Abstract
Purpose
Several bioabsorbable and metal options are available for internal fixation of an unstable osteochondritis dissecans (OCD) lesion, but currently there are little data on outcomes with metal headless compression screws in the adult knee. The purpose of this study was to determine (1) the radiographic healing rates, (2) midterm clinical outcomes, and (3) comparison between healed and unhealed OCD fragments after use of headless metal compression screws for the treatment of unstable OCD lesions in the knees of skeletally mature patients.
Methods
Retrospective chart review for all skeletally mature patients who presented with unstable femoral condyle OCD lesions of the knee was conducted. All patients underwent open or arthroscopic reduction and internal fixation using headless metal compression screws. Preoperative and postoperative radiographs were reviewed with healing defined as radiographic evidence of union of the OCD progeny fragment with the condyle. Clinical outcome data were collected retrospectively using 3 validated outcome scores: International Knee Documentation Committee (IKDC), Knee Injury and Osteoarthritis Outcome Score (KOOS), and Marx.
Results
Twenty-two knees in 22 patients with a mean age of 21 years (range= 14-37 years) were followed for an average of 8.7 years (range = 2-22 years). Metal, headless, cannulated compression screws were used in all 22 cases. At a mean of 31 months postoperatively (range = 2-262), fragment union was observed in 18 knees (82%). The remaining 4 knees (18%) required loose fragment excision and hardware removal at a mean of 9 months (range = 2-16 months) postoperatively. Mean postoperative Marx score was 7 (range = 0-16), the mean postoperative IKDC score was 85 (range = 62-100), and mean KOOS scores included KOOS Pain (93; range = 69-100), KOOS Symptoms (86; range = 71-100), KOOS ADL (98; range = 90-100), KOOS Sports (82; range = 50-100), and KOOS QOL (76; range = 50-100).
Conclusion
Headless metal compression screws provide a satisfactory union rate for treatment of unstable OCD lesions of the femoral condyles in skeletally mature patients. Patients achieving union have good knee function, maintain satisfactory activity levels, and have superior knee outcomes compared with those that failed to heal after fixation at mid to long-term follow-up.
Keywords: knee, cartilage repair, articular cartilage
Introduction
The majority of cases of osteochondritis dissecans (OCD) are diagnosed prior to skeletal maturity.1 OCD presenting in adulthood is thought primarily to represent juvenile disease that went unrecognized, although de novo cases have been reported in the literature.2 Unlike those patients with open physes, skeletally mature patients have a poor prognosis with nonoperative treatment.2 Linden3 showed that only 10% of adult patients treated without surgery show signs of healing on magnetic resonance imaging (MRI) follow-up. Furthermore, the large majority of these patients develop early arthritis in the knee.
Nonoperative management may play a role in treating asymptomatic stable OCD lesions in the skeletally mature patient, but operative fixation is indicated for all symptomatic unstable lesions.4 OCD lesions in the adult population are typically larger, demonstrate a greater degree of chondral damage, and are more often displaced when compared with lesions in the juvenile patient.1,5,6 Carey and Grimm4 created an algorithm to aid clinicians in the treatment of OCD. Operative fixation is indicated for salvageable unstable lesions with at least 3 mm of attached subchondral bone and minimal fragmentation. As well, operative fixation has been shown to have superior clinical and radiographic outcomes in comparison to nonoperative treatment.7,8
There are multiple methods reported for fixation of OCD lesions including metal and bioabsorbable headless compression screws, barbed arrows, and other devices. Previous studies have assessed the effectiveness of bioabsorbable fixation for OCD lesions in the skeletally mature population with concerning results due to hardware complications.9 Existing studies assessing metal fixation technique either included multiple surgical techniques10 or related specifically to the juvenile population.11 The purpose of this study was to determine (1) the radiographic healing rates, (2) midterm clinical outcomes, and (3) comparison between healed and unhealed OCD fragments after use of headless metal compression screws for the treatment of unstable OCD lesions in the knees of skeletally mature patients.
