Abstract
Background:
In recent years, the incidence of cervical cancer has been rising, particularly in young adults, as the second most common gynecological cancer in China. The aim of this study was to explore the incidence change and the epidemiological characteristics of cervical cancer in Beijing over the past 16 years.
Methods:
All the cases of the study were limited to Beijing residents diagnosed with cervical cancer and registered in Beijing from January 1, 1993, to December 31, 2008. A total of 4100 patients with cervical cancer were obtained from the Statistics Database of Beijing Cancer Registry (BJCaR). According to the registered data, we retrospectively reviewed all original cases which we can acquired in reported hospital. Cervical situ cancer, cervical metastatic cancer, non-Beijing residents and repeatedly registered cases were excluded. Totally, 3641 registered cases were verified correctly. Meanwhile, we also collected the following data: Age, occupation, detected methods, histological type, and staging. The trends of incidence and mortality were analyzed by Joinpoint Regression Program 4.1.1.1 produced by National Cancer Institute (NCI, USA). The annual percent change (APC) was calculated using the Joinpoint regression model.
Results:
The crude rates of incidence and mortality were 10.4 and 1.0 per 100,000 women, respectively during 1993 to 2008. The average WHO age-standardized incidence rates were 11.5 per 100,000 women. There was a decrease in incidence annually by 8.0% (P = 0.3) during 1993–1996 and a rapid increase annually by 18.9% after 1999 (P < 0.01). The median age was 67 years in 1993, but the median age decreased to 45 years in 2008. The peak of the age-specific incidence curve was at 40 years in the most recent period (2005–2008), which was 25–30 years earlier than that in previous periods (1993–1996). In the 2224 cases, the numbers of patients with stage I, II, III and IV were 910 (40.9%), 601 (27%), 542 (24.4%), 171 (7.7%), respectively. The percentage of patients with stage I was 7.6% (13/171) in 1993–1996, but the percentage increased to 51.6% (643/1247) in 2005–2008 (P < 0.01). Otherwise the percentage of advanced stage (stage III–IV) during the same period was dropped down significantly from 52.0% (89/171) to 22.5% (280/1247) (P < 0.01). Unemployed and housewife ranked first accounting for 27.3% of the total (607/2224). Urban low-income people such as worker ranked the second accounting for 17.0% (377/2224), the third place was farmer accounting for 14.0% (312/2224). Only 381 (17.1%, 381/2224) women in 2224 were first detected cervical cancer by routine screenings. Company staff (36.5%, 139/381), professional and technical personnel (22.6%, 86/381), national official (22.0%, 84/381) occupied the top three (total 81.1%) in the 381 patients detected cervical cancer by screening.
Conclusions:
The cervical cancer incidence has showed a continuous rise in Beijing since 1999. Government-led mass screening should target the low socioeconomic population primarily. Meanwhile the government should enhance public health education of cancer screening to increase the rate of screening.
Keywords: Cervical Cancer, Diagnosis, Epidemiology, Screening
INTRODUCTION
Cervical cancer is one of the most common cancers among women worldwide: Third in incidence overall. According to the statistical data of international cancer research center, in 2008 approximately 530,000 women were newly diagnosed with cervical cancer throughout the world.[1] In China, cervical cancer is the second most common gynecological cancer. There were nearly 100,000 cases in China, accounting for approximately 1/5 of the world total new cases. Approximately 30,000 women die from the disease in China each year.[1,2] As a result of cervical cancer screening, the epidemiological reports from many developing countries suggest that the incidence of cervical cancer has declined since the nineteen sixties. In recent years, some researchers reported rising incidences in China, particularly in young adults.[3,4,5]
The cervical cancer incidence in Beijing was 46.4/100,000 in 1977. A government-led, in planned, mass cervical cancer screening and treatment project had carried out during 1977–1993 in Beijing. In total, 3,582,978 person-time women aged 35–70 years were screened during the 16 years. The screening rate was 13.01/100,000. The incidence dropped down to 2.23 per 100,000 women in 1992.[6] The project was stopped in 1993. How did the morbidity and mortality of cervical cancer fluctuate since 1993? What did the age-specific incidence change? What was the high-risk population in these years? Whether the cervical cancer staging spectrum has changed a lot in the past 16 years? Such a study would investigate whether cervical cancer staging spectrum has altered significantly in the past 16 years and the kinds of population at high-risk of cervical cancer.
