Abstract
Objectives
To explore attitudes of Swiss older adults towards personal genomics (PG).
Methods
Using an anonymized voluntary paper-and-pencil survey, data were collected from 151 men and women aged 60–89 years attending the Seniorenuniversität Zurich, Switzerland (Seniors' University). Analyses were conducted using descriptive and inferential statistics.
Results
One third of the respondents were aware of PG, and more than half indicated interest in undergoing PG testing. The primary motivation provided was respondents' interest in finding out about their own disease risk, followed by willingness to contribute to scientific research. Forty-four percent were not interested in undergoing testing because results might be worrisome, or due to concerns about the validity of the results. Only a minority of respondents mentioned privacy-related concerns. Further, 66% were interested in undergoing clinic-based PG motivated by the opportunity to contribute to scientific research (78%) and 75% of all study participants indicated strong preferences to donate genomic data to public research institutions.
Conclusion
This study indicates a relatively positive overall attitude towards personal genomic testing among older Swiss adults, a group not typically represented in surveys about personal genomics. Genomic data of older adults can be highly relevant to late life health and maintenance of quality of life. In addition they can be an invaluable source for better understanding of longevity, health and disease. Understanding the attitudes of this population towards genomic analyses, although important, remains under-examined.
Keywords: Personal genomics, Attitudes of older adults, Ethics, Personalized medicine, Privacy, Research participation
1. Introduction
The emergence of increasingly inexpensive genome sequencing technologies has increased our potential to identify genetic components of health and disease, thereby contributing to progress towards more individualized, predictive, preventive and precise medicine (Van El et al., 2013). To facilitate this development, genome-wide association and gene–environment interaction studies have become valuable resources for investigating the genetic basis of disease.
Capitalizing on hopes and expectations regarding personalized medicine, commercial companies began offering large-scale personal genomic testing and disease-risk profiling outside clinical settings in 2007. Such companies appeared in many countries, operating via online interfaces and initially using a direct-to-consumer approach (DTC) whereby users order tests online and receive personal predictive risk assessments for a variety of diseases directly, without the mediation of a health professional (Vayena and Prainsack, 2013). However, the analytical validity, clinical utility of such tests including the appropriate involvement of health care providers have been highly contested, and significant debate has surrounded these companies ever since their first emergence (Bloss et al., 2013, Vayena et al., 2014a, Vayena, 2014). The leading company in this area remains 23andme, claiming to have one million genotypes in their database (23andme, 2015). Since November 2013, at the request of the US FDA, the company can offer only limited health risk information depending on whether the FDA has been provided with sufficient evidence of the link between a variant and a condition. In the UK, the same company offers a wider range of health risk information as the UK regulators have not stepped into controlling the services.
Expert views differ over whether this type of genomic risk information has any value for disease prevention or would only inappropriately burden individuals and the healthcare system (Bloss et al., 2013 & McGowan et al., 2014). Systematic evidence of the impact of personal genomic information on behavior and health outcomes remains limited. Overall, early findings indicate increased physician utilization by DTC-PG customers (Bloss et al., 2014). Healthier lifestyle changes on the basis of genomic results was only reported by Egglestone et al., (2013), while others observed no changes or even decreased self-efficacy and control over one's health (Bloss et al., 2013, Boeldt et al., 2015). Further, differences in anxiety levels or after test distress in DTC-PG users were reported as non-significant and correct interpretation and understanding of PG findings varies with demographic characteristics, level of education and numeracy, genetic knowledge and the format in which the information is presented (Ostergren et al., 2015, Schmidlen et al., 2015). Most findings come from early adopters of DTC-PG. We are still lacking conclusive evidence of how lay people receiving complex genomic information would react to it, given the limited genomic literacy in the general public (Carere et al., 2015, Critchley et al., 2015a, Critchley et al., 2015b, Boeldt et al., 2015, Meisel et al., 2015, Ostergren et al., 2015, Schmidlen et al., 2015, Gigerenzer et al., 2007, Gigerenzer and Muir Gray, 2011, Wasson et al., 2013).
To date a number of studies have sought to improve understanding of the attitudes of people who have accessed their genomic data, or those willing to do so (Carere et al., 2015, Roberts and Ostergren, 2013, Vayena et al., 2012, Vayena et al., 2014a). While patterns have begun to emerge, empirical data remain limited (Vayena et al., 2014a): findings indicate that the general public's awareness about genomics is increasing, even though the number of actual test takers remains low (Almeling and Gadarian, 2014, Carere et al., 2015, Critchley et al., 2015a, Critchley et al., 2015b, Hall et al., 2012; Schmidlen et al., 2015). The most commonly reported motives for undergoing personal genomic testing outside the clinical context are to obtain information about personal traits; to explore genetic makeup and ancestry; or wanting to learn about individual genetic risk factors (Cherkas et al., 2010, Gollust et al., 2012, McGowan et al., 2010, Vayena et al., 2012, Vayena et al., 2014a). Other reasons include the use of genetic information for disease prevention (Rahm et al., 2012); planning to adopt healthier lifestyles in cases of higher-than-average risk (Cherkas et al., 2010); explanation for the cause of a current health condition (Meisel et al., 2015) and taking personal responsibility for future health (McGowan et al., 2010). An additional reason has been the opportunity to contribute to research, despite privacy and confidentiality concerns being reported as obstacles to the donation of data (Brown Trinidad et al., 2010, Critchley et al., 2015a, Critchley et al., 2015b).One study found people accepting trade-offs between privacy and the utility of research participation for the common good (McGuire et al., 2009, Oliver et al., 2012). However, conditions for such trade-offs or expectations associated with utility are still an underexplored area. Since we anticipate an increase in the use of genomic data within and beyond the clinical setting, it is important to fill gaps in empirical data on public attitudes concerning these issues.