Methods
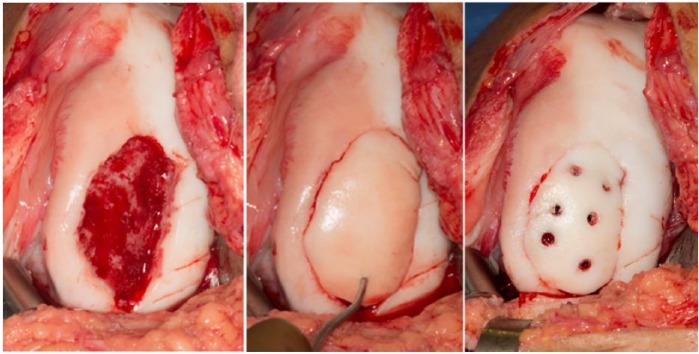
Institutional review board approval was obtained prior to initiation of this study. Twenty-two skeletally mature patients who underwent fixation of an unstable OCD lesion (CPT 732.7) with metal headless compression screws between 1993 and 2014 were identified from our institutional surgical database. The decision to proceed with surgical fixation was determined by x-ray or MRI imaging that suggested an unstable lesion4 and clinical symptoms that warranted intervention. Retrospective review of each patient’s medical record identified the size and location of each lesion, the type of surgery performed, the type of internal fixation used, and any subsequent operations. The indication for a salvageable progeny fragment was at least 3 mm of subchondral bone and viable undamaged articular cartilage as suggested by Carey and Grimm4 in all cases. The exact amount of bone in each case was not quantified consistently in the operative reports. Preoperative radiographs were reviewed to confirm that the physes were fully closed prior to operative intervention. The stability of each lesion was graded preoperatively using the Ewing and Voto classification.12 Following diagnostic arthroscopy all lesions were fixed with metal headless compression screws (Fig. 1). This was accomplished through either an arthroscopic approach in 23% or by conversion to a parapatellar arthrotomy in 77%. The type of metal fixation varied by surgeon and technique requirements but included AcuTrak Acumed (Hillsboro, OR) and Arthrex (Naples, FL) cannulated headless compression screws. Following operative intervention all patients were touch weight-bearing for 6 weeks, instructed in a program of hip flexor strengthening and encouraged to regain full active and passive range of motion in the knee.
Figure 1.
Open reduction and internal fixation of OCD fragment using 6 headless metal compression screws in the lateral femoral condyle.
This is a retrospective study. All postoperative images were reviewed by the primary author to assess for radiographic union according to previously delineated criteria.13 Radiographic degenerative changes were assessed using the Kellgren-Lawrence scale.14 All included patients were contacted just prior to the data collection period for routine follow-up and asked to complete clinically validated knee performance (Knee Injury and Osteoarthritis Outcome Score [KOOS], International Knee Documentation Committee [IKDC]) and activity (Marx) scores for entry into the medical record. All patient information was stored securely in an institutionally maintained REDCap database15 (Center for Clinical and Translational Science grant support; UL1 TR000135).
Statistical Analysis
Descriptive analyses of baseline patient characteristics and outcomes scores were performed with use of means and standard deviations for continuous variables and frequencies and percentages for discrete variables. Wilcoxon signed rank test was used to compare IKDC, KOOS, and Marx scores between patients who went on to radiographic healing and those who did not. Statistical significance was set to 0.05. All subsequent analysis was performed using SAS software.
Results
A total of 159 skeletally mature knees underwent operative treatment for osteochondritis dissecans at our institution between 1993 and 2014. Out of this group 69 knees were treated with fragment fixation. A total of 22 knees in 22 skeletally mature patients were treated with metal compression screws for an unstable OCD lesion. The cohort consisted of 16 males (73%) and 6 females (17%) with a mean age of 21 years at the time of surgery (range = 14-37 years). The medial femoral condyle was involved in 16 knees (73%) and the lateral femoral condyle in 6 knees (17%) (Table 1). Patients were followed radiographically for a mean of 2.5 years postoperatively (range = 1-22), and clinical outcome scores were obtained at a minimum of 2 years, with a mean of 8.7 years (range = 2-22 years).
Table 1.