The purpose of the population-based survey was to understand the incidence fluctuation and epidemiological characteristics of cervical cancer in Beijing in the past 16 years. By means of the analysis of the data (cervical cancer incidence, high-incidence-rate ages groups, high-risk crowds, pathological diagnosis, and staging) the valuable results would be provided to make effective and economical screening program for the government organizing large-scale cervical cancer screening in the future.
METHODS
Patients and population
The patients of the study were limited to Beijing residents diagnosed with cervical cancer and registered in Beijing from January 1, 1993, to December 31, 2008. The research source data were obtained from the Statistics Database of Beijing Cancer Registry (BJCaR). BJCaR is a population-based registry established in 1976 covering the entire population in Beijing. BJCaR has constantly collected cancer incident case data from all of hospital in Beijing, especially hospitals which provide cancer treatment. A total of 4100 patients with cervical cancer were registered from January 1, 1993, to December 31, 2008. According to the registered data, we retrospectively reviewed all original cases which we can acquired in reported hospital. Cervical situ cancer, cervical metastatic cancer, non-Beijing residents, and repeatedly registered cases were excluded. We totally excluded 459 cases. Totally, 3641 registered cases were verified eligible [Figure 1]. Meanwhile, we also collected the following data: Age, occupation, contraceptive method, detected methods, histological type (according to the International Classification of Diseases for Oncology), and staging (according to the criteria of the Federation of International Gynecology and Obstetrics [FIGO]). Patients were divided into the following age-group for analysis: Younger than 30, 30–39, 40–49, 50–59, 60–69, and 70 years or older.
Figure 1.
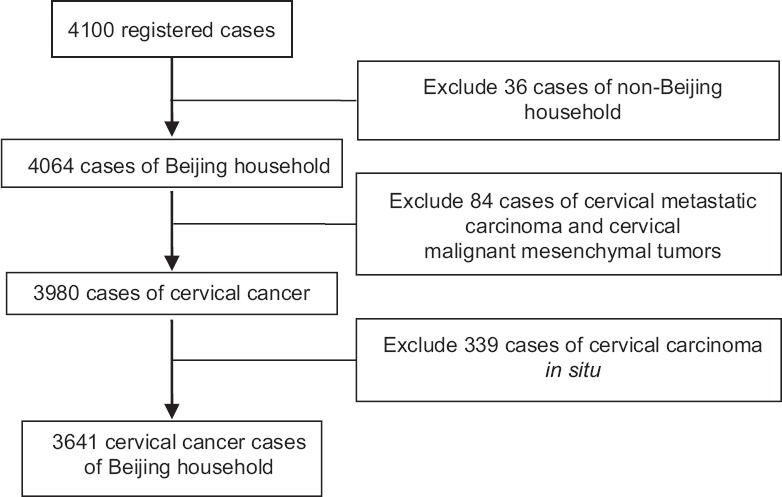
Flow chart of cases selected.
Population estimates were obtained from Beijing Statistical Information Net and Beijing Statistical Yearbook.[7,8] The standard rates were standardized by the WHO world standard population (WHO 2000–2025). The world (WHO 2000–2025) standard population data were obtained from the America National Cancer Institute.[9]
Statistical analysis
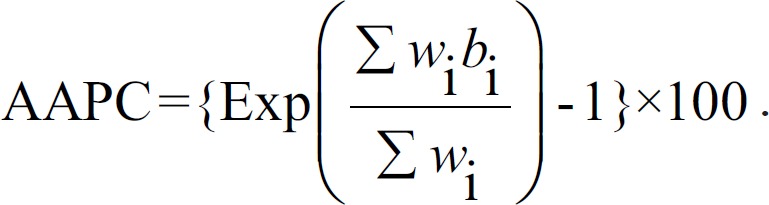
Descriptive and analytical approaches were used to analysis the data. The annual rude, standard, and age-specific incidence and mortality were calculated by the direct method using Excel 2003 (Microsoft Office 2003, Microsoft Corporation, USA). The trends of incidence and mortality were analyzed by Joinpoint Regression Program 4.1.1.1 produced by National Cancer Institute (NCI, USA).[10] The annual percent change (APC) was calculated using the Joinpoint Regression model. Rates that change at a constant percentage every year change linearly on a log scale. To estimate the APC for a series of data, the following regression model is used:
The APC from year y to year y + 1= [(Ry + 1 − Ry)/Ry × 100 = [eb0 + b1(y + 1) − eb0 + b1(y)]/eb0 + b1(y) ×100 = (eb1 − 1) ×100.
