Abstract
Objectives:
Primary objective was to assess the prevalence of tuberculosis (TB) among household contacts of newly diagnosed sputum smear (SS) positive TB index cases. Secondary objectives were the evaluation of risk factors in household contacts for acquiring TB disease; and the evaluation of various characteristics of index cases which influence the transmission of disease to household contacts.
Settings and Design:
This exploratory cohort study included 521 household contacts of 133 newly diagnosed SS positive TB patients who were registered under the Revised National Tuberculosis Control Program at the Directly Observed Treatment-Short Course Centres of District Tuberculosis Centre, Kolhapur, Maharashtra from July 1, 2013 to February 28, 2014 (8 months).
Subjects and Methods:
Household contacts with symptoms suggestive to TB were subjected to SS examination of two samples for acid fast bacilli by Ziehl-Neelsen staining and for X-ray chest postero-anterior view. Presence of risk factors in symptomatic contacts was also recorded.
Results:
Eighteen contacts out of 521 (3.45%) had symptoms suggestive of TB. Of these, 6 contacts were diagnosed to have TB; 5 being sputum positive cases and one with X-ray suggestive of TB; giving a prevalence of 1.15 %. The study achieved a yield of 4.51% secondary cases.
Conclusions:
Household contact screening of newly diagnosed TB index cases provides modest yield of cases. Relatively fewer secondary symptomatic persons need to be investigated by this method for achieving additional yield proving it to be a practical and feasible approach.
KEY WORDS: Case detection, contact screening, tuberculosis
INTRODUCTION
Achieving tuberculosis (TB) control depends on maximizing early case detection, in the community and their effective treatment using the Directly Observed Treatment-Short Course (DOTS) strategy. Household contacts are highly susceptible to acquire TB infection from the index cases because of their close proximity. Active tracing of such contacts and their screening for TB could lead to the detection of additional cases of TB maximizing the impact of case detection and effective treatment.
Household contact tracing not only results in detection of additional cases but further offers several indirect advantages in the form of lead time obtained for these cases by early diagnosis, reduced duration of morbidity and reduced risk of transmission to others.
Various studies have shown the importance of active case detection among the household contacts of TB cases.[1,2,3,4,5,6] Household contact investigation can easily be implemented with the help of lay workers and could help detect majority of secondary cases among close contacts.[7] Most of the secondary cases can be found at the time of baseline investigation.[1] Even though questions have been raised about the cost effectiveness of this intervention in high burden countries,[8,9] not much resources are expensed to catch these cases.[10]
Various factors are known to affect yield of household contact intervention, background prevalence of TB, duration of follow up, and access to health care services being few of them.[2] To the best of our knowledge, there has been no study from India, looking into feasibly of household contact intervention as case detection tool. Results from studies carried out in other countries cannot be directly extrapolated to the Indian setup due to differences in epidemiology and health care system.
SUBJECTS AND METHODS
The primary objective of the present study was to assess the prevalence of TB among the household contacts of newly diagnosed sputum smear (SS) positive TB cases. Secondary objectives were the evaluation of risk factors in household contacts for acquiring TB disease and evaluation of various characteristics of index cases which influence the transmission of disease to household contacts. The study was approved by the institutional ethical committee. Written informed consent was taken from all the patients as well as their symptomatic contacts included in the study.
This exploratory cohort study was conducted among the household contacts of all newly diagnosed SS positive pulmonary TB patients which were being diagnosed at/referred to the DOTS centre of District Tuberculosis Centre (DTC), Kolhapur from July 2013 to February 2014 (8 months). Cases included in the study were from both rural and urban areas.
An index case was defined as the first SS positive TB case identified in the household. Newly diagnosed SS positive pulmonary TB cases in which none of the household contacts had history of taking anti tubercular treatment in the previous 6 months were included for the study. Household contacts were defined to be those people who shared meals with the index case; stayed together as a family with the index case; spent 8 or more hours per day with the patient in a single room and/or resided with the index case for any 7 consecutive days during 3 months before the diagnosis of TB. Symptomatic contacts were defined as household contacts with one or more symptoms suggestive of TB including cough, expectoration, hemoptysis, weight loss, or fever irrespective of duration at baseline or within 3 months of diagnosis of index case.
Index cases and household contacts not confirming to the case definitions were excluded from the study. All the symptomatic contacts were interviewed and screened within 2 weeks of diagnosis of their index case.
