Abstract
The National Health Service (NHS) is currently facing a financial crisis with a projected deficit of £2billion by the end of financial year 2015/16. As operating rooms (OR) are one of the costliest components in secondary care, improving theatre efficiency should be at the forefront of efforts to improve health service efficiency. The objectives of this study were to characterize the causes of trauma OR delays and to estimate the cost of this inefficiency.
A 1-month prospective single-centre study in St. Mary's Hospital. Turnaround time (TT) was used as the surrogate parameter to measure theatre efficiency. Factors including patient age, ASA score and presence of surgical and anaesthetic consultant were evaluated to identify positive or negative associations with theatre delays. Inefficiency cost was calculated by multiplying the time wasted with staff capacity costs and opportunity costs, found to be £24.77/minute.
The commonest causes for increased TT were delays in sending for patients (50%) and problems with patient transport to the OR (31%). 461 min of delay was observed in 12 days, equivalent to loss of £951.58/theatre/day. Non-statistically significant trends were seen between length of delays and advancing patient age, ASA score and absence of either a senior clinician or an anaesthetic consultant. Interestingly, the trend was not as strong for absence of an anaesthetic consultant.
This study found delays in operating TT to represent a sizable cost, with potential efficiency savings based on TT of £347,327/theatre/year. Further study of a larger sample is warranted to better evaluate the identified trends.
Keywords: Theatre efficiency, Efficiency savings, Theatre delays, Orthopaedics, Cost-analysis
Highlights
-
•
Delays in operating turnaround time result in substantial financial waste.
-
•
Causes of delays are reported in this study.
-
•
Trends between age, ASA score and senior clinician presence with delays were found.
-
•
Resolving this issue could potentially save an estimated £350,000/theatre/year.
1. Introduction
Operating room (OR) inefficiency is a common and well recognised source of financial waste within health services [1]. Currently, the National Health Service (NHS) is facing an unprecedented financial crisis with a projected deficit of £2billion by the end of financial year 2015/16 [2]. Moreover, ongoing austerity measures within the United Kingdom have further increased financial pressure on healthcare expenditure [3]. Although recent health policy has called for efficiency savings of £22billion by 2020 [4], this figure is viewed to be overly ambitious owing to the limitations in productivity within existing NHS services [5]. New evidence-based methods are needed to increase healthcare efficiency so that health services can remain financially viable.
As OR is one of the costliest components in secondary care [6], improving OR efficiency should be at the forefront of efforts to improve health service efficiency. Current recommendations to optimise OR efficiency include improved staff managements and judicious compliance with OR start time [8], [9], [10].
A single-centre service evaluation reported potential savings of approximately £3000/day in its hospital if delays of only 16 min per operation could be avoided [7]. In terms of supply management methods, regulated procurement procedures could also achieve potential savings of £500 million [11], [12].
Whilst several studies have proposed different approaches to improve efficiency within different surgical specialties [13], [14], [15], [16], there is an absence of research evaluating the cost of orthopaedic trauma OR inefficiency to the hospital. The aims of this study were to characterize and quantify delays in orthopaedic trauma ORs, as well as to estimate the cost incurred as a result of OR inefficiency.
2. Methods
2.1. Study design
This prospective study was registered as a healthcare service evaluation at Imperial College NHS Trust. An orthopaedic trauma OR was observed by a study author for 12 days during August 2015, on Mondays, Wednesdays and Fridays for 4 weeks. Data was collected using a self-designed recording sheet. Data collected included patient information (ASA, age, procedure), OR staff involved in the operation, surgical time records and reasons for delays. Surgical timing records included time patient sent for, time patient arrived for anaesthetic, time patient arrived operating room, knife to skin time, time of end of surgery and time patient left the operating room. All operations were carried out under general anaesthetic.
