Abstract
Androgens are essential for the development and maintenance of male reproductive tissues and sexual function and for overall health and well being. Testosterone, the predominant and most important androgen, not only affects the male reproductive system, but also influences the activity of many other organs. In the cardiovascular system, the actions of testosterone are still controversial, its effects ranging from protective to deleterious. While early studies showed that testosterone replacement therapy exerted beneficial effects on cardiovascular disease, some recent safety studies point to a positive association between endogenous and supraphysiological levels of androgens/testosterone and cardiovascular disease risk. Among the possible mechanisms involved in the actions of testosterone on the cardiovascular system, indirect actions (changes in the lipid profile, insulin sensitivity, and hemostatic mechanisms, modulation of the sympathetic nervous system and renin-angiotensin-aldosterone system), as well as direct actions (modulatory effects on proinflammatory enzymes, on the generation of reactive oxygen species, nitric oxide bioavailability, and on vasoconstrictor signaling pathways) have been reported. This mini-review focuses on evidence indicating that testosterone has prooxidative actions that may contribute to its deleterious actions in the cardiovascular system. The controversial effects of testosterone on ROS generation and oxidant status, both prooxidant and antioxidant, in the cardiovascular system and in cells and tissues of other systems are reviewed.
Keywords: cardiovascular, prooxidant, antioxidant
testosterone1 is the predominant and most important androgen, playing a major role in the development of male reproductive tissues (130, 135). “Androgen” is a broad term for any natural or synthetic compound that primarily influences the growth and development of the male reproductive system, including the activity of the accessory male sex organs and development of male secondary sex characteristics (21, 135). Androgens are also essential for health and well being, and their beneficial and stimulant effects have been known for a long time, since the seminal studies from Brown-Séquard in the nineteenth century2 (22, 135): “…in the seminal fluid, as secreted by the testicles, a substance or several substances exist which, entering the blood by resorption, have a most essential use in giving strength to the nervous system and to other parts….”
Other androgens include androstenedione, 5α-dihydrotestosterone (DHT), which is produced from testosterone by the enzyme 5α-reductase, dehydroepiandrosterone (DHEA), DHEA sulfate (DHEA-S), and synthetic androgens in their many steroid ester variations (e.g., testosterone cypionate, decanoate, undecanoate, enanthate, propionate, heptylate, caproate, phenylpropionate, isocaproate, and acetate) (21, 135).
Testosterone plays a major role in the development of male reproductive tissues and is found in mammals, reptiles, birds, and other vertebrates. In men, testosterone also promotes secondary sexual characteristics, such as increased muscle, bone mass, and the growth of body hair (128, 130, 135).
More than 95% of testosterone is produced by the testes and secreted by the Leydig cells (interstitial cells of the testes), after a series of enzymatic reactions using the cholesterol molecule. Small amounts of testosterone are also secreted by the zona reticularis of the adrenal glands (130, 135). Although adult human males produce about 10 times more testosterone than their female counterparts, females are very sensitive to the hormone. In women, the thecal cells of the ovaries synthesize testosterone, as does the placenta and the adrenal cortex (135, 141).
DHT is also very important in male development. DHT in embryonic development causes differentiation of the penis, scrotum, prostate, and their maturation during puberty and maintenance during adult life. Later in life, DHT contributes to male balding, prostate growth, and sebaceous gland activity. DHT is more biologically active than testosterone since it binds to the androgen receptor with a 15-fold higher affinity than testosterone, but circulates at a significantly lower level than testosterone. DHT may be considered a hormone with mainly paracrine/autocrine actions in the reproductive target tissues, not being directly secreted into the bloodstream. Thus, testosterone is the most common sex steroid in circulation of men (6, 21, 128, 135).
Although ∼7% of testosterone is reduced to DHT by the cytochrome P-450 enzyme, 5α-reductase (an enzyme highly expressed in male accessory sex organs and hair follicles) in men, small amounts (around 0.5%) are converted into estradiol by aromatase (CYP19A1, an enzyme expressed in the brain, liver, adipose, and cardiovascular tissues) (21, 135).
Through classic cytosolic androgen receptors (AR) or membrane receptors, testosterone induces genomic and nongenomic effects, respectively. The genomic or classical effects of testosterone depend on its binding to the AR, which acts as a transcription factor upon binding with the androgen response element, and modulates gene transcription and protein synthesis. Unlike testosterone-mediated genomic effects, nongenomic effects are rapidly produced, can be elicited even when androgens are prevented from entering the cell, do not require the association of AR to DNA, are insensitive to the inhibition of RNA and protein synthesis, and involve the activation of various signaling pathways, including calcium (Ca2+), nitric oxide (NO), PKA, PKC, and MAPK (62, 165). While a membrane receptor has been identified for testosterone, it is not clear that it mediates all of the rapid, nongenomic effects of androgens in the cardiovascular system and other nonreproductive tissues.
AR are widely distributed in several cells/tissues, including vascular smooth muscle cells and endothelial cells (70). Activation of AR may vary depending on whether naturally produced or commercially available hormones are being used, as well as whether metabolic products of androgens are being generated [e.g., testosterone is metabolized by 5α-reductase to the more potent AR ligand, DHT; alternatively, testosterone is metabolized by CYP19A1 to the primary form of estrogen, 17β-estradiol]. The effects of AR activation also may vary depending on whether androgen effects are tested in tissues or cells derived from male or female animals, or whether an underlying disease is present (49, 113, 188).
Testosterone supplements are mainly used in the treatment of hypogonadism, i.e., in males with very low levels or no endogenous testosterone production. Appropriate use for hypogonadism is known as hormone replacement therapy (testosterone replacement therapy) and aims to maintain serum testosterone levels in the normal range (14).
Because of its anabolic effects, testosterone has also been used in many other conditions, including infertility, lack of libido or erectile dysfunction, osteoporosis, and appetitie stimulation, as well as to stimulate penile enlargement and height growth, to promote bone marrow stimulation, and to reverse the effects of anemia (14, 141). High-dose testosterone is administered to female-to-male transsexuals, and very low doses are used to treat female androgen insufficiency-associated symptoms (reduced libido, diminished well being, and lowered mood or low energy state) in postmenopausal women (14, 141). Women, who experience surgical menopause, have adrenal insufficiency or pituitary insufficiency, and those who experience premature ovarian failure, also have reduced androgen production and may undergo androgen replacement therapy, either with DHEA or testosterone (141). Finally, testosterone and other anabolic steroids are used by athletes3 to enhance muscle development, strength, or endurance, i.e., to improve performance (12). Because most circulating testosterone is bound to sex hormone-binding globulin (SHBG), with a small fraction bound to albumin, SHBG-binding abnormalities can lead to either increased or decreased bioavailable testosterone levels, such as with aging.
Other common causes of pronounced elevations of testosterone include genetic conditions (e.g., congenital adrenal hyperplasia) and adrenal, testicular, and ovarian tumors. Excessive production of testosterone during childhood induces premature puberty in boys and masculinization in girls. Mild-to-moderate testosterone elevations are usually asymptomatic in adult males but can cause varying degrees of virilization, including hirsutism, acne, oligo-amenorrhea, or infertility in adult females (134, 141). The polycystic ovary syndrome (PCOS) is the most frequent endocrinopathy (hirsutism, acne, menstrual disturbances, insulin resistance, and, frequently, obesity and elevated blood pressure) and is characterized by hyperandrogenemia in women of reproductive age (192).
Is Testosterone a Good or Bad Guy for Cardiovascular Systems of Men and/or Women? The Differences May Be Related to Endogenous Levels Versus Supplementation
In addition to its effects on the male reproductive system or sexual function, testosterone influences the activity of other organs and systems. Studies on the effects of testosterone in the cardiovascular system were initially reported in the late 1930s into the early 1940s (48, 75, 80, 110, 198). Results from these initial studies to the present day show that the cardiovascular actions of testosterone (androgens) are still controversial, its effects ranging from protective to deleterious.
Numerous studies in the literature demonstrate increased cardiovascular risk and mortality with testosterone deficiency. In addition, testosterone therapy has been demonstrated to attenuate cardiovascular risk factors and also cardiovascular outcomes. Khaw et al. (100) conducted a prospective study with 11,606 men, aged 40–79 yr, and mean follow up of 7 yr. Testosterone baseline levels were inversely related to mortality due to all causes, cardiovascular diseases, and cancer. The same trend was also observed for coronary heart disease, although statistical significance was not achieved (100). Similarly, Hyde et al. (90) studied 4,249 men with 5.1 yr of follow-up on average. Lower free testosterone levels were associated with all-cause mortality [hazard ratio (HR) = 1.62; 95% confidence interval (CI) = 1.20–2.19, for 100 vs. 280 pmol/l] and also predicted cardiovascular disease mortality (HR = 1.71; 95% CI = 1.12–2.62, for 100 vs. 280 pmol/l) (90). Prospective data from the European Male Aging Study on 2,599 men, aged 40–79 yr, in eight European countries, demonstrated that late-onset hypogonadism increases the risk of all-cause mortality by five-fold. In addition, men with testosterone levels less than 8 nmol/l had a twofold higher risk of mortality compared with eugonadal men, and a threefold higher risk when presenting three symptoms of abnormal sexual function (irrespective of serum testosterone) (154). In Type 2 diabetic patients, low testosterone levels also predict an increase in all-cause mortality. In diabetic men, testosterone replacement therapy reduced mortality to 8.4% compared with 19.2% in the untreated group (P = 0.002) (133). Shores et al. (173) found similar results with testosterone treatment in men with low testosterone levels, in whom the mortality was decreased to 10.3% in testosterone-treated group compared with 20.7% in the untreated group. Furthermore, testosterone treatment decreased the risk of death (HR = 1.71; 95% CI = 1.12–2.62, for 100 vs. 280 pmol/l) when adjusted for age, body mass index, testosterone level, medical morbidity, diabetes, and coronary heart disease (173).
Maintaining normal testosterone levels in elderly men improves many parameters that are linked to increased cardiovascular disease risk. Men whose testosterone levels are slightly above average are less likely to have hypertension, to experience a myocardial infarction, to be obese, and less likely to rate their own health as fair or poor (17, 179). Accordingly, testosterone increases lean body mass, decreases visceral fat mass, total cholesterol, low-density lipoprotein, and triglyceride levels, and inhibits fatty streak formation (128).
Testosterone deficiency has also been linked to increased mortality due to all-cause and/or cardiovascular disease in different groups of patients with myocardial infarction (127), coronary heart disease (117), erectile dysfunction (40), diabetes (133, 150), renal disease (24), and patients referred to coronary angiography (109). In addition to the several studies that have demonstrated an association between low testosterone levels and coronary artery disease (46, 53, 87, 164), other evidence demonstrated that low testosterone is not only associated with coronary artery disease, but also with its severity (46, 111, 145, 164).
Svartberg et al. (182) demonstrated an inverse association between total testosterone levels and intima-media thickness after adjusting for smoking, physical activity, blood pressure, and lipid levels, in a population-based and cross-sectional study of 1,482 men. However, these changes were not independent of body mass index (182). Similarly, Vikan et al. (196), studying 2,290 men, found an inverse association between testosterone levels and total carotid plaque area, even after adjusting for age, systolic blood pressure, smoking, and use of lipid-lowering drugs (196). In addition to these studies, testosterone therapy increased time delay to angina onset evoked by a treadmill test in three randomized, placebo-controlled studies (54, 163, 199). These results corroborate other studies in the literature suggesting that testosterone causes brachial and coronary artery vasodilation (98, 136, 200). Finally, testosterone deficiency has been shown as an independent risk factor for worse outcomes in congestive heart failure patients. Toma et al. (186) conducted a meta-analysis of four randomized controlled trials. Testosterone therapy for 52 wk improved peak oxygen consumption, 6-min walk test, and incremental shuttle walk test. Importantly, no adverse cardiovascular events were observed (186).
Further support to protective effects of testosterone comes from a very recent and large observational cohort, in which testosterone therapy was used in 83,010 men with documented low testosterone levels. In this study, total testosterone levels were assessed after testosterone replacement therapy was introduced. The subjects were categorized into three groups: 1) men who received testosterone therapy and total testosterone levels were normalized; 2) men who received testosterone therapy and total testosterone levels were not normalized; and 3) men who did not receive testosterone therapy. The all-cause mortality, the risk of myocardial infarction and stroke were higher in untreated men and in testosterone-treated men without normalization of testosterone levels compared with testosterone-treated men whose hormone levels were normalized (171).
Taken together, this group of scientific studies and clinical evidence strongly suggests that testosterone at physiological levels promotes cardiovascular health and decreases morbidity and mortality in men under several conditions.
Although early studies showed that testosterone-replacement therapy did not increase the incidence of cardiovascular disease or cardiac events, such as myocardial infarction, stroke, or angina in men (59, 78, 79), recent safety studies point to a positive association between endogenous androgen and cardiovascular disease risk, as noted below. In addition, a group of studies failed to show any association between low testosterone levels with coronary artery disease (5, 10, 26, 97).
In women, testosterone may have different effects than in men. In a cross-sectional study evaluating 344 women, aged 65–98 years, high total testosterone levels were associated with a threefold greater risk of coronary heart disease. In addition, a significant association was found between high total and free testosterone levels and an adverse metabolic profile, i.e., insulin resistance and abdominal obesity (143).
