade | Cartilage lesion | Treatment |
|---|---|---|
| 1 | Softening | Debridement and localized synovectomy |
| 2 | Fibrillation and fissuring | Debridement and localized synovectomy |
| 3 | Fibrillated lesion of varying depth | Debridement and localized synovectomy |
| 4 | Full-thickness defect down to bone | Abrasion chondroplasty and subchondral drilling |
2.5. Wrist contracture
Patients lacking a functional arc of wrist motion who have failed a trial of dynamic/static progressive splinting are candidates for arthroscopic release of wrist construction.1
Lee and Hausman et al.29 devised a classification system based on pathologic anatomic location (Table 8). Type I represents intrinsic adhesions, which are subdivided into radiocarpal (A), midcarpal (B), DRUJ (C), and combined (D). Type II represents extrinsic contracture, which can be dorsal (A), volar (B), DRUJ (C), and combined (D). The surgical approach should be wrist arthroscopy for Types IA (radiocarpal adhesions) and IB (midcarpal adhesions) where intra-articular adhesions are present. Types IC (DRUJ adhesions) and IIC (DRUJ capsular contracture) are best approached in an open manner where dorsal and palmar capsulectomies of the DRUJ are performed. For Types IIA, B, and D (dorsal, palmar, and combination extrinsic contracture, respectively), both open and arthroscopic methods are used.
Table 8.
Wrist arthrofibrosis classification and treatment.1
| Type | Site of arthrofibrosis | Treatment |
|---|---|---|
| Type I | Intrinsic (adhesions) | |
| A | Radiocarpal joint | Arthroscopic release |
| B | Midcarpal joint | Arthroscopic release |
| C | Distal radioulnar joint | Open release |
| D | Combination of above | Open release |
| Type II | Extrinsic (capsular fibrosis) | |
| A | Dorsal | Arthroscopic/open release |
| B | Palmar | Arthroscopic/open release |
| C | Distal radioulnar joint | Arthroscopic/open release |
| D | Combination of above | Arthroscopic/open release |
3. Conclusion
Wrist arthroscopy has become an essential tool for the hand and upper extremity surgeon. It is useful in diagnosing and/or staging a wide range of conditions of the wrist, including TFCC tears, Kienböck's disease, ligament injury, and cartilage injury. It can be of great benefit in evaluating wrist pain of unclear cause when imaging studies fail to elucidate the disease.
Wrist arthroscopy has steadily grown from a mostly diagnostic tool to a valuable adjunctive procedure in the treatment of myriad wrist disorders. The number of conditions that are amenable to arthroscopic treatment continues to grow. A detailed knowledge of the topographical and intracarpal anatomy, however, is essential to minimize complications and maximize the benefits.
Authors’ contributions
M.B. participated in the sequence alignment and drafted the manuscript, H.E. participated in its design and coordination and helped to draft the manuscript, H.G. conceived the study, A.E. and W.S. collected the data about the whole subject.
Conflicts of interest
All authors have none to declare.
References
- 1.Slutsky D.J., Nagle D.J. Wrist arthroscopy: current concepts. J Hand Surg. 2008;33A:1228–1244. doi: 10.1016/j.jhsa.2008.07.015. [DOI] [PubMed] [Google Scholar]
- 2.Bain G., Munt J., Turner P.C. New advances in wrist arthroscopy. Arthroscopy. 2008;24:355e67. doi: 10.1016/j.arthro.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Gupta R., Bozentka D.J., Lee Osterman A. Wrist arthroscopy: principles and clinical applications. J Am Acad Orthop Surg. 2001;9 doi: 10.5435/00124635-200105000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Bednar J.M., Osterman A.L. The role of arthroscopy in the treatment of traumatic triangular fibrocartilage injuries. Hand Clin. 1994;10:605–614. 14. [PubMed] [Google Scholar]
- 5.Jantea C.L., Baltzer A., Rüther W. Arthroscopic repair of radial-sided lesions of the triangular fibrocartilage complex. Hand Clin. 1995;11:31–36. [PubMed] [Google Scholar]
- 6.Palmer A.K. Triangular fibrocartilage complex lesions: a classification. J Hand Surg [Am] 1989;14:594–606. doi: 10.1016/0363-5023(89)90174-3. [DOI] [PubMed] [Google Scholar]
- 7.Palmer A.K., Werner F.W. The triangular fibrocartilage complex of the wrist: anatomy and function. J Hand Surg [Am] 1981;6:153–162. doi: 10.1016/s0363-5023(81)80170-0. [DOI] [PubMed] [Google Scholar]
- 8.Trumble T.E., Dodds S.D. The peripheral tears of TFCC: diagnosis and management. In: Slutsky D.J., Nagle D.J., editors. Techniques in Wrist and Hand Arthroscopy. Elsevier, Inc.; Philadelphia: 2007. pp. 127–135. [Google Scholar]