Following up on previous work we did on PG attitudes in Switzerland, this study focuses on investigating perspectives of older Swiss adults. In most western societies the older adult population is the fastest growing segment; medical advances and the baby boom between 1955 and 1964 have resulted in a current population in which 1/6 of people are 65 or older, with a steadily increasing percentage aged 80 or older (BFS 2013). Compared to the general population, older adults are more vulnerable to physical changes, decreasing mobility, chronic illness, loss of support systems, and changes in cognitive ability, particularly in advanced old age. However, they are also characterized by large inter-individual differences in level, rate and direction of change of these characteristics. In the context of genetic research, given their long life history of health and disease, they also represent an extremely rich source of insight into genetic associations with human longevity, as well as genetic associations leading to individual fitness (van den Akker et al., 2015, Tan et al., 2006).
In general, older adults are frequently under-recruited or excluded from biomedical and pharmaceutical research, although most drugs and treatments under development are more likely to be used in this age group. The elderly perspective is also missing from the discussion of personal genomics, since studies have mainly focused on younger populations with concerns corresponding to earlier phases in life where health issues are typically a concern of the future, as opposed to the more current concern of many older adults (Smith and Freund, 2002, Wurm et al., 2009). This project aimed to start filling the gap in our knowledge regarding attitudes of older adults towards human genomics. More specifically, we wanted to explore whether this age group is aware of developments within genetic testing, in particular personal genomics; their interest in undergoing such testing themselves; the motivational factors contributing to their willingness or lack thereof; how they view access modalities to such data; and their concerns and expectations in relation to participating in genomics research. To our knowledge this is the first study of this kind.
2. Method
We conducted an anonymized voluntary self-completion survey in two sessions on 19 November 2013 and 6 March 2014, before lectures of the Seniors' University Program at the University of Zurich with approximately 500 older adults attending on the first date, and 300 on the second date. After a short presentation of the study purpose, we showed a multimedia file including a soundless black and white animation and text describing the customer journey of internet-based personal genomic services. The file was developed in collaboration with the IT support group of the University of Zurich, and its content, design and presentation were reviewed by experts in genetics, psychology, social science, medicine, law, ethics, and information technology. The same multimedia file was used in a study we conducted with young adults and results of which have been published (Vayena et al., 2014a). After the presentation of the movie, the audience was invited to ask questions of clarification about the movie and the project. They were also invited to pick up a paper-pencil questionnaire, including a pre-paid return envelope, which was designed based on our previous study of similar research questions in young adults (Vayena et al., 2012, Vayena et al., 2014a), and after reviewing similar questionnaires in other published studies (Vernez et al., 2013, Wilde et al., 2011, Gollust et al., 2012). Permission to conduct this study was received by the Research Ethics Committee of the Canton of Zurich.
The questionnaire included 31 multiple-choice and 7-point Likert scale questions and was pretested among peers and five older adults unrelated to the study. Questions were designed to capture awareness about personal genomics services, motivation for testing, and concerns about genomic results. Moreover, a number of questions were included that explored attitudes towards sharing genomic data and research participation in genomic research studies. Since the majority of respondents were unlikely to have had experience with personal genomic testing, we also explored the motives and concerns of hypothetical participation in testing. Demographic data were collected including gender, age, education, health concerns, offspring, importance of religion, and internet usage.
Statistical analysis was carried out using SPSS Statistics 20.0. We conducted Pearson's chi-squared test and, where required, Fisher's exact test in order to establish associations between attitudes to personal genomics and the demographic variables. Due to our small sample, the 7-point-Likert scale scores were split into groups for comparison of different measures by pooling answer categories 1–3 and 5–7. The neutral category, 4, was excluded. Again, analysis was conducted and analyzed using Pearson's chi-squared or Fisher's exact test. Significance was accepted at a p < 0.05 level. Participants' answers to open-ended questions were reported in free text fields for “other reasons” or additional comments. These were post-coded into categories and analyzed qualitatively or saved as illustrating quotations.
3. Results
In total, 151 respondents participated in the survey, a response rate of 19% based on the total number of attendees at the lecture. General sample characteristics are displayed in Table 1. Gender was fairly equally distributed and the mean age reported was 76 years, with a range between 60 and 89 years. The level of education was above average, and 92% of our sample reported regular internet use. Participants expressed moderate concern about their own health, with 4.89 on a 7-point Likert-scale, and one third reported being affected by a serious disease either personally or within their family. The importance of religion in daily life seemed less prominent. One third of participants reported having heard of personal genomic testing. Pearson's chi-squared test revealed that the oldest age group (born 1925–1935) was less likely to be aware of DTC-PG (χ2 (1,n = 84) = 6.025, p = 0.024), and also reported less internet use ( χ2 (1,-n = 84) = 19.704, p = 0.0.
Table 1.
Demographics.
| Sample characteristic | N | % | |
| Sample size | 151 | ||
| Age | 76 years | SD = 6.052 | |
| Gender | Male | 82 | 54.3% |
| Female | 69 | 45.7% | |
| Children/grandchildren | Yes | 126 | 83.4% |
| No | 25 | 16.6% | |
| Disease in family | Yes | 48 | 31.8% |
| No | 99 | 65.6% | |
| Internet | Yes | 139 | 92.1% |
| No | 12 | 7.9% | |
| Education | Secondary school | 7 | 4.6% |
| Vocational education | 67 | 44.4% | |
| High School | 28 | 18.5% | |
| University degree | 49 | 32.5% | |
| Health | Concerned | 104 | 68.9% |
| Not concerned | 19 | 12.6% | |
| Religion | Religious | 38 | 25.2% |
| Not religious | 88 | 58.3% |
3.1. Direct-to-consumer personal genomics (DTC-PG): motivation to undergo testing
Only one respondent had personal experience with DTC personal genomics; this person had participated in a research project. Of the remaining respondents, 56% were interested in hypothetically undergoing DTC-PG. The primary motivation for considering testing was interest in receiving information about one's personal disease risk, followed by the wish to contribute to scientific research (Table 2). The exploration of demographic characteristics and the willingness to undergo testing revealed that people concerned about their health were more likely to consider DTC-GT (χ2 (1,n = 122) = 5.348, p = 0.021).