Insulin resistance is considered the major player in the metabolic abnormalities and increased cardiovascular risk associated with PCOS. However, androgen excess, as well as a proinflammatory profile, further aggravates the cardiovascular and metabolic aberrations in women with PCOS (38, 153). Women with PCOS harbor a twofold increased risk for arterial disease (coronary heart and stroke), independent of their body mass index (43). In a study with 390 postmenopausal women followed for 5 yr, 79% of women that presented clinical features of PCOS experienced a 5-yr cardiovascular disease event-free survival vs. 89% of women without PCOS, independent of hypertension, diabetes status, or other cardiovascular disease risk factors (172).
In another study with 200 nondiabetic postmenopausal women, half of whom had cardiovascular disease and half served as matched controls, the free androgen index was significantly higher in women with cardiovascular disease compared with controls (139).
Studies in men who already have cardiovascular disease show different responses to testosterone supplementation. Concerns about the risk of heart attacks with testosterone therapy were highlighted in a clinical trial involving 209 men, with an average age of 74 and with a high prevalence of hypertension, diabetes, hyperlipidemia, and obesity. Patients were scheduled to receive either testosterone gel or placebo for 6 mo. The data and safety monitoring board recommended discontinuation of the trial due to a significantly higher rate of adverse cardiovascular events in the testosterone group compared with the placebo group (a total of 23 subjects in the testosterone group, compared with 5 in the placebo group, had adverse cardiovascular events) (13).
Very recent clinical trials further raised concerns about the safety of testosterone therapy. Another randomized clinical trial that aimed to assess the association between testosterone therapy and all-cause mortality, myocardial infarction, or stroke among male veterans with low testosterone levels (<300 ng/dl) who underwent coronary angiography in the Veterans Affairs (VA) system between 2005 and 2011, was stopped prematurely because of adverse cardiovascular events (195). The use of testosterone therapy in this retrospective national cohort study was significantly associated with increased risk of adverse outcomes, the rate of adverse events was 25.7% among the 1,223 patients that started testosterone therapy, compared with a rate of 19.9% among the 7,489 men who were not using testosterone (195).
Early this year, a cohort study on the risk of acute nonfatal myocardial infarction showed that older men, and younger men with preexisting diagnosed heart disease, may be twice as likely to suffer a nonfatal heart attack following initiation of testosterone therapy. The study involved 55,593 men who received an initial prescription for low-dose testosterone between 2006 and 2010 (60). The authors reported that the incidence rate of myocardial infarction in men, aged 65 yr and older, in the 90 days following an initial prescription of testosterone (postprescription interval) was higher than the incidence rate in the one year prior to the initial prescription (preprescription interval) with a post/pre rate of 2.19. The study also showed that the post/pre rate for testosterone prescription increased with age from 0.95 for men under age 55 years to 3.43 for men aged ≥75 years (60).
Increasing the debate on the beneficial/deleterious effects of testosterone, Morgentaler et al. (131) have raised a series of methodological problems and limitations in these studies and pointed that the conclusions drawn from these trials should be taken cautiously.
Finally, a number of lawsuits, alleging a significantly increased rate of stroke and heart attack in elderly men using testosterone supplements, are currently under way against testosterone manufacturers, and the Food and Drug Administration added a warning regarding deep vein thrombosis and pulmonary embolism among testosterone users (61a, 61b). The number of lawsuits is rapidly increasing, since it has been alleged that the manufacturers of testosterone supplements and prescriptions failed to adequately investigate the potential side effects of testosterone therapy, yet aggressively marketed the products in a way that resulted in the widespread overuse of testosterone supplements among men who may have had no real medical need for testosterone treatments but may have had underlying cardiovascular diseases.
Nonmedical testosterone use (or testosterone abuse) has been shown to increase arterial blood pressure and to induce left ventricular hypertrophy, myocardial infarction due to coronary vasospasm, or thrombosis (4, 56, 61, 69, 83, 125).
Possible Mechanisms Responsible for Deleterious Effects of Testosterone Supplements
Among the possible mechanisms involved in the deleterious actions of supraphysiological doses of testosterone, both direct actions in the vasculature and indirect actions have been reported. Unfavorable changes in the lipid profile (88), procoagulatory effects, activation of the sympathetic nervous system, and renin-angiotensin-aldosterone system, and insulin resistance are some of the indirect actions of testosterone that can affect the vasculature (25, 52, 66, 76, 105, 119). Among the direct effects of testosterone, stimulation of proinflammatory enzymes in the vasculature [e.g., thromboxane synthase, as well as cyclooxygenase-1 (COX-1) and COX-2 in rat thoracic aorta and mesenteric arteries (31, 177)], reactive oxygen species (ROS) generation in vascular smooth muscle cells (33), which may decrease NO bioavailability and lead to increased blood pressure and renal dysfunction (36, 95, 155, 159), activation of vasoconstrictor signaling pathways (PKC, MAPKs), and increased vasoconstriction have been reported (34, 35, 99). It is worth mentioning that the beneficial effects of testosterone have been linked to modulatory effects on some of the same pathways mentioned above, adding to the controversial nature of testosterone supplementation.
In the next section, we will focus on evidence indicating that testosterone has prooxidative actions that may contribute to the deleterious actions of testosterone in the cardiovascular system.
Other Mechanisms: Testosterone and ROS Generation/Oxidative Status
Since comprehensive and excellent recent reviews have highlighted the effects of ROS in the cardiovascular system, as well as the implications of ROS in cardiovascular diseases (142, 146, 170, 189, 190), only key points on ROS generation will be included in this mini-review.
ROS play a major role in various biological responses, such as host defense, activation of transcription factor, modulation of kinase and ion transport systems activity (47, 170). ROS and reactive nitrogen species (RNS) are products of cellular metabolism and are well recognized for their dual roles as both deleterious and beneficial species. Although ROS, such as superoxide anion (O2·−), hydrogen peroxide (H2O2), and the hydroxyl radical, are generated as the natural byproducts of normal oxygen metabolism, they can create oxidative damage via interaction with other biomolecules (47, 170). In the situation of uncontrolled ROS generation or impaired ROS inactivation, termed oxidative stress, the excessive availability of oxidants activates signaling pathways that have been implicated in the development of organ damage in cardiovascular and metabolic diseases, including hypertension, atherosclerosis, heart failure, diabetes, and stroke (189, 190). Increased ROS production has been directly linked to vascular remodeling, endothelial dysfunction, altered vasoconstrictor responses, inflammation and modifications of the extracellular matrix, all important features of cardiovascular disease pathophysiology (142, 189).
ROS can be produced from complexes in the cell membrane [NAD(P)H-oxidase, or Nox], cellular organelles (peroxisomes and mitochondria), and in the cytoplasm (by xanthine oxidase). Furthermore, low levels of tetrahydrobiopterin and l-arginine, the rate-limiting cofactor and substrate for endothelial nitric oxide synthase (eNOS), respectively, can cause the uncoupling of eNOS, resulting in decreased NO production and increased ROS generation (47, 189).
NAD(P)H oxidases (Nox) are the main source of ROS in the vasculature. They function as electron transport chains across membranes, using NAD(P)H as the electron donor to reduce molecular oxygen to superoxide, and participate not only in normal cell function, but also trigger the development of injury in pathological conditions (170, 189). The Nox family is composed of catalytic subunits (Nox1-5, Duox1, and Duox2), and the docking subunit p22phox, all present in the cell membrane. The regulatory subunits Nox organizer 1 (or Noxo1), Nox activator 1 (or Noxa1), p67phox, p47phox, and p40phox, are located in the cytosol. Activation of Rac1/2 regulates the translocation and assembly of the NAD(P)H oxidase subunits in the plasma membrane, and is a key event in Nox activation (19, 51, 142, 146).
Antioxidants, on the other hand, act by scavenging or chain-breaking ROS and RNS. Antioxidants are molecules that accept or donate electrons and, as a consequence, can convert ROS and RNS into less reactive products, thus neutralizing them. Antioxidants can be enzymes, such as superoxide dismutase, glutathione peroxidase, catalase, glutathione reductase, and glutathione transferase, as well as nonenzymatic endogenous molecules, such as α-tocopherol, β-carotene, glutathione, ascorbic acid, adenosine, lipoic acid, coenzyme Q, and lactoferrin. Synthetic molecules, such as thiols, ebselen (selenium-based peroxide scavenger), idebenone (coenzyme Q-analog), mitoQ (mitochondrial-targeted ubiquinone), and α-tocopheryl-succinate nanoparticles, as well as plant-derived molecules, such as polyphenol compounds (including quercitin, myricetin, catechins, anthocyanins), proanthocyanidin, and lycopene, are also antioxidants (68, 149). Considering that redox homeostasis of the cell is ensured by a delicate balance between ROS production and its antioxidant capacity, it is also important to consider the effects of androgens upon cell antioxidant systems. To make it easier for the reader, the effects of testosterone on the main components that influence ROS generation and degradation (or that control the cell redox status) will be discussed.
NAD(P)H oxidase.
Our group reported that testosterone induces ROS generation in cultured VSMC, with greater production of ROS in cells from hypertensive compared with normotensive animals (33). Testosterone's effects are not due to conversion of testosterone to 17β-estradiol, since the aromatase inhibitor, anastrazole, has no effect on ROS formation. While testosterone effects on steady-state mRNA levels of NAD(P)H oxidase subunits Nox1 and p22phox are not evident, testosterone upregulates the expression of Nox4 only in vascular smooth muscle cells (VSMC) from normotensive but not from hypertensive animals (33). Although vascular NAD(P)H oxidases have been generally implicated in excessive and deleterious ROS formation, Nox4 (unlike Nox1) has been shown to exhibit protective effects. Nox4 maintains VSMC in a differentiated state, counteracting proliferation and vascular hypertrophy (39); Nox4-derived H2O2 mediates vasodilation through hyperpolarization (156), and mice overexpressing Nox4 exhibit increased vasodilator function and lower blood pressure (20). Therefore, the lack of stimulatory effects of testosterone on Nox4 expression in cells from hypertensive rats might indirectly promote VSMC growth under hypertensive, but not normotensive, conditions.
The nongenomic stimulatory effects of testosterone on ROS generation in VSMC from hypertensive animals are insensitive to the AR antagonist, flutamide, and lead to phosphorylation of the nonreceptor tyrosine kinase, c-Src (33). Of importance, c-Src mediates vascular contraction and hypertrophy and is upregulated in experimental polygenic hypertension (23, 191). It is possible that testosterone actions on VSMC may further aggravate vascular dysfunction associated with cardiovascular diseases (e.g., hypertension). Further support to this idea is the fact that testosterone abolishes the beneficial effect of estrogen treatment in the aorta of ovariectomized SHR by increasing ROS production through p47phox phosphorylation (41). On the other hand, a genetic vascular predisposition may lead to development or aggravation of cellular dysfunction produced by testosterone, with cells on a specific background responding to a greater degree to testosterone.
Testosterone metabolites may play a role in ROS generation in the cardiovascular system. The cytochrome P-4501B1 (CYP1B1) also metabolizes testosterone into 6β-hydroxytestosterone, 2α-, 15α- and 16α-hydroxytestosterone (178). 6β-hydroxytestosterone contributes to ANG II-induced hypertension and its associated cardiac damage. All changes are accompanied by increased NAD(P)H oxidase activity and ROS generation (147). Similarly, rats with DHT-induced hypertension display increased expression of p47phox, gp91phox, and, consequently, increased superoxide generation in renal interlobar arteries (175). In addition, female rats treated with DHT (to mimic/imitate PCOS condition) display increased mRNA expression of gp91phox, p22phox, p47phox, and NOX4 in the renal cortex (202). Increased circulating androgens, such as dehydroepiandrosterone (DHEA), in healthy, ovulating women, as occurs in women with PCOS, also increases leukocyte ROS generation, p47(phox) gene expression, and plasma thiobarbituric acid-reactive substances (TBARS) (72). These studies highlight the possible effects of testosterone and its metabolites inducing NAD(P)H oxidase-dependent ROS production in the cardiovascular system. However, it is not clear whether these effects are directly produced by testosterone or indirectly through testosterone-induced cytokine release, eicosanoid production, or upregulation of vasoactive substances. Therefore, more studies are warranted to investigate these possibilities.
Considering that some actions of testosterone do not rely on AR activation, i.e., AR-independent effects, it is possible that an as yet unidentified receptor may be involved. As suggested by Barton et al. (11), the orphan G protein-coupled receptor GPRC6A, which has been shown to mediate nongenomic responses to testosterone, might be a possible candidate to mediate the rapid, AR-independent effects of testosterone on ROS generation in VSMC (11). In addition, testosterone induces Duox1 activation through GPRC6A in keratinocytes that leads to H2O2 generation (104).
Mitochondrial ROS and androgens.
The mitochondrial respiratory chain is also an important source of ROS, mainly superoxide, that is quickly converted into H2O2. It is estimated that 1–4% of oxygen is reduced to superoxide, especially by complexes I and III of the mitochondrial respiratory chain (18, 30, 45, 203). Mitochondrial dysfunction contributes to inflammation, cell senescence, and apoptosis, and it plays an important role in vascular disease (203). Our group recently reported that testosterone, in addition to its effects on NAD(P)H activity, also induces mitochondria-associated ROS generation and apoptosis in VSMC via activation of AR (115).
Apoptosis, or programmed cell death, occurs in multicellular organisms, and includes a series of biochemical events (blebbing, cell shrinkage, nuclear fragmentation, chromatin condensation, and chromosomal DNA fragmentation) that lead to characteristic cell changes and death. Apoptosis deregulation is considered a pathogenetic process in a variety of human diseases and is an important mechanism underlying the changes observed in hypertension, diabetes, and arteriosclerosis (73). As ROS are important activators of the apoptotic cascade, it is reasonable to assume that testosterone-induced ROS may modulate the apoptosis-associated damage in these diseases.