2.2. Data analysis
For the purpose of this study the authorship agree that turnaround time would be the surrogate measure used to evaluate inefficiency, and was defined as the time period in between one patient leaving and a subsequent patient arriving the OR. Turnaround times, TT were split into two groups: turnaround times of more than 25 min (TT > 25 min) and less than 25 min (TT < 25 min), with TT > 25 min considered a delay. ASA score, patient age, presence of a surgical consultant and presence of an anaesthetic consultant were evaluated, as individual factors, to determine whether there was a positive or negative association with turnaround time. ASA was categorized into 2 groups: ≤2 or ≥3. Age was also categorized as either ≤65 or >65. Independent t-test was conducted to identify any significant differences between patient characteristics. Value of p < 0.05 was considered to be statistically significant.
2.3. Capacity cost of staff and opportunity cost
Capacity cost of each staff involved in the operations was calculated, with costs derived from the Unit Costs of Health and Social Care 2014 [17]. In addition to the capacity cost for the staff we also added an additional £15/min of opportunity cost to calculate the total financial loss after a delay of >25 min. Opportunity costs are the loss of income that would have been generated from utilization of the OR by national reimbursement tariffs and this has been estimated to be approximately £15/min from existing health policy research [7].
3. Results
33 surgeries were observed within the 12 days, averaging to 2.8 operations a day per OR. There were 6 days (50%) when the planned trauma list was not completed and 5 days (41.7%) of late starts (>0900a.m.). 21/33 surgeries observed had measurable turnaround times. Surgical procedures that did not have a measureable turnaround time were those cases that were performed at the end of the day. Of the 21 turnaround times, there were 16 with TT > 25 min and 5 with TT < 25 min. The individual reasons for the 16 cases of delays are as presented in Table 1. There were 3 delays in the anaesthetic room (AR), 8 delays in sending for patients and 5 delays in patient arriving.
Table 1.
Reasons for delays in turnaround times between surgeries along with occurring frequency.
| Reason for delay | Specific reasons |
|---|---|
| Delays in the AR | Delay in AR as patient had to be confirmed to have a post op bed [1] Delay in AR as anaesthetist had difficulty locating femoral nerve [2] |
| Delays in patient arriving | Delay in patient arrival as ward was at the far end of the hospital [1] Delay in patient arrival due to availability of porter [3] Delay in patient arrival as time take to transfer from ITU [1] |
| Delays in sending for patients | Delay in sending for patient as patient is unable to give consent [2] Delay in sending for patient as pre-op checks had to be done by the anaesthetists to be fit for surgery [1] Delay in sending for patient as the surgery schedule was not clear and patient was not consented for surgery [1] Delay in OR team sending for the patient due to miscommunication [1] Lack of OR staff hence delay in sending for patient + AR [1] Delay in sending as there was uncertainty regarding next case [1] Delay sending for patient as AR had to be cleaned [1] |
Mean patient age was 47.9 (4–87); mean ASA was 1.9 [1], [2], [3]; mean turnaround time was 45.7 min (13–104 min). A surgical consultant was present in 15/21 of the surgeries whilst an anaesthetic consultant was present in 14/21 of the surgeries. Individual patient data are shown in Table 2. Results of the independent t-test are shown in Table 3, which shows there are no significant differences between the subgroups across all 4 factors.
Table 2.
Information of the 21 surgeries with turnaround time delays.
| Age | ASA | Presence of surgical consultant | Presence of anaesthetic consultant | Turnaround time (minutes) | Delay reason |
|---|---|---|---|---|---|
| 70 | 3 | Present | Present | 31 | Delay in AR |
| 49 | 1 | Present | Present | 13 | – |
| 87 | 3 | Absent | Present | 56 | Delay in AR |
| 47 | 2 | Absent | Present | 23 | – |
| 52 | 1 | Absent | Present | 57 | Delay in patient arrival |
| 81 | 3 | Absent | Present | 41 | – |
| 55 | 3–4 | Absent | Present | 68 | Delay in AR |
| 64 | 2 | Present | Absent | 54 | Delay in sending |
| 14 | 1 | Absent | Absent | 78 | Delay in sending |
| 61 | 2 | Present | Absent | 46 | Delay in sending |
| 71 | 3 | Present | Absent | 63 | Delay in patient arrival |
| 16 | 1 | Present | Present | 29 | Delay in sending |
| 78 | 2 | Present | Present | 104 | Delay in sending |
| 18 | 1 | Present | Absent | 24 | – |
| 15 | 2 | Present | Absent | 28 | Delay in sending |
| 41 | 2 | Present | Absent | 50 | Delay in patient arrival |
| 9 | 1 | Present | Present | 64 | Delay in patient arrival |
| 4 | 1 | Present | Present | 18 | – |
| 5 | 1 | Present | Present | 46 | Delay in patient arrival |
| 84 | 2 | Present | Present | 21 | Delay in sending |
| 81 | 2 | Present | Present | 46 | Delay in sending |
Table 3.