Table 2.
Ranked reasons for considering undergoing DTC-GT.
| Response (N = 84) | No of responses | [%] |
|---|---|---|
| I would like to know if I am at risk of certain disease | 59 | 70.2 |
| I would like to contribute my genetic data to scientific research | 53 | 63.1 |
| I would like to know my sensitivity to certain medication | 48 | 57.1 |
| I would like to find out about my genetic ancestry | 46 | 54.8 |
| I would like to know the risk that I have passed a disease predisposition | ||
| on to my children | 45 | 53.6 |
| I would like to find out about my genetic traits | 36 | 42.9 |
| I was curious about how such a test works | 33 | 39.3 |
| I am interested in genetics in general | 30 | 35.7 |
| If I were able to buy the test at low cost | 29 | 34.5 |
| Just for fun | 5 | 6 |
A χ2-test including all demographic characteristics was conducted and revealed the following results: People without children or grandchildren are less concerned about passing on predispositions (χ2 (1,n = 84) = 16.154, p = 0.000); People without children or grandchildren are less likely to want to find out about their genetic ancestry (χ2 (1,n = 84) = 8.201, p = 0.004); People with sickness in family are more likely to prefer having health professional supervision (χ2 (1,n = 82) = 4.353, p = 0.037; Comparing the two extreme groups in terms of age, the oldest group (1935–1925) was less likely to prefer medical professional supervision (χ2 (1,n = 50) = 6.637, p = 0.01).
3.2. Reasons for not being interested in DTC-PG
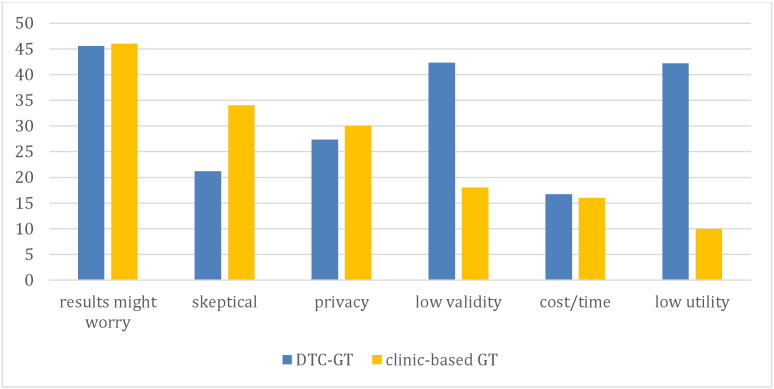
Those respondents who were not interested in undergoing DTC-PG (44%) would refrain mainly because of concerns that the results might worry them (45.5%) and concerns about the validity of the results (42.4%, see also Table 3).
Table 3.
Ranked reasons for not being interested DTC-PG.
| Response (N = 66) | No of responses | [%] |
|---|---|---|
| I am concerned that the results will worry me | 30 | 45.5 |
| I do not think the test results are valid | 28 | 42.4 |
| I do not see any utility in such tests/I am not interested in my genetic profile | 28 | 42.4 |
| I am concerned about the privacy of my data | 18 | 27.3 |
| I am skeptical about genetic testing in general | 14 | 21.2 |
| Cost is an obstacle to undergo testing | 11 | 16.7 |
| The test is not advised by a doctor | 11 | 16.7 |
A χ2-test including the demographic variables was conducted and revealed the following results: Females see costs as an obstacle (χ2 (1,n = 66) = 3.960, p = 0.047); People with sickness in family are less likely to report “no utility” (χ2 (1,n = 64) = 7.721, p = 0.005) and would not undergo testing since it is not prescribed by the doctor (χ2 (1,n = 64) = 5.217, p = 0.032); People in the oldest age group are less concerned about privacy (χ2 (1,n = 47) = 5.631, p = 0.02) and religious people refrain since it is not prescribed by the doctor (χ2 (1,n = 53) = 6.280, p = 0.019).
3.3. Attitudes towards online PG vs clinic-based PG for research purposes
In contrast to 56% interested in an online PG test, 66% of the respondents were interested in participating in a clinic-based personal genomic test for research purposes, with those concerned about their health more likely to be interested (χ2 (1,n = 122) = 4.419, p = 0.036). Overall, the main reason for interest was the opportunity to contribute to scientific research (78%) and second, to help increase the validity of the test (69%). More specifically, participants who had experienced disease personally or in their family were motivated by their interest in the development of new therapies (χ2 (1,n = 97) = 7.904, p = 0.005), as well as improving the validity of available personal genomic tests (χ2 (1,n = 97) = 5.489, p = 0.019). Participants with lower levels of education were less interested in developing therapies for affected family members or themselves (χ2 (1,n = 100) = 6.354, p = 0.012), and also reported lower interest in genetics generally (χ2 (1,n = 100) = 6.135, p = 0.013).
Of those respondents expressing interest in undergoing clinic-based PG for research purposes, the vast majority reported an interest in receiving back their results, with 60% wanting unrestricted access to results and 30% wanting only to be informed about curable diseases. Only 4 respondents chose not to receive any results, because they doubted the validity of the results. An additional reason for refusal provided in the open-ended questions was the potential burden associated with more information about disease risk.