Cross-Sectional Table Demonstrating the Relevant Demographic and Surgical Characteristics of the Study Population.
| Age at Index Surgery (Years) | Gender | Laterality | Ewing-Voto Grade | Lesion Area (cm2) | Follow-up (Years) |
|---|---|---|---|---|---|
| 14 | Male | Medial | 4 | 1.60 | 16 |
| 17 | Male | Medial | 3 | 2.25 | 16 |
| 14 | Male | Medial | 3 | 3.75 | 19 |
| 18 | Male | Medial | 4 | 4.00 | 2 |
| 14 | Male | Medial | 3 | 3.74 | 17 |
| 17 | Female | Lateral | 4 | 1.80 | 16 |
| 22 | Male | Medial | 3 | 1.50 | 2 |
| 17 | Male | Medial | 3 | 6.00 | 22 |
| 16 | Male | Medial | 3 | 6.00 | 19 |
| 32 | Female | Lateral | 4 | 2.40 | 8 |
| 37 | Male | Medial | 3 | 3.22 | 2 |
| 15 | Male | Medial | 4 | 6.00 | 2 |
| 17 | Male | Medial | 3 | 3.00 | 2 |
| 21 | Female | Lateral | 4 | 5.72 | 15 |
| 15 | Male | Medial | 3 | 9.00 | 16 |
| 17 | Female | Lateral | 3 | 1.76 | 2 |
| 25 | Female | Lateral | 4 | 4.00 | 5.4 |
| 37 | Male | Medial | 3 | 1.87 | 3.3 |
| 31 | Male | Medial | 4 | 9.80 | 3.1 |
| 15 | Male | Medial | 4 | 2.40 | 2.8 |
| 18 | Female | Lateral | 4 | 1.60 | 2 |
| 27 | Male | Medial | 3 | 2.25 | 2.9 |
All 22 knes (100%) were classified as unstable with 12 knees (55%) classified as Ewing and Voto grade III (partially attached), while the remaining 10 knees (45%) were grade IV lesions (detached). The average size of the progeny fragment in this series was 3.8 cm2. The grade IV lesions were significantly larger than grade III lesions (5.1 ± 2.9 cm2 vs. 3.3 ± 1.6 cm2, P < 0.05). All patients underwent reduction and internal fixation using metal compression screws from several different manufacturers. The average number of screws was 2 (range = 1-5). No supplementary bone graft was used in any of the cases. Seventeen of 22 patients (77%) required a limited arthrotomy to achieve fragment fixation and the remaining patients were treated arthroscopically.
Radiographic Healing
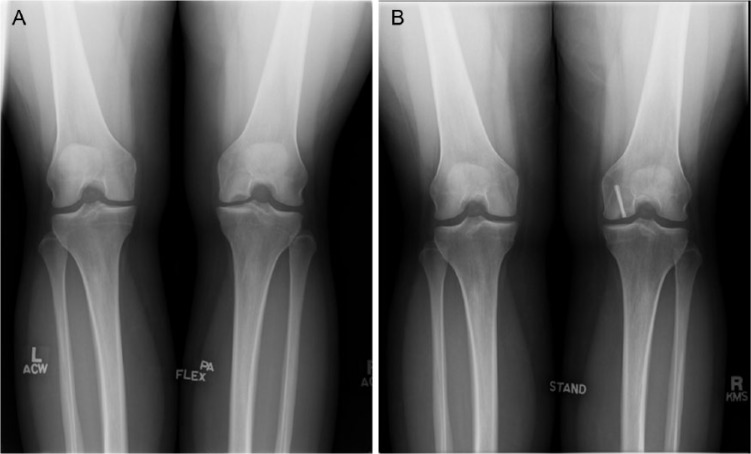
An 82% (18/22) healing rate was observed in this cohort (Fig. 2). There were no significant differences in healing rate by lesion grade (grade III, 67% [8/12]; grade IV, 100% [10/10]; P = 0.09), lesion location (medial femoral condyle, 75% [12/16]; lateral femoral condyle, 100% [6/6]; P = 0.54), or gender (male, 88% [14/16]; female, 67% [4/6]; P = 0.29). Four knees underwent loose fragment excision and hardware removal at a mean of 9 months (range = 2-16 months) after the initial surgery. Three of these 4 patients did require additional procedures. Two were treated with microfracture and chondroplasty, one at the time fragment excision and the other several months later in conjunction with the repair of a meniscal tear. One patient was treated with osteochondral autologous transplantation approximately 6 months following OCD fragment excision. Of the 18 knees that healed, 17 patients underwent additional surgical procedures. Fifteen patients (88%) underwent planned elective screw removal at 6 months following insertion, and 2 patients (12%) required reoperation for screw advancement. Screw advancement was undertaken in both cases because at the time of surgery the osteochondral lesion was found to be well fixed but not fully healed and the screw head had backed out past subchondral bone.