The mean turnaround times for the 3 factors (presence of consultant, ASA score and age) along with its p-value between the relevant groups.
| Factors | N = number of patients | Mean turnaround time (minutes) | P-value | |
|---|---|---|---|---|
| Surgical Consultant | Present | N = 15 | 42.5 | P = 0.308 |
| Absent | N = 6 | 53.8 | ||
| Anaesthetic Consultant | Present | N = 14 | 44.1 | P = 0.649 |
| Absent | N = 7 | 49.0 | ||
| ASA score | <3 | N = 16 | 16 | P = 0.503 |
| >2 | N = 5 | 51.8 | ||
| Age | <66 | N = 14 | 42.7 | P = 0.402 |
| >65 | N = 7 | 51.7 | ||
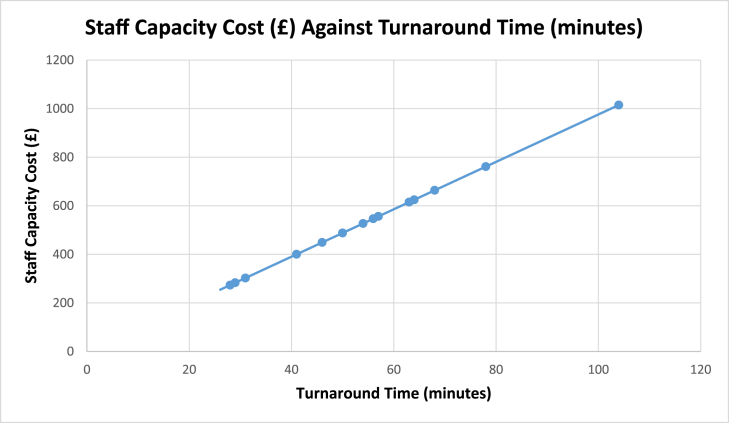
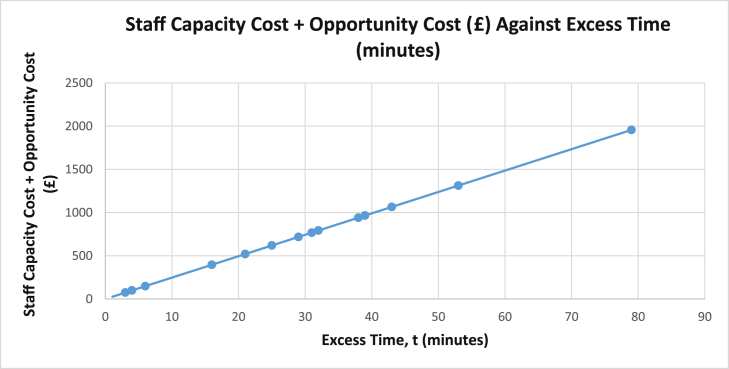
All operations were designated to have 9 dedicated OR staff, although it is to be noted that there were occasions where not all 9 OR staffs were present in theatre; either due to staff on sick leave, unavailability of a senior clinician or that a senior clinician chose not to be present to oversee the operation. The designated 9 OR staff included: consultant anaesthetist, trainee anaesthetist, consultant orthopaedic surgeon, trainee orthopaedic surgeon, operating department practitioner (ODP), two scrub nurses, health care assistant (HCA) and a radiographer. The overall unit cost of the OR staff would be £9.77 per minute, as shown in Table 4. The staff capacity cost in proportion to the total turnaround time is shown in Fig. 1 and illustrates the overall relationship of cost capacity with time. To quantify the overall cost of inefficiency, we have also taken into account the opportunity cost (£15/min) alongside the staff capacity cost for turnaround times exceeding 25 min. This amounted to a financial loss of £24.77/min after the 25-min turnaround. The total cost of inefficiency for delayed turnaround times is shown in Fig. 2 whereby staff capacity costs within the initial 25 min have not been included. By considering the minutes after the 25-min turnaround cut off as delays, over a 12-day period, we observed a total of 461 min in delays of turnaround times, equivalent to an overall cost of £11,418.97 or £951.58/OR/day.