The average APC (AAPC) is a summary measure of the trend to describe the AAPCs over a period of multiple years. It is computed as a weighted average of the APC's from the Joinpoint model with the weights equal to the length of the APC interval.
The rest data were described and analyzed by the Statistical Package for the Social Sciences (Windows version 15.0; SPSS Inc., USA). Statistical tests used chi-square test and Kruskal–Wallis test. All tests were two-sided, and P values of <0.05 were considered statistically significant.
RESULTS
Overall trend
Between 1993 and 2008, there were total 3641 women diagnosed with invasive cervical cancer. The crude rates of incidence and mortality were 10.4 and 1.0 per 100,000 women, respectively, during 1993 to 2008. The average WHO age-standardized incidence rates were 11.5 per 100,000 women. Overall, there were significant increases in incidence and nonsignificant increases in mortality [Figure 2]. The WHO age-specific incidence rate was 8.76/100,000 in 1993, but the incidence increased to 23.1/100,000 in 2008. The APC was 11.0% (P < 0.001). The incidence trend graph [Figure 3] shows there was a decrease in incidence annually by 8.0% (P = 0.3) during 1993–1996 and a slow increase by 2.7% (P = 0.9) during 1996–1999. After 1999, the APC increased rapidly by 18.9% (P < 0.01). The speed has no significant change since 2006 [APC = −1.51%, P = 0.9, Table 1].
Figure 2.
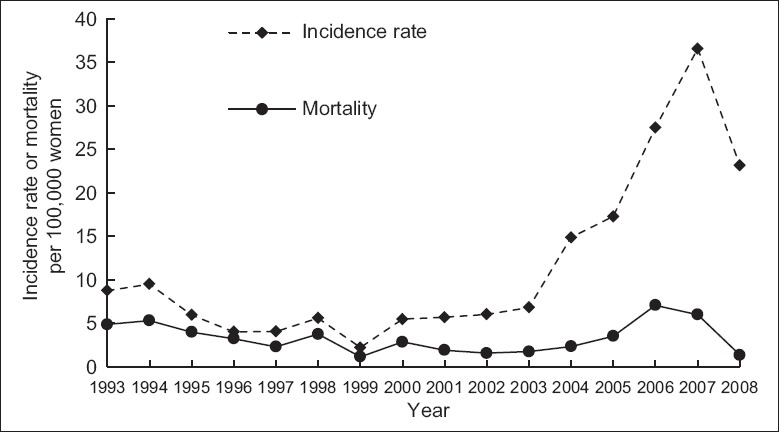
The WHO age-standardized incidence rate and mortality of cervical cancer in Beijing during 1993–2008.
Figure 3.
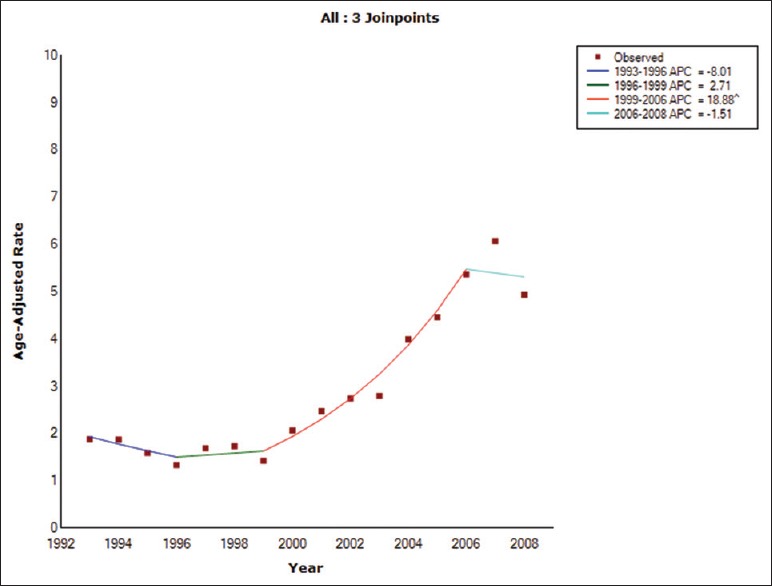
Incidence trend graph of cervical cancer in Beijing during 1993–2008. APC: Annual percent change.