Two pathways are responsible for initiating apoptosis, one mediated by cell death receptors located on the membrane surface, termed the extrinsic pathway, and another mediated by mitochondria, termed the intrinsic pathway. Both pathways are modulated by activation of caspases, which trigger the cellular alterations characteristic of apoptosis (169). In VSMC, testosterone-induced apoptosis is associated with a decrease in the ratio of Bax/Bcl-2 (proapoptotic and antiapoptotic proteins) in total cell homogenates, as well as in the mitochondrial fraction. Because there is no evident cytochrome c release from mitochondria to cytosol, and procaspase 8 is activated and gene expression of two cell death receptor ligands is increased, it seems that testosterone activates the extrinsic pathway of apoptosis in VSMC, in association with AR activation and mitochondrial-generated ROS (115). In prostate cancer cell lines, in addition to directly inducing ROS generation (166), testosterone enhances H2O2-induced apoptosis (91), indicating that under oxidative stress conditions, androgen signaling may further enhance apoptosis and DNA damage response.
Although studies on the role of testosterone and/or androgens upon mitochondrial ROS generation in the cardiovascular system are scarce, there are a few studies in the literature showing this possibility in other cells. DHT induces mitochondrial ROS production through p66Shc protein in AR-positive prostate cancer cells (193). Similarly, methyltrienolone (synthetic AR agonist) induces mitochondrial ROS generation in prostate cancer cells through mitochondrial fatty acid oxidation (112). In addition, testosterone increases mitochondrial oxygen consumption, membrane potential, and ROS production in leukocytes from female-to-male transsexuals (194). Testosterone, DHEA and 3α-androstanediol increase mitochondrial ROS levels, oxygen consumption rate and ATP levels in neuroblastoma cells. Moreover, testosterone increases mitochondrial respiratory capacity (74). Conversely, stanozolol (an anabolic androgenic steroid) decreases mitochondrial ROS and oxidative stress induced by acute exercise in rat skeletal muscle (167). Considering the anabolic effects of testosterone and its related androgens and also their effects upon mitochondrial metabolism, it is likely that androgens can modulate mitochondrial ROS generation. However, there are very few studies that have tested this hypothesis, whereas all of the aforementioned studies point to a possible modulation of mitochondrial ROS by androgens. However, caution must be taken when interpreting these results, since they were performed under pathological, supraphysiological doses of androgens. Therefore, whether these effects of androgens are produced physiologically, and if so, what relevance do they have for the cardiovascular system remains unknown.
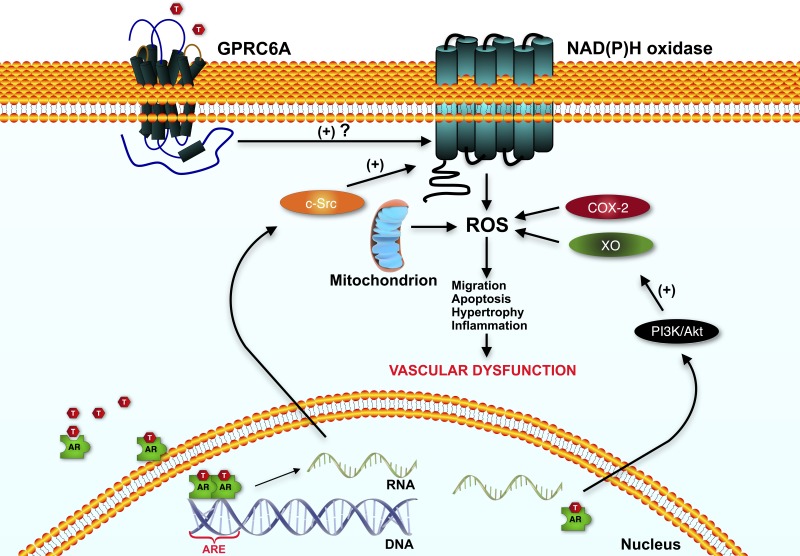
Similarly, how testosterone-induced ROS preferentially induces vasodilation and VSMC migration or interferes with mitochondrial function is not known, but may be related to the theory that the location of ROS generation is of major importance. In addition, it is not clear why testosterone activates different sources of ROS-generating enzymes/organelles in these studies. Figure 1 summarizes signaling pathways implicated in testosterone's effects on ROS generation and cellular oxidant status in the cardiovascular system.
Fig. 1.
Testosterone's effects on reactive oxygen species (ROS) generation and cellular oxidant status in the vascular system. Testosterone has been shown to increase ROS in smooth muscle cells via different cellular sources, such as activation of NAD(P)H oxidase, mitochondria, cyclooxygenase 2 (COX-2), and xanthine oxidase. The genomic action of testosterone induces c-Src and PI3K/Akt pathways, which in turn, activates NAD(P)H oxidase and xanthine oxidase, respectively. Testosterone may also increase ROS, via its nongenomic action, through GPRC6A receptor. Increased ROS production may lead to migration, apoptosis, hypertrophy, and inflammation, causing vascular dysfunction. AR, androgen receptor; T, testosterone; ARE, androgen responsive element; COX-2, cyclooxygenase-2; XO, xanthine oxidase; c-Src, Proto-oncogene tyrosine kinase Src; PI3K/Akt, phosphoinositide-3-kinase/protein kinase B; GPRC6A, G protein-coupled receptor, family C, group 6, member A.
Xanthine oxidase.
Testosterone-induced ROS generation is also coupled to a commonly described effect of testosterone in the vasculature: vasodilation. Testosterone stimulates the generation of superoxide and NO, to produce peroxynitrite, which has direct vasodilator effects. Furthermore, the vasodilator influence of testosterone is inhibited by scavenging peroxynitrite, indicating the latter may play an important role in testosterone vascular effects. Xanthine oxidase was identified as the likely source of testosterone-stimulated superoxide production via activation of AR and the PI3 kinase-Akt signaling cascade (152). Similarly to VSMC, in the renal macula densa-like cell line MMDD1, testosterone induces superoxide generation via xanthine oxidase-, NAD(P)H oxidase-, and AR-dependent pathways. This effect is associated with an increase in tubuloglomerular feedback, which results in lower tubular perfusion and altered control of renal microcirculation, potentially contributing to the higher prevalence of hypertension and renal injury in males (65). On the other hand, in an ischemia/reperfusion model, testosterone exhibits a protective effect in the spinal cord by decreasing xanthine oxidase activity (77), and in kidneys of aged rats (24 mo), testosterone treatment decreases xanthine oxidase activity (201).
Cyclooxygenase.
There are three isoforms of cyclooxygenase, namely COX1, COX2, and COX3. In most tissues, COX1 is constitutively expressed. COX2, initially thought to be expressed only during an inflammatory process, has been shown to be constitutively expressed in cardiovascular, renal, and central nervous systems. COX-3 is a splice variant of COX-1 with all catalytic features of COX-1 and COX-2. These enzymes oxidize arachidonic acid into prostaglandins, which play a crucial role in vascular tone control (58, 185). In recent years, studies have shown that ROS activate COX, and that COX and its products induce ROS generation. This reciprocal association was mainly identified in hypertensive conditions (123) and in endotoxic shock (197).
Androgens modulate COX1 and COX2 expression, and some of the effects of androgens rely on COX activation/inhibition. Castration dramatically decreases COX1 and COX2 mRNA expression in rat epididymis (31). Testosterone-induced hyperplasia is decreased by treatment with flavocoxid [a dual inhibitor of COX and 5-lipoxygenase (5-LOX)] (3). Testosterone-induced relaxation is decreased in diabetic animals with COX inhibition (122). The relaxation effect of testosterone on renal arteries is also mediated by COX enzymes, and possibly, via modulation of thromboxane A2 production in smooth muscle cells and prostacyclin in endothelial cells (121). Despite the evidence showing a positive modulation of COX2 by androgens, Martorell et al. (124) found increased COX2 expression in aorta of orchidectomized rats.
Testosterone metabolites also modulate COX enzymes. DHT treatment in rats or ex vivo incubation of pial arteries with DHT upregulates COX2 expression and increases constriction of middle cerebral arteries (71). In human coronary smooth muscle cells, DHT also increases COX2 expression. Interestingly, DHT attenuates the increases in COX2 expression in coronary arteries produced by either LPS or IL-1β, suggesting a differential role for DHT under inflammatory conditions (137). The same protective effect of DHT was demonstrated in cerebral arteries under hypoxic conditions (207).
Considering the number of reports demonstrating the effects of androgens on COX expression and that COX is a source of ROS, the lack of studies evaluating COX-derived ROS by androgens in the cardiovascular system is surprising, especially taking into account the importance of ROS for vascular tone control. Our group recently demonstrated that COX2-dependent ROS production is obligatory for testosterone-induced leukocyte migration (32), which may contribute to inflammation and vascular dysfunction. However, more studies on the role of androgens modulating COX-derived ROS and its implications for the cardiovascular system are warranted.
Other sources of ROS.
Uncoupled eNOS and 5-LOX are also potential sources of ROS in the vasculature. eNOS uncoupling decreases NO production and increases ROS generation (47, 189). ANG II-induced ROS production in smooth muscle cells is partly dependent on 5-LOX and, its product, leukotriene B4 (116). Although uncoupled eNOS and 5-LOX have been implicated in ROS generation and several aspects of cardiovascular disease, the effects of testosterone on ROS production by these enzymes still need to be determined.
Antioxidant status.
The main function of antioxidants is to prevent and/or delay protein and lipid oxidation, DNA mutation, and, ultimately, cellular oxidative damage. However, when ROS production is maintained at high levels, the system's defenses against ROS can be overwhelmed, which may lead to disease conditions. Fortunately, there are many endogenous factors that can serve as modulators of the production and actions of ROS. The enzymatic antioxidant system is considered “the first line of defense” against ROS production, and is composed of superoxide dismutase (SOD), which depletes superoxide, catalase (CAT), which decomposes H2O2, and the glutathione peroxidase/glutathione reductase system. Thiols and low-molecular-weight antioxidants such as tocopherols, ascorbate, retinols, urate, and reduced glutathione represent “the second line of defense” (149).
Besides increasing ROS, a single supraphysiological dose of testosterone decreases SOD, CAT, and glutathione peroxidase expression in human endothelial cells (176). Moreover, testosterone decreases the total antioxidant capacity in urine (176). On the other hand, Zhang et al. (206) demonstrated that castration decreased SOD and glutathione peroxidase activity and increased malondialdehyde (MDA) levels, an indicator of lipid peroxidation, in murine cardiomyocytes. Testosterone replacement to physiological levels restored all changes by AR-independent mechanisms (206). In addition, the same research group demonstrated that cardiomyocytes from testicular feminized mice displayed decreased SOD and glutathione peroxidase activities combined with increased MDA levels. Testosterone replacement normalized these changes (205). Similarly, Klapcinska and colleagues showed that castration decreases SOD, CAT, glutathione peroxidase, and glutathione reductase activity in rat left ventricals. In contrast to the Zhang studies, castration did not increase lipid peroxidation, and testosterone replacement did not restore antioxidant enzyme activities in this study (103). SOD activity was decreased in cardiac muscle of castrated rats, but CAT and glutathione were not changed (9). In humans, hypogonadism is associated with decreased plasma antioxidant capacity. After testosterone replacement and eugonadal reestablishment, the antioxidant capacity returns to normal values, suggesting that normal levels of testosterone are essential to maintain the antioxidant status (118).
Other androgens are also capable of modulating the antioxidant capacity and, therefore, the redox balance in the cardiovascular system. DHEA acute treatment (6 h) increases SOD activity in rat heart homogenates. Conversely, DHEA treatment for 24 h decreases SOD and increases glutathione-S-transferase activities (93). Nandrolone decanoate is frequently used by bodybuilders and recreational athletes to increase performance. Recently, Frankenfeld et al. (64) demonstrated that nandrolone decanoate treatment increases cardiac NOX2 mRNA levels and H2O2 generation. In addition, these changes were accompanied by decreased renal CAT activity, total reduced thiol residues, and carnonyl content (64). Treatment with nandrolone decanoate also prevents the increase in cardiac expression of SOD, glutathione peroxidase, and glutathione reductase induced by exercise in rats. Moreover, nandrolone decanoate treatment blocks around 50% of the exercise-induced cardiac tolerance to ischemic events (29). Similarly, turinabol treatment increases TBARS levels by 46% with slight increases in CAT activity in rabbit plasma. Methandienone treatment reduces total antioxidant capacity by 46% (67). Interestingly, only high doses of the anabolic androgenic steroids were able to provoke these effects.
Table 1 summarizes the effects of testosterone and other androgens (or the lack of them) on ROS generation/oxidative status in various cell types. In addition to those mentioned above, and as shown in Table 1, testosterone-induced ROS generation has been reported in renal cells (37, 65, 144), in human prostate cancer cells (112, 148, 151, 181), and leukocytes, among others. However, in myocardial (50, 103, 206) and neuronal cells (2, 55, 85), testosterone also has antioxidant effects. It reinforces the notion that the effects of testosterone on ROS generation are controversial, mainly because androgens have prooxidant, as well as antioxidant effects, depending on the tissue/cell being studied (and sometimes even when the same cell type is being studied).
Table 1.