Figure 2.
(A) Preoperative PA flexion radiograph demonstrating OCD lesion in the medial femoral condyle of a 33-year old female. (B) Postoperative radiograph demonstrating union of progeny fragment.
Clinical and Functional Outcomes
At an average follow-up of 8.7 years, mean postoperative Marx score was 7 (range = 0-16). The mean postoperative IKDC score was 85 (range = 62-100). Mean KOOS scores were as follows: KOOS Pain (93; range = 69-100), KOOS Symptoms (86; range = 71-100), KOOS ADL (98; range = 90-100), KOOS Sports (82; range = 50-100), KOOS QOL (76; range = 50-100).
Comparison of Outcomes
In comparison to the patients that had healed OCD lesions, patients with lesions that did not heal demonstrated inferior KOOS Symptoms (77 vs. 88, P = 0.02), KOOS Sports (70 vs. 84, P = 0.04), and KOOS QOL (67 vs. 78, P = 0.03) and Marx Activity (4.6 vs. 7.9, P = 0.04) outcome scores.
Complications
Reported intraoperative complications in this series include one incident of intraoperative guide wire breakage. The fractured guide wire was left in place and surgery proceeded without further incident. As discussed earlier there were 2 reported postoperative complications in the form of screw back out noted at the time of planned screw removal. In both cases the screw head had migrated to be nearly flush with articular surface from its initial countersunk position but there were no abrasions noted on the tibial plateau at the time of reoperation. In both cases the prominent screws were advanced and left in place. In all cases the patients went on to uneventful radiographic healing.
Discussion
A symptomatic, unstable OCD lesion in a skeletally mature patient has limited surgical treatment options. The healing potential of an unstable progeny fragment is variable, and there are limited data to guide surgical implant choice for internal fixation. In this study, we demonstrated an 82% union rate with headless, metal compression screw fixation. When union occurred, patients reported good function and pain relief at a mean of 8.7 years after surgery with superior results when compared to knees that did not obtain union. To our knowledge, this is the first study to report on metal fixation devices for OCD fixation in all skeletally mature knees.
The radiographic union rates found in this study were lower than previously reported in the literature for OCD lesions fixed with metal implants. In one study utilizing titanium Herbert screw fixation, Makino et al.16 demonstrated a 93% rate of healing as demonstrated on MRI and confirmed during arthroscopic screw removal. Another study assessing metal fixation of OCD lesions demonstrated 16/17 patients to be healed by arthroscopic inspection at 12 weeks. Both of these studies included over 50% of patients with open physes. Multiple prior investigations have demonstrated superior healing with any therapeutic modality in skeletally immature patients in comparison to an adult population.17,18 The union rate in this series was superior to reports of OCD fragment fixation using bioabsorbable devices. Millington et al.9 reported radiographic healing rates of only 67% in patients with closed physes fixed with a bioabsorbable implants. Dines et al.19 cited residual instability in 2/7 (28%) knees in a small series of OCD lesions treated with bioabsorbable nails and followed by MRI at the 6-month time point. The most likely explanation for the lower healing rate with bioabsorbable pins, nails, and screws is the inferior compression of the progeny fragment when compared to the headless, metal compression screws used in the current series.