Table 1.
Joinpoint incidence trend analysis of cervical cancer with the APC in Beijing during 1993–2008
| Segment | Lower endpoint (year) | WHO age-specific incidence (/106 women) | Upper endpoint (year) | WHO age-specific incidence (/106 women) | APC (%) | Lower CI | Upper CI | P |
|---|---|---|---|---|---|---|---|---|
| 1 | 1993 | 8.76 | 1996 | 4.73 | −8.0 | −25.6 | 13.7 | 0.3 |
| 2 | 1996 | 4.73 | 1999 | 9.22 | 2.7 | −31.3 | 53.5 | 0.9 |
| 3 | 1999 | 9.22 | 2006 | 27.48 | 18.9 | 13.5 | 24.6 | 0.0 |
| 4 | 2006 | 27.48 | 2008 | 23.14 | −1.5 | −20.7 | 22.3 | 0.9 |
CI: Confidence interval; APC: Annual percent change.
Incidence age trend
Age box figure of cervical cancer in Beijing [Figure 4] shows the two straight lines above and underrepresent the incidence age from 25% confidence interval (CI) to 75% CI every year. The horizontal lines in the middle of the box represent the median age. Figure 4 shows the incidence age overall declined during the 16 years. The median age was 67 years old in 1993, but the median age decreased to 45 years old in 2008. Figure 5 shows the change in age-specific incidence over the 16 years. The incidence in the age-group younger than 30 years was always very low and has no significant changes during the period. There was the most obvious increase in 40–49 years-group, second in 30–39 years-group after 2003. The incidence in 60–69 and 70 or older years-group has always been trending down. Figure 6 shows the change in age-specific incidence rates over the four periods. For the most recent period (2005–2008), the age-specific incidence curve shows a peak at 40 years, which was 25–30 years earlier than in previous periods (1993–1996).
Figure 4.
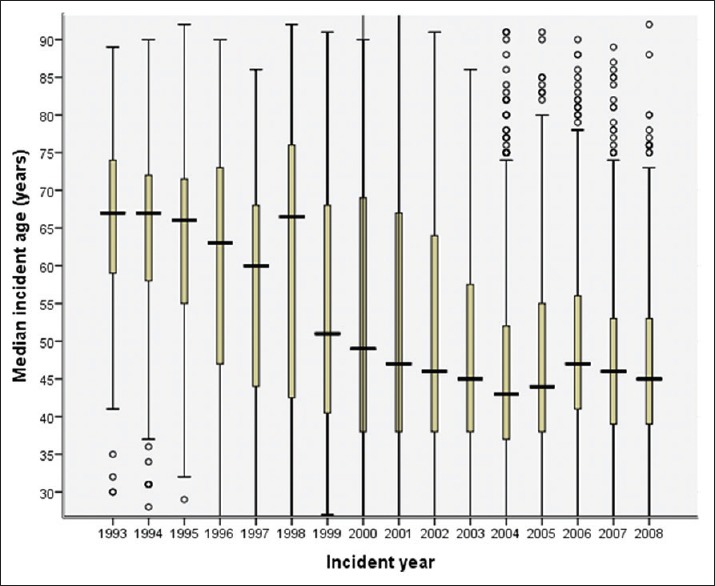
Age box figure of cervical cancer in Beijing.
Figure 5.
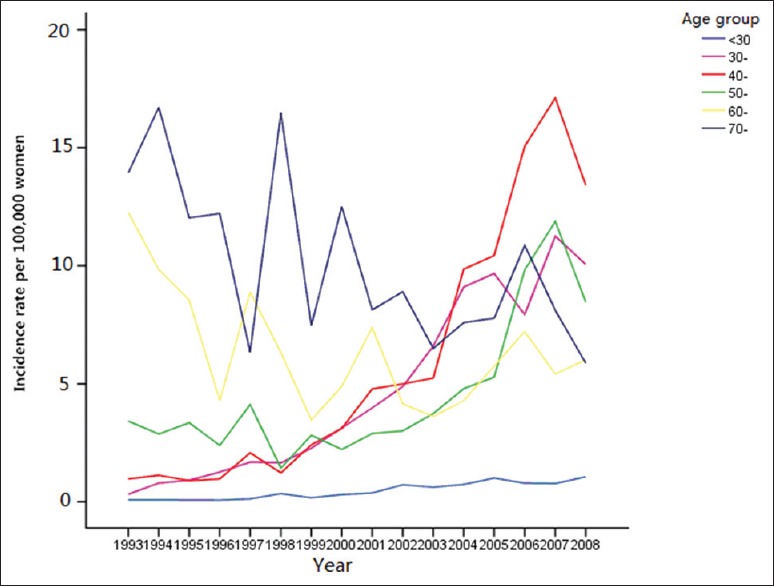
Age-specific incidence rates for cervical cancer in Beijing.
