Abstract
Chondroblastoma is a rare, benign cartilaginous neoplasm that accounts for approximately 1% of all bone tumors, and approximately 4% of all chondroblastomas arise in the clavicle. Here, we report a case of chondroblastoma in the right clavicle. 27-year-old female patient presented with a 12-month history of shoulder pain. Based on radiological and pathological examination, the diagnosis was compatible with chondroblastoma. After resection of the tumor, 1 cm of the distal clavicle was preserved, 15 cm of the non-vascularized fibula was taken from the contralateral leg and placed on the site of the clavicle and fixed with hook plate at distal clavicle and reconstruction plate attached to the sternum. 13 months of follow-up is scheduled for removal of osteosynthesis material, finding full consolidation of sternoclavicular segment and the distal segment. A good functional outcome was apparent after a limited 14-month follow-up, and the patient was highly satisfied with the result. We found no recurrence or metastasis.
Keywords: Chondroblastoma, Non-vascularized fibular, Autograft, Clavicular tumors, Reconstruction
1. Introduction
Chondroblastoma is an uncommon benign bone tumor arising from a secondary ossification center. It usually occurs in adolescents and young adults and involves the tibia, accounts for approximately 1% of all bone tumors, and approximately 4% of all chondroblastomas arise in the clavicle. The purported neoplastic cell is the chondroblast, a cell that normally populates areas of secondary ossification. Rare cases have been reported in the talus, calcaneus, and many of these involve metacarpals or metatarsals, which may lack a true anatomic diaphysis.1 Although the lesions frequently are treated satisfactorily with intralesional procedures, such as curettage, they are sometimes very aggressive locally and require marginal or wide resection. A total claviculectomy is the procedure of choice if a definitive cure is the goal for clavicular tumors.2, 3
2. Case
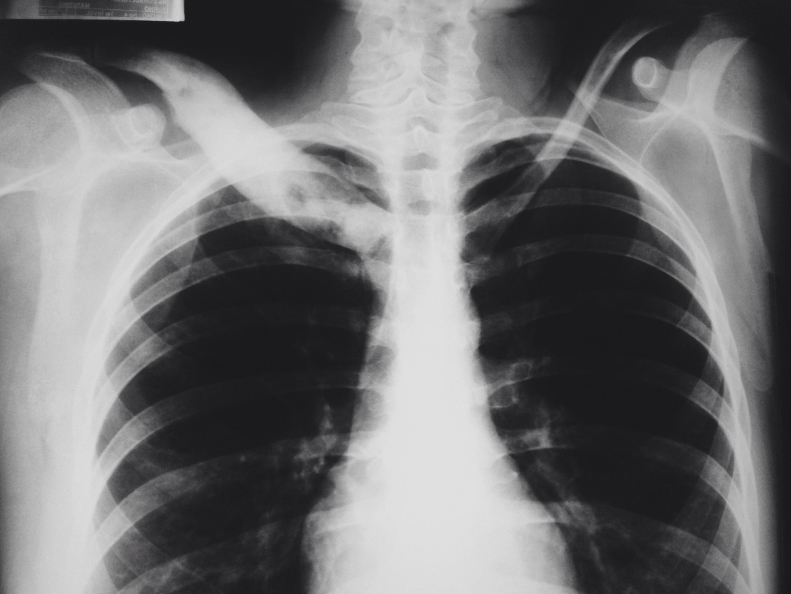
A 27-year-old female patient presented with a 14-month history of shoulder pain, pain and palpable mass in the right clavicle region, and pain on movement of the shoulder, mainly flexion and abduction. There was tenderness in clavicular region and distal sensitivity was preserved. Plain radiograph and CT scan show circumscribed lesion with sclerotic margins and lytic appearance inside without periosteal reaction (Fig. 1, Fig. 2).