Testosterone effects on ROS generation and cellular oxidant status
| Effect on Redox Status |
||||
|---|---|---|---|---|
| Cell/Tissue/Animal | Prooxidant | Antiooxidant | Associated Effects | Ref. |
| PCOS/menopause | ↑ | − | ↑ lipid peroxidation and ROS generation | (160) (84) |
| (Experimental models and patients) | ||||
| − | ↓ | ↓ Total antioxidant capacity | (63) | |
| Cardiovascular system | ||||
| Heart/cardiac cells from experimental animal models [e.g., orchidectomized and testosterone-treated animals, Testicular feminized mice] | ↑ | − | ↑ lipid peroxidation, MDA levels | (176) |
| − | ↓ | (101) | ||
| ↓ SOD, GPx, catalase, GR enzyme activities | (161) | |||
| (50) | ||||
| ↓ | − | ↓ MDA levels | (206) | |
| − | ↑ | ↑ activities of SOD and GSH-Px enzymes | (103) (9) | |
| Arteries from experimental animal models [andropause- follitropin receptor knockout male mice; androgen receptor knockout mice] | ↑ | − | ↑ superoxide anion production, lipid peroxidation, gene expression of NADPH oxidase components, phosphorylation of JNK and Smad2/3 | (158) (94) (92) |
| ↓ NO availability, eNOS expression and phosphorylation, Akt phosphorylation | ||||
| Blood/immune system cells | ||||
| Leukocytes from individuals that received testosterone/androgens | ↑ | − | ↑ ROS production, p47(phox), plasma TBARS. | (194) |
| − | ↓ | ↓ GSH levels, (GSH)/(GSSG) ratio | (72) | |
| (44) | ||||
| Immune cells from experimental animals | (28) | |||
| ↓ | − | ↓ superoxide anion production, lipid peroxidation (TBARS) | (120) | |
| (15) | ||||
| − | ↑ | ↑ GSH-R activity, CoQ10 levels | (82) | |
| (118) | ||||
| − | − | no changes in oxidant/antioxidant status | (8) | |
| Cell lines [HL-60 (Human promyelocytic leukemia cells), THP-1 cells (human monocytic cell line)] | ↓ | − | ↓ NOx production, iNOS protein, superoxide anion, NADPH oxidase activity, p67phox and p47phox expression | (16) (96) |
| Prostatic cells | (89) (112) (151) (107) (187) (174) (7) (27) (181) (162) | |||
| [TM3 Leydig cell line, 22rv1 cells (human prostate carcinoma cell line), AR-negative PC3 human prostatic cancer cell line, LNCaP cells (androgen-sensitive human prostate adenocarcinoma cells)]. | ↑ | − | ↑ ROS generation, lipid peroxide contents, mitochondrial fatty acid oxidation | |
| − | ↓ | ↓ activity of catalase, SOD, GSH-Px, GSH-ST, and GSH-R; levels of reduced GSH and vitamin C. | ||
| Prostate | ↓ | − | ↓ ROS-generating NAD(P)H oxidases expression [Nox1, gp91(phox), Nox4] | (148) (183) |
| (from testosterone-treated experimental animals) | ||||
| − | ↑ | ↑ activity of catalase, SODs, GSH-R, SOD2, GSH-Px1, thioredoxin, and peroxiredoxin 5 | ||
| − | − | ↓ ROS-detoxifying enzymes (SOD2, GSH-Px1, thioredoxin, and peroxiredoxin 5) | (184) | |
| Neuronal cells | ↓ | − | ↑ aconitase activity (a ROS-sensitive mitochondrial enzyme) | (157) |
| [PC-12 cells (cell line derived from a pheochromocytoma of the rat adrenal medulla) and brain cells from experimental animals (cerebellar granule cells, astrocytes, N27 dopaminergic cells. | − | ↑ | ↑ expression of Nrf2, HO-1 and NQO1 | (2) (1) (55) (108) (85) (204) (138) (126) (42) |
| ↑ activities of catalase, SOD and GSH-Px enzymes | ||||
| ↓ MDA levels | ||||
| Kidneys and renal cells | ↑ | − | ↑ renal lipid peroxidation, H2O2 levels, urinary excretion of H2O2, superoxide anion formation | (101) (159) (180) (37) (102) (144) |
| (from experimental animal models) | ||||
| − | ↓ | ↓ expression and activity of MnSOD, catalase, SOD1, SOD2. | ||
| Skeletal muscle | ↑ | − | ↑ TBARs, lipid peroxidation. | (140) |
| (e.g.,gastrocnemius soleus and extensor digitorum longus muscles) | ||||
| ↓ | ↑ | ↑ MnSOD | (168) (106) | |
| Pancreatic cells/diabetes-related conditions | ↓ | − | ↓ nitrotyrosine levels, ER stress markers | (81) |
| INS-1 cells (rat insulinoma cell line) and animal experimental models | ↑ | ↑ | ↑ MDA levels | (129) |
| ↑ activities of GSH and catalase | (114) | |||
| Bladder/urinary-genital tract | ↓ | − | ↓ MDA levels | (132) |
| Cavernous tissue from experimental animal models | − | ↑ | ↑ GPx, cGMP | |
AR, androgen receptor; CoQ10, coenzymeQ10; SOD1 or Cu/ZnSOD, copper-zinc superoxide dismutase; eNOS, endothelial NO synthase; SOD3 or ecSOD, extracellular superoxide dismutase; ER, endoplasmic reticulum; G6PD, glucose-6-phosphate dehydrogenase; GPx, glutathione peroxidase; GR, glutathione reductase; GSH, glutathione; GSH-Px, glutathione peroxidase; GSH-R, glutathione reductase; GSH-ST, glutathione S-transferase; HO-1, heme oxygenase-1; H2O2,hydrogen peroxide; iNOS, inducible nitric oxide synthase; INS-1, rat insulinoma cell line; LNCap, androgen-sensitive human prostate adenocarcinoma cells; MDA, malondialdehyde; NO, nitric oxide; NOx, nitrogen oxides; Nrf2, nuclear factor erythroid 2-related factor 2; SOD2 or MnSOD, manganese superoxide dismutase; NQO1, NAD(P)H:quinone oxidoreductase-1; PCOS, polycystic ovary syndrome; ROS, reactive oxygen species; TBARS, thiobarbituric acid reactive substances.
Summary
The role of testosterone in mediating or protecting against ROS and antioxidant capacity in the cardiovascular system is far from being clear, with testosterone presenting prooxidant as well as antioxidant effects. There are various possible contributing factors to these discrepant effects of testosterone in the cardiovascular system and in the other tissues and organs: 1) acute vs. chronic differential effects are possibly due to activation of distinct sets of signaling pathways, as reported with other hormones and neurotransmitters; 2) the initial metabolic-energetic-redox status of the cell may exacerbate cardiovascular risk; 3) global (or local) increases in testosterone may produce differential effects based on the specific cell types that are stimulated; 4) the concentrations of testosterone (physiological, supraphysiological) may produce different effects; 5) the steroid ester used (testosterone cypionate, decanoate, undecanoate, enanthate, propionate, heptylate, caproate, phenylpropionate, isocaproate, acetate) changes the compound solubility in water and slows the release of the parent steroid, i.e., changes absorption time. Different esters are also susceptible to the presence of native and selective esterases in the many complex biological/cellular environments and can mask specific functional groups. These processes may confer different responses to different esters; 6) the “sex” of the individual or cell/tissue may determine differential effects of testosterone; and not least, 7) different animal species (mice, rats, humans, rabbits, birds) and the age, duration, and characteristics of the diseases/conditions upon which testosterone effects are determined are not fully understood. The complexity of testosterone effects is evident, and further basic and clinical studies are required for a better understanding of the mechanisms by which testosterone gains its biological activity independent of reproduction, which may be detrimental and/or beneficial to the cardiovascular system.
GRANTS
This work was supported by grants from Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP 2004/13796-9, 2013/08216-2), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Brazil (to R. C. Tostes, F. S. Carneiro, and M. H. C. Carvalho), and National Institutes of Health, National Heart, Lung, and Blood Institute (R01HL-66072 and P01HL-05971 to J. F. Reckelhoff).
DISCLOSURES
The content of this mini-review was presented at the Novel Actions of Sex Steroids Symposium, 1st Pan American Congress of Physiological Sciences, Iguassu Falls, PR, Brazil, August 2–6, 2014. No conflicts of interest, financial or otherwise, are declared by the authors.
AUTHOR CONTRIBUTIONS
Author contributions: R.C.T. and F.S.C. interpreted results of experiments; R.C.T. and F.S.C. prepared figures; R.C.T. drafted manuscript; R.C.T., M.H.C.C., and J.F.R. approved final version of manuscript; F.S.C., M.H.C.C., and J.F.R. edited and revised manuscript.
Footnotes
Testosterone, from “testo” = testes + “ster” = sterol + “one” = ketone, was isolated by Karoly David, Elizabeth Dingemanse, Janos Freud, and Ernst Laqueur from tons of bull testes [quoted from Oettel, 2004 135. Oettel M. The endocrine pharmacology of testosterone therapy in men. Naturwissenschaften 91: 66-76, 2004.].
Charles-Édouard Brown-Séquard. The effects produced on man by subcutaneous injections of a liquid obtained from the testicles of animals. Lancet July 20, 1889, p. 105-107. Check also http://en.wikipedia.org/wiki/Charles-Édouard_Brown-Séquard.
Testosterone use is considered to be a form of doping in most sports and in many countries. Along with other anabolic androgenic steroids, testosterone is a controlled substance, and its nonmedical use is considered drug abuse.
REFERENCES
- 1.Ahlbom E, Grandison L, Bonfoco E, Zhivotovsky B, Ceccatelli S. Androgen treatment of neonatal rats decreases susceptibility of cerebellar granule neurons to oxidative stress in vitro. Eur J Neurosci 11: 1285–1291, 1999. [DOI] [PubMed] [Google Scholar]
- 2.Ahlbom E, Prins GS, Ceccatelli S. Testosterone protects cerebellar granule cells from oxidative stress-induced cell death through a receptor mediated mechanism. Brain Res 892: 255–262, 2001. [DOI] [PubMed] [Google Scholar]
- 3.Altavilla D, Minutoli L, Polito F, Irrera N, Arena S, Magno C, Rinaldi M, Burnett BP, Squadrito F, Bitto A. Effects of flavocoxid, a dual inhibitor of COX and 5-lipoxygenase enzymes, on benign prostatic hyperplasia. Br J Pharmacol 167: 95–108, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 4.Angell P, Chester N, Green D, Somauroo J, Whyte G, George K. Anabolic steroids and cardiovascular risk. Sports Med 42: 119–134, 2012. [DOI] [PubMed] [Google Scholar]
- 5.Arnlov J, Pencina MJ, Amin S, Nam BH, Benjamin EJ, Murabito JM, Wang TJ, Knapp PE, D'Agostino RB, Bhasin S, Vasan RS. Endogenous sex hormones and cardiovascular disease incidence in men. Ann Intern Med 145: 176–184, 2006. [DOI] [PubMed] [Google Scholar]
- 6.Askew EB, Gampe RT Jr, Stanley TB, Faggart JL, Wilson EM. Modulation of androgen receptor activation function 2 by testosterone and dihydrotestosterone. J Biol Chem 282: 25,801–25,816, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aydilek N, Aksakal M, Karakilcik AZ. Effects of testosterone and vitamin E on the antioxidant system in rabbit testis. Andrologia 36: 277–281, 2004. [DOI] [PubMed] [Google Scholar]
- 8.Azevedo RB, Lacava ZG, Miyasaka CK, Chaves SB, Curi R. Regulation of antioxidant enzyme activities in male and female rat macrophages by sex steroids. Braz J Med Biol Res 34: 683–687, 2001. [DOI] [PubMed] [Google Scholar]
- 9.Barp J, Araujo AS, Fernandes TR, Rigatto KV, Llesuy S, Bello-Klein A, Singal P. Myocardial antioxidant and oxidative stress changes due to sex hormones. Braz J Med Biol Res 35: 1075–1081, 2002. [DOI] [PubMed] [Google Scholar]
- 10.Barrettconnor E, Khaw KT. Endogenous sex-hormones and cardiovascular-disease in men—a prospective population-based study. Circulation 78: 539–545, 1988. [DOI] [PubMed] [Google Scholar]
- 11.Barton M, Prossnitz ER, Meyer MR. Testosterone and secondary hypertension: new pieces to the puzzle. Hypertension 59: 1101–1103, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Basaria S. Androgen abuse in athletes: detection and consequences. J Clin Endocrinol Metab 95: 1533–1543, 2010. [DOI] [PubMed] [Google Scholar]
- 13.Basaria S, Coviello AD, Travison TG, Storer TW, Farwell WR, Jette AM, Eder R, Tennstedt S, Ulloor J, Zhang A, Choong K, Lakshman KM, Mazer NA, Miciek R, Krasnoff J, Elmi A, Knapp PE, Brooks B, Appleman E, Aggarwal S, Bhasin G, Hede-Brierley L, Bhatia A, Collins L, LeBrasseur N, Fiore LD, Bhasin S. Adverse events associated with testosterone administration. N Engl J Med 363: 109–122, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bassil N, Alkaade S, Morley JE. The benefits and risks of testosterone replacement therapy: a review. Ther Clin Risk Manag 5: 427–448, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bekesi G, Kakucs R, Varbiro S, Racz K, Sprintz D, Feher J, Szekacs B. In vitro effects of different steroid hormones on superoxide anion production of human neutrophil granulocytes. Steroids 65: 889–894, 2000. [DOI] [PubMed] [Google Scholar]