Table 4.
Table showing the unit cost of each OR staff in terms of hour and minute respectively.
| Staff position | Unit cost per hour (£) | Unit cost per minute (£) |
|---|---|---|
| Consultant Anaesthetist | 142 | 2.37 |
| Specialist Registrar Anaesthetist | 60 | 1.00 |
| Consultant Orthopaedic Surgeon | 142 | 2.37 |
| Specialist Registrar Orthopaedic Surgeon | 60 | 1.00 |
| Operating Department Practitioner | 41 | 0.68 |
| Scrub Nurse 1 | 41 | 0.68 |
| Scrub Nurse 2 | 41 | 0.68 |
| HCA | 21 | 0.35 |
| Radiographer | 38 | 0.63 |
| Total | 586 | 9.77 |
Fig. 1.
Graph of staff capacity cost in GBP against overall turnaround time.
Fig. 2.
Graph of staff capacity cost + opportunity cost in GBP against excess time, t, which is derived from turnaround time deducted by 25 min; t = TT-25 min.
4. Discussion
This study found a number of factors contributing to OR inefficiency which represent a sizable cost to the hospital. Over a 12-day period, we observed a total of 461 min in delay of turnaround times, equivalent to an overall cost of £11,418.97 or £951.58/OR/day. Extrapolation of this value would amount to £347,327/OR/year. This suggests that a hospital with 10 ORs could potentially save up to £3million annually by better control of OR turnaround time.
OR inefficiency can generally be categorized into hospital-wide or doctor-related factors. Hospital-wide factors such as availability of ward beds, transfer of patients and poor pre-operative preparations have been found to contribute the most to delays [18]. A few studies have cited doctor-related factors such as the unavailability of surgeons, anaesthetists and nurses as the primary cause of delay [19], [20]. In this study, by using turnaround time as a measure for theatre efficiency, our results found both doctor-related and hospital-wide factors to be substantial, with delay in sending for the patient and delay in the patient arriving in the OR being the main causes of delay. These were due to absent consent forms, incomplete pre-operative assessment and lack of theatre staff, as shown in Table 1. Our finding that delay in sending for patients was a significant cause of delay has never been previously described in existing research. The underlying reasons for these delays were poor communication between staff and absence of a senior clinician to manage the team effectively. Difficulties with patient transport, which was a common problem at our hospital, seems to be a widespread problem as studies have reported that patient arrival or patient transport are the commonest causes of delays [21], [22]. A dedicated portering team may have a role in solving this problem. With regards to delays in the AR, we found several factors contributed to an increase in anaesthetic times, as shown in Table 1. Although training needs and medically complex patients mean that some ‘delays’ are necessary, better communication between surgical team and anaesthetists may aid in improving turnaround times efficiency. For example, a surgeon coming towards the end of the procedure should ask the anaesthetic team if the next patient is having a GA/block, or if they are medically complex, and such patients could be sent for earlier.
In our study, further analysis of factors including ASA score, patient age, presence of a surgical consultant and presence of an anaesthetic consultant have showed that, despite displaying trends with overall turnaround time, these trends were not statistically significant. However it was interesting to note that with absence of an anaesthetic consultant the trend was not as strong as the other factors. Nonetheless, existing research has demonstrated that ASA score is associated with delays of surgery [23] while advanced patient age and absence of senior doctor supervision to have significant associations with surgery delays as well [24]. Based on the trends in this study and limited published findings related to these factors, there is a need for further research or service evaluation to investigate these associations.