Figure 6.
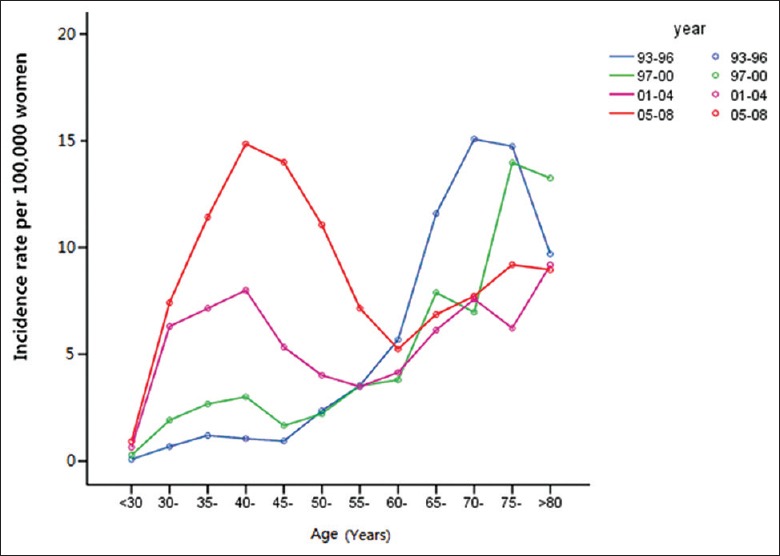
Incidence rates for cervical cancer in Beijing for 4 years period 1993–2008.
Diagnosis and staging
Among the 3641 cases, 342 cases (9.4%, 342/3641) had no pathologic diagnosis. The percentage of squamous carcinoma, adenocarcinoma, adenosquamous carcinoma, and undifferentiated/peculiar carcinoma were 70.4% (2564/3641), 12.2% (446/3641), 3.9% (141/3641), and 4.1% (148/3641), respectively. Mean age at onset of squamous carcinoma were 48.7 years old, adenocarcinoma were 48.4 years old, adenosquamous carcinoma were 43.4 years old, undifferentiated/peculiar carcinoma were 44 years old. The age at onset of adenosquamous carcinoma and undifferentiated/peculiar carcinoma were significantly younger than Squamous carcinoma and Adenocarcinoma (P < 0.01).
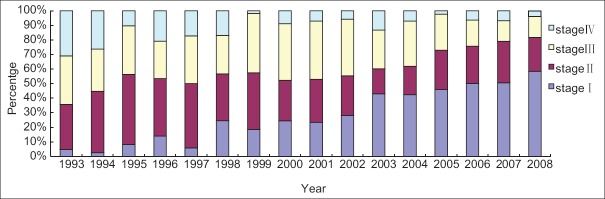
In the 2224 cases with FIGO staging record, the number of patients with Stage I, II, III, and IV were 910 (40.9%), 601 (27.0%), 542 (24.4%), and 171 (7.7%), respectively [Table 2]. The percentage of Stage I was 7.6% (13/171) in 1993–1996, but the percentage increased to 51.6% (643/1247) in 2005–2008 (P < 0.01). Otherwise, the percentage of advanced stage (Stage III–IV) during the same period was dropped down significantly from 52.0% (89/171) to 22.5% (280/1247) (P < 0.01). [Figure 7] shows the changes of cervical cancer staging spectrum from 1993 to 2008. Table 3 shows only 381 (17.1%, 381/2224) women in 2224 were first detected cervical cancer by routine screenings. 70.6% (269/381) patients of the 381 cases were Stage I when they were diagnosed, which was much more than nonscreening patients (Table 4, P < 0.01). The proportion of new cases detected by routine screening did not change in the 16 years.
Table 2.