A χ2-test including the demographic variables was conducted and revealed the following results: people aware about genetic testing were less concerned about privacy (χ2 (1,n = 47) = 4.362, p = 0.037). The same holds true for people with sickness in family (χ2 (1,n = 47) = p = 0.040). People without children or grandchildren reported quality concerns (χ2 (1,n = 47) = , p = 0.029).
One third of all respondents were not interested in participating in a clinical study overall worry about possible test results was cited as the key reason. The second most common reason was skepticism about genetic testing in general (see Table 4).
Table 4.
Ranked reasons for not considering a clinic-based PG for research purposes.
| Response (N = 50) | No of responses | [%] |
|---|---|---|
| I am concerned that the results will worry me | 23 | 46 |
| I am skeptical about genetic testing | 17 | 34 |
| I am concerned about the privacy of my data | 15 | 30 |
| I question the validity of the test | 9 | 18 |
| Time would be an obstacle to participating | 8 | 16 |
| I am not interested in genetics at all | 5 | 10 |
Finally, Fig. 1 illustrates reasons for not interested in undergoing either DTC-PG or clinic-based PG for research purposes, indicating a common concern about the nature of the results. Low utility and low validity were only attributed to privately and self-administered DTC-PG.
Fig. 1.
Comparison of reasons for not undergoing DTC-PG or clinic-based PG for research purposes. To enable comparison and adjust for varying total numbers, data have been normalized. Categories have been grouped and slightly renamed.
3.4. Donating genomic data to research institutions
Finally, 75% of all respondents indicated strong preferences to contribute their genomic data to public research institutions such as universities or university hospitals as opposed to private institutions (15%). Forty-five percent would also support contributing data to private but not-for-profit institutions.
4. Discussion
4.1. Awareness of personal genomic testing
Some researchers have reported declining awareness of personal genomic testing with increasing age. Additionally, psychological and consumer behavior studies link increasing age with decreasing capacity for processing information from media sources (Ostergren et al., 2015, Kolor et al., 2012, Langford et al., 2012), which might lead to the reported lower awareness of PG in older people. Since some of the personal genomics services are online, it is also likely that the low internet use, especially among the oldest study participants of our group, might diminish awareness of online genomic services. However, a recent survey of internet use in older Swiss adults indicated that 68% of those aged 60–69 and 40.6% of those aged 70 years and older reported using the internet to some degree (Schelling and Seifert, 2010).
In the present study, one third of participants were familiar with the concept of personal genomics, a proportion that can be classified as moderate compared to other studies involving young and middle-aged adults (Cherkas et al., 2010, Finney Rutten et al., 2012, Hall et al., 2012, Kolor et al., 2012, Ortiz et al., 2011). This finding is likely to be related to the increasing media attention and current public debate around a revision of the Swiss laws on genetic testing. In addition, one of the senior citizens' lectures used for recruitment was on innovations in medicine, which might imply pre-existing interest in the medical field within our sample.
4.2. Reasons for DTC-PG-testing
Only one person in the current study reported personal experience with genetic testing in the context of a genetic research study. This is in line with previous findings of a relatively low participation rate in personal genomic testing in other age groups (Kolor et al., 2012, Ortiz et al., 2011). More than half of our respondents expressed interest to participate in a hypothetical PG-study. Other studies characterized individuals with prior personal experience of a genetic disease in themselves or within their family as particularly open-minded towards genetic testing (Kettis-Lindblad et al., 2005); our findings, however, indicate more critical attitude to personal genomics within this group. Those with a family history of disease were particularly likely to question the utility of this type of test, and indicated that they would not undergo testing without involving a health professional.
Respondents were interested in access to information on personal disease risk and the opportunity to contribute to scientific research. Those respondents who were concerned about their health in general expressed a stronger interest in undergoing testing. Similarly, in the case of a clinic-based PG for research purposes, an additional motive for participation was to help increase the validity of the test. Other studies have reported analogous findings (Goldsmith and Jackson, 2012, Vayena, 2014): the moral duty of contributing — for reasons of reciprocity — to the societal good; altruism; and self-interest in medical treatment have all been described as common motivations to participate in genetic research for elderly groups (Frazier et al., 2006, Merz et al., 2002). Generally, altruism involves an act in which benefits are attributed to others rather than the actor; in genetic research, the recipient (a research institution), is considered to reciprocate the gift by contributing towards publicly accessible medical advances; therefore, a third party, society, eventually receives the benefits of the individual's altruistic act (Harmon and Chen, 2012). Erikson and Kivnick (1986) considered this type of altruism ‘generativity’: an increasing concern, with age, to guide and care for the next generation, coupled with greater willingness to provide positive opportunities for the next generation. Consequently, participation of the elderly may be seen by older adults themselves as a reciprocal act, whereby the older adult experiences personal benefits from participation, including increased or maintained life satisfaction, greater confidence and self-esteem, as well feeling more socially integrated through having contributed personally to the common good and/or the next generation (Harmon and Chen, 2012).