- 16.Boje A, Moesby L, Timm M, Hansen EW. Immunomodulatory effects of testosterone evaluated in all-trans retinoic acid differentiated HL-60 cells, granulocytes, and monocytes. Int Immunopharmacol 12: 573–579, 2012. [DOI] [PubMed] [Google Scholar]
- 17.Booth A, Johnson DR, Granger DA. Testosterone and men's health. J Behav Med 22: 1–19, 1999. [DOI] [PubMed] [Google Scholar]
- 18.Boveris A, Cadenas E. Mitochondrial production of superoxide anions and its relationship to the antimycin insensitive respiration. FEBS Lett 54: 311–314, 1975. [DOI] [PubMed] [Google Scholar]
- 19.Brandes RP, Schroder K. NOXious phosphorylation: Smooth muscle reactive oxygen species production is facilitated by direct activation of the NADPH oxidase Nox1. Circ Res 115: 898–900, 2014. [DOI] [PubMed] [Google Scholar]
- 20.Brandes RP, Takac I, Schroder K. No superoxide–no stress?: Nox4, the good NADPH oxidase! Arterioscler Thromb Vasc Biol 31: 1255–1257, 2011. [DOI] [PubMed] [Google Scholar]
- 21.Brinkmann AO. Molecular mechanisms of androgen action—a historical perspective. Methods Mol Biol 776: 3–24, 2011. [DOI] [PubMed] [Google Scholar]
- 22.Brown-Séquard C. The effects produced on man by subcutaneous injections of a liquid obtained from the testicles of animals. Lancet 20: 105–107, 1889. [Google Scholar]
- 23.Callera GE, Montezano AC, Yogi A, Tostes RC, He Y, Schiffrin EL, Touyz RM. c-Src-dependent nongenomic signaling responses to aldosterone are increased in vascular myocytes from spontaneously hypertensive rats. Hypertension 46: 1032–1038, 2005. [DOI] [PubMed] [Google Scholar]
- 24.Carrero JJ, Qureshi AR, Nakashima A, Arver S, Parini P, Lindholm B, Barany P, Heimburger O, Stenvinkel P. Prevalence and clinical implications of testosterone deficiency in men with end-stage renal disease. Nephrol Dial Transplant 26: 184–190, 2011. [DOI] [PubMed] [Google Scholar]
- 25.Carter JR, Durocher JJ, Larson RA, DellaValla JP, Yang H. Sympathetic neural responses to 24-hour sleep deprivation in humans: sex differences. Am J Physiol Heart Circ Physiol 302: H1991–H1997, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cauley JA, Gutai JP, Kuller LH, Dai WS. Usefulness of sex steroid-hormone levels in predicting coronary-artery disease in men. Am J Cardiol 60: 771–777, 1987. [DOI] [PubMed] [Google Scholar]
- 27.Chainy GB, Samantaray S, Samanta L. Testosterone-induced changes in testicular antioxidant system. Andrologia 29: 343–349, 1997. [DOI] [PubMed] [Google Scholar]
- 28.Chao TC, Van Alten PJ, Walter RJ. Steroid sex hormones and macrophage function: modulation of reactive oxygen intermediates and nitrite release. Am J Reprod Immunol 32: 43–52, 1994. [DOI] [PubMed] [Google Scholar]
- 29.Chaves EA, Pereira-Junior PP, Fortunato RS, Masuda MO, de Carvalho AC, de Carvalho DP, Oliveira MF, Nascimento JH. Nandrolone decanoate impairs exercise-induced cardioprotection: role of antioxidant enzymes. J Steroid Biochem Mol Biol 99: 223–230, 2006. [DOI] [PubMed] [Google Scholar]
- 30.Chen YR, Zweier JL. Cardiac mitochondria and reactive oxygen species generation. Circ Res 114: 524–537, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cheuk BL, Leung PS, Lo AC, Wong PY. Androgen control of cyclooxygenase expression in the rat epididymis. Biol Reprod 63: 775–780, 2000. [DOI] [PubMed] [Google Scholar]
- 32.Chignalia AZ, Oliveira MA, Debbas V, Dull RO, Laurindo FR, Touyz RM, Carvalho MH, Fortes ZB, Tostes RC. Testosterone induces leucocyte migration by NADPH oxidase-driven ROS- and COX2-dependent mechanisms. Clin Sci (Lond) 129: 39–48, 2015. [DOI] [PubMed] [Google Scholar]
- 33.Chignalia AZ, Schuldt EZ, Camargo LL, Montezano AC, Callera GE, Laurindo FR, Lopes LR, Avellar MC, Carvalho MH, Fortes ZB, Touyz RM, Tostes RC. Testosterone induces vascular smooth muscle cell migration by NADPH oxidase and c-Src-dependent pathways. Hypertension 59: 1263–1271, 2012. [DOI] [PubMed] [Google Scholar]
- 34.Chinnathambi V, Blesson CS, Vincent KL, Saade GR, Hankins GD, Yallampalli C, Sathishkumar K. Elevated testosterone levels during rat pregnancy cause hypersensitivity to angiotensin II and attenuation of endothelium-dependent vasodilation in uterine arteries. Hypertension 64: 405–414, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chinnathambi V, More AS, Hankins GD, Yallampalli C, Sathishkumar K. Gestational exposure to elevated testosterone levels induces hypertension via heightened vascular angiotensin II type 1 receptor signaling in rats. Biol Reprod 91: 6, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chinnathambi V, Yallampalli C, Sathishkumar K. Prenatal testosterone induces sex-specific dysfunction in endothelium-dependent relaxation pathways in adult male and female rats. Biol Reprod 89: 97, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cho MH, Jung KJ, Jang HS, Kim JI, Park KM. Orchiectomy attenuates kidney fibrosis after ureteral obstruction by reduction of oxidative stress in mice. Am J Nephrol 35: 7–16, 2012. [DOI] [PubMed] [Google Scholar]
- 38.Christakou CD, Diamanti-Kandarakis E. Role of androgen excess on metabolic aberrations and cardiovascular risk in women with polycystic ovary syndrome. Womens Health 4: 583–594, 2008. [DOI] [PubMed] [Google Scholar]
- 39.Clempus RE, Sorescu D, Dikalova AE, Pounkova L, Jo P, Sorescu GP, Schmidt HH, Lassegue B, Griendling KK. Nox4 is required for maintenance of the differentiated vascular smooth muscle cell phenotype. Arterioscler Thromb Vasc Biol 27: 42–48, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Corona G, Monami M, Boddi V, Cameron-Smith M, Fisher AD, de Vita G, Melani C, Balzi D, Sforza A, Forti G, Mannucci E, Maggi M. Low testosterone is associated with an increased risk of MACE lethality in subjects with erectile dysfunction. J Sex Med 7: 1557–1564, 2010. [DOI] [PubMed] [Google Scholar]
- 41.Costa TJ, Ceravolo GS, dos Santos RA, de Oliveira MA, Araujo PX, Giaquinto LR, Tostes RC, Akamine EH, Fortes ZB, Dantas AP, Carvalho MH. Association of testosterone with estrogen abolishes the beneficial effects of estrogen treatment by increasing ROS generation in aorta endothelial cells. Am J Physiol Heart Circ Physiol 308: H723–H732, 2015. [DOI] [PubMed] [Google Scholar]
- 42.Cunningham RL, Singh M, O'Bryant SE, Hall JR, Barber RC. Oxidative stress, testosterone, and cognition among Caucasian and Mexican-American men with and without Alzheimer's disease. J Alzheimers Dis 40: 563–573, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.de Groot PC, Dekkers OM, Romijn JA, Dieben SW, Helmerhorst FM. PCOS, coronary heart disease, stroke and the influence of obesity: a systematic review and meta-analysis. Hum Reprod Update 17: 495–500, 2011. [DOI] [PubMed] [Google Scholar]
- 44.de Souza-Junior TP, Yamada AK, Simao R, Polotow TG, Curi R, Pope Z, Willardson JM, Barros MP. Supra-physiological doses of testosterone affect membrane oxidation of human neutrophils monitored by the fluorescent probe C(1)(1)-BODIPY(5)(8)(1)/(5)(9)(1). Eur J Appl Physiol 113: 1241–1248, 2013. [DOI] [PubMed] [Google Scholar]
- 45.Dikalov SI, Ungvari Z. Role of mitochondrial oxidative stress in hypertension. Am J Physiol Heart Circ Physiol 305: H1417–H1427, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dobrzycki S, Serwatka W, Nadlewski S, Korecki J, Jackowski R, Paruk J, Ladny JR, Hirnle T. An assessment of correlations between endogenous sex hormone levels and the extensiveness of coronary heart disease and the ejection fraction of the left ventricle in males. J Med Invest 50: 162–169, 2003. [PubMed] [Google Scholar]
- 47.Droge W. Free radicals in the physiological control of cell function. Physiol Rev 82: 47–95, 2002. [DOI] [PubMed] [Google Scholar]
- 48.Edwards EA, Hamilton JB, Duntley SQ. Testosterone propionate as a therapeutic agent in patients with organic disease of the peripheral vessels—preliminary report. N Engl J Med 220: 865–865, 1939. [Google Scholar]
- 49.ElBaradie K, Wang Y, Boyan BD, Schwartz Z. Rapid membrane responses to dihydrotestosterone are sex dependent in growth plate chondrocytes. J Steroid Biochem Mol Biol 132: 15–23, 2012. [DOI] [PubMed] [Google Scholar]
- 50.Eleawa SM, Sakr HF, Hussein AM, Assiri AS, Bayoumy NM, Alkhateeb M. Effect of testosterone replacement therapy on cardiac performance and oxidative stress in orchidectomized rats. Acta Physiol (Oxf) 209: 136–147, 2013. [DOI] [PubMed] [Google Scholar]
- 51.Elnakish MT, Hassanain HH, Janssen PM, Angelos MG, Khan M. Emerging role of oxidative stress in metabolic syndrome and cardiovascular diseases: important role of Rac/NADPH oxidase. J Pathol 231: 290–300, 2013. [DOI] [PubMed] [Google Scholar]
- 52.Ely D, Caplea A, Dunphy G, Daneshvar H, Turner M, Milsted A, Takiyyudin M. Spontaneously hypertensive rat Y chromosome increases indexes of sympathetic nervous system activity. Hypertension 29: 613–618, 1997. [DOI] [PubMed] [Google Scholar]
- 53.English KM, Mandour O, Steeds RP, Diver MJ, Jones TH, Channer KS. Men with coronary artery disease have lower levels of androgens than men with normal coronary angiograms. Eur Heart J 21: 890–894, 2000. [DOI] [PubMed] [Google Scholar]
- 54.English KM, Steeds RP, Jones TH, Diver MJ, Channer KS. Low-dose transdermal testosterone therapy improves angina threshold in men with chronic stable angina: A randomized, double-blind, placebo-controlled study. Circulation 102: 1906–1911, 2000. [DOI] [PubMed] [Google Scholar]
- 55.Fanaei H, Karimian SM, Sadeghipour HR, Hassanzade G, Kasaeian A, Attari F, Khayat S, Ramezani V, Javadimehr M. Testosterone enhances functional recovery after stroke through promotion of antioxidant defenses, BDNF levels and neurogenesis in male rats. Brain Res 1558: 74–83, 2014. [DOI] [PubMed] [Google Scholar]
- 56.Fanton L, Belhani D, Vaillant F, Tabib A, Gomez L, Descotes J, Dehina L, Bui-Xuan B, Malicier D, Timour Q. Heart lesions associated with anabolic steroid abuse: comparison of post-mortem findings in athletes and norethandrolone-induced lesions in rabbits. Exp Toxicol Pathol 61: 317–323, 2009. [DOI] [PubMed] [Google Scholar]
- 58.Feletou M, Huang Y, Vanhoutte PM. Endothelium-mediated control of vascular tone: COX-1 and COX-2 products. Br J Pharmacol 164: 894–912, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fernandez-Balsells MM, Murad MH, Lane M, Lampropulos JF, Albuquerque F, Mullan RJ, Agrwal N, Elamin MB, Gallegos-Orozco JF, Wang AT, Erwin PJ, Bhasin S, Montori VM. Clinical review 1: Adverse effects of testosterone therapy in adult men: a systematic review and meta-analysis. J Clin Endocrinol Metab 95: 2560–2575, 2010. [DOI] [PubMed] [Google Scholar]
- 60.Finkle WD, Greenland S, Ridgeway GK, Adams JL, Frasco MA, Cook MB, Fraumeni JF Jr, Hoover RN. Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men. PLoS One 9: e85805, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fisher M, Appleby M, Rittoo D, Cotter L. Myocardial infarction with extensive intracoronary thrombus induced by anabolic steroids. Br J Clin Pract 50: 222–223, 1996. [PubMed] [Google Scholar]
- 61a.Food and Drug Administration. Adding general warning to testosterone products about potential for venous blood clots. http://www.fda.gov/Drugs/DrugSafety/ucm401746. htm. [06/19/2014, 2014].
- 61b.Food and Drug Administration. FDA evaluating risk of stroke, heart attack and death with FDA-approved testosterone products. http://www.fda.gov/downloads/Drugs/DrugSafety/UCM383909.pdf.
