Abstract
Background
The aims of the study were to compare the dimensions of oral-health-related quality-of-life measured by a generic health state measure, the EuroQol, and a specific oral health measure, the Oral Health Impact Profile.
Methods
Data were collected in 2001–02 from a random sample of South Australian dentists using mailed self-complete questionnaires. Dentists recorded the diagnosis of dental problems and provided patients with self-complete questionnaires to record the nature, severity and duration of symptoms using the EuroQol (EQ-5D+) and 14-item version of the Oral Health Impact Profile (OHIP-14) instruments.
Results
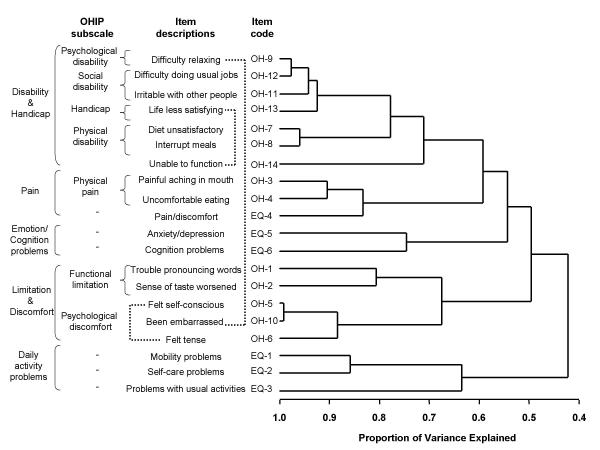
Data were available from 375 patients (response rate = 72%). The EuroQol items of mobility, self care and usual activities formed a separate cluster of variables, as did anxiety/depression and cognition, while pain clustered with items from the OHIP physical pain subscale. OHIP items tended to form clusters consistent with the subscales of social disability, physical disability, physical pain, functional limitation and psychological discomfort. The OHIP handicap items clustered between the OHIP social disability and physical disability subscales. The OHIP psychological disability items split between the social disability and psychological discomfort subscales.
Conclusions
The observed clusters of variables empirically supported most of the conceptual dimensions of the OHIP. Both instruments covered symptom experience of pain indicating overlapping domains. However there was partial separation of the generic and specific items, EuroQol covered daily activities such as self-care and usual activities and OHIP covered oral health-specific aspects of functional limitation and physical disability as well as psychological and social aspects of disability and handicap.
Background
Health-related quality-of-life is typically measured using disease-specific or generic measures, and both types may be used together in order to address both clinical and broader policy questions, and to detect unexpected differences [1]. Disease-specific measures are used when disease-related attributes need to be assessed and greater sensitivity to the clinical condition under consideration is required. Generic measures are used when the relevant variables are covered and when comparisons between different diseases are required.
The Oral Health Impact Profile (OHIP) measures people's perceptions of the social impact of oral disorders on their well-being [2]. The OHIP-49 contains 49 questions that capture seven conceptually formulated dimensions based on Locker's theoretical model of oral health [3] adapted from the WHO framework used to classify impairments, disabilities and handicaps [4], and the OHIP-14 was developed as a shorter version of the OHIP for settings where the full battery of 49 questions is inappropriate [5].
The EuroQol was developed as a standardised non-disease-specific instrument for describing and valuing health-related quality of life [6]. The EuroQol is intended to complement other forms of quality of life measures and it was purposefully developed to generate a generic index of health. Any classified health state can be valued using preferences elicited from a general population [6], and values can be modelled from such data sets [7]. The EuroQol is widely used internationally and reported to have adequate construct and convergent validity, but is highly skewed and has relatively poor sensitivity especially in relation to disease-based outcomes research [1].