4.3. Reasons for not being interested in PG-testing
The primary reason for refraining from PG-testing was the possible implications of the results, which might cause worry (Bloss et al., 2010, Gollust et al., 2012, McGuire et al., 2009, Rahm et al., 2012, Vayena et al., 2014a). This finding relates to a rather prominent point in the debate about PG, namely the concern about whether people are able to understand the nature of genetic data and interpret predictive results correctly. Studies of investigating this question in the context of genetic literacy have had contradictory results. Some found that people lacked sophisticated knowledge about genetics and genomics while holding misconceptions about the value and limitations of genetic tests (Boeldt et al., 2015, Schmidlen et al., 2015, Hahn et al., 2010, Hahn et al., 2010, Rose et al., 2005). Other studies found that participants have realistic expectations and understand the low predictive power of results (McGowan et al., 2010, McGuire et al., 2009, Meisel et al., 2015, Ostergren et al., 2015). It is therefore difficult to draw firm conclusions at this point about individual perceptions of actual test results. The risk of being surprised and unable to cope with probabilistic results might still occur in some instances, especially given the often observed limited ability of both doctors and patients to interpret probabilistic information about health risks correctly, even when those risks are unrelated to genetics (Boeldt et al., 2015, Carere et al., 2015, Dressler et al., 2014, Gigerenzer et al., 2007, Gigerenzer and Muir Gray, 2011, Kaye and Korf, 2013, Ostergren et al., 2015, Powell et al., 2012, Schmidlen et al., 2015). Those with a family history of disease were more likely to question the utility of this type of test, and indicated that they would not undergo testing without involving a health professional. Another interesting finding that emerged in the open questions was that some participants did not wish to be treated for illness after a certain stage; they were concerned, however, that having genetic information might lead to increased external pressure on them to undergo treatment despite their own wishes. Although the design of our study did not allow us to explore this further, we consider this an issue worthy of deeper investigation.
Given the prominence of privacy concerns in all discussions about genomic testing, privacy considerations were one of our possible reasons for not undergoing PG testing. Such concerns were very low among our respondents. A number of other studies have reported concerns about privacy, confidentiality of results and fear of discrimination as a key consideration in deciding whether or not to participate in genetic research (Critchley et al., 2015a, Critchley et al., 2015b, Vayena et al., 2014a, Goldsmith and Jackson, 2012, McGuire et al., 2009, Wilde et al., 2011). This is significantly different from our findings and should be explored in more detail. It is unclear whether lack of privacy concerns is due to a privacy knowledge gap or whether respondents in this study do not really consider genetic privacy an issue. Among the older participants in this study, privacy concerns were very rare, and diminished with increasing age. Given limited previous data on older adults' perception of privacy in the context of data sharing, we can only assume a number of reasons. First, many older adults might not be concerned about privacy because they are not affected by certain risks identified earlier: for example, they do not have employment concerns, they already have established (health) insurance plans, and they have already survived a substantial part of adult life. Second, in line with arguments relating to altruistic motives, older persons might consider the risk of diminished assurance of privacy due to data disclosure to be outweighed by the high potential benefits of scientific research (McGuire and Burke, 2008, Oliver et al., 2012, Vayena, 2014). Finally another reason that may potentially explain reduced privacy concerns, is the high level of privacy protection afforded to personal data in Switzerland (Vayena et al., 2014a). None of our respondents mentioned concerns about the privacy of their relatives in relation to their own genomic testing. A possible explanation could be low genomic literacy and limited understanding of the genetic privacy implications for relatives. The level of genomic literacy of this population and the perception of privacy risks need further exploration.
4.3.1. Comparison of DTC-PG and clinic-based PG
We compared participants' interest in undergoing DTC-PG and personal genomic testing in a clinical context for research purposes. According to Swiss law, for companies that operate from Switzerland, it is illegal to offer personal genomic services to consumers without physician prescription and counseling. It is not illegal for Swiss citizens to access such services online, but the ministry of health has issued advise against such online services. The genetic testing law is currently under revision, which includes relaxing some of these prohibitions, however, at the time of the survey no revision was effected. We were interested in exploring whether the context in which the genomic testing takes place is relevant in people's motivation or concerns. The comparison was most interesting in relation to the reasons for refraining from testing. As in the DTC-PG the primary reason was concerns that results may cause worry. Drawing on other findings from earlier studies, although in different age groups, we still observe that this concern persists as reasons of avoiding personal genomics irrespective of the context of testing. It is important to explore this sentiment towards genomic information in more depth. Is the underlying concern the result of a deterministic understanding of genomics, or is it a general attitude towards information with predictive value? Ultimately better understanding the reasons behind such concerns will also prove relevant for the design of genomic literacy activities.
4.3.2. Not-for profit vs for-profit
The vast majority of study participants indicated strong preference to donate data to public research institutions as opposed to private research institutions. Even though we did not further explore the underlying reasons for this preference, our hypothesis is that people trust not-for profit publicly funded organizations more for prioritizing the common good. Given the growing number of private for-profit companies operating in the space of genomic and personal data, it would be interesting to further explore such views also against people's broader notion of ownership and exploitation of genomic data.
4.4. Limitations of the present study
All participants in this study were recruited via the Seniorenuniversität Zurich, a continuing education program for seniors. These seniors are characterized by an above average level of education and high levels of social participation and engagement in physical, cultural and social activities. This profile implies that our sample represents a selected part of the aging population rather than being fully representative of the general population. The Seniorenuniversität itself claims that their members are ‘the pioneers of a new culture of aging’, and such a new culture is likely to involve higher levels of engagement in activities such as participating in research. Additionally, future generations of older adults will also include the so-called baby boom generation, with demographics more similar to the population in this survey.
The low response rate, 19%, may indicate a substantial group of older adults outside the study with a critical perspective towards genetics, with only those holding a sufficiently strong preexisting interest in genetics and genomics actually participating.
We approached this sample in two sessions of a lecture series and introduced the topic by showing an informational multimedia file. We offered the change to pose clarifying questions, but we did not assess the viewers' comprehension of the video. The first time we approached the older adults was before a lecture on new developments in cardiology, a theme closely related to medical issues. This could imply an a priori increased interest in and awareness of new advances in medicine. Another limitation of the study is that due to the limited number of actual test takers in this age group, we investigated a hypothetical scenario by asking participants to imagine whether they would participate in genomic testing, and assessing their motivation for or against such participation. As our participants were aware of the hypothetical nature of this scenario, it is possible that motivational responses differed from those in a real-world test taking situation: the survey respondents might not have been as emotionally invested in the overall topic and in their decision as participants in a real-life personal genomic test.