- 62.Foradori CD, Weiser MJ, Handa RJ. Non-genomic actions of androgens. Front Neuroendocrinol 29: 169–181, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fortepiani LA, Zhang H, Racusen L, Roberts LJ 2nd, Reckelhoff JF. Characterization of an animal model of postmenopausal hypertension in spontaneously hypertensive rats. Hypertension 41: 640–645, 2003. [DOI] [PubMed] [Google Scholar]
- 64.Frankenfeld SP, Oliveira LP, Ortenzi VH, Rego-Monteiro IC, Chaves EA, Ferreira AC, Leitao AC, Carvalho DP, Fortunato RS. The anabolic androgenic steroid nandrolone decanoate disrupts redox homeostasis in liver, heart and kidney of male Wistar rats. PLoS One 9: e102699, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fu Y, Lu Y, Liu EY, Zhu X, Mahajan GJ, Lu D, Roman RJ, Liu R. Testosterone enhances tubuloglomerular feedback by increasing superoxide production in the macula densa. Am J Physiol Regul Integr Comp Physiol 304: R726–R733, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Garrido P, Salehzadeh F, Duque-Guimaraes DE, Al-Khalili L. Negative regulation of glucose metabolism in human myotubes by supraphysiological doses of 17β-estradiol or testosterone. Metabolism 63: 1178–1187, 2014. [DOI] [PubMed] [Google Scholar]
- 67.Germanakis I, Tsarouhas K, Fragkiadaki P, Tsitsimpikou C, Goutzourelas N, Champsas MC, Stagos D, Rentoukas E, Tsatsakis AM. Oxidative stress and myocardial dysfunction in young rabbits after short-term anabolic steroids administration. Food Chem Toxicol 61: 101–105, 2013. [DOI] [PubMed] [Google Scholar]
- 68.Giorgio M. Oxidative stress and the unfulfilled promises of antioxidant agents. Ecancermedicalscience 9: 556, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Goldstein DR, Dobbs T, Krull B, Plumb VJ. Clenbuterol and anabolic steroids: a previously unreported cause of myocardial infarction with normal coronary arteriograms. South Med J 91: 780–784, 1998. [PubMed] [Google Scholar]
- 70.Gonzales RJ, Ansar S, Duckles SP, Krause DN. Androgenic/estrogenic balance in the male rat cerebral circulation: metabolic enzymes and sex steroid receptors. J Cereb Blood Flow Metab 27: 1841–1852, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gonzales RJ, Duckles SP, Krause DN. Dihydrotestosterone stimulates cerebrovascular inflammation through NF-κB, modulating contractile function. J Cereb Blood Flow Metab 29: 244–253, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gonzalez F, Nair KS, Daniels JK, Basal E, Schimke JM, Blair HE. Hyperandrogenism sensitizes leukocytes to hyperglycemia to promote oxidative stress in lean reproductive-age women. J Clin Endocrinol Metab 97: 2836–2843, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Green DR. Means to an end: apoptosis and other cell death mechanisms. Cold Spring Harbor, NY: Cold Spring Harbor Laboratory Press, 2011, p. xii, 220 p. [Google Scholar]
- 74.Grimm A, Schmitt K, Lang UE, Mensah-Nyagan AG, Eckert A. Improvement of neuronal bioenergetics by neurosteroids: implications for age-related neurodegenerative disorders. Biochim Biophys Acta 1842: 2427–2438, 2014. [DOI] [PubMed] [Google Scholar]
- 75.Grollman A, Harrison TR, Williams JR. The effect of various sterol derivatives on the blood pressure of the rat. J Pharmacol Exp Ther 69: 149–155, 1940. [Google Scholar]
- 76.Grossmann M. Testosterone and glucose metabolism in men: current concepts and controversies. J Endocrinol 220: R37–R55, 2014. [DOI] [PubMed] [Google Scholar]
- 77.Gurer B, Kertmen H, Kasim E, Yilmaz ER, Kanat BH, Sargon MF, Arikok AT, Erguder BI, Sekerci Z. Neuroprotective effects of testosterone on ischemia/reperfusion injury of the rabbit spinal cord. Injury 46: 240–248, 2015. [DOI] [PubMed] [Google Scholar]
- 78.Haddad RM, Kennedy CC, Caples SM, Tracz MJ, Bolona ER, Sideras K, Uraga MV, Erwin PJ, Montori VM. Testosterone and cardiovascular risk in men: a systematic review and meta-analysis of randomized placebo-controlled trials. Mayo Clin Proc 82: 29–39, 2007. [DOI] [PubMed] [Google Scholar]
- 79.Hajjar RR, Kaiser FE, Morley JE. Outcomes of long-term testosterone replacement in older hypogonadal males: a retrospective analysis. J Clin Endocrinol Metab 82: 3793–3796, 1997. [DOI] [PubMed] [Google Scholar]
- 80.Hamm L. Testosterone propionate in the treatment of angina pectoris. J Clin Endocrinol 2: 325–328, 1942. [Google Scholar]
- 81.Hanchang W, Semprasert N, Limjindaporn T, Yenchitsomanus PT, Kooptiwut S. Testosterone protects against glucotoxicity-induced apoptosis of pancreatic β-cells (INS-1) and male mouse pancreatic islets. Endocrinology 154: 4058–4067, 2013. [DOI] [PubMed] [Google Scholar]
- 82.Haring R, Baumeister SE, Volzke H, Dorr M, Kocher T, Nauck M, Wallaschofski H. Prospective inverse associations of sex hormone concentrations in men with biomarkers of inflammation and oxidative stress. J Androl 33: 944–950, 2012. [DOI] [PubMed] [Google Scholar]
- 83.Hartgens F, Kuipers H. Effects of androgenic-anabolic steroids in athletes. Sports Med 34: 513–554, 2004. [DOI] [PubMed] [Google Scholar]
- 84.Hilali N, Vural M, Camuzcuoglu H, Camuzcuoglu A, Aksoy N. Increased prolidase activity and oxidative stress in PCOS. Clin Endocrinol (Oxf) 79: 105–110, 2013. [DOI] [PubMed] [Google Scholar]
- 85.Holmes S, Abbassi B, Su C, Singh M, Cunningham RL. Oxidative stress defines the neuroprotective or neurotoxic properties of androgens in immortalized female rat dopaminergic neuronal cells. Endocrinology 154: 4281–4292, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hu XR, Rui L, Zhu TJ, Xia H, Yang XH, Wang XH, Liu HF, Lu ZB, Jiang H. Low testosterone level in middle-aged male patients with coronary artery disease. Eur J Intern Med 22: E133–E136, 2011. [DOI] [PubMed] [Google Scholar]
- 88.Hurley BF, Seals DR, Hagberg JM, Goldberg AC, Ostrove SM, Holloszy JO, Wiest WG, Goldberg AP. High-density-lipoprotein cholesterol in bodybuilders v powerlifters. Negative effects of androgen use. JAMA 252: 507–513, 1984. [PubMed] [Google Scholar]
- 89.Hwang TI, Liao TL, Lin JF, Lin YC, Lee SY, Lai YC, Kao SH. Low-dose testosterone treatment decreases oxidative damage in TM3 Leydig cells. Asian J Androl 13: 432–437, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hyde Z, Norman PE, Flicker L, Hankey GJ, Almeida OP, McCaul KA, Chubb SAP, Yeap BB. Low free testosterone predicts mortality from cardiovascular disease but not other causes: the Health in Men Study. J Clin Endocrinol Metab 97: 179–189, 2012. [DOI] [PubMed] [Google Scholar]
- 91.Ide H, Lu Y, Yu J, China T, Kumamoto T, Koseki T, Yamaguchi R, Muto S, Horie S. Testosterone promotes DNA damage response under oxidative stress in prostate cancer cell lines. Prostate 72: 1407–1411, 2012. [DOI] [PubMed] [Google Scholar]
- 92.Ikeda Y, Aihara K, Yoshida S, Sato T, Yagi S, Iwase T, Sumitomo Y, Ise T, Ishikawa K, Azuma H, Akaike M, Kato S, Matsumoto T. Androgen-androgen receptor system protects against angiotensin II-induced vascular remodeling. Endocrinology 150: 2857–2864, 2009. [DOI] [PubMed] [Google Scholar]
- 93.Jacob MH, Janner Dda R, Bello-Klein A, Llesuy SF, Ribeiro MF. Dehydroepiandrosterone modulates antioxidant enzymes and Akt signaling in healthy Wistar rat hearts. J Steroid Biochem Mol Biol 112: 138–144, 2008. [DOI] [PubMed] [Google Scholar]
- 94.Javeshghani D, Sairam MR, Schiffrin EL, Touyz RM. Increased blood pressure, vascular inflammation, and endothelial dysfunction in androgen-deficient follitropin receptor knockout male mice. J Am Soc Hypertens 1: 353–361, 2007. [DOI] [PubMed] [Google Scholar]
- 95.Ji H, Menini S, Mok K, Zheng W, Pesce C, Kim J, Mulroney S, Sandberg K. Gonadal steroid regulation of renal injury in renal wrap hypertension. Am J Physiol Renal Physiol 288: F513–F520, 2005. [DOI] [PubMed] [Google Scholar]
- 96.Juliet PA, Hayashi T, Daigo S, Matsui-Hirai H, Miyazaki A, Fukatsu A, Funami J, Iguchi A, Ignarro LJ. Combined effect of testosterone and apocynin on nitric oxide and superoxide production in PMA-differentiated THP-1 cells. Biochim Biophys Acta 1693: 185–191, 2004. [DOI] [PubMed] [Google Scholar]
- 97.Kabakci G, Yildirir A, Can I, Unsal I, Erbas B. Relationship between endogenous sex hormone levels, lipoproteins and coronary atherosclerosis in men undergoing coronary angiography. Cardiology 92: 221–225, 1999. [DOI] [PubMed] [Google Scholar]
- 98.Kang SM, Jang Y, Kim J, Chung N, Cho SY, Chae JS, Lee JH. Effect of oral administration of testosterone on brachial arterial vasoreactivity in men with coronary artery disease. Am J Cardiol 89: 862–864, 2002. [DOI] [PubMed] [Google Scholar]
- 99.Khalil RA. Sex hormones as potential modulators of vascular function in hypertension. Hypertension 46: 249–254, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Khaw KT, Dowsett M, Folkerd E, Bingham S, Wareham N, Luben R, Welch A, Day N. Endogenous testosterone and mortality due to all causes, cardiovascular disease, and cancer in men: European prospective investigation into cancer in Norfolk (EPIC-Norfolk) prospective population study. Circulation 116: 2694–2701, 2007. [DOI] [PubMed] [Google Scholar]
- 101.Kienitz T, Quinkler M. Testosterone and blood pressure regulation. Kidney Blood Press Res 31: 71–79, 2008. [DOI] [PubMed] [Google Scholar]
- 102.Kim J, Kil IS, Seok YM, Yang ES, Kim DK, Lim DG, Park JW, Bonventre JV, Park KM. Orchiectomy attenuates post-ischemic oxidative stress and ischemia/reperfusion injury in mice. A role for manganese superoxide dismutase. J Biol Chem 281: 20,349–20,356, 2006. [DOI] [PubMed] [Google Scholar]
- 103.Klapcinska B, Jagsz S, Sadowska-Krepa E, Gorski J, Kempa K, Langfort J. Effects of castration and testosterone replacement on the antioxidant defense system in rat left ventricle. J Physiol Sci 58: 173–177, 2008. [DOI] [PubMed] [Google Scholar]
- 104.Ko E, Choi H, Kim B, Kim M, Park KN, Bae IH, Sung YK, Lee TR, Shin DW, Bae YS. Testosterone stimulates Duox1 activity through GPRC6A in skin keratinocytes. J Biol Chem 289: 28,835–28,845, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Komukai K, Mochizuki S, Yoshimura M. Gender and the renin-angiotensin-aldosterone system. Fundam Clin Pharmacol 24: 687–698, 2010. [DOI] [PubMed] [Google Scholar]
- 106.Kovacheva EL, Hikim AP, Shen R, Sinha I, Sinha-Hikim I. Testosterone supplementation reverses sarcopenia in aging through regulation of myostatin, c-Jun NH2-terminal kinase, Notch, and Akt signaling pathways. Endocrinology 151: 628–638, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kumar DG, Deepa P, Rathi MA, Meenakshi P, Gopalakrishnan VK. Modulatory effects of Crataeva nurvala bark against testosterone and N-methyl-N-nitrosourea-induced oxidative damage in prostate of male albino rats. Pharmacogn Mag 8: 285–291, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lepore G, Gadau S, Peruffo A, Mura A, Mura E, Floris A, Balzano F, Zedda M, Farina V. Aromatase expression in cultured fetal sheep astrocytes after nitrosative/oxidative damage. Cell Tissue Res 344: 407–413, 2011. [DOI] [PubMed] [Google Scholar]
- 109.Lerchbaum E, Pilz S, Boehm BO, Grammer TB, Obermayer-Pietsch B, Marz W. Combination of low free testosterone and low vitamin D predicts mortality in older men referred for coronary angiography. Clin Endocrinol 77: 475–483, 2012. [DOI] [PubMed] [Google Scholar]
- 110.Lesser MA. The treatment of angina pectoris with testosterone propionate. Preliminary report. N Engl J Med 226: 51–54, 1942. [Google Scholar]
- 111.Li L, Guo CY, Jia EZ, Zhu TB, Wang LS, Cao KJ, Ma WZ, Yang ZJ. Testosterone is negatively associated with the severity of coronary atherosclerosis in men. Asian J Androl 14: 875–878, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Lin H, Lu JP, Laflamme P, Qiao S, Shayegan B, Bryskin I, Monardo L, Wilson BC, Singh G, Pinthus JH. Inter-related in vitro effects of androgens, fatty acids and oxidative stress in prostate cancer: a mechanistic model supporting prevention strategies. Int J Oncol 37: 761–766, 2010. [DOI] [PubMed] [Google Scholar]