In comparing generic and disease-specific measures it has been noted that possible explanations for the disease-specific measures being more sensitive to change could relate to the fact that patients perceive assessments of overall health as independent from condition-specific assessments which tend to focus on symptoms of the condition [8]. It has also been noted that disease-specific instruments may focus too narrowly on symptoms so that they fail to capture some broader domains included in generic instruments. It has also been suggested that even some generic instruments may not overlap but represent different domains of knowledge [9]. Oral health-related quality of life has been compared using specific and generic instruments. For example, a comparison between conventional and implant denture patients showed that the specific measure of oral health (OHIP-20) was better in the implant group but no significant differences between patient groups were found in the generic measure (SF-36) that was used [10]. Other studies have also concluded that oral specific measures such as OHIP will be of greater use in measuring outcomes of oral disorders than generic measures such as SF-36 because the majority of the SF-36 domains are not sensitive to changes in oral health and exhibit limited construct validity [11]. However, despite being a generic measure the EuroQol has shown discriminant validity in relation to a range of dental patient, visit and oral health measures [12]. The aims of this study were to compare the dimensions of oral-health-related quality-of-life measured by a generic health state measure, the EuroQol, and a specific oral health measure, the OHIP. By comparing the dimensions of these measures we aim to obtain a clearer picture of what they are measuring, which has application in determining whether one instrument can be interchanged with the other (if they measure the same thing), or if there is justification in using both (if they measure different things). The EuroQol could be useful in terms of efficiently broadening the domains measured if it did not overlap with OHIP.
Methods
Design
The Burden of oral disease study was conducted using a 2-stage sampling design whereby dentists were randomly sampled from the South Australian Dental Register, randomised into one of seven equal-sized study groups (n = 100) and sent a mailed self-complete dentist questionnaire along with up to five self-complete patient questionnaires depending on the study group. The dentist questionnaire collected data on dentist and practice details and patient oral health details. A pilot study was conducted which collected five patients per dentist in order to establish the feasibility of the 2-stage methodology. Since the optimum number of patients to sample from dentists was not known, dentists in the main study were randomised into six groups in order to assess the sample size-related efficiency and response properties of recording data on from 1 to 5 patients and distributing between 0 to 5 patient questionnaires. Note that dentists in the group that had no patient questionnaires to distribute recorded details of 5 patients in their dentist questionnaire, while dentists in all other groups recorded the same number of patients in their dentists questionnaire as they distributed patient questionnaires. Within the questionnaire dentists were provided with a practitioner logbook in which to record for the first 1 to 5 adult patients (depending on study group assignment of dentist) of a random clinical day the diagnosis of the oral disease or condition treated and the treatment they performed. At the conclusion of treatment each practitioner (except dentists in the study group that had no patient questionnaires to distribute) passed on a survey kit to their sampled patient(s) containing a cover letter and explanation sheet, and a patient questionnaire. Sampled patients completing the patient questionnaire recorded basic socio-demographic characteristics and data concerning the nature, severity and duration of their symptoms. The patient questionnaires were identified using the practitioner identification number allowing linkage between the practitioner logbook data and patient questionnaire data, but maintaining the anonymity of each patient to the investigators. While the primary rationale for this 2-stage methodology was to allow linkage of dentist-assessed oral health status to patient perceptions of quality of life this paper reports solely on the patient perception data. The research project was reviewed and approved by the Human Research Ethics Committee of the University of Adelaide.
Sampling and data collection
Data were collected during 2001–2 with a primary approach letter sent initially to each dentist, followed a week later by the survey materials, with a reminder card two weeks later, and up to four follow-up mailings of survey materials to dentists who had not yet responded in order to ensure higher response rates [13].
Data items
Dentists recorded the details of the dental conditions that patients had, and patients recorded their experience of those dental conditions. Diagnosis of dental conditions was collected from dentists using an open-ended question in the dentist questionnaire. In the patient questionnaire, patients were asked if the dental conditions had caused problems in each of six health state dimensions. The six health state dimensions were: mobility (e.g, walking about), self-care (e.g, washing, dressing), usual activities (e.g., work, study, housework, family or leisure), pain/discomfort, anxiety/depression and cognition (e.g, memory, concentration, coherence, IQ). They were measured using the European Quality of Life indicator or EuroQol (EQ-5D+) instrument [6]. The EuroQol measures each of these six dimensions according to a 3-level response grading from 1 = no problems, 2 = some / moderate problems and 3 = extreme problems. Patients were also asked to rate their experience of dental problems in the last year using the OHIP-14 [5], which uses 14 items to capture measures of the seven dimensions of functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability and handicap. For each of the 14 OHIP questions subjects were asked how frequently they had experienced impact in the preceding 12 months using a 5-point scale coded 4 = very often, 3 = fairly often, 2 = occasionally, 1 = hardly ever and 0 = never.
Data analysis
The characteristics of responding patients were compared descriptively with published data on dental patients and the Australian population. The distributions of responses to the EQ-5D+ and OHIP items were examined, and the items were analysed by factor analysis and cluster analysis. Factor analysis was used to examine the battery of quality-of-life items for underlying component factors. Standard errors and confidence intervals were reported adjusted for the effect of clustering within the primary sampling unit of dentist.