- 9.Bednar M.S., Arnoczky S.P., Weiland A.J. The microvasculature of the triangular fibrocartilage complex: its clinical significance. J Hand Surg [Am] 1991;16:1101–1105. doi: 10.1016/s0363-5023(10)80074-7. [DOI] [PubMed] [Google Scholar]
- 10.Palmer A.K., Werner F.W., Glisson R.R., Murphy D.J. Partial excision of the triangular fibrocartilage complex. J Hand Surg [Am] 1988;13:391–394. doi: 10.1016/s0363-5023(88)80015-7. [DOI] [PubMed] [Google Scholar]
- 11.Adams B.D. Partial excision of the triangular fibrocartilage complex articular disk: a biomechanical study. J Hand Surg [Am] 1993;18:334–340. doi: 10.1016/0363-5023(93)90371-9. [DOI] [PubMed] [Google Scholar]
- 12.Trumble T.E., Gilbert M., Vedder N. Isolated tears of the triangular fibrocartilage: management by early arthroscopic repair. J Hand Surg [Am] 1997;22:57–65. doi: 10.1016/S0363-5023(05)80180-7. [DOI] [PubMed] [Google Scholar]
- 13.Palmer A.K. Triangular fibrocartilage disorders: injury patterns and treatment. Arthroscopy. 1990;6:125e32. doi: 10.1016/0749-8063(90)90013-4. [DOI] [PubMed] [Google Scholar]
- 14.Villanova J.F., Del Pino J.G. Wrist arthroscopy. Mini symposium: the hand. Orthp Trauma. 2011;25:344–352. [Google Scholar]
- 15.Atzei A., Rizzo A., Luchetti R., Fairplay T. Arthroscopic foveal repair of triangular fibrocartilage complex peripheral lesion with distal radioulnar joint instability. Tech Hand Up Extrem Surg. 2008;12:226e35. doi: 10.1097/BTH.0b013e3181901b1. [DOI] [PubMed] [Google Scholar]
- 16.Tomaino M.M., Weiser R.W. Combined arthroscopic TFCC debridement and wafer resection of the distal ulna in wrists with triangular fibrocartilage complex tears and positive ulnar variance. J Hand Surg [Am] 2001;26:1047e452. doi: 10.1053/jhsu.2001.28757. [DOI] [PubMed] [Google Scholar]
- 17.Henry M. Arthroscopic treatment of acute scapholunate and lunotriquetral ligament injuries. Atlas Hand Clin. 2004;9:187–197. [Google Scholar]
- 18.Watson H., Ottoni L., Pitts E.C., Handal A.G. Rotary subluxation of the scaphoid: a spectrum of instability. J Hand Surg [Br] 1993;18:62e4. doi: 10.1016/0266-7681(93)90199-p. [DOI] [PubMed] [Google Scholar]
- 19.Geissler W.B., Freeland A.E., Savoie F.H. Carpal instability associated with intra-articular distal radius fractures. Proc AAOS; San Francisco; 1993. [Google Scholar]
- 20.Darlis N.A., Weiser R.W., Sotereanos D.G. Partial scapholunate ligament injuries treated with arthroscopic debridement and thermal shrinkage. J Hand Surg [Am] 2005;30:908e14. doi: 10.1016/j.jhsa.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 21.Hirsh L., Sodha S., Bozentka D. Arthroscopic electrothermal collagen shrinkage for symptomatic laxity of the scapholunate interosseous ligament. J Hand Surg [Br] 2005;30:643e7. doi: 10.1016/j.jhsb.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 22.Hausman M.R. Arthroscopic RASL. In: Slutsky D., Nagle D., editors. Techniques in Wrist and Hand Arthroscopy. Churchill Livingstone; Philadelphia: 2007. p. 79e85. [Google Scholar]
- 23.Slutsky D.J. The incidence of dorsal radiocarpal ligament tears in the presence of other intercarpal derangements. Arthroscopy. 2008;24:526–533. doi: 10.1016/j.arthro.2007.12.014. [DOI] [PubMed] [Google Scholar]
- 24.Lichtman D.M., Mack G.R., MacDonald R.I., Gunther S.F., Wilson J.N. Kienbock's disease: the role of silicone replacement arthroplasty. J Bone Jt Surg Am. 1977;59:899–908. [PubMed] [Google Scholar]
- 25.Goldfarb C.A., Hsu J., Gelberman R.H., Boyer M.I. The Lichtman classification for Kienbock's disease: an assessment of reliability. J Hand Surg [Am] 2003;28:74–80. doi: 10.1053/jhsu.2003.50035. [DOI] [PubMed] [Google Scholar]
- 26.Ribak S. Presented at the 10th Triennial Congress of the International Federation of Societies for Surgery of the Hand, Sydney, March; 2007. The importance of wrist arthroscopy for staging and treatment of Kienbock's disease. [Google Scholar]
- 27.Bain G.I., Begg M. Arthroscopic assessment and classification of Kienbock's disease. Tech Hand Up Extrem Surg. 2006;10:8–13. doi: 10.1097/00130911-200603000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Culp R., Osterman A.L., Kaufmann R.A. Wrist arthroscopy: operative procedures. In: Green D.P., Hotchkiss R.N., Pederson W.C., Wolfe S.W., editors. Green's Operative Hand Surgery. 5th ed. Churchill Livingstone; New York: 2005. pp. 781–803. [Google Scholar]
- 29.Lee S.K., Gargano F., Hausman M.R. Wrist arthrofibrosis. Hand Clin. 2006;22:529–538. doi: 10.1016/j.hcl.2006.09.002. [abstract vii] [DOI] [PubMed] [Google Scholar]