- 113.Littleton-Kearney M, Hurn PD. Testosterone as a modulator of vascular behavior. Biol Res Nurs 5: 276–285, 2004. [DOI] [PubMed] [Google Scholar]
- 114.Liu S, Navarro G, Mauvais-Jarvis F. Androgen excess produces systemic oxidative stress and predisposes to beta-cell failure in female mice. PLoS One 5: e11302, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lopes RA, Neves KB, Pestana CR, Queiroz AL, Zanotto CZ, Chignalia AZ, Valim YM, Silveira LR, Curti C, Tostes RC. Testosterone induces apoptosis in vascular smooth muscle cells via extrinsic apoptotic pathway with mitochondria-generated reactive oxygen species involvement. Am J Physiol Heart Circ Physiol 306: H1485–H1494, 2014. [DOI] [PubMed] [Google Scholar]
- 116.Luchtefeld M, Drexler H, Schieffer B. 5-Lipoxygenase is involved in the angiotensin II-induced NAD(P)H-oxidase activation. Biochem Biophys Res Commun 308: 668–672, 2003. [DOI] [PubMed] [Google Scholar]
- 117.Malkin CJ, Pugh PJ, Morris PD, Asif S, Jones TH, Channer KS. Low serum testosterone and increased mortality in men with coronary heart disease. Heart 96: 1821–1825, 2010. [DOI] [PubMed] [Google Scholar]
- 118.Mancini A, Leone E, Festa R, Grande G, Silvestrini A, de Marinis L, Pontecorvi A, Maira G, Littarru GP, Meucci E. Effects of testosterone on antioxidant systems in male secondary hypogonadism. J Androl 29: 622–629, 2008. [DOI] [PubMed] [Google Scholar]
- 119.Maric-Bilkan C, Manigrasso MB. Sex differences in hypertension: contribution of the renin-angiotensin system. Gend Med 9: 287–291, 2012. [DOI] [PubMed] [Google Scholar]
- 120.Marin DP, Bolin AP, dos Santos Rde C., Curi R., Otton R. Testosterone suppresses oxidative stress in human neutrophils. Cell Biochem Funct 28: 394–402, 2010. [DOI] [PubMed] [Google Scholar]
- 121.Marrachelli VG, Miranda FJ, Centeno JM, Burguete MC, Castello-Ruiz M, Jover-Mengual T, Perez AM, Salom JB, Torregrosa G, Alborch E. Mechanisms involved in the relaxant action of testosterone in the renal artery from male normoglycemic and diabetic rabbits. Pharmacol Res 61: 149–156, 2010. [DOI] [PubMed] [Google Scholar]
- 122.Marrachelli VG, Miranda FJ, Centeno JM, Salom JB, Torregrosa G, Jover-Mengual T, Perez AM, Moro MA, Alborch E. Role of NO-synthases and cyclooxygenases in the hyperreactivity of male rabbit carotid artery to testosterone under experimental diabetes. Pharmacol Res 61: 62–70, 2010. [DOI] [PubMed] [Google Scholar]
- 123.Martinez-Revelles S, Avendano MS, Garcia-Redondo AB, Alvarez Y, Aguado A, Perez-Giron JV, Garcia-Redondo L, Esteban V, Redondo JM, Alonso MJ, Briones AM, Salaices M. Reciprocal relationship between reactive oxygen species and cyclooxygenase-2 and vascular dysfunction in hypertension. Antioxid Redox Signal 18: 51–65, 2013. [DOI] [PubMed] [Google Scholar]
- 124.Martorell A, Blanco-Rivero J, Aras-Lopez R, Sagredo A, Balfagon G, Ferrer M. Orchidectomy increases the formation of prostanoids and modulates their role in the acetylcholine-induced relaxation in the rat aorta. Cardiovasc Res 77: 590–599, 2008. [DOI] [PubMed] [Google Scholar]
- 125.Ment J, Ludman PF. Coronary thrombus in a 23 year old anabolic steroid user. Heart 88: 342, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Meydan S, Kus I, Tas U, Ogeturk M, Sancakdar E, Dabak DO, Zararsiz I, Sarsilmaz M. Effects of testosterone on orchiectomy-induced oxidative damage in the rat hippocampus. J Chem Neuroanat 40: 281–285, 2010. [DOI] [PubMed] [Google Scholar]
- 127.Militaru C, Donoiu I, Dracea O, Ionescu DD. Serum testosterone and short-term mortality in men with acute myocardial infarction. Cardiol J 17: 249–253, 2010. [PubMed] [Google Scholar]
- 128.Mooradian AD, Morley JE, Korenman SG. Biological actions of androgens. Endocr Rev 8: 1–28, 1987. [DOI] [PubMed] [Google Scholar]
- 129.Morakinyo AO, Adekunbi DA, Dada KA, Adegoke OA. Testosterone promotes glucose intolerance, lipid disorder and oxidative stress in type 1 diabetic rats. J Basic Clin Physiol Pharmacol 25: 1–8, 2013. [DOI] [PubMed] [Google Scholar]
- 130.Morales A. The long and tortuous history of the discovery of testosterone and its clinical application. J Sex Med 10: 1178–1183, 2013. [DOI] [PubMed] [Google Scholar]
- 131.Morgentaler A, Miner MM, Caliber M, Guay AT, Khera M, Traish AM. Testosterone therapy and cardiovascular risk: advances and controversies. Mayo Clin Proc 90: 224–251, 2015. [DOI] [PubMed] [Google Scholar]
- 132.Mostafa T, Rashed L, Kotb K, Taymour M. Effect of testosterone and frequent low-dose sildenafil/tadalafil on cavernous tissue oxidative stress of aged diabetic rats. Andrologia 44: 411–415, 2012. [DOI] [PubMed] [Google Scholar]
- 133.Muraleedharan V, Marsh H, Kapoor D, Channer KS, Jones TH. Testosterone deficiency is associated with increased risk of mortality and testosterone replacement improves survival in men with type 2 diabetes. Eur J Endocrinol 169: 725–733, 2013. [DOI] [PubMed] [Google Scholar]
- 134.New MI, Josso N. Disorders of gonadal differentiation and congenital adrenal hyperplasia. Endocrinol Metab Clin North Am 17: 339–366, 1988. [PubMed] [Google Scholar]
- 135.Oettel M. The endocrine pharmacology of testosterone therapy in men. Naturwissenschaften 91: 66–76, 2004. [DOI] [PubMed] [Google Scholar]
- 136.Ong PJ, Patrizi G, Chong WC, Webb CM, Hayward CS, Collins P. Testosterone enhances flow-mediated brachial artery reactivity in men with coronary artery disease. Am J Cardiol 85: 269–272, 2000. [DOI] [PubMed] [Google Scholar]
- 137.Osterlund KL, Handa RJ, Gonzales RJ. Dihydrotestosterone alters cyclooxygenase-2 levels in human coronary artery smooth muscle cells. Am J Physiol Endocrinol Metab 298: E838–E845, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ota H, Akishita M, Akiyoshi T, Kahyo T, Setou M, Ogawa S, Iijima K, Eto M, Ouchi Y. Testosterone deficiency accelerates neuronal and vascular aging of SAMP8 mice: protective role of eNOS and SIRT1. PLoS One 7: e29598, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Page-Wilson G, Goulart AC, Rexrode KM. Interrelation between sex hormones and plasma sex hormone-binding globulin and hemoglobin A1c in healthy postmenopausal women. Metab Syndr Relat Disord 7: 249–254, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Pansarasa O, D'Antona G, Gualea MR, Marzani B, Pellegrino MA, Marzatico F. “Oxidative stress”: effects of mild endurance training and testosterone treatment on rat gastrocnemius muscle. Eur J Appl Physiol 87: 550–555, 2002. [DOI] [PubMed] [Google Scholar]
- 141.Papalia MA, Davis SR. What is the rationale for androgen therapy for women? Treat Endocrinol 2: 77–84, 2003. [DOI] [PubMed] [Google Scholar]
- 142.Paravicini TM, Touyz RM. NADPH oxidases, reactive oxygen species, and hypertension: clinical implications and therapeutic possibilities. Diabetes Care 31 Suppl 2: S170–S180, 2008. [DOI] [PubMed] [Google Scholar]
- 143.Patel SM, Ratcliffe SJ, Reilly MP, Weinstein R, Bhasin S, Blackman MR, Cauley JA, Sutton-Tyrrell K, Robbins J, Fried LP, Cappola AR. Higher serum testosterone concentration in older women is associated with insulin resistance, metabolic syndrome, and cardiovascular disease. J Clin Endocrinol Metab 94: 4776–4784, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Perez-Torres I, Roque P, El Hafidi M, Diaz-Diaz E, Banos G. Association of renal damage and oxidative stress in a rat model of metabolic syndrome. Influence of gender. Free Radic Res 43: 761–771, 2009. [DOI] [PubMed] [Google Scholar]
- 145.Phillips GB, Pinkernell BH, Jing TY. The association of hypotestosteronemia with coronary-artery disease in men. Arterioscler Thromb 14: 701–706, 1994. [DOI] [PubMed] [Google Scholar]
- 146.Pick E. Role of the Rho GTPase Rac in the activation of the phagocyte NADPH oxidase: outsourcing a key task. Small GTPases 5: e27952, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Pingili AK, Kara M, Khan NS, Estes AM, Lin Z, Li W, Gonzalez FJ, Malik KU. 6β-Hydroxytestosterone, a cytochrome P450 1B1 metabolite of testosterone, contributes to angiotensin II-induced hypertension and its pathogenesis in male mice. Hypertension 65: 1279–1287, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Pinthus JH, Bryskin I, Trachtenberg J, Lu JP, Singh G, Fridman E, Wilson BC. Androgen induces adaptation to oxidative stress in prostate cancer: implications for treatment with radiation therapy. Neoplasia 9: 68–80, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Pisoschi AM, Pop A. The role of antioxidants in the chemistry of oxidative stress: A review. Eur J Med Chem 97: 55–74, 2015. [DOI] [PubMed] [Google Scholar]
- 150.Ponikowska B, Jankowska EA, Maj J, Wegrzynowska-Teodorczyk K, Biel B, Reczuch K, Borodulin-Nadzieja L, Banasiak W, Ponikowski P. Gonadal and adrenal androgen deficiencies as independent predictors of increased cardiovascular mortality in men with type II diabetes mellitus and stable coronary artery disease. Int J Cardiol 143: 343–348, 2010. [DOI] [PubMed] [Google Scholar]
- 151.Prasad S, Kalra N, Singh M, Shukla Y. Protective effects of lupeol and mango extract against androgen induced oxidative stress in Swiss albino mice. Asian J Androl 10: 313–318, 2008. [DOI] [PubMed] [Google Scholar]
- 152.Puttabyatappa Y, Stallone JN, Ergul A, El-Remessy AB, Kumar S, Black S, Johnson M, Owen MP, White RE. Peroxynitrite mediates testosterone-induced vasodilation of microvascular resistance vessels. J Pharmacol Exp Ther 345: 7–14, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Puurunen J, Piltonen T, Morin-Papunen L, Perheentupa A, Jarvela I, Ruokonen A, Tapanainen JS. Unfavorable hormonal, metabolic, and inflammatory alterations persist after menopause in women with PCOS. J Clin Endocrinol Metab 96: 1827–1834, 2011. [DOI] [PubMed] [Google Scholar]
- 154.Pye SR, Huhtaniemi IT, Finn JD, Lee DM, O'Neill TW, Tajar A, Bartfai G, Boonen S, Casanueva FF, Forti G, Giwercman A, Han TS, Kula K, Lean ME, Pendleton N, Punab M, Rutter MK, Vanderschueren D, Wu FCW, Grp ES. Late-onset hypogonadism and mortality in aging men. J Clin Endocrinol Metab 99: 1357–1366, 2014. [DOI] [PubMed] [Google Scholar]
- 155.Quan A, Chakravarty S, Chen JK, Chen JC, Loleh S, Saini N, Harris RC, Capdevila J, Quigley R. Androgens augment proximal tubule transport. Am J Physiol Renal Physiol 287: F452–F459, 2004. [DOI] [PubMed] [Google Scholar]
- 156.Ray R, Murdoch CE, Wang M, Santos CX, Zhang M, Alom-Ruiz S, Anilkumar N, Ouattara A, Cave AC, Walker SJ, Grieve DJ, Charles RL, Eaton P, Brewer AC, Shah AM. Endothelial Nox4 NADPH oxidase enhances vasodilatation and reduces blood pressure in vivo. Arterioscler Thromb Vasc Biol 31: 1368–1376, 2011. [DOI] [PubMed] [Google Scholar]
- 157.Razmara A, Duckles SP, Krause DN, Procaccio V. Estrogen suppresses brain mitochondrial oxidative stress in female and male rats. Brain Res 1176: 71–81, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Reckelhoff JF. Gender differences in the regulation of blood pressure. Hypertension 37: 1199–1208, 2001. [DOI] [PubMed] [Google Scholar]
- 159.Reckelhoff JF, Yanes LL, Iliescu R, Fortepiani LA, Granger JP. Testosterone supplementation in aging men and women: possible impact on cardiovascular-renal disease. Am J Physiol Renal Physiol 289: F941–F948, 2005. [DOI] [PubMed] [Google Scholar]
- 160.Rezvanfar MA, Shojaei Saadi HA, Gooshe M, Abdolghaffari AH, Baeeri M, Abdollahi M. Ovarian aging-like phenotype in the hyperandrogenism-induced murine model of polycystic ovary. Oxid Med Cell Longev 2014: 948951, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Riezzo I, De Carlo D, Neri M, Nieddu A, Turillazzi E, Fineschi V. Heart disease induced by AAS abuse, using experimental mice/rats models and the role of exercise-induced cardiotoxicity. Mini Rev Med Chem 11: 409–424, 2011. [DOI] [PubMed] [Google Scholar]