Change of cervical cancer staging proportion in Beijing from 1993 to 2008
| Year | Stage (n, %) | Total | |||
|---|---|---|---|---|---|
| I | II | III | IV | ||
| 1993–1996 | 13 (7.6)* | 69 (40.4) | 52 (30.4)* | 37 (21.6)* | 171 |
| 1997–2000 | 48 (19.3) | 86 (34.5) | 88 (35.3) | 27 (10.8) | 249 |
| 2001–2004 | 206 (37.0) | 122 (21.9) | 183 (32.9) | 46 (8.3) | 557 |
| 2005–2008 | 643 (51.6)* | 324 (26.0) | 219 (17.6)* | 61 (4.9)* | 1247 |
| Total | 910 (40.9) | 601 (27.0) | 542 (24.4) | 171 (7.7) | 2224 |
*Chi-square test, P<0.01.
Figure 7.
Change of cervical cancer staging spectrum in Beijing from 1993 to 2008.
Table 3.
Analysis of first detection method in different years (n, %)
| Years | Routine screening | Nonscreening | All patients |
|---|---|---|---|
| 1993–1996 | 29 (17.0) | 142 (83.0) | 171 (100) |
| 1997–2000 | 43 (17.3) | 206 (82.7) | 249 (100) |
| 2001–2004 | 68 (12.2) | 489 (87.8) | 557 (100) |
| 2004–2008 | 241 (19.3) | 1006 (80.7) | 1247 (100) |
| Total | 381 (17.1) | 1843 (82.9) | 2224 (100) |
Table 4.
Analysis of first detection method in different stages (n, %)
| Stages | Routine screening | Nonscreening | All patients |
|---|---|---|---|
| I | 269 (70.6)* | 641 (34.8) | 910 (40.9) |
| II–IV | 112 (29.4) | 1202 (65.2) | 1314 (59.1) |
| Total | 381 (100) | 1843 (100) | 2224 (100) |
*Chi-square test, P<0.01
Incidence in different population
We found occupation information in 2224 cases. Unemployed and homemaker ranked first accounting for 27.3% of the total (607/2224). Urban low-income people such as worker ranked the second accounting for 17.0% (377/2224); the third place was farmer accounting for 14.0% (312/2224). All these low-income population accounted for 58.3% of total. Table 5 shows the staging distribution in different occupation of cervical cancer patients. 63.1% company staffs (151/248), 50.3% national civil servants (95/189), and 50.0% professional (49/98) were cases with Stage I. The proportion was far more than unemployed persons/housemaker (37.6%, 228/607), workers (30.2%, 114/377), and farmers (29.8%, 93/312) (P < 0.05). Company staff (36.5%, 139/381), professional and technical personnel (22.6%, 86/381), and national official (22.0%, 84/381) occupied the top three (total 81.1%) in the 381 patients detected cervical cancer by screening.
Table 5.
Stage constituent ratio of cervical cancer patients in different occupation (n, %)
| Occupation | Stage I | Stage II | Stage III | Stage IV | Total |
|---|---|---|---|---|---|
| Professionals | 49 (50.0) | 22 (22.4) | 22 (22.4) | 5 (5.1) | 98 |
| Company staff | 151 (60.9) | 52 (21.0) | 33 (13.3) | 12 (4.8) | 248 |
| Civil servants | 95 (50.3) | 46 (24.3) | 40 (21.2) | 8 (4.2) | 189 |
| Worker | 114 (30.2) | 106 (28.1) | 118 (31.3) | 39 (10.3) | 377 |
| Farmer | 93 (29.8) | 86 (27.6) | 97 (31.1) | 36 (11.5) | 312 |
| Service personnel | 37 (48.7) | 23 (30.3) | 11 (14.5) | 5 (6.6) | 76 |
| Unemployed and housemaker | 228 (37.6) | 179 (29.5) | 148 (24.4) | 52 (8.6) | 607 |
| Others | 143 (45.1) | 87 (27.4) | 73 (23.0) | 14 (4.4) | 317 |
| Total | 910 (40.9) | 601 (27.0) | 542 (24.4) | 171 (7.7) | 2224 |
DISCUSSION
The study was the epidemiological report based on incidence and population characteristic for cervical cancer. The scope of this study is population-based, covering different hospitals, different districts, and different social classes, rural, and urban. The cervical cancer incidence has showed a continuous rise in Beijing since 1999. WHO age-specific incidence rate was 8.76/100,000 in 1993, but the incidence increased to 23.1/100,000 in 2008. The AAPC increased rapidly by 18.9% during 1999 to 2006. Cervical cancer incidence trending toward younger women became more obvious. The data show that the average onset age has decreased, and the highest age peak has gone ahead about 25–30 years during the 16 years. There was the most obvious increase in 40 years-group, second in 30–40 years-group after 2003.