Principal components factor analyses were performed using varimax rotation [14]. A range of n-factor solutions were performed and assessed. While selecting the number of factors involves the reasonableness of the solution and knowledge of the subject matter [15,16], retaining factors with eigenvalues greater than 1.0 is commonly used, based on heuristic and practical grounds. Sampling adequacy, or the degree that the subset of variables used represents a potentially larger domain, was assessed by Kaiser's measure of sampling adequacy [15]. Communality measures the common factor variance of a variable. A communality of 0.3 or less indicates that a variable may be unreliable [17], while a value greater than 0.3 indicates a large percentage of the sample variance of each variable is accounted for by the factors [16].
Hierarchical clustering of variables was performed using SAS PROC VARCLUS [14], an oblique multiple-group component analysis. Associated with each cluster is a linear combination of the variables in the cluster, the first principal component. The first principal component is a weighted average of the variables that explains as much variance as possible. Clusters are chosen to maximise the variation accounted for by the first principal component of each cluster. SAS PROC TREE was used to construct a dendrogram to present the results of the hierarchical clustering as a tree structure [14].
Results
Response
A total of 378 dentists responded to the survey (response rate = 60%). Response rates between study groups ranged from 49% to 70% and tended to be higher in study groups that required dentists to sample less patients, but the effect was not monotonic (Table 1). Data were available for 375 patients from the patient questionnaire, comprising a response rate of 72% of patients sampled, with response rates between study groups ranging from 69% to 92%.
Table 1.
Response to the dentist and patient questionnaires
| Dentist questionnaire | Patient questionnaire | |||||||
| Patients recorded | Patients recorded | |||||||
| Patients sampled per dentist | Number of dentists responding | Response rate (%) | Number | Percent | Number | Percent | Response rate (%) | |
| Pilot study | 5 | 60 | (65) | 135 | (17.9) | 93 | (24.8) | (69) |
| Main study (a) | 0 | 61 | (70) | 237 | (31.4) | - | (-) | (-) |
| Main study (b) | 1 | 56 | (62) | 37 | (4.9) | 29 | (7.7) | (78) |
| Main study (c) | 2 | 54 | (60) | 49 | (6.5) | 45 | (12.0) | (92) |
| Main study (d) | 3 | 43 | (49) | 61 | (8.1) | 41 | (10.9) | (67) |
| Main study (e) | 4 | 50 | (58) | 118 | (15.6) | 84 | (22.4) | (71) |
| Main study (f) | 5 | 54 | (57) | 119 | (15.7) | 83 | (22.1) | (70) |
| Total | 378 | (60) | 756 | (100.0) | 375 | (100.0) | (72) | |
Characteristics of patients
The characteristics of patients are presented in Table 2 where data from private general practice [18] and Australian population estimates [19,20] are presented for comparison. The majority of patients were female (59.5%), born in Australia (75.5%), had dental insurance (64.8%) and had visited a dentist in the last 12 months (65.3%). The main reason for dental visiting was for other dental problems not involving relief of pain (46.7%), followed by check-ups (35.2%) and emergency visits involving relief of pain (18.1%). The 95% confidence intervals around the estimates include the population estimates for place of birth and time since last visit and include the private general practice estimate for sex of patient indicating no significant difference. However, both the population and private general practice estimates are not included in the confidence intervals for dental insurance and visit type showing the sampled patients as having higher insurance coverage and being more likely to visit for dental problems not involving relief of pain.
Table 2.