Despite the reported limitations, this study provides a first descriptive approach to unveiling attitudes and motives relating to personal genomics in later adulthood—a source of information largely untapped, but one that is likely to inform the current debate and approaches to policy making.
4.5. Outlook and conclusion
How to harness people's willingness to engage with their genomic data and contribute to research, while making sure they are not exploited and their individual rights are not being violated, remains a key challenge. As PG is a relatively new development we are only at the beginning of the debate about necessary measures, for example, at the regulatory level; how to engage the broader public in the debate; and ultimately how to protect individual rights, like privacy and confidentiality, while avoiding undue paternalism. Although these are global developments, policies tend to be developed and implemented at the national level and therefore they need to be responsive to different public perceptions about genomics, public trust in scientific and medical research, the health care systems, as well as different regulatory regimes.
This exploratory study shows that older Western European adults of higher educational level and with familiarity with online technologies are generally interested in personal genomics. The participants were motivated by the possibility to participate in research and interest in one's actual and future health. This population is of particular importance for genomic studies. Genomic data from this population can contribute to better understanding of longevity, gene–environment interactions and wellbeing. In addition, as this segment of the population is rapidly growing, more thought should be given on how to involve this group in genomic research. If that were to be the case, it is imperative to understand the attitudes, preferences and concerns of this population group in relation to genomic data. Such an understanding is crucial for developing appropriate policies and practices in relation to recruitment, informed consent and privacy-setting options relevant to personal genomics. We hope that our exploratory findings will help set a broader research agenda for genomics and senior adults.
Acknowledgments
We would like to thank the Seniorenuniversität (http://www.seniorenuni.uzh.ch/index.html) for allowing us to conduct this study. We are grateful to Professor Martin Richards for very helpful comments on an early draft of the manuscript and to Christian Ineichen for reviewing the statistical analysis.
References
- Almeling R., Gadarian S. Public opinion on policy issues in genetics and genomics. GIM. 2014:491–494. doi: 10.1038/gim.2013.175. [DOI] [PubMed] [Google Scholar]
- Bloss C.S., Ornowski L., Silver E., Cargill M., Vanier V., Schork N.J., Topol E.J. Consumer perceptions of direct-to-consumer personalized genomic risk assessments. Genet. Med. 2010;12(9):556–566. doi: 10.1097/GIM.0b013e3181eb51c6. [DOI] [PubMed] [Google Scholar]
- Bloss C.S., Wineinger N.E., Darst B.F., Schork N.J., Topol E.J. Impact of direct-to-consumer genomic testing at long term follow-up. J. Med. Genet. 2013;50(6):393–400. doi: 10.1136/jmedgenet-2012-101207. (Jun) [DOI] [PubMed] [Google Scholar]
- Bloss C.S., Schork N.J., Topol E.J. Direct-to-consumer pharmacogenomic testing is associated with increased physician utilisation. J. Med. Genet. 2014;51(2):83–89. doi: 10.1136/jmedgenet-2013-101909. (Feb) [DOI] [PubMed] [Google Scholar]
- Boeldt D.L., Schork N.J., Topol E.J., Bloss C.S. Influence of individual differences in disease perception on consumer response to direct-to-consumer genomic testing. Clin. Genet. 2015;87(3):225–232. doi: 10.1111/cge.12419. (Mar) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown Trinidad S., Fullerton S.M., Bares J.M., Jarvik G.P., Larson E.B., Burke W. Genomic research and wide data sharing: views of prospective participant. GIM. 2010;12:486–495. doi: 10.1097/GIM.0b013e3181e38f9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bundesamt für Statistik Informationen aus der Demografie. Newsletter Nr.1. 2013. http://www.bfs.admin.ch/bfs/portal/de/index/news/publikationen.html?publicationID=3864 March 2010. Accessed 15 March 2014.
- Carere D.A., Kraft P., Kaphingst K.A., Roberts J.S., Green R.C. Consumers report lower confidence in their genetics knowledge following direct-to-consumer personal genomic testing. Genet. Med. 2015 doi: 10.1038/gim.2015.34. (Mar 26) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherkas L.F., Harris J.M., Levinson E., Spector T.D., Prainsack B. A survey of UK public interest in internet-based personal genome testing. PLoS One. 2010:5. doi: 10.1371/journal.pone.0013473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Critchley C., Nicol D., Otlowski M., Chalmers D. Public reaction to direct-to-consumer online genetic tests: Comparing attitudes, trust and intentions across commercial and conventional providers. Public Underst. Sci. 2015;24(6):731–750. doi: 10.1177/0963662513519937. (Aug) [DOI] [PubMed] [Google Scholar]
- Critchley C., Nicol D., Otlowski M. The impact of commercialisation and genetic data sharing arrangements on public trust and the intention to participate in biobank research. Public Health Genomics. 2015;18(3):160–172. doi: 10.1159/000375441. [DOI] [PubMed] [Google Scholar]