There are many reasons causing this situation. Sexual behavior and the increasing incidence of human papillomavirus (HPV) infection were important factors. HPV infection is the necessary pathogenesis of cervical carcinoma.[11,12] HPV is sexually transmitted and aspects of sexual behavior, and reproductive factors affect the risk of cervical intraepithelial neoplasia (CIN) and invasive cancer. These include number of sexual partners, age at first intercourse, early age at first full-term pregnancy. With the opening of the sexuality and the growth of the sexual freedom, the age of first intercourse has decreased, and the number of sexual partners increased. The investigation data from Beijing senior high school students in 1981 showed less than 1% teenagers aged 15–18 years old had sexual intercourse. The percentage rose to 3.1% in 2000.[13] A study in 2164 mean age 20.3 years old unmarried women in 2002 showed 17.1% had more than two sexual partners and only 8.7% often used condoms.[14] All these reasons have caused HPV infection rates to increase. Some research has reported the infection rate of HR-HPV (high-risk HPV) in Europe was 6.8–9.3% and the high-risk age was 18–30 years old.[15,16] A sampling survey of female HR-HPV infection in Beijing revealed that the rate of infection was 9.3%, which was similar to the previous result in Europe.[17,18]
Another important reason was related to cervical cancer screening. A government-led, in planned, large-scale cervical cancer screening and treatment project had carried out during 1977–1993 in Beijing. In total, 3,582,978 person-times women aged 35–70 years old had participated the screening project during the 16 years. The screening rate was 13.01/100,000. The incidence of cervical cancer dropped down from 46.4 per 100,000 women in 1977 to 2.23 per 100,000 women in 1992. The project was stopped in 1993. The incidence trend graph [Figure 3] shows there was a decrease in incidence annually by 8.0% during 1993–1996 and a slow increase by 2.7% (P = 0.9) during 1996–1999. After 1999, the APC increased rapidly by 18.9% (P = 0.0). The overall reduction in incidence in these earlier years (1993–1999) might be attributed to period and cohort effects. Not only cancer, but also the CIN can be found through the screening. The detection of precancerous lesions and the subsequent therapy blocked the progress forward invasive cancer so that the incidence can decrease efficiently. The effect usually appeared after several years of the mass screening. That is called cohort effect of mass screening. With the cohort effect disappearing, the incidence will go up again. The study showed there was the most obvious increase in 40–49 years-group, second in 30–39 years-group after 2003. These women aged 30–49 years after 2003 were just 20–39 year old 10 years ago, and they were in sexually active period over the 10 years (1993–2003). The women aged 20–30 years were high-risk group of HPV infection. Most of them did not enter into the mass cervical cancer screening project because they were younger than the minimum age-35 years old before 1993. Disappeared cohort effect may be one of the reasons leading to the increase of incidence.
Government-led mass screening can reduce the incidence efficiently, but the screening involved in whole adult women population need the government invest large amounts of money and labor input. If we chose the specific population scope to carry out cancer screening and aimed at the high-risk population, public health resource can play more important role.[19,20] The figure of age-specific incidence in Beijing shows the incidence in the age-group younger than 30 years was always far lower than other age-group and has no obvious changes over 16 years. The screening will become inefficient if the younger than 30 years old age-group is accepted into the mass screening project scope. So we suggest the appropriate age range of government-led mass screening is 30–70 years old.