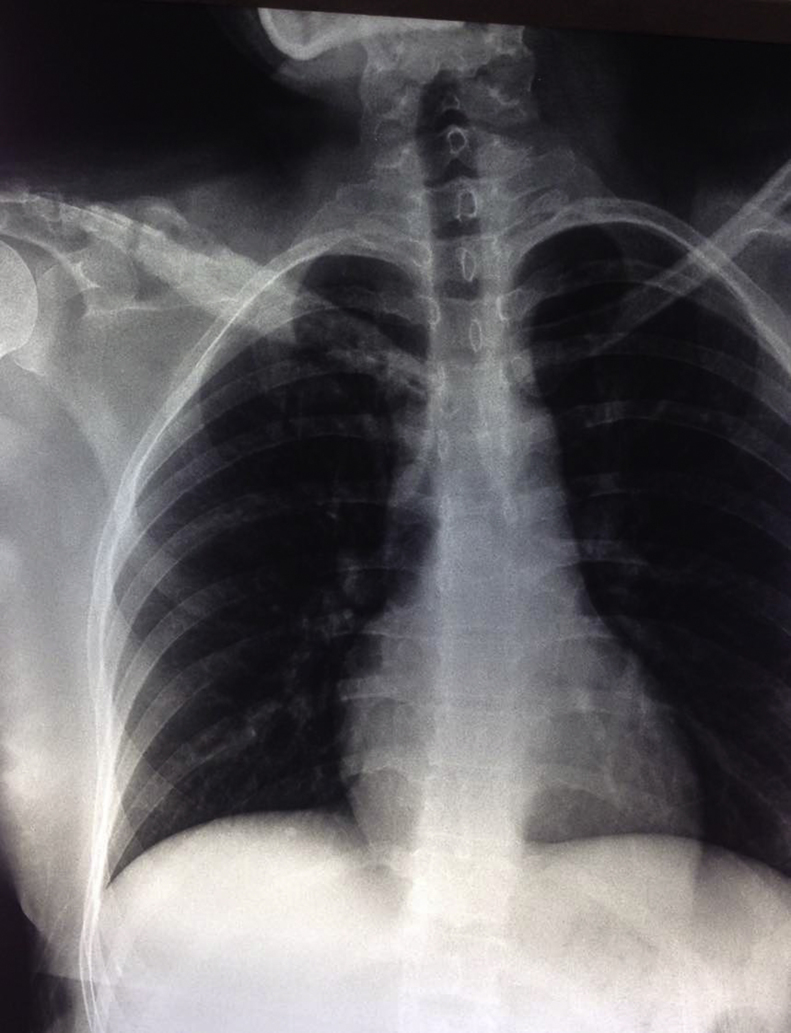
Fig. 1.
Thoracic X-ray. Circumscribed lesion in the right clavicle.
Fig. 2.
CT scan – sclerotic margins and lytic appearance.
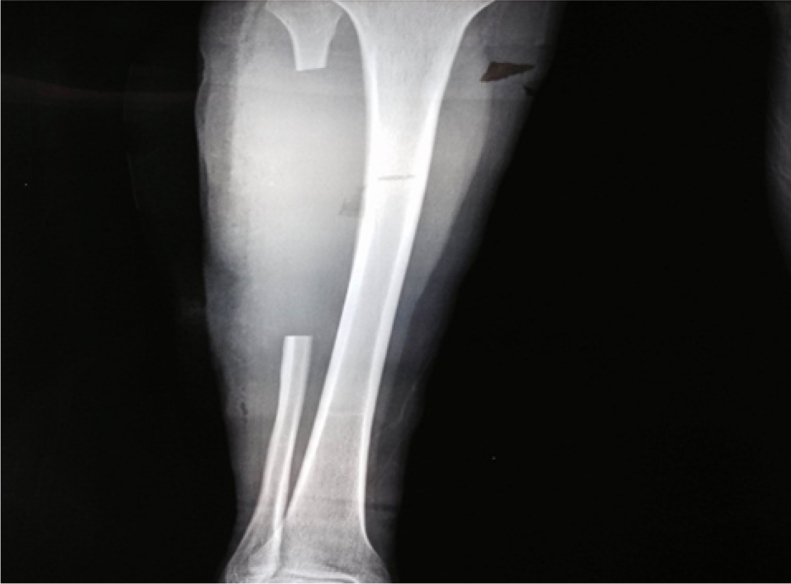
Incisional biopsy was performed for histopathological examination. Reports revealed chondroblastoma. She was scheduled for surgery, performing tumor resection, leaving 1.5 cm of distal clavicle unaltered and complete resection of the proximal segment (Fig. 3).