Characteristics of patients compared with private general practice and Australian population estimates
| Burden of Oral Disease Study | Private General Practice (a) | Australian Population | |
| % (95% CI) | % | % | |
| Sex | |||
| % Female | 59.5 (54.8–64.2) | 54.9 | (b) 50.4 |
| Place of birth | |||
| % Australian | 75.5 (70.6–80.4) | n.a. | (b) 76.4 |
| Dental insurance status | |||
| % Insured | 64.8 (59.1–70.5) | 47.8 | (c) 34.8 |
| Reason for dental visit | |||
| Check-up | 35.2 (30.1–40.3) | 41.1 | (c) 45.1 |
| Emergency | 18.1 (13.8–22.4) | 28.6 | n.a. |
| Other dental problem | 46.7 (41.6–51.8) | 30.8 | n.a. |
| Time since last dental visit | |||
| % visited in last 12 months | 65.3 (60.0–70.6) | n.a. | (c) 61.3 |
(a): Longitudinal Study of Dentists' Practice Activity 1998–99 (b): Australian Bureau of Statistics 2002 (c): National Dental Telephone Interview Survey 1999 n.a.: denotes data not available
Distribution of items
The distribution of responses to the EuroQol items are presented in Table 3, which shows that the majority of patients had no problems on the six dimensions measured, ranging between 69.7% for pain/discomfort to 98.6% for self-care. The highest percentages of patients reporting some/moderate problems were observed for pain/discomfort (25.7%) and anxiety/depression (14.7%). The highest percentage of patients reporting extreme problems was observed for pain/discomfort (4.6%). Mean scores ranged between 1.01 for self-care to 1.35 for pain/discomfort.
Table 3.
Distribution of EuroQol items, ranging from 1 (No problems), 2 (Some/moderate problems) to 3 (Extreme problems)
| Item | Description of item | Distribution of responses (%) | Mean | (S.E.) | ||
| 1 | 2 | 3 | ||||
| EQ1 | Mobility (1) | 97.5 | 2.5 | 0.0 | 1.025 | (.008) |
| EQ2 | Self-care (2) | 98.6 | 1.4 | 0.0 | 1.014 | (.007) |
| EQ3 | Usual activities (3) | 93.7 | 6.3 | 0.0 | 1.063 | (.014) |
| EQ4 | Pain/discomfort (4) | 69.7 | 25.7 | 4.6 | 1.350 | (.031) |
| EQ5 | Anxiety/depression (5) | 84.5 | 14.7 | 0.8 | 1.163 | (.020) |
| EQ6 | Cognition (6) | 91.5 | 8.5 | 0.0 | 1.085 | (.015) |
1: No problems, or some problems in walking about, or confined to bed 2: No problems, or some problems with self-care (eg, washing, dressing), or unable to wash or dress 3: No problems, or some problems, or unable to perform usual activities (eg, work, study, housework, family or leisure) 4: No, moderate or extreme pain or discomfort 5: Not anxious or depressed, moderately anxious or depressed, or extremely anxious or depressed 6: No, some or extreme problems in cognitive functioning (eg, memory, concentration, coherence, IQ)
The distribution of responses to the OHIP-14 items are presented in Table 4, which shows that the majority of patients reported never having had problems in the last year on all items (ranging from 57.0% for felt tense to 89.2% for unable to function) except painful aching in the mouth (37.3%), uncomfortable eating any foods (32.3%) and felt self-conscious (48.8%). There were generally low percentages of patients reporting that they had problems very often in the last year. Mean scores ranged between 0.14 for unable to function to 1.36 for uncomfortable eating any foods.
Table 4.
Distribution of OHIP items, ranging from 0 (Never), 1 (Hardly ever), 2 (Occasionally), 3 (Very often) to 4 (Fairly often)
| Description of item | Distribution of responses (%) | |||||||
| Item | How often in the last year have you had problems with your teeth mouth or dentures? | 0 | 1 | 2 | 3 | 4 | Mean | (S.E.) |
| OH1 | Have you had trouble pronouncing any words because of problems with your teeth, mouth or dentures | 81.2 | 10.0 | 6.2 | 2.2 | 0.5 | 0.309 | (.038) |
| OH2 | Have you felt that your sense of taste has worsened because of problems with your teeth, mouth or dentures? | 76.5 | 11.1 | 9.4 | 2.5 | 0.6 | 0.395 | (.047) |
| OH3 | Have you had painful aching in your mouth? | 37.3 | 29.0 | 25.5 | 4.7 | 3.6 | 1.082 | (.057) |
| OH4 | Have you found it uncomfortable to eat any foods because of problems with your teeth, mouth or dentures? | 32.3 | 21.4 | 30.6 | 9.2 | 6.5 | 1.363 | (.064) |
| OH5 | Have you felt self conscious because of problems with your teeth, mouth or dentures? | 48.8 | 14.9 | 21.7 | 7.6 | 7.1 | 1.092 | (.069) |