- Dressler L.G., Jones S.S., Markey J.M., Byerly K.W., Roberts M.C. Genomics education for the public: perspectives of genomic researchers and ELSI advisors. Genet. Test. Mol. Biomarkers. 2014;18(3):131–140. doi: 10.1089/gtmb.2013.0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egglestone C., Morris A., O′Brien A. Effect of direct-to-consumer genetic tests on health behaviour and anxiety: a survey of consumers and potential consumers. J. Genet. Couns. 2013;22:565–575. doi: 10.1007/s10897-013-9582-6. [DOI] [PubMed] [Google Scholar]
- Erikson J.M., Kivnick H.Q. Norton; NY: 1986. Vital Involvement in Old Age. [Google Scholar]
- Finney Rutten L.J., Gollust S.E., Naveed S., Moser R.P. Increasing public awareness of direct-to-consumer genetic tests: health care access, internet use, and population density correlates. J. Cancer Epidemiol. 2012 doi: 10.1155/2012/309109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier L., Calvin A.O., Mudd G.T., Cohen M.Z. Understanding of genetics among older adults. J. Nurs. Scholarsh. 2006;38:126–132. doi: 10.1111/j.1547-5069.2006.00089.x. [DOI] [PubMed] [Google Scholar]
- Gigerenzer G., Muir Gray J.A. MIT Press; Cambridge, MA: 2011. Better Doctors, Better Patients, Better Decisions: Envision Health Care 2, Better = 020. (Eds.) [Google Scholar]
- Gigerenzer G., Gaissmaier W., Kurz-Milcke E., Schwartz L.M., Woloshin S. Helping doctors and patients to make sense of health statistics. Psychol. Sci. Public Interest. 2007;8:53–96. doi: 10.1111/j.1539-6053.2008.00033.x. [DOI] [PubMed] [Google Scholar]
- Goldsmith L., Jackson L., O′Connor A., Skirton H. Direct-to-consumer genomic testing: a systematic review of the literature on user perspectives. Eur. J. Hum. Genet. 2012;20:811–816. doi: 10.1038/ejhg.2012.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gollust S.E., Gordon E.S., Zayac C., Griffin G., Christman M.F., Pyeritz R.E., Wawak L., Bernhardt B.A. Motivations and perceptions of early adopters of personalized genomics: perspectives from research participants. Public Health Genomics. 2012;15:22–30. doi: 10.1159/000327296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn S., Letvak S., Powell K., Christianson C., Wallace D., Speer M., Lietz P., Blanton S., Vance J., Pericak-Vance M., Henrich V.C. Genomedical connection: a communities' awareness and perceptions of genomic medicine. Public Health Genomics. 2010;13:63–71. doi: 10.1159/000218712. [DOI] [PubMed] [Google Scholar]
- Hall T.O., Renz A.D., Snapinn K.W., Bowen D.J., Edwards K.L. Awareness and uptake of direct-to-consumer genetic testing among cancer cases, their relatives, and controls: The Northwest Cancer Genetics Network. Genet. Test. Mol. Biomarkers. 2012;16:744–748. doi: 10.1089/gtmb.2011.0235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmon S.H.E., Chen K.H. Medical research data-sharing: the ‘public good’ and vulnerable groups. Med. Law Rev. 2012;20:516–539. doi: 10.1093/medlaw/fws006. [DOI] [PubMed] [Google Scholar]
- Kaye C., Korf B. Genetic literacy and competency. Pediatrics. 2013;132(Suppl. 3):S224–S230. doi: 10.1542/peds.2013-1032G. [DOI] [PubMed] [Google Scholar]
- Kettis-Lindblad A., Ring L., Viberth E., Hansson M.G. Genetic research and donation of tissue samples to biobanks. What do potential sample donors in the Swedish general public think? Eur. J. Pub. Health. 2005;16:433–440. doi: 10.1093/eurpub/cki198. [DOI] [PubMed] [Google Scholar]
- Kolor K., Duquette D., Zlot A., Foland J., Anderson B., Giles R., Wrathall J., Khoury M.J. Public awareness and use of direct-to-consumer personal genomic tests from four state population-based surveys, and implications for clinical and public health practice. Genet. Med. 2012;14:860–867. doi: 10.1038/gim.2012.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langford A.T., Resnicow K., Roberts J.S. Racial and ethnic differences in direct-to-consumer genetic test awareness in HINTS2007: socio-demographic and numeracy correlates. J. Genet. Couns. 2012;21:440–447. doi: 10.1007/s10897-011-9478-2. [DOI] [PubMed] [Google Scholar]
- McGowan M.L., Fishman J.R., Lambrix M.A. Personal genomics and individual identities: motivations and moral imperatives of early users. New Genet. Soc. 2010;29:261–290. doi: 10.1080/14636778.2010.507485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan M.L., Fishman J.R., Settersten R.A., Jr., Lambrix M.A., Juengst E.T. Gatekeepers or intermediaries? The role of clinicians in commercial genomic testing. PLoS ONE. 2014;9(9) doi: 10.1371/journal.pone.0108484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire A.L., Burke W. An unwelcome side effect of direct-to-consumer personal genome testing: raiding the medical commons. JAMA. 2008;300:2669–2671. doi: 10.1001/jama.2008.803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire A.L., Diaz C.M., Wang T., Hilsenbeck S.G. Social networkers' attitudes toward direct-to-consumer personal genome testing. Am. J. Bioeth. 2009;9:3–10. doi: 10.1080/15265160902928209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meisel S.F., Carere D.A., Wardle J., Kalia S.S., Moreno T.A., Mountain J.L., Roberts J.S., Green R.C., PGen Study Group Explaining, not just predicting, drives interest in personal genomics. Genome Med. 2015;7(1):74. doi: 10.1186/s13073–015-0188-5. (Aug 1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merz J.F., Magnus D., Cho M.K., Caplan A.L. Protecting subjects' interest in genetic research. Am. J. Hum. Genet. 2002;5:35–42. doi: 10.1086/339767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver J.M., Slashinski M.J., Wang T., Kelly P.A., Hilsenbeck S.G., McGuire A.L. Balancing the risks and benefits of genomic data sharing: genome research participants' perspectives. Public Health Genomics. 2012;15:106–114. doi: 10.1159/000334718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz A.P., López M., Flores L.T., Soto-Salgado M., Finney Rutten L.J., Serrano-Rodriguez R.A., Hesse B.W., Tortolero-Luna G. Awareness of direct-to-consumer genetic tests and use of genetic tests among Puerto Rican adults. Prev. Chronic Dis. 2011;8:A110. [PMC free article] [PubMed] [Google Scholar]