As the present study included a skeletally mature population with mid- to long-term follow-up, it is not unexpected that the clinical outcomes were lower relative to previous reports on skeletally immature patients with shorter follow-up for fixation of unstable OCD lesions. Only 70% of our adult patients had good or excellent results based on their IKDC scoring as opposed to over 90% in studies including skeletally immature patients.16,20 Patients who did not achieve radiographic healing had worse clinical outcome scores. Fragment excision for clinical and radiographic nonunion regardless of subsequent treatment had inferior IKDC (76 vs. 87), KOOS Sports (70 vs. 84), and KOOS QOL (67 vs. 78) and Marx scores (4.6 vs. 7.9) relative to the healed group. This finding is consistent with previous studies where fragment excision was the primary intervention.21 In one study, 71% of patient demonstrated early degenerative changes by 11 years following the index operation.22
Previous studies have investigated the use of bioabsorbable implants for fixation in the adult population and reported suboptimal results. Weckstrom et al.23 compared bioabsorbable pin and nail fixation of adult OCD in 30 knees. They found at an average of 5-year follow-up that only 35% of the pin group had good or excellent results compared to 73% good or excellent results in the nail group. By contrast, previous preliminary studies assessing metal fixation of OCD lesions show excellent results. In a study by Makino et al.16 of 15 knees, they found 14 of 15 knees had evidence of a stable fragment and intact smooth surface at the time of second-look arthroscopy. In addition, 14 had evidence of subchondral bone healing on MRI. Even in the pediatric population unstable lesions treated with metal fixation appear to demonstrate superior outcome scores at midterm follow-up when compared with bioabsorbable fixation.11 Previous biomechanical studies have shown that screw breakage, screw back out, and loss of compressive force over time are all associated with the use of bioabsorbable implants.24 However, bioabsorbable fixation does have some advantages compared to metal fixation, including no metal artifact on postoperative MRI scans and no second surgery required for implant removal if the progeny fragment heals.25
If the OCD progeny fragment fails to heal, or is not salvageable at the index operation, then other salvage treatment options include autologous osteochondral mosaicplasty, osteochondral allograft transplantation (OCA), and autologous chondrocyte implantation with sandwich bone grafting technique (ACI). Each of these treatment options have been shown to be effective in selected patients, but represent a salvage operation rather than a primary procedure.26 Allograft transplantation is perhaps the most well-established of the salvage techniques and in a recent long-term follow-up study demonstrated good or excellent clinical outcomes in over 70% of patients.27 This technique is ultimately limited by the availability and costs of donor specimens. Autologous mosaicplasty is an excellent alternative to OCA and has in some studies demonstrated significantly better clinical results than microfracture at midterm follow-up and higher return to sport.28 Unlike allograft transplantation this technique is significantly limited by the size of the chondral defect.26 Chondrocyte implantation (ACI) allows for coverage of large defects, uses the patient’s own tissue, and in one study was demonstrated to have superior results to mosaicplasty at midterm follow-up.29 The drawback of this technique is that it requires 2 anesthetics to allow for chondrocyte collection and cell line expansion. In this respect ACI is similar to metal compression screw fixation. In our series, 15 out of the 18 knees that went on to healing underwent planned screw removal at 6 months postoperatively. Removal of metal fixation devices is considered the standard of care at our institution as a result of early studies demonstrating screw back out over time with attendant articular damage and recurrence of symptoms.1,30,31
The goal of OCD treatment should be to restore the articular surface, preferably with salvage of the progeny fragment, but possibly with osteochondral autograft, osteochondral allograft, or autologous chondrocyte implantation with sandwich technique in salvage cases.32 The healing potential of an unstable OCD lesion in a skeletally mature population is unpredictable. Based on our results, we feel that reduction and fixation is justified with a reasonable union rate, even in type IV detached fragments that were deemed salvageable.
This study was limited by its retrospective design, small sample size, and nonstandardized implants. The number of screws applied and the configuration of screws was dependent on the size and location of lesions as well as surgeon preference. The long length of the study period also introduces confounding variables as the techniques and implants varied over time. In addition, the sample size was not large enough to make a statistically meaningful analysis of risk factors for failure. Finally, we were unable to consistently identify from the operative reports the exact amount of subchondral bone attached to fixed OCD fragments. Despite these limitations, to our knowledge this is the largest series of treatment of unstable OCD lesions in an adult population with metal headless compression screws. Controversy remains over optimal fixation and certainly there is room for innovation and further study in this area.
Headless, metal compression screws provide a satisfactory union rate for treatment of unstable OCD lesions of the femoral condyles in skeletally mature patients. Patients achieving union have good knee function, maintain satisfactory activity levels, and have superior knee outcomes compared to fragment excision at mid- to long-term follow-up.