| OH6 | Have you felt tense because of problems with your teeth, mouth or dentures? | 57.0 | 16.8 | 16.8 | 6.5 | 3.0 | 0.816 | (.060) |
| OH7 | Has your diet been unsatisfactory because of problems with your teeth, mouth or dentures? | 73.6 | 12.5 | 9.5 | 2.7 | 1.6 | 0.462 | (.050) |
| OH8 | Have you had to interrupt meals because of problems with your teeth, mouth or dentures? | 64.6 | 20.3 | 12.4 | 1.6 | 1.1 | 0.543 | (.047) |
| OH9 | Have you found it difficult to relax because of problems with your teeth, mouth or dentures? | 66.0 | 16.2 | 13.5 | 2.4 | 1.9 | 0.581 | (.052) |
| OH10 | Have you been a bit embarrassed because of problems with your teeth, mouth or dentures? | 57.1 | 18.0 | 15.8 | 5.9 | 3.2 | 0.802 | (.055) |
| OH11 | Have you been a bit irritable with other people because of problems with your teeth, mouth or dentures? | 66.9 | 18.6 | 11.9 | 1.4 | 1.4 | 0.518 | (.048) |
| OH12 | Have you had difficulty doing your usual jobs because of problems with your teeth, mouth or dentures? | 80.4 | 12.6 | 6.2 | 0.3 | 0.5 | 0.279 | (.037) |
| OH13 | Have you felt that life in general was less satisfying because of problems with your teeth, mouth or dentures? | 68.7 | 13.5 | 12.7 | 3.8 | 1.4 | 0.557 | (.052) |
| OH14 | Have you been totally unable to function because of problems with your teeth, mouth or dentures? | 89.2 | 7.3 | 3.5 | 0.0 | 0.0 | 0.143 | (.024) |
Factor structure
A number of n-factor solutions ranging from 4 to 6 factors were considered, with the 4-factor solution presented in Table 5. This solution was selected on the basis on the eigenvalues greater than 1.0 rule, however there was little difference in interpretation based on the other solutions. Sampling adequacy was high, as indicated by Kaiser's measure of sampling adequacy and communality values of over 0.3 indicated that the variables were reliable (i.e., a large percentage of the sample variance of each variable is accounted for by the factors). While the EuroQol items tended to load separately – anxiety/depression and cognition loaded on factor 4, and mobility, self-care and usual activities loaded together on factor 3 – the EuroQol item pain/discomfort loaded on factor 2 along with a range of OHIP items including those in the physical pain subscale (items OH3 and OH4). However, a range of OHIP items loaded highly on both factor 1 and factor 2 – OH4 and OH11 loaded most highly on factor 2 but also loaded highly on factor 1, and items OH6 to OH9, OH12 and OH13 loaded most highly on factor 1 but also loaded highly on factor 2.
Table 5.
Factor analysis of EQ-5D+ and OHIP-14 items
| Initial statistics (a) | Final statistics (b) | ||||||||
| Factor loadings | |||||||||
| Factor | Eigen-value | Variance (%) | Item | Item label | 1 | 2 | 3 | 4 | h2 |
| 1 | 8.44 | 42.2 | EQ1 | Mobility problems | .068 | .097 | .844 | -.031 | .73 |
| 2 | 1.71 | 8.6 | EQ2 | Self-care problems | .045 | -.088 | .776 | .142 | .63 |
| 3 | 1.37 | 6.9 | EQ3 | Problems with usual activities | .066 | .368 | .500 | .121 | .40 |
| 4 | 1.05 | 5.3 | EQ4 | Pain/discomfort | -.001 | .829 | .070 | .154 | .72 |
| 5 | 0.91 | 4.6 | EQ5 | Anxiety/depression | .158 | .351 | .071 | .693 | .63 |
| 6 | 0.81 | 4.1 | EQ6 | Cognition | .187 | .032 | .122 | .820 | .72 |
| 7 | 0.77 | 3.9 | OH1 | Trouble pronouncing words | .672 | .087 | .354 | .062 | .59 |
| 8 | 0.66 | 3.3 | OH2 | Sense of taste worsened | .575 | .278 | .152 | .177 | .46 |
| 9 | 0.61 | 3.1 | OH3 | Painful aching in mouth | .286 | .709 | .035 | .013 | .59 |
| 10 | 0.56 | 2.8 | OH4 | Uncomfortable eating | .503 | .596 | .092 | -.029 | .62 |
| 11 | 0.50 | 2.5 | OH5 | Felt self-conscious | .838 | .161 | -.074 | .065 | .74 |
| 12 | 0.39 | 2.0 | OH6 | Felt tense | .681 | .479 | -.014 | .176 | .72 |
| 13 | 0.37 | 1.9 | OH7 | Diet unsatisfactory | .578 | .448 | .252 | .154 | .62 |
| 14 | 0.35 | 1.8 | OH8 | Interrupt meals | .540 | .519 | .180 | .029 | .59 |
| 15 | 0.34 | 1.7 | OH9 | Difficulty relaxing | .600 | .577 | .075 | .179 | .73 |
| 16 | 0.30 | 1.5 | OH10 | Been embarrassed | .881 | .040 | -.039 | .145 | .80 |
| 17 | 0.29 | 1.4 | OH11 | Irritable with other people | .471 | .593 | -.031 | .149 | .60 |
| 18 | 0.26 | 1.3 | OH12 | Difficulty doing usual jobs | .561 | .531 | .078 | .157 | .63 |