Newly diagnosed SS positive TB cases were explained the purpose and objectives of the study. They were interviewed to find out details of their household contacts. Two sputum samples of all symptomatic contacts were collected. The samples were subjected to sputum acid fast bacilli (AFB) examination by Ziehl-Neelsen (ZN) method as per the Revised National Tuberculosis Control Program guidelines. The x-ray chest postero-anterior view was also carried out for all symptomatic contacts. The presence of risk factors such as human immunodeficiency virus (HIV) status, diabetes, malnutrition, immunosuppressant drugs in suspected contacts was also recorded. In addition, the duration of illness, result of sputum AFB examination, the type of involvement of lung, and the presence of other co morbidities were also noted for the index cases.
All the new cases diagnosed among the household contacts were enrolled into the DOTS program for their treatment. Other household contacts were counselled about the symptoms of TB and advised to approach health care workers in case such symptoms appear. Contacts reporting within 3 months of diagnosis index case with symptoms suggestive of TB were included in the study for the purpose of evaluating this approach to calculate additional yield of cases.
RESULTS
The household contacts of 134 index cases, which were registered at DTC Kolhapur from July 2013 to February 2014, were considered for inclusion in the study. 521 contacts (273 males and 248 females) of 133 index cases were finally included. One index case was excluded from the study, for not fulfilling the case definition.
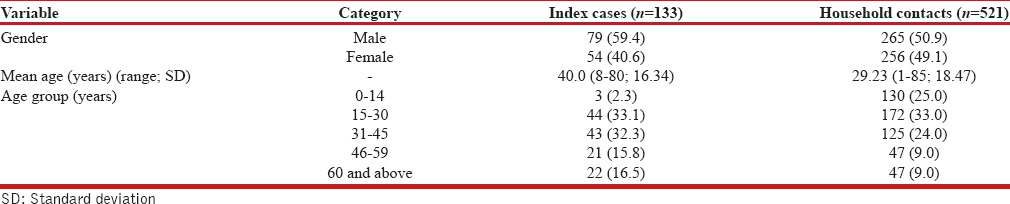
Approximately, four household contacts were enrolled for each index case. In all, 521 household contacts were enrolled. Mean age was 40.0 years ±16.34 years (range 8–80 years) for index cases and 29.23 ± 18.47 years (range 1–85 years) for household contacts.
Twelve of the household contacts presented with symptoms suggestive of TB at baseline and 6 others reported with symptoms later (within 3 months of diagnosis of index case). In all 6 household contacts were diagnosed with TB, of which 5 were diagnosed at baseline and one case was diagnosed 4 weeks after diagnosis of the index case. Five of the diagnosed cases were SS positive, and one was SS negative but had radiological features suggestive of TB in the chest X-ray.
Table 1 shows the sociodemographic profile of index cases and household contacts who were positive for TB.
Table 1.
Comparative characteristics of index cases and household contacts
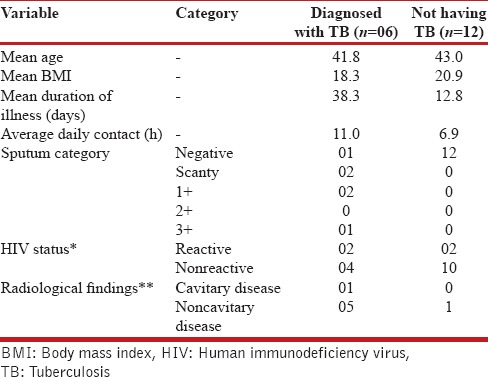
Anthropometric and clinical characteristics were compared for index cases and positive contacts [Table 2] and for index cases which were sources of secondary cases (among contacts) with those who were not [Table 3]. Similar analysis was also performed to compare the characteristics of symptomatic contacts diagnosed with TB and those who were not having TB [Table 4].
Table 2.
Anthropometric and clinical characteristics of index cases and positive contacts
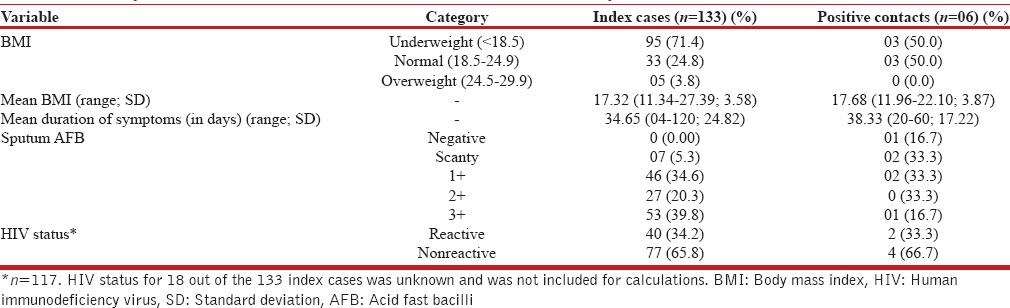
Table 3.