Delays in turnaround time result in loss of theatre utilization which is a substantial source of financial waste and loss for hospitals [7]. In this study, we have quantified the cost of every minute wasted (turnaround times after 25 min) based on the combined staff capacity cost and opportunity cost, which together was calculated to be £24.77/min. It is challenging to establish a standardized and acceptable turnaround time. Some studies have used one hour to be the cut-off point [25], [26] with turnaround times exceeding 60 min considered a delay. However, other research in this field has used between 15 and 28 min as the threshold value [27], [28]. In this study, we used 25 min as a maximum turnaround time when establishing a delay. Based on the experience of the authorship and the practices at our institution, there was consensus within the study group that this was an appropriate threshold to use.
A number of recommendations have been put forward to improve OR efficiency including; streamlining administration of preoperative medication [15], [29], improving communication [29], [30], new OR design [31] and stricter schedules to prevent late start to cases [29]. Nonetheless, methods such as process redesign and improving interdisciplinary work flow with well-defined team roles have more substantial evidence in being able to significantly reduce turnaround time [15], [30], [32], [33]. Parallel processing through strategies such as cleaning up the OR whilst the anaesthetists anaesthetize the subsequent patient or beginning OR clean up whilst dressings are placed could also be effective, with one study showing that the amount of saved time allowed addition of cases without a need to hire more staff [32], [33].
Throughout this study, it was observed that problems such as delays in sending for patients, patient transport difficulties, conflicts in case scheduling and poor communication contributed to increased turnaround time. Taking into account that the estimate of inefficiency cost was £347,327 per OR annually, hiring extra porters would seem to be a pragmatic solution to reduce turnaround time. Studies have also shown that employing another anaesthetist in the AR for perioperative process could actually increase profit of the hospital as the gained time outweighs the expense required to hire an additional staff [29], [34]. The delays in turnaround time identified in this study underline the need for further research evaluating the application of the discussed efficiency measures, and their ability to reduce turnaround time delays, and the financial waste it causes.
5. Limitations
There are a few limitations to the study design adopted. Firstly, the small sample size observed meant that the absence of statistical significance demonstrated when evaluating how various factors influence OR efficiency is vulnerable to type II error. Unfortunately, the expansion of our study was restricted because a more expensive prospective observation of OR practices requires increased human and financial resources to enable robust data collection. Further research is required in this field and funding should be considered in advance to facilitate this.
Secondly, this study was mainly focused on the analysis of turnaround time. There are a number of other causes of inefficiency in the operating theatre such as intra-operative delay caused by equipment failure, availability of surgeons, delay of X-ray machines and surgical complications. Therefore our study is likely to grossly underestimate the true financial loss when other aspects of OR inefficiency are considered. Finally, the estimated cost of savings is based on the OR staff in trauma ORs hence may not be applicable in all types of surgery. Nonetheless, the estimates calculated illustrate the potential savings to other hospitals and specialties within the NHS.
Lastly, with this study being a small scale, single-centre study, it may be argued that there are limitations in terms of its external validity. Health service research from single-institutions can be important in improving service design despite this limitation [35]. These studies also provide an observational evidence base to shape health policy and study design [13], [36], [37], [38]. Single-centre pilots form a large proportion of National Health Service Improving Quality research [39] and such research do contribute to informing NHS policy, despite being often arising from only one institution. From the perspective of costing inefficiency, we adopted units of cost from the Personal Social Services Research Unit and these are recognised as having applicability across the National Health Service.
6. Conclusion
This study has found the commonest causes of delay in turnaround times to be the operating team having difficulty in sending for the scheduled patient and problems with transport of the patient to the OR. Although no significant relationship between evaluated factors and delay were found, there were noticeable trends. These trends suggest further analysis with a larger sample size is warranted. Finally, this study has shown that potential efficiency savings based on turnaround time on one OR are sizeable with an estimation of £347,327 annually.