| 19 | 0.17 | 0.9 | OH13 | Life less satisfying | .618 | .464 | .039 | .305 | .69 |
| 20 | 0.12 | 0.6 | OH14 | Unable to function | .189 | .500 | .087 | .260 | .36 |
| Variance (%): | 25.3 | 20.3 | 9.4 | 7.8 | |||||
(a) method = principal components (b) rotation = varimax h2 = communality Kaiser's measure of sampling adequacy = 0.91
Cluster structure
Figure 1 shows that the first branch in the dendrogram split the EuroQol items mobility (EQ1), self-care (EQ2) and usual activities (EQ3) from the OHIP items and the remaining EuroQol items. Moving from the bottom towards the top of the dendrogram the next major branch split the OHIP psychological discomfort subscale items (OH5 and OH6) together with one psychological disability subscale item (OH10) and the functional limitation subscale items (OH1 and OH2). At the next major branch the EuroQol anxiety/depression (EQ5) and cognition problems (EQ6) items were split from the remaining items. At the next major branch the EuroQol pain/discomfort item (EQ4) split together with the OHIP physical pain subscale items (OH3 and OH4). At the next major branch the OHIP item OH14 (unable to function) split from the remaining items. At the next major branch the OHIP physical disability items (OH7 and OH8) split from the OHIP social disability items (OH11 and OH12) together with the psychological disability item, OH9 (difficulty relaxing).
Figure 1.
Dendrogram from cluster analysis of EQ-5D+ and OHIP-14 items
OHIP items tended to cluster together in subscales, either in the same branch or as adjacent items in a sub-branch, with the main exception being the psychological disability subscale being split between social disability and psychological discomfort (highlighted by the dotted line connecting OH9 at the top of the dendrogram to OH10 in the lower portion of the dendrogram). Handicap subscale items were not widely separated in the branching structure (on either side of OH7 and OH8, indicated by the dotted line connecting OH13 to OH14 in the upper portion of the dendrogram) and were in the same major branch as the disability subscale items. The dotted line connecting OH5 and OH6 indicates that these OHIP psychological discomfort subscale items were separated on either side of the OH10 item.
Discussion
Response
Response rates to the survey were adequate for both the dentist and patient questionnaires [21]. Comparison of respondents against estimates for private general practice and the Australian population indicated a slightly higher percentage of female patients compared to the population consistent with higher reported visiting rates by females [20], but both place of birth and time since last visit were similar. While dental insurance was higher, the percentage of check-up visits was lower among patients indicating a higher percentage of dental problems for patients compared to the population. The respondents tend to be representative in terms of demographics and dental visiting but have higher levels of dental problems. The method of sampling patients showed that response rates tended to be higher among dentists who had to sample fewer patients consistent with a lower response burden, but selection of an optimal collection methodology requires consideration of efficiency of collection as well as response rates.
Factor structure
While EuroQol items tended to load on separate factors to OHIP items, there was some overlap in dimensions for the EuroQol pain/discomfort item and the OHIP physical pain subscale. In general, OHIP items loaded highly on each of the first two factors. Since it is often recommended to sample 4 or more variables to identify each factor [22], it might be argued that using the full OHIP-49 rather than the shorter OHIP-14 would provide a better factor analytic solution, however previous analysis of a wider range of OHIP items drawn from the full OHIP-49 battery [2] showed that one principal component accounted for a large percentage of variance, with another three principal components having eigenvalues greater than one [5]. High intercorrelation of items was suggested as the reason that one principal component dominated the factor analysis [5], and interpreted as indicating that one single underlying construct could be interpreted to represent "oral ill-health".