- 162.Ripple MO, Hagopian K, Oberley TD, Schatten H, Weindruch R. Androgen-induced oxidative stress in human LNCaP prostate cancer cells is associated with multiple mitochondrial modifications. Antioxid Redox Signal 1: 71–81, 1999. [DOI] [PubMed] [Google Scholar]
- 163.Rosano GM, Leonardo F, Pagnotta P, Pelliccia F, Panina G, Cerquetani E, della Monica PL, Bonfigli B, Volpe M, Chierchia SL. Acute anti-ischemic effect of testosterone in men with coronary artery disease. Circulation 99: 1666–1670, 1999. [DOI] [PubMed] [Google Scholar]
- 164.Rosano GMC, Sheiban I, Massaro R, Pagnotta P, Marazzi G, Vitale C, Mercuro G, Volterrani M, Aversa A, Fini M. Low testosterone levels are associated with coronary artery disease in male patients with angina. Intl J Impot Res 19: 176–182, 2007. [DOI] [PubMed] [Google Scholar]
- 165.Roy AK, Tyagi RK, Song CS, Lavrovsky Y, Ahn SC, Oh TS, Chatterjee B. Androgen receptor: structural domains and functional dynamics after ligand-receptor interaction. Ann NY Acad Sci 949: 44–57, 2001. [DOI] [PubMed] [Google Scholar]
- 166.Saad F, Gooren LJ, Haider A, Yassin A. A dose-response study of testosterone on sexual dysfunction and features of the metabolic syndrome using testosterone gel and parenteral testosterone undecanoate. J Androl 29: 102–105, 2008. [DOI] [PubMed] [Google Scholar]
- 167.Saborido A, Naudi A, Portero-Otin M, Pamplona R, Megias A. Stanozolol treatment decreases the mitochondrial ROS generation and oxidative stress induced by acute exercise in rat skeletal muscle. J Appl Physiol (1985) 110: 661–669, 2011. [DOI] [PubMed] [Google Scholar]
- 168.Sadowska-Krepa E, Klapcinska B, Jagsz S, Chalimoniuk M, Chrapusta SJ, Wanke A, Grieb P, Langfort J. Diverging oxidative damage and heat shock protein 72 responses to endurance training and chronic testosterone propionate treatment in three striated muscle types of adolescent male rats. J Physiol Pharmacol 64: 639–647, 2013. [PubMed] [Google Scholar]
- 169.Schmitz I, Kirchhoff S, Krammer PH. Regulation of death receptor-mediated apoptosis pathways. Int J Biochem Cell Biol 32: 1123–1136, 2000. [DOI] [PubMed] [Google Scholar]
- 170.Sedeek M, Hebert RL, Kennedy CR, Burns KD, Touyz RM. Molecular mechanisms of hypertension: role of Nox family NADPH oxidases. Curr Opin Nephrol Hypertens 18: 122–127, 2009. [DOI] [PubMed] [Google Scholar]
- 171.Sharma R, Oni OA, Gupta K, Chen G, Sharma M, Dawn B, Sharma R, Parashara D, Savin VJ, Ambrose JA, Barua RS. Normalization of testosterone level is associated with reduced incidence of myocardial infarction and mortality in men. Eur Heart J 36: 2706–2715, 2015. [DOI] [PubMed] [Google Scholar]
- 172.Shaw LJ, Bairey Merz CN, Azziz R, Stanczyk FZ, Sopko G, Braunstein GD, Kelsey SF, Kip KE, Cooper-Dehoff RM, Johnson BD, Vaccarino V, Reis SE, Bittner V, Hodgson TK, Rogers W, Pepine CJ. Postmenopausal women with a history of irregular menses and elevated androgen measurements at high risk for worsening cardiovascular event-free survival: results from the National Institutes of Health—National Heart, Lung, and Blood Institute sponsored Women's Ischemia Syndrome Evaluation. J Clin Endocrinol Metab 93: 1276–1284, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 173.Shores MM, Smith NL, Forsberg CW, Anawalt BD, Matsumoto AM. Testosterone treatment and mortality in men with low testosterone levels. J Clin Endocrinol Metab 97: 2050–2058, 2012. [DOI] [PubMed] [Google Scholar]
- 174.Siddiqui IA, Raisuddin S, Shukla Y. Protective effects of black tea extract on testosterone induced oxidative damage in prostate. Cancer Lett 227: 125–132, 2005. [DOI] [PubMed] [Google Scholar]
- 175.Singh H, Cheng J, Deng H, Kemp R, Ishizuka T, Nasjletti A, Schwartzman ML. Vascular cytochrome P450 4A expression and 20-hydroxyeicosatetraenoic acid synthesis contribute to endothelial dysfunction in androgen-induced hypertension. Hypertension 50: 123–129, 2007. [DOI] [PubMed] [Google Scholar]
- 176.Skogastierna C, Hotzen M, Rane A, Ekstrom L. A supraphysiological dose of testosterone induces nitric oxide production and oxidative stress. Eur J Prev Cardiol 21: 1049–1054, 2013. [DOI] [PubMed] [Google Scholar]
- 177.Song D, Arikawa E, Galipeau D, Battell M, McNeill JH. Androgens are necessary for the development of fructose-induced hypertension. Hypertension 43: 667–672, 2004. [DOI] [PubMed] [Google Scholar]
- 178.Song J, Wadhwa L, Bejjani BA, O'Brien WE. Determination of 3-keto-4-ene steroids and their hydroxylated metabolites catalyzed by recombinant human cytochrome P450 1B1 enzyme using gas chromatography-mass spectrometry with trimethylsilyl derivatization. J Chromatogr B Analyt Technol Biomed Life Sci 791: 127–135, 2003. [DOI] [PubMed] [Google Scholar]
- 179.Stanworth RD, Jones TH. Testosterone for the aging male; current evidence and recommended practice. Clin Interv Aging 3: 25–44, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Sullivan JC, Sasser JM, Pollock JS. Sexual dimorphism in oxidant status in spontaneously hypertensive rats. Am J Physiol Regul Integr Comp Physiol 292: R764–R768, 2007. [DOI] [PubMed] [Google Scholar]
- 181.Sun XY, Donald SP, Phang JM. Testosterone and prostate specific antigen stimulate generation of reactive oxygen species in prostate cancer cells. Carcinogenesis 22: 1775–1780, 2001. [DOI] [PubMed] [Google Scholar]
- 182.Svartberg J, Von Muhlen D, Mathiesen E, Joakimsen O, Bonaa KH, Stensland-Bugge E. Low testosterone levels are associated with carotid atherosclerosis in men. J Int Med 259: 576–582, 2006. [DOI] [PubMed] [Google Scholar]
- 183.Tam NN, Gao Y, Leung YK, Ho SM. Androgenic regulation of oxidative stress in the rat prostate: involvement of NAD(P)H oxidases and antioxidant defense machinery during prostatic involution and regrowth. Am J Pathol 163: 2513–2522, 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Tam NN, Ghatak S, Ho SM. Sex hormone-induced alterations in the activities of antioxidant enzymes and lipid peroxidation status in the prostate of Noble rats. Prostate 55: 1–8, 2003. [DOI] [PubMed] [Google Scholar]
- 185.Tang EH, Vanhoutte PM. Prostanoids and reactive oxygen species: team players in endothelium-dependent contractions. Pharmacol Ther 122: 140–149, 2009. [DOI] [PubMed] [Google Scholar]
- 186.Toma M, McAlister FA, Coglianese EE, Vidi V, Vasaiwala S, Bakal JA, Armstrong PW, Ezekowitz JA. Testosterone supplementation in heart failure: a meta-analysis. Circ Heart Fail 5: 315–321, 2012. [DOI] [PubMed] [Google Scholar]
- 187.Tothova L, Celec P, Ostatnikova D, Okuliarova M, Zeman M, Hodosy J. Effect of exogenous testosterone on oxidative status of the testes in adult male rats. Andrologia 45: 417–423, 2013. [DOI] [PubMed] [Google Scholar]
- 188.Toufexis DJ, Wilson ME. Dihydrotestosterone differentially modulates the cortisol response of the hypothalamic-pituitary-adrenal axis in male and female rhesus macaques, and restores circadian secretion of cortisol in females. Brain Res 1429: 43–51, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Touyz RM. Reactive oxygen species in vascular biology: role in arterial hypertension. Expert Rev Cardiovasc Ther 1: 91–106, 2003. [DOI] [PubMed] [Google Scholar]
- 190.Touyz RM, Briones AM. Reactive oxygen species and vascular biology: implications in human hypertension. Hypertens Res 34: 5–14, 2011. [DOI] [PubMed] [Google Scholar]
- 191.Touyz RM, Wu XH, He G, Park JB, Chen X, Vacher J, Rajapurohitam V, Schiffrin EL. Role of c-Src in the regulation of vascular contraction and Ca2+ signaling by angiotensin II in human vascular smooth muscle cells. J Hypertens 19: 441–449, 2001. [DOI] [PubMed] [Google Scholar]
- 192.Trabado S, Lamothe S, Maione L, Bouvattier C, Sarfati J, Brailly-Tabard S, Young J. Congenital hypogonadotropic hypogonadism and Kallmann syndrome as models for studying hormonal regulation of human testicular endocrine functions. Ann Endocrinol (Paris) 75: 79–87, 2014. [DOI] [PubMed] [Google Scholar]
- 193.Veeramani S, Yuan TC, Lin FF, Lin MF. Mitochondrial redox signaling by p66Shc is involved in regulating androgenic growth stimulation of human prostate cancer cells. Oncogene 27: 5057–5068, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Victor VM, Rocha M, Banuls C, Rovira-Llopis S, Gomez M, Hernandez-Mijares A. Mitochondrial impairment and oxidative stress in leukocytes after testosterone administration to female-to-male transsexuals. J Sex Med 11: 454–461, 2014. [DOI] [PubMed] [Google Scholar]
- 195.Vigen R, O'Donnell CI, Baron AE, Grunwald GK, Maddox TM, Bradley SM, Barqawi A, Woning G, Wierman ME, Plomondon ME, Rumsfeld JS, Ho PM. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA 310: 1829–1836, 2013. [DOI] [PubMed] [Google Scholar]
- 196.Vikan T, Johnsen SH, Schirmer H, Njolstad I, Svartberg J. Endogenous testosterone and the prospective association with carotid atherosclerosis in men: the Tromso study. Eur J Epidemiol 24: 289–295, 2009. [DOI] [PubMed] [Google Scholar]
- 197.Virdis A, Colucci R, Fornai M, Blandizzi C, Duranti E, Pinto S, Bernardini N, Segnani C, Antonioli L, Taddei S, Salvetti A, Del Tacca M. Cyclooxygenase-2 inhibition improves vascular endothelial dysfunction in a rat model of endotoxic shock: role of inducible nitric-oxide synthase and oxidative stress. J Pharmacol Exp Ther 312: 945–953, 2005. [DOI] [PubMed] [Google Scholar]
- 198.Walker TC. Use of testosterone propionate and estrogenic substance in treatment of essential hypertension, angina pectoris and peripheral vascular disease. J Clin Endocrinol 2: 560–568, 1942. [Google Scholar]
- 199.Webb CM, Adamson DL, de Zeigler D, Collins P. Effect of acute testosterone on myocardial ischemia in men with coronary artery disease. Am J Cardiol 83: 437–439, A439, 1999. [DOI] [PubMed] [Google Scholar]
- 200.Webb CM, McNeill JG, Hayward CS, de Zeigler D, Collins P. Effects of testosterone on coronary vasomotor regulation in men with coronary heart disease. Circulation 100: 1690–1696, 1999. [DOI] [PubMed] [Google Scholar]
- 201.Yanar K, Atukeren P, Cebe T, Kunbaz A, Ozan T, Kansu AD, Durmaz S, Gulec V, Belce A, Aydin S, Cakatay U, Rizvi SI. Ameliorative effects of testosterone administration on renal redox homeostasis in naturally aged rats. Rejuvenation Res 18: 299–312, 2015. [DOI] [PubMed] [Google Scholar]
- 202.Yanes LL, Romero DG, Moulana M, Lima R, Davis DD, Zhang H, Lockhart R, Racusen LC, Reckelhoff JF. Cardiovascular-renal and metabolic characterization of a rat model of polycystic ovary syndrome. Gend Med 8: 103–115, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Yu E, Mercer J, Bennett M. Mitochondria in vascular disease. Cardiovasc Res 95: 173–182, 2012. [DOI] [PubMed] [Google Scholar]
- 204.Zhang GL, Wang W, Kang YX, Xue Y, Yang H, Zhou CM, Shi GM. Chronic testosterone propionate supplement could activated the Nrf2-ARE pathway in the brain and ameliorated the behaviors of aged rats. Behav Brain Res 252: 388–395, 2013. [DOI] [PubMed] [Google Scholar]
- 205.Zhang L, Lei D, Zhu GP, Hong L, Wu SZ. Physiological testosterone retards cardiomyocyte aging in Tfm mice via androgen receptor-independent pathway. Chin Med Sci J 28: 88–94, 2013. [DOI] [PubMed] [Google Scholar]
- 206.Zhang L, Wu S, Ruan Y, Hong L, Xing X, Lai W. Testosterone suppresses oxidative stress via androgen receptor-independent pathway in murine cardiomyocytes. Mol Med Rep 4: 1183–1188, 2011. [DOI] [PubMed] [Google Scholar]
- 207.Zuloaga KL, Gonzales RJ. Dihydrotestosterone attenuates hypoxia inducible factor-1α and cyclooxygenase-2 in cerebral arteries during hypoxia or hypoxia with glucose deprivation. Am J Physiol Heart Circ Physiol 301: H1882–H1890, 2011. [DOI] [PubMed] [Google Scholar]