Ethical approval
Service evaluation hence did not need ethical approval.
Sources of funding
No funding.
Author contribution
Miss Wan Wei Ang: study design, data collections, data analysis, writing.
Mr. Sanjeeve Sabharwal: study design, data analysis, writing.
Dr. Helgi Johannsson: study design, review paper.
Mr. Rajarshi Bhattacharya: study design, review paper.
Mr. Chinmay Gupte: study design, review paper.
Conflicts of interest
No conflict of interest.
Guarantor
Miss Wan Wei Ang
Mr. Sanjeeve Sabharwal
Dr. Helgi Johannsson
Mr. Rajarshi Bhattacharya
Mr. Chinmay Gupte
References
- 1.Volpin A., Khan O., Haddad F. Theater cost is £16/Minute so what are you doing just standing there? J. Arthroplast. 2016 Jan;31(1) doi: 10.1016/j.arth.2015.08.008. 18/11/2015-22-6. [DOI] [PubMed] [Google Scholar]
- 2.Campbell D. 2015. NHS Facing £2bn Deficit and ‘Worst Financial Crisis in a Generation’.http://www.theguardian.com/society/2015/oct/09/nhs-trusts-in-england-run-up-almost-1bn-deficit-in-three-months Available at: (accessed 25.10.15) [Google Scholar]
- 3.Price C. 2015. Government Announces £200m Cuts to Public Health Budget.http://www.pulsetoday.co.uk/news/commissioning-news/government-announces-200m-cuts-to-public-health-budget/20010183.fullarticle Available at: (accessed 25.10.15) [Google Scholar]
- 4.Gauke D. 2015. Summer Budget 2015.https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/443232/50325_Summer_Budget_15_Web_Accessible.pdf Available at: (accessed 25.10.15) [Google Scholar]
- 5.The King's Fund . 2015. 1. New Funding and Higher Productivity.http://www.kingsfund.org.uk/health-social-care-three-priorities-new-government/new-funding-higher-productivity Available at: (accessed 18.11.15) [Google Scholar]
- 6.Denton B., Viapiano J., Vogl A. Optimization of surgery sequencing and scheduling decisions under uncertainty. Health Care Manag. Sci. 2007 Feb;10(1) doi: 10.1007/s10729-006-9005-4. 18/11/2015-13-24. [DOI] [PubMed] [Google Scholar]
- 7.Fordyce A. 2007. Operating Theatre Efficiency Improvements Using Operations Management Science.http://www.institute.nhs.uk/index.php?option=com_mtree&task=viewlink&link_id=2983&Itemid=301 Available at: (accessed 25.10.15) [Google Scholar]
- 8.Kasivisvanathan R., Chekari A. 2013. 7 Ways to Improve Theatre Efficiency.http://www.ldfa.co.uk/articles/2013/12/2/7-ways-to-improve-theatre-efficiency Available at: (accessed 25.10.15) [Google Scholar]
- 9.Department of Health . 2015. Hospital Productivity Report Shows How NHS Can Make Large Savings.https://www.gov.uk/government/news/hospital-productivity-report-shows-how-nhs-can-make-large-savings Available at: (accessed 25.10.15) [Google Scholar]
- 10.Gamble M. 2013. 6 Cornerstones of Operating Room Efficiency: Best Practices for Each.http://www.beckershospitalreview.com/or-efficiencies/6-cornerstones-of-operating-room-efficiency-best-practices-for-each.html Available at: (accessed 25.10.15) [Google Scholar]
- 11.Finance & NHS Directorate, Procurement, Investment & Commercial Division (PICD) 2015. Procurement Transparency.https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/417554/Procurement_Transp_2015-16_acc.pdf Available at: (accessed 25.10.15) [Google Scholar]