Some technical aspects of factor analysis might be raised in relation to why the OHIP items were not separated. While interval level of measurement is implied by the use of correlation or covariance matrices as the basic input into factor analysis many variables such as measures of attitudes and opinions that do not have a clearly established metric base may be given numeric values without distorting the underlying properties [15]. Additionally, the assumption that variables have a multivariate normal distribution is only required in the case of maximum likelihood (ML) solutions. However, as a descriptive method ML factor analysis does not require a multivariate normal distribution, although the validity of Bartlett's test for the number of factors does require such an assumption [14]. The factor analysis model itself does not require such an assumption [15], with the solution presented here being based on a principal components factor analysis. Another consideration is that factor analysis may not be preferred as a scale validation method for instruments that contain causal indicators such as disease-related groups of symptoms, as these factors are likely to vary between different patient subgroups [23]. While this phenomenon may have particular relevance to quality of life measurement in terms of being able to measure both good and poor quality of life rather than just poor quality of life [24], factors in general should be interpreted with caution. Reification of factors may occur, and researchers are cautioned against attributing reality and uniqueness to factors (i.e., giving a factor a name does not give it reality). However, factors that recur from different samples and conditions point to an underlying variable [25].
Cluster structure
The purpose of cluster analysis is to place objects (i.e., variables) into groups (i.e., clusters) suggested by the data, not defined a priori, so that the variables in a given cluster tend to be similar to each other. Factor analysis is often used to classify variables into groups (i.e., factors) but the resultant groups are overlapping. While factor analysis may be preferred when overlapping groups are desired, cluster analysis can be used for both hierarchical and disjoint clustering of variables [14]. The results of the cluster analysis showed that there was some separation of the generic items from the specific items, with the EuroQol mobility, self-care and usual activities items branching off from the root of the tree structure. However, the EuroQol items anxiety/depression and cognition formed a cluster adjacent to the EuroQol pain item that clustered with the OHIP pain subscale items, and the OHIP functional limitation subscale items indicating that the separation was partial and there was a degree of overlap in the domains measured by both instruments.
Most of the items from the conceptually derived OHIP subscales formed clusters providing empirical support for those conceptual subscales. The positioning of the OHIP handicap and disability items in adjacent clusters of a major sub-branch of the tree structure fits conceptual expectations, as does the positioning of the limitation and discomfort items in adjacent clusters of another major sub-branch of the tree structure. The main departure from expected groupings was that one item from the OHIP psychological disability subscale clustered with items from the OHIP psychological discomfort subscale instead. Replication would be required to determine whether this represents incorrect assignment of the item to the conceptual subscale or the response preferences of this particular study group. The nature and magnitude of impacts may vary according to the cultural background of the population measured, and there has been some questioning of whether existing oral health status measures are sufficiently robust in their conceptual underpinning [26].
Conclusions
The generic and specific instruments showed a degree of overlap in dimensions, particularly for pain. While the highly inter-correlated OHIP items were difficult to separate using factor analysis, the use of hierarchical cluster analysis showed that most of the conceptually derived subscales of the OHIP could be confirmed empirically. The partial separation in the domains of both instruments confirms that generic and specific measures can be used in combination to capture different elements of quality of life – with both instruments covering symptom experience of pain but EuroQol tapping daily activities such as self-care and usual activities and OHIP tapping oral health-specific aspects of functional limitation and physical disability as well as psychological and social aspects of disability and handicap.
Authors' contributions
DSB and AJS were chief investigators on the grants obtained to fund the study. DSB performed data collection, analysis and drafting of the manuscript. AJS participated in the design and coordination of the study, and completion of the manuscript. All authors read and approved the manuscript.
Acknowledgments
Acknowledgements
This research was performed at the Australian Research Centre for Population Oral Health, Dental School, Faculty of Health Sciences at The University of Adelaide with funding from the Australian Dental Research Foundation and Adelaide University Small Research Grants Scheme. The participation of responding dentists and patients is acknowledged.
Contributor Information
David S Brennan, Email: david.brennan@adelaide.edu.au.
A John Spencer, Email: john.spencer@adelaide.edu.au.