Fig. 3.
Intraoperative resection.
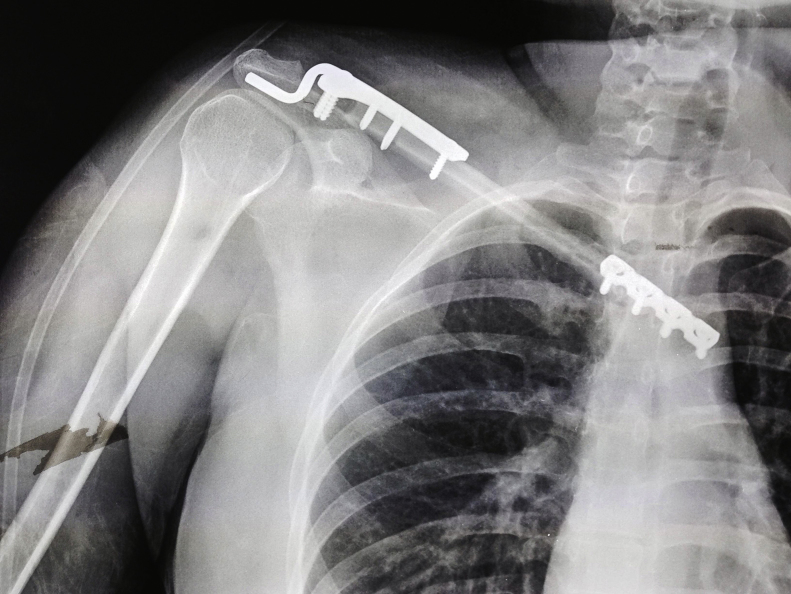
Reconstruction of the defect is performed with autologous non-vascularized fibula and fixed with hook plate in the distal segment and reconstruction plate attached to the sternum. Decortication around the fibula is made and demineralized bone matrix is placed in distal and proximal segment (Fig. 4, Fig. 5).
Fig. 4.
Fibular autograft.
Fig. 5.
Fibular autograft attached to the distal clavicle and sternum.
In the immediate postoperative the patient reports, mild pain, distal sensitivity unaltered, muscle strength decreased by pain, is discharged after 3 days (Fig. 6).
Fig. 6.
Postoperative radiograph.
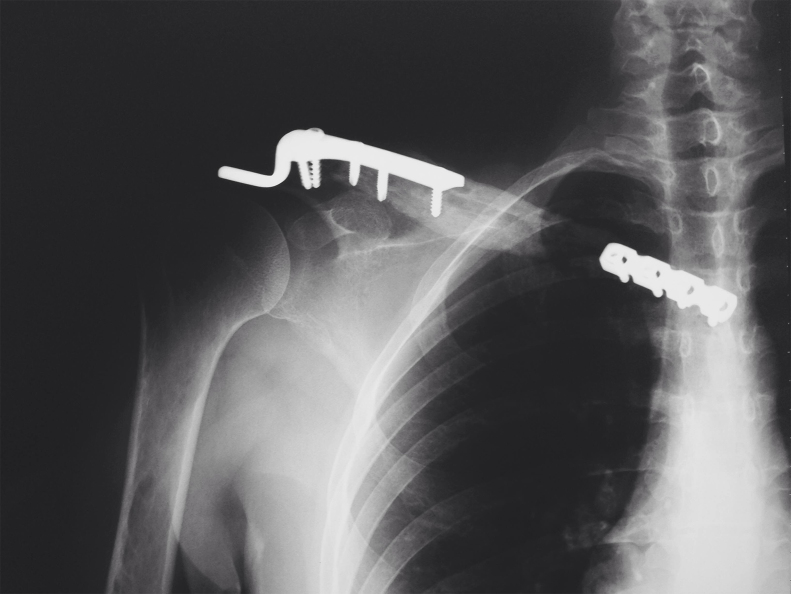
13 months of follow-up is scheduled for removal of osteosynthesis material, finding full consolidation of sternoclavicular segment and the distal segment (Fig. 7).