Comparative profile of index cases
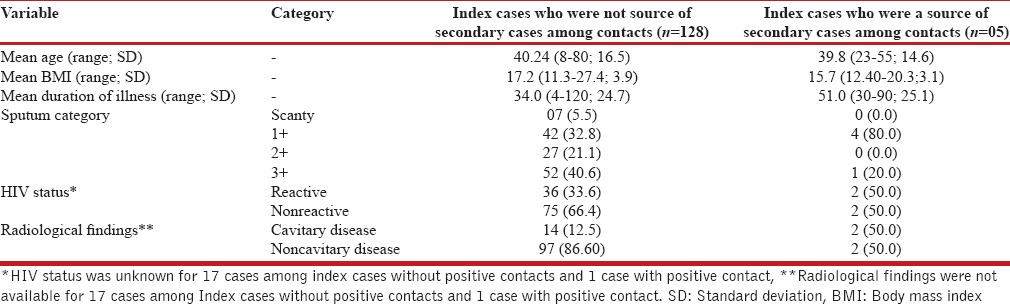
Table 4.
Comparative profile of symptomatic contacts
DISCUSSION
Present study showed that 3.45% (n = 18) of household contacts were symptomatic with symptoms suggestive of TB. One third of these symptomatic contacts were later diagnosed to have TB giving a prevalence of 1.15% among the household contacts of index cases. This amounts to an additional yield of 4.51% for the 133 index cases. This highlights that symptomatic household contact screening could be used as a prospective case detection tool. A prospective cohort study conducted in Uganda reported the detection of 6% secondary cases among the household contacts of index TB cases.[1] In another study conducted in Kenya, mothers attending maternal and child welfare clinics were interviewed for detecting TB suspects in their households. Mothers were asked to give letters to the suspects asking them to come to clinic for screening. This approach resulted in 4% of annual incidence of SS positive cases being detected with very few resources being expensed.[10] A source case investigation for children with TB disease in Pune, India also showed that opportunities for TB prevention and control were being missed because contact tracing is poorly implemented in India.[11]
Blok et al.[2] recently published a meta-analysis from 19 projects across Asia, Africa, and Middle-East. They reported a pooled yield of 1.5% (range: 0.1–6.2%) among the contacts screened and 1.8% of total cases being reported by means of contact investigation. They also concluded that background prevalence of TB and setting of project (rural/urban/mixed) results in variation of yield.
Our study suggests that index cases with contacts positive for TB had lower body mass index (BMI) (severe disease) and greater duration of illness as compared to index cases with all contacts negative for TB [Table 3].
Comparison of symptomatic contacts [Table 4] shows that those diagnosed with TB had lower BMI (mean 18.3 Kg/m2) when compared to those who did not have TB (mean 20.3 Kg/m2). The finding is in agreement with published literature. A prospective follow up study conducted in Iraq on household contacts of children under 15 years of age indicated that contacts diagnosed with TB had significantly lower BMI than those without TB.[12] Our study also showed that symptomatic contacts with diagnosed TB had comparatively longer duration of symptoms and greater duration of contact with index cases [Table 4]. These findings suggest that BMI, duration of symptoms and duration of contact with index cases could be important predictors for risk of TB among symptomatic contacts. Prevalence of smear positive TB in general population of India is about 75/100,000, which is far less than that among symptomatic contacts. Hence screening of asymptomatic contacts is likely to give a very low yield and does not appear to be a cost effective option. Nonetheless, wherever resources and infrastructure permits, one can consider screening of all contacts whether symptomatic or asymptomatic, limitation of present study is the relatively small sample size which precludes application of any statistical test to the data and evaluation of significance of individual risk factors for transmission of disease. Nonetheless, it provides considerable evidence for moderate additional yield of cases of TB by means of contact screening. The approach is practical since minimal resources are required to achieve this additional yield. Furthermore, the method offers the potential to approach the exposed contacts through their family members; since even today, there is an element of stigma attached with the disease. Systematic screening of household contacts of TB patients has been strongly recommended by the World Health Organization.[13]