References
- Bowling A. Measuring disease A review of disease-specific quality of life measurement scales. Second. Buckingham: Open University Press; 2001. [Google Scholar]
- Slade GD, Spencer AJ. Development and evaluation of the oral health impact profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- Locker D. Measuring oral health: a conceptual framework. Community Dent Health. 1988;5:3–18. [PubMed] [Google Scholar]
- WHO . International classification of impairments, disabilities and handicaps. Geneva: World Health Organization; 1980. [Google Scholar]
- Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–290. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35:1095–1108. doi: 10.1097/00005650-199711000-00002. [DOI] [PubMed] [Google Scholar]
- Jenkinson C, Gray A, Doll H, Lawrence K, Keoghane S, Layte R. Evaluation of index and profile measures of health status in a randomised controlled trial. Comparison of the Medical Outcomes Study 36-item Short Form Health Survey, EuroQol, and disease-specific measures. Med Care. 1997;35:1109–1118. doi: 10.1097/00005650-199711000-00003. [DOI] [PubMed] [Google Scholar]
- Oberg U, Oberg T. Do EuroQol and SF-36 yield equivalent information, or do they represent different domains of knowledge? In: Norinder AL, Pedersen KM, Roos P, editor. In Proceedings of the 18th Plenary Meeting of the EuroQol Group. EuroQol Group; 2001. pp. 177–185.http://www.euroqol.org/news/meeting2001/proceedings.php [Google Scholar]
- Heydecke G, Locker D, Awad MA, Lund JP, Feine JS. Oral and general health-related quality of life with conventional and implant dentures. Community Dent Oral Epidemiol. 2003;31:161–168. doi: 10.1034/j.1600-0528.2003.00029.x. [DOI] [PubMed] [Google Scholar]
- Allen PF, McMillan AS, Walshaw D, Locker D. A comparison of the validity of generic- and disease-specific measures in the assessment of oral health-related quality of life. Community Dent Oral Epidemiol. 1999;27:344–352. doi: 10.1111/j.1600-0528.1999.tb02031.x. [DOI] [PubMed] [Google Scholar]
- Brennan DS, Spencer AJ. Comparison of a generic and a specific measure of oral health related quality of life. Community Dent Health. [PubMed]
- Dillman DA. Mail and telephone surveys The total design method. NY: Wiley; 1978. [Google Scholar]
- SAS Institute . SAS/STAT User's guide Version 6. 4. Cary, NC: SAS Institute Inc; 1989. [Google Scholar]
- Kim J, Mueller CW. Sage university paper series on quantitative applications in the social sciences, 07-014. Beverly Hills and London: Sage publications; 1978. Factor analysis. Statistical methods and practical issues. [Google Scholar]
- Johnson RA, Wichern DW. Applied multivariate statistical analysis. Second. Englewood Cliffs, NJ: Prentice-Hall; 1988. [Google Scholar]
- Child D. The essentials of factor analysis. London: Holt, Rinehart and Winston; 1978. [Google Scholar]
- Brennan DS, Spencer AJ. Dentists' practice activity in Australia: 1983–84 to 1998–99. Canberra: AIHW; 2002. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics . Australian demographic statistics – March quarter 2002. Canberra: ABS, 3101.0; 2002. [Google Scholar]
- Carter KD, Stewart JF, Spencer AJ. National dental telephone interview survey 1999. Adelaide: AIHW DSRU; 2001. [Google Scholar]
- Mangione TW. Mail surveys Improving the quality. CA: Sage; 1995. [Google Scholar]
- Short R, Horn J. Some notes on factor analysis of behavioural data. Behaviour. 1984;90:203–214. [Google Scholar]
- Fayers PM, Hand DJ. Factor analysis, causal indicators and quality of life. Qual Life Res. 1997;6:139–150. doi: 10.1023/a:1026490117121. [DOI] [PubMed] [Google Scholar]
- Fayers PM, Hand DJ, Bjordal K, Groenvold M. Causal indicators in quality of life research. Qual Life Res. 1997;6:393–406. doi: 10.1023/A:1018491512095. [DOI] [PubMed] [Google Scholar]
- Kerlinger FN. Foundations of behavioural research. Third. Florida: Holt, Rinehart and Winston, Inc; 1986. [Google Scholar]
- Allen PF. Assessment of oral health related quality of life. Health Qual Life Outcomes. 2003;1:40. doi: 10.1186/1477-7525-1-40. [DOI] [PMC free article] [PubMed] [Google Scholar]