- 12.Department of Health . 2013. Better Procurement Better Value Better Care: a Procurement Development Programme for the NHS.https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/226835/procurement_development_programme_for_NHS.pdf Available at: (accessed 25.10.15) [Google Scholar]
- 13.Keller A., Ashrafi A., Ali A. Causes of elective surgery cancellation and theatre throughput efficiency in an Australian urology unit. F1000 Res. 2014 Aug 19;3(197) doi: 10.12688/f1000research.4824.1. 25/10/2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGowan J., Truwit J., Cipriano Pea. Operating room efficiency and hospital capacity: factors affecting operating room use during maximum hospital census. J. Am. Coll. Surg. 2007 May;204(5) doi: 10.1016/j.jamcollsurg.2007.01.052. 25/10/2015-865-71. [DOI] [PubMed] [Google Scholar]
- 15.Overdyk F., Harvey S., Fishman R., Shippey F. Successful strategies for improving operating room efficiency at academic institutions. Anesth. Anal. 1998;86(4) doi: 10.1097/00000539-199804000-00039. 25/10/2015-896-906. [DOI] [PubMed] [Google Scholar]
- 16.Sandberg W., Daily B., Egan Mea. Deliberate perioperative systems design improves operating room throughput. Anesthesiology. 2005 Aug;103(2) doi: 10.1097/00000542-200508000-00025. 10/25/2015-406-18. [DOI] [PubMed] [Google Scholar]
- 17.Curtis L. Kent: Personal Social Services Research Unit; 2014. Hospital-based Health Care Staff. Unit Costs of Health & Social Care 2014; pp. 231–259. [Google Scholar]
- 18.Ciechanowicz S., Wilson N. Delays to operating theatre lists: observations from a UK Centre. Internet J. Health. 2010;13(1):31/10/2015. [Google Scholar]
- 19.Wright J., Ann Roche R., Khoury A. Improving on-time surgical starts in an operating room. Can. J. Surg. 2010 Jun;53(3) 31/10/2015-167-170. [PMC free article] [PubMed] [Google Scholar]
- 20.Weinbroum A., Ekstein P., Ezri T. Efficiency of the operating room suite. Am. J. Surg. 2003 Mar;185(3) doi: 10.1016/s0002-9610(02)01362-4. 31/10/2015-244-50. [DOI] [PubMed] [Google Scholar]
- 21.Saha P., Pinjani A., Al-Shabibi N., Madari S., Ruston J., Magos A. Why we are wasting time in the operating theatre? Int. J. Health Plan. Manag. 2009 July–Sept;24(3) doi: 10.1002/hpm.966. 31/10/2015-225-32. [DOI] [PubMed] [Google Scholar]
- 22.Ricketts D., Hartley J., Patterson M., Harries W., Hitchin D. An orthopaedic theatre timings survey. Ann. R. Coll. Surg. Engl. 1994 May;76(3) 31/10/2015-200-204. [PMC free article] [PubMed] [Google Scholar]
- 23.Ricci W., Brandt A., McAndrew C., Gardner M. Factors affecting delay to surgery and length of stay for patients with hip fracture. J. Orthop. Trauma. 2015 Mar;29(3) doi: 10.1097/BOT.0000000000000221. 31/10/2015-e109-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schneider C., Tyler L., Scull E., Pryle B., Barr H. A case-control study investigating factors of preoperative delay in emergency laparotomy. Int. J. Surg. 2015 Oct;22 doi: 10.1016/j.ijsu.2015.08.028. 31/10/2015-131-5. [DOI] [PubMed] [Google Scholar]
- 25.Epstein R., Dexter F. Uncertainty in knowing the operating rooms in which cases were performed has little effect on operating room allocations or efficiency. Anesth. Analg. 2002 Dec;95(6) doi: 10.1097/00000539-200212000-00048. 1/11/2015-1726-30. [DOI] [PubMed] [Google Scholar]
- 26.Dexter F., Macario A., Qian F., Traub R. Forecasting surgical groups' total hours of elective cases for allocation of block time: application of time series analysis to operating room management. Anesthesiology. 1999 Nov;91(5) doi: 10.1097/00000542-199911000-00044. 1/11/2015. [DOI] [PubMed] [Google Scholar]