Footnotes
Acknowledgments and Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: As part of the IRB approval process, the ethical implications of this study were evaluated and declared of minimal risk. This study was approved by our institutional review board. No further ethical committee approval was required.
References
- 1. Cahill BR. Osteochondritis dissecans of the knee: treatment of juvenile and adult forms. J Am Acad Orthop Surg. 1995;3:237-47. [DOI] [PubMed] [Google Scholar]
- 2. DellaMaggiora R, Vaishnav S, Vangsness CT. Osteochondritis dissecans of the adult knee. Oper Tech Sports Med. 2008;16:65-9. [Google Scholar]
- 3. Linden B. Osteochondritis dissecans of the femoral condyles: a long-term follow-up study. J Bone Joint Surg Am. 1977;59:769-76. [PubMed] [Google Scholar]
- 4. Carey JL, Grimm NL. Treatment algorithm for osteochondritis dissecans of the knee. Clin Sports Med. 2014;33:375-82. [DOI] [PubMed] [Google Scholar]
- 5. Friederichs MG, Greis PE, Burks RT. Pitfalls associated with fixation of osteochondritis dissecans fragments using bioabsorbable screws. Arthroscopy. 2001;17:542-5. [DOI] [PubMed] [Google Scholar]
- 6. Hefti F, Beguiristain J, Krauspe R, Moller-Madsen B, Riccio V, Tschauner C, et al. Osteochondritis dissecans: a multicenter study of the European Pediatric Orthopedic Society. J Pediatr Orthop B. 1999;8:231-45. [PubMed] [Google Scholar]
- 7. Magnussen RA, Carey JL, Spindler KP. Does operative fixation of an osteochondritis dissecans loose body result in healing and long-term maintenance of knee function? Am J Sports Med. 2009;37:754-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. De Smet AA, Ilahi OA, Graf BK. Untreated osteochondritis dissecans of the femoral condyles: prediction of patient outcome using radiographic and MR findings. Skeletal Radiol. 1997;26:463-7. [DOI] [PubMed] [Google Scholar]
- 9. Millington KL, Shah JP, Dahm DL, Levy BA, Stuart MJ. Bioabsorbable fixation of unstable osteochondritis dissecans lesions. Am J Sports Med. 2010;38:2065-70. [DOI] [PubMed] [Google Scholar]
- 10. Pascual-Garrido C, Friel NA, Kirk SS, McNickle AG, Bach BR, Bush-Joseph CA, et al. Midterm results of surgical treatment for adult osteochondritis dissecans of the knee. Am J Sports Med. 2009;37(Suppl 1):125S-30S. [DOI] [PubMed] [Google Scholar]
- 11. Webb JE, Lewallen LW, Christophersen C, Krych AJ, McIntosh AL. Clinical outcome of internal fixation of unstable juvenile osteochondritis dissecans lesions of the knee. Orthopedics. 2013;36:e1444-e1449. [DOI] [PubMed] [Google Scholar]
- 12. Ewing JW, Voto SJ. Arthroscopic surgical management of osteochondritis dissecans of the knee. Arthroscopy. 1988;4:37-40. [DOI] [PubMed] [Google Scholar]
- 13. Kocher MS, Micheli LJ, Yaniv M, Zurakowski D, Ames A, Adrignolo AA. Functional and radiographic outcome of juvenile osteochondritis dissecans of the knee treated with transarticular arthroscopic drilling. Am J Sports Med. 2001;29:562-6. [DOI] [PubMed] [Google Scholar]
- 14. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Makino A, Muscolo DL, Puigdevall M, Costa-Paz M, Ayerza M. Arthroscopic fixation of osteochondritis dissecans of the knee: clinical, magnetic resonance imaging, and arthroscopic follow-up. Am J Sports Med. 2005;33:1499-504. [DOI] [PubMed] [Google Scholar]
- 17. Cahill BR, Phillips MR, Navarro R. The results of conservative management of juvenile osteochondritis dissecans using joint scintigraphy. A prospective study. Am J Sports Med. 17:601-5. [DOI] [PubMed] [Google Scholar]