There is evidence that risk of active TB among household contacts of active case subjects is very high[14] which indicates that investigating the symptomatic household contacts could provide a powerful approach to explore undiagnosed cases in the community. The focus on symptomatic contacts offers a cost effective alternative and the findings of this study suggest the need for more research to assess the cost effectiveness and large scale adoption of household contact tracing for detection of TB in India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Guwatudde D, Nakakeeto M, Jones-Lopez EC, Maganda A, Chiunda A, Mugerwa RD, et al. Tuberculosis in household contacts of infectious cases in Kampala, Uganda. Am J Epidemiol. 2003;158:887–98. doi: 10.1093/aje/kwg227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blok L, Sahu S, Creswell J, Alba S, Stevens R, Bakker MI. Comparative meta-analysis of tuberculosis contact investigation interventions in eleven high burden countries. PLoS One. 2015;10:e0119822. doi: 10.1371/journal.pone.0119822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sekandi JN, Neuhauser D, Smyth K, Whalen CC. Active case finding of undetected tuberculosis among chronic coughers in a slum setting in Kampala, Uganda. Int J Tuberc Lung Dis. 2009;13:508–13. [PMC free article] [PubMed] [Google Scholar]
- 4.Saunders MJ, Koh GC, Small AD, Dedicoat M. Predictors of contact tracing completion and outcomes in tuberculosis: A 21-year retrospective cohort study. Int J Tuberc Lung Dis. 2014;18:640–6. doi: 10.5588/ijtld.13.0486. [DOI] [PubMed] [Google Scholar]
- 5.Bayona J, Chavez-Pachas AM, Palacios E, Llaro K, Sapag R, Becerra MC. Contact investigations as a means of detection and timely treatment of persons with infectious multidrug-resistant tuberculosis. Int J Tuberc Lung Dis. 2003;7(12 Suppl 3):S501–9. [PubMed] [Google Scholar]
- 6.Maciel EL, Golub JE, Peres RL, Hadad DJ, Fávero JL, Molino LP, et al. Delay in diagnosis of pulmonary tuberculosis at a primary health clinic in Vitoria, Brazil. Int J Tuberc Lung Dis. 2010;14:1403–10. [PMC free article] [PubMed] [Google Scholar]
- 7.Shah SA, Qayyum S, Abro R, Baig S, Creswell J. Active contact investigation and treatment support: An integrated approach in rural and urban Sindh, Pakistan. Int J Tuberc Lung Dis. 2013;17:1569–74. doi: 10.5588/ijtld.13.0169. [DOI] [PubMed] [Google Scholar]
- 8.Yadav RP, Nishikiori N, Satha P, Eang MT, Lubell Y. Cost-effectiveness of a tuberculosis active case finding program targeting household and neighborhood contacts in Cambodia. Am J Trop Med Hyg. 2014;90:866–72. doi: 10.4269/ajtmh.13-0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deery CB, Hanrahan CF, Selibas K, Bassett J, Sanne I, Van Rie A. A home tracing program for contacts of people with tuberculosis or HIV and patients lost to care. Int J Tuberc Lung Dis. 2014;18:534–40. doi: 10.5588/ijtld.13.0587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aluoch JA, Oyoo D, Swai OB, Kwamanga D, Agwanda R, Edwards EA, et al. A study of the use of maternity and child welfare clinics in case-finding for pulmonary tuberculosis in Kenya. Tubercle. 1987;68:93–103. doi: 10.1016/0041-3879(87)90024-9. [DOI] [PubMed] [Google Scholar]
- 11.De D, Kinikar A, Adhav PS, Kamble S, Sahoo P, Koli H, et al. Source case investigation for children with TB disease in Pune, India. Tuberc Res Treat 2014. 2014:182836. doi: 10.1155/2014/182836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al Kubaisy W, Al Dulayme A, Hashim DS. Active tuberculosis among Iraqi schoolchildren with positive skin tests and their household contacts. East Mediterr Health J. 2003;9:675–88. [PubMed] [Google Scholar]
- 13.Geneva: World Health Organization; 2013. World Health Organization. Systematic Screening for Active Tuberculosis: Principles and Recommendations. [PubMed] [Google Scholar]
- 14.Becerra MC, Pachao-Torreblanca IF, Bayona J, Celi R, Shin SS, Kim JY, et al. Expanding tuberculosis case detection by screening household contacts. Public Health Rep. 2005;120:271–7. doi: 10.1177/003335490512000309. [DOI] [PMC free article] [PubMed] [Google Scholar]