- 27.Vitez T., Macario A. Setting performance standards for an anesthesia department. J. Clin. Anesth. 1998 Mar;10(2):166–175. doi: 10.1016/s0952-8180(97)00228-6. 1/11/2015-166-75. [DOI] [PubMed] [Google Scholar]
- 28.Collar R., Shuman A., Feiner S. Lean management in academic surgery. J. Am. Coll. Surg. 2012 Jun;214(6) doi: 10.1016/j.jamcollsurg.2012.03.002. 1/11/2015-928-36. [DOI] [PubMed] [Google Scholar]
- 29.Vigoda M., Gayer S., Tutiven J. Targeting operating room inefficiencies in the complex management of vision-threatening diseases in children. Arch. Ophthalmol. 2008;126(9) doi: 10.1001/archopht.126.9.1241. 1/11/2015-1241-43. [DOI] [PubMed] [Google Scholar]
- 30.Cendán J., Good M. Interdisciplinary work flow assessment and redesign decreases operating room turnover time and allows for additional caseload. Arch. Surg. 2006;141(1) doi: 10.1001/archsurg.141.1.65. 1/11/2015-65-69. [DOI] [PubMed] [Google Scholar]
- 31.Mangum S., Cutler K. Increased efficiency through OR redesign and process simplification. AORN J. 2002 Dec;76(6) doi: 10.1016/s0001-2092(06)61006-5. 1/11/2015-1041-6. [DOI] [PubMed] [Google Scholar]
- 32.Harders M., Malangoni M., Weight S., Sidhu T. Improving operating room efficiency through process redesign. Surgery. 2006 Oct;140(4) doi: 10.1016/j.surg.2006.06.018. 1/11/2015-509-14. [DOI] [PubMed] [Google Scholar]
- 33.Friedman D., Sokal S., Chang Y., Berger D. Increasing operating room efficiency through parallel processing. Ann. Surg. 2006 Jan;243(1) doi: 10.1097/01.sla.0000193600.97748.b1. 1/11/2015-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dexter F., Traub R. How to schedule elective surgical cases into specific operating rooms to maximize the efficiency of use of operating room time. Anesth. Analg. 2002 Apr;94(4) doi: 10.1097/00000539-200204000-00030. 1/11/2015-933-42. [DOI] [PubMed] [Google Scholar]
- 35.McIntosh C., Dexter F., Epstein R. The impact of service-specific staffing, case scheduling, turnovers, and first-case starts on anesthesia group and operating room productivity: a tutorial using data from an Australian hospital. Anesth. Analg. 2006 Dec;103(6) doi: 10.1213/01.ane.0000244535.54710.28. 1/11/2015-1499-516. [DOI] [PubMed] [Google Scholar]
- 36.Epstein R., Dexter F. Uncertainty in knowing the operating rooms in which cases were performed has little effect on operating room allocations or efficiency. Anesth. Analg. 2002 Dec;95(6):1726–1730. doi: 10.1097/00000539-200212000-00048. 1/11/2015-1726-30. [DOI] [PubMed] [Google Scholar]
- 37.Sulecki L., Dexter F., Zura A., Saager L., Epstein R. Lack of value of scheduling processes to move cases from a heavily used main campus to other facilities within a health care system. Anesth. Analg. 2012 Aug;115(2) doi: 10.1213/ANE.0b013e3182575e05. 1/11/2015-395-401. [DOI] [PubMed] [Google Scholar]
- 38.Hanss R., Buttgereit B., Tonner P. Overlapping induction of anesthesia: an analysis of benefits and costs. Anesthesiology. 2005 Aug;103(2) doi: 10.1097/00000542-200508000-00023. 1/11/2015-391-400. [DOI] [PubMed] [Google Scholar]
- 39.National Health Service. NHS Improving Quality Publications. Available from: http://www.nhsiq.nhs.uk/resource-search/publications.aspx (accessed 23.01.16).