- 18. Pill SG, Ganley TJ, Milam RA, Lou JE, Meyer JS, Flynn JM. Role of magnetic resonance imaging and clinical criteria in predicting successful nonoperative treatment of osteochondritis dissecans in children. J Pediatr Orthop. 2003;23:102-8. [PubMed] [Google Scholar]
- 19. Dines JS, Fealy S, Potter HG, Warren RF. Outcomes of osteochondral lesions of the knee repaired with a bioabsorbable device. Arthroscopy. 2008;24:62-8. [DOI] [PubMed] [Google Scholar]
- 20. Rey Zuniga JJ, Sagastibelza J, Lopez Blasco JJ, Martinez Grande M. Arthroscopic use of the Herbert screw in osteochondritis dissecans of the knee. Arthroscopy. 1993;9:668-70. [DOI] [PubMed] [Google Scholar]
- 21. Aglietti P, Ciardullo A, Giron F, Ponteggia F. Results of arthroscopic excision of the fragment in the treatment of osteochondritis dissecans of the knee. Arthroscopy. 2001;17:741-6. [DOI] [PubMed] [Google Scholar]
- 22. Murray JRD, Chitnavis J, Dixon P, Hogan NA, Parker G, Parish EN, et al. Osteochondritis dissecans of the knee; long-term clinical outcome following arthroscopic debridement. Knee. 2007;14:94-8. [DOI] [PubMed] [Google Scholar]
- 23. Weckstrom M, Parviainen M, Kiuru MJ, Mattila VM, Pihlajamaki HK. Comparison of bioabsorbable pins and nails in the fixation of adult osteochondritis dissecans fragments of the knee: an outcome of 30 knees. Am J Sports Med. 2007;35:1467-76. [DOI] [PubMed] [Google Scholar]
- 24. Friederichs MG, Greis PE, Burks RT. Pitfalls associated with fixation of osteochondritis dissecans fragments using bioabsorbable screws. Arthroscopy. 2001;17:542-5. [DOI] [PubMed] [Google Scholar]
- 25. Tabaddor RR, Banffy MB, Andersen JS, McFeely E, Ogunwole O, Micheli LJ, et al. Fixation of juvenile osteochondritis dissecans lesions of the knee using poly 96L/4D-lactide copolymer bioabsorbable implants. J Pediatr Orthop. 2010;30:14-20. [DOI] [PubMed] [Google Scholar]
- 26. Polousky JD, Albright J. Salvage techniques in osteochondritis dissecans. Clin Sports Med. 2014;33:321-33. [DOI] [PubMed] [Google Scholar]
- 27. Emmerson BC, Görtz S, Jamali AA, Chung C, Amiel D, Bugbee WD. Fresh osteochondral allografting in the treatment of osteochondritis dissecans of the femoral condyle. Am J Sports Med. 2007;35:907-14. [DOI] [PubMed] [Google Scholar]
- 28. Gudas R, Simonaityte R, Cekanauskas E, Tamosiūnas R. A prospective, randomized clinical study of osteochondral autologous transplantation versus microfracture for the treatment of osteochondritis dissecans in the knee joint in children. J Pediatr Orthop. 2009;29:741-8. [DOI] [PubMed] [Google Scholar]
- 29. Vijayan S, Bartlett W, Bentley G, Carrington RWJ, Skinner JA, Pollock RC, et al. Autologous chondrocyte implantation for osteochondral lesions in the knee using a bilayer collagen membrane and bone graft: a two- to eight-year follow-up study. J Bone Joint Surg Br. 2012;94:488-92. [DOI] [PubMed] [Google Scholar]
- 30. Cugat R, Garcia M, Cusco X, Monllau JC, Vilaro J, Juan X, et al. Osteochondritis dissecans: a historical review and its treatment with cannulated screws. Arthroscopy. 1993;9:675-84. [DOI] [PubMed] [Google Scholar]
- 31. Johnson LL, Uitvlugt G, Austin MD, Detrisac DA, Johnson C. Osteochondritis dissecans of the knee: arthroscopic compression screw fixation. Arthroscopy. 1990;6:179-89. [DOI] [PubMed] [Google Scholar]
- 32. Lyon R, Nissen C, Liu XC, Curtin B. Can fresh osteochondral allografts restore function in juveniles with osteochondritis dissecans of the knee? Clin Orthop Relat Res. 2013;471:1166-73. [DOI] [PMC free article] [PubMed] [Google Scholar]