- Ostergren J.E., Gornick M.C., Carere D.A., Kalia S.S., Uhlmann W.R., Ruffin M.T., Mountain J.L., Green R.C., Roberts J.S. How well do customers of direct-to-consumer personal genomic testing services comprehend genetic test results? Findings from the impact of personal genomics study. Public Health Genomics. 2015;18(4):216–224. doi: 10.1159/000431250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell K.P., Christianson C.A., Cogswell W.A., Dave G., Verma A., Eubanks S., et al. Educational needs of primary care physicians regarding direct-to-consumer genetic testing. J. Genet. Couns. 2012;21(3):469–478. doi: 10.1007/s10897-011-9471-9. [DOI] [PubMed] [Google Scholar]
- Rahm A.K., Feigelson H.S., Wagner N., Le A.Q., Halterman E., Cornish N., Dearing J.W. Perception of direct-to-consumer genetic testing and direct-to-consumer advertising of genetic tests among members of a large managed care organization. J. Genet. Couns. 2012;21:448–456. doi: 10.1007/s10897-011-9477-3. [DOI] [PubMed] [Google Scholar]
- Roberts J.S., Ostergren J. direct-to-consumer genetic testing and personal genomics services: a review of recent empirical studies. Curr. Genet. Med. Rep. 2013;1:182–200. doi: 10.1007/s40142-013-0018-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose A.L., Peters N., Shea J.A., Armstrong K. Attitudes and misconceptions about predictive genetic testing for cancer risk. Community Genet. 2005;8:145–151. doi: 10.1159/000086757. [DOI] [PubMed] [Google Scholar]
- Schelling H.R., Seifert A. Zurich Open Repository and Archive, University of Zurich; 2010. Internet-Nutzung im Alter. Gründe der (Nicht-)Nutzung von Informations- und Kommunikationstechnologien (IKT) durch Menschen ab 65 Jahren in der Schweiz. [Google Scholar]
- Schmidlen T.J., Scheinfeldt L., Zhaoyang R., Kasper R., Sweet K., Gordon E.S., Keller M., Stack C., Gharani N., Daly M.B., Jarvis J., Christman M.F. Genetic knowledge among participants in the Coriell Personalized Medicine Collaborative. J. Genet. Couns. 2015 doi: 10.1007/s10897-015-9883-z. Aug 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J., Freund A. The dynamics of possible selves in very old age. J. Gerontol. B Psychol. Sci. Soc. Sci. 2002;57B:492–500. [Google Scholar]
- Tan Q., Christiansen L., Bathum L., Li L., Kruse T.A., Christensen K. Genetic association analysis of human longevity in cohort studies of elderly subjects: an example of the PON1 gene in the Danish 1905 birth cohort. Genetics. 2006;172:1821–1828. doi: 10.1534/genetics.105.050914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Akker E.B., Deelen J., Slagboom P.E., Beekman M. Exome and whole genome sequencing in aging and longevity. Adv. Exp. Med. Biol. 2015;847:127–139. doi: 10.1007/978–1-4939-2404-2_6. [DOI] [PubMed] [Google Scholar]
- Van El C.G., Cornel M.C., Borry P., Hastings R.J., Fellmann F., Hodgson S.V., Howard H.C., Cambon-Thomsen A., Knoppers B.M., Meijers-Heijboer H., Scheffer H., Tranebjaerg L., Dondorp W., de Wert G. Whole-genome sequencing in health care. On behalf of the ESHG Public and Professional Policy Committee. Eur. J. Hum. Genet. 2013;21:580–584. doi: 10.1038/ejhg.2013.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vayena E. Direct to consumer genomics on the scales of autonomy. J. Med. Ethics. 2014 doi: 10.1136/medethics-2014-102026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vayena E., Prainsack B. The challenge of personal genomics in Germany. Nat. Biotechnol. 2013;31:16–17. doi: 10.1038/nbt.2469. [DOI] [PubMed] [Google Scholar]
- Vayena E., Gourna E., Streuli J., Hafen E., Prainsack B. Experiences of early users of direct-to-consumer genomics in Switzerland: an exploratory study. Public Health Genomics. 2012;15:352–362. doi: 10.1159/000343792. [DOI] [PubMed] [Google Scholar]
- Vayena E., Ineichen C., Stoupka E., Hafen E. Playing a part in research? University students' attitudes to direct-to-consumer genomics. Public Health Genomics. 2014;17:158–168. doi: 10.1159/000360257. [DOI] [PubMed] [Google Scholar]
- Vernez S.L., Salari K., Ormond K.E., Lee S.S. Personal genome testing in medical education: student experiences with genotyping in the classroom. Genome Med. 2013;19:24. doi: 10.1186/gm428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasson K., Sanders T.N., Hogan N.S., Cherny S., Helzlsouer K.J. Primary care patients' views and decisions about, experience of and reactions to direct to consumer genetic testing: a longitudinal study. J. Community Genet. 2013;4:495–505. doi: 10.1007/s12687-013-0156-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilde A., Meiser B., Mitchell P.B., Hadzi-Pavlovic D., Schofield P.R. Community interest in predictive genetic testing for susceptibility to major depressive disorder in a large national sample. Psychol. Med. 2011;41:1605–1613. doi: 10.1017/S0033291710002394. [DOI] [PubMed] [Google Scholar]
- Wurm S., Lampert T., Menning S., Alter Gesundheit und Krankheit im. Robert-Koch Institute; Berlin: 2009. Subjektive Gesundheit; pp. 79–91. [Google Scholar]
Other sources:
- 23andme Power of one million. 2015. https://blog.23andme.com/news/one-in-a-million/ 18 June. Accessed.