Fig. 7.
Radiography after 12 months of follow-up (this image is in another position within the manuscript, so the confusion).
Follow-up at 14 months, limitation of abduction, 80 degrees, flexion 90, extension 20 (Fig. 8, Fig. 9), all this without pain and that does not stop their daily activities, the limitation of abduction, further the wide resection, can be explained by irritation of the rotator cuff by the hook plate, and it is expected that rehabilitation will improve range of motion. Bony union was achieved in this case, and there was no recurrence (Fig. 10).
Fig. 8.
Patient with right shoulder abduction.
Fig. 9.
Patient with right shoulder flexion.
Fig. 10.
Radiography after 14 months of follow-up, full consolidation is shown.
3. Discussion
Chondroblastoma term was first described in 1942 by Jaffe and Lichtenstein. It is a rare tumor of cartilaginous origin, with a peak incidence at ages 10–25 years, with a predilection for the male gender ratio 2:1, representing 1% of bone tumors.2, 3 The clavicle is a strange place to tumors has been reported an incidence of 0.45–1.01% of all bone tumors and the experience is limited.4 The distal femur, proximal humerus, and proximaltibia are the most common sites of occurrence.3, 4 Radiographic findings usually presented well-circumscribed lesion that is centered in an epiphysis of a long bone; however, it also may be located in the mid bone. In adults, it must be differentiated from giant cell tumor, and it differs in that it does not usually present intratumoral calcifications, no thin layer sclerosis, affecting soft tissues surrounding the lesion.4
At follow-up, radiograph should be obtained from the site of the tumor and chest every 6 months for 3 years, and annually thereafter. Has been reported recurrence 10–20% to 1–40% by some authors. Metastasis occurs in 1% of cases and usually benign lung and which are managed with resection. Malignant transformation is rare. However, there have been reports of chondroblastomas with aggressive behavior, with articular invasion at diagnosis.5
A few reports have documented satisfied oncologic results with subtotal or total claviculectomy. Although relatively good functional results after claviculectomy without reconstruction others have suggested reconstruction with an allograft or vascularized fibula after claviculectomy. Complications of performing reconstruction are nonunion, infection of the graft, and surgical site. Reconstruction patients often require more time for rehabilitation. Some patients continue to have chronic pain following claviculectomy. Reconstruction is recommended for patients with benign tumors with good prognosis.6, 7, 11 The clavicle tumors can be managed with partial or total claviculectomy. There is currently no consensus recommending the reconstruction after resection of clavicle because the functional prognosis as reported by previous cases following total claviculectomy is good returning to previous occupational activities.8, 9
There have been reports of non-vascularized fibular graft for reconstruction of bone defects presenting good clinical and radiological results. Non-vascularized autogenous bone grafts are biologically active grafts with relatively low donor site complications that will be replaced completely by living bone and that are capable of remodeling to fulfill the function need.10, 11
In this case, a chondroblastoma clavicle was treated with complete claviculectomy and reconstruction with non-vascularized fibular autograft with rigid fixation, To ensure long-term graft incorporation, we made decortication around the fibula and demineralized bone matrix was placed in the distal a proximal segment. Then, 13 months of follow-up is scheduled for removal of osteosynthesis material, finding full consolidation of sternoclavicular segment and the distal segment. Clinical results and stability were good, as was medium term patient satisfaction. There was no recurrence at 14 months of postoperative evolution. The ability of the implanted fibular autograft to induce bone formation depends on the early periosteal connections between the autograft and the ends of the resected bone, and it spreads distally along the graft, resulting in autograft to bone union. Osteogenic activity of the fibular autograft is confined to callus formation and trabecular formation within. We attributed the success of incorporation of the fibular, the rich blood supply of the recipient sites, and the surrounding well-vascularized soft tissues.11, 12
Although there were no clinical or radiological signs of recurrence or nonunion after 14 months of follow-up, a longer period is required to better define the long-term fate of this autologous reconstruction. A good functional outcome was apparent after a limited 14-month follow-up, and the patient was highly satisfied with the result.
4. Conclusions
Chondroblastoma is an uncommon benign bone tumor arising from a secondary ossification center. Although the lesions frequently are treated satisfactorily with intralesional procedures, such as curettage, they are sometimes very aggressive locally and require marginal or wide resection. This case report presents a 27-year-old female patient with diagnosis of clavicular chondroblastoma who was operated with resection of the tumor and reconstruction with non-vascularized fibula autograft which was taken from the contralateral leg and placed on the site of the clavicle. After 14 months of follow-up, we found no recurrence or metastasis. A good functional outcome was apparent after a limited 14-month follow-up, and the patient was highly satisfied with the result.
Conflicts of interest
The authors have none to declare.
References
- 1.Nasir-Ud-Din, Ahmed A., Pervez S., Ahmed R., Kayani N. Chondroblastoma: a clinico-pathological analysis. J Coll Phys Surg Pak. 2014;24:898–901. doi:12.2014/JCPSP.898901. [PubMed] [Google Scholar]
- 2.Ren K., Wu S., Shi X., Zhao J., Liu X. Primary clavicle tumors and tumorous lesions: a review of 206 cases in East Asia. Arch Orthop Trauma Surg. 2012;132:883–889. doi: 10.1007/s00402-012-1462-2. [DOI] [PubMed] [Google Scholar]
- 3.Li J., Wang Z., Fu J., Shi L., Pei G., Guo Z. Surgical treatment of clavicular malignancies. J Shoulder Elbow Surg. 2011;20:295–300. doi: 10.1016/j.jse.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 4.Kapoor S., Tiwari A., Kapoor S. Primary tumours and tumorous lesions of clavicle. Int Orthop. 2008;32:829–834. doi: 10.1007/s00264-007-0397-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ozkurt B1, Başarir K., Yildiz Y., Sağlik Y. Aggressive chondroblastoma of the acromion in a forty-one-year-old patient. J Shoulder Elbow Surg. 2008;17:e14–e17. doi: 10.1016/j.jse.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 6.Li Z., Ye Z., Zhang M. Functional and oncological outcomes after total claviculectomy for primary malignancy. Acta Orthop Belg. 2012;78:170–174. [PubMed] [Google Scholar]
- 7.Rubright J., Kelleher P., Beardsley C. Long-term clinical outcomes, motion, strength, and function after total claviculectomy. J Shoulder Elbow Surg. 2014;23:236–244. doi: 10.1016/j.jse.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 8.Guo Z., Wang Z., Wang Z., Zhang Y. Allograft of clavicle for reconstruction of bone defect after tumor resection. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2008;22:102–105. [PubMed] [Google Scholar]
- 9.Taraz-Jamshidi M.H., Gharadaghi M., Mazloumi S.M., Hallaj-Moghaddam M., Ebrahimzadeh M.H. Clinical outcome of en-block resection and reconstruction with nonvascularized fibular autograft for the treatment of giant cell tumor of distal radius. J Res Med Sci. 2014;19:117–121. [PMC free article] [PubMed] [Google Scholar]
- 10.Başarir K., Selek H., Yildiz Y., Sağlik Y. Nonvascularized fibular grafts in the reconstruction of bone defects in orthopedic oncology. Acta Orthop Traumatol Turc. 2005;39:300–306. [PubMed] [Google Scholar]
- 11.Krieg A.H.F., Hefti F. Reconstruction with non-vascularised fibular grafts after resection of bone tumours. J Bone Joint Surg. 2007;89:215–221. doi: 10.1302/0301-620X.89B2.17686. [DOI] [PubMed] [Google Scholar]
- 12.Finkemeier C.G. Bone grafting and bone graft substitutes. J Bone Joint Surg Am. 2002;84:454–464. doi: 10.2106/00004623-200203000-00020. [DOI] [PubMed] [Google Scholar]