The proportion of patients with Stage I have been increasing gradually during the past 16 years. With the growth of social, economic level and the improvement of medical security, more people see a doctor earlier due to all sorts of cancer symptoms. However, it can be seen from the data that unemployed people, workers, and farmers are major at-risk populations. The proportion of Stage III and Stage IV in the unemployed people, workers, and farmers was higher than that in other occupation. It was confirmed that the workers, farmers, and unemployed persons had higher proportions of invasive cervical carcinoma diagnosed at later stages than the company staff, professional personnel, and national official. This suggests that cervical cancer is not being detected and treated as early in the unemployed people, workers, and farmers as in other groups. Unemployed people, workers, and farmers mean the lower educational level, poorer income, and health condition. These people often do not have dependable medical insurance. They frequently lack education and understanding of the need for regular early cervical cancer screening. The company staff, professional and technical personnel, and national official occupied the top three (total 81.1%) in the patients who found cervical cancer by screening. They often have good educational background and a high level of disposable income, and dependable medical insurance as well. Most of them always get organized regular medical examinations every 1–2 years. Thus, when cervical cancer screening system guidelines are developed in the future, the risk factors of different economic populations must be considered. To improve the efficiency of screening, we should pay attention to these parts of people.[19,20,21] The government should carry out regular free screening for working class, unemployed, rural, and urban poor.
Screening has benefit to reduce the mortality.[19,20] Early cervical cancer can be detected by screening. The survival of early cancer is higher than advanced carcinoma so that the mortality can be decreased by screening. The data revealed 70.6% (269/381) patients were Stage I when they were detected by screening, which was much more than nonscreening patients. Unfortunately, the proportion of asymptomatic screening did not improve over the past 16 years. This suggests that people do not pay attention to regular screening. Continued strengthening of the health education for cervical cancer screening and increased public awareness is vital.
Malignant tumor laid huge financial burden to every family and society, especially to the low-income family. Cervical cancer screening can effectively detect this malignancy at an early stage and, therefore, help to reduce the morbidity and mortality. By targeting the population at increased risk of cervical cancer, the screening may be high efficient with reasonable cost. These results emphasize the importance of future cervical cancer prevention programs, including CIN and cervical cancer screening. Government-led mass screening should target the low socioeconomic population primarily in order to conform to cost-benefit principle. Meanwhile, the government should enhance public health education of cancer screening, for increasing the rate of screening.
Financial support and sponsorship
This work was supported by a grant from Beijing Municipal Science and Technology Commission (No. D09050703650902).
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors thank the staff of the Beijing Cancer Registry (BJCaR) and the follow-up team from the Department of Gynecological Oncology, Beijing Obstetrics and Gynecology Hospital Affiliated to Capital Medical University for their cooperation.
Footnotes
Edited by: Li-Shao Guo
REFERENCES
- 1.Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001;94:153–6. doi: 10.1002/ijc.1440. [DOI] [PubMed] [Google Scholar]
- 2.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Globocan 2008, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 10. 2010. [Last accessed on 2011 Jun 22]. Available from: http://www.globocan.iarc.fr .
- 3.Elliott PM, Tattersall MH, Coppleson M, Russell P, Wong F, Coates AS, et al. Changing character of cervical cancer in young women. BMJ. 1989;298:288–90. doi: 10.1136/bmj.298.6669.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jeng CJ, Phdl, Ko ML, Ling QD, Shen J, Lin HW, et al. Prevalence of cervical human papillomavirus in Taiwanese women. Clin Invest Med. 2005;28:261–6. [PubMed] [Google Scholar]
- 5.Manhart LE, Koutsky LA. Do condoms prevent genital HPV infection, external genital warts, or cervical neoplasia? A meta-analysis. Sex Transm Dis. 2002;29:725–35. doi: 10.1097/00007435-200211000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Liu FY. The report of cervial cancer mass screening in Beijing. Beijing Med J. 1996;18:30. [Google Scholar]
- 7.Population (2005-2008). Beijing Statistical Yearbook. Beijing Bureau of Statistics. [Last accessed on 2014 Sep 15]. Available from: http://www.bjstats.gov.cn/nj/main/2005-2008 .
- 8.Beijing Statistical Yearbook. Beijing: China Statistics Press; 1994-2004. Beijing Bureau of Statistics. [Google Scholar]
- 9.World (WHO 2000-2025) Standard. National Cancer Institute. [Last accessed on 2014 Sep 15]. Available from: http://www.seer.cancer.gov/stdpopulations .
- 10.Joinpoint Trend Analysis Software. National Cancer Institute. [Last accessed on 2014 Sep 10]. Available from: http://www.surveillance.cancer.gov/joinpoint/
- 11.Wheeler CM. Natural history of human papillomavirus infections, cytologic and histologic abnormalities, and cancer. Obstet Gynecol Clin North Am. 2008;35:519–36. doi: 10.1016/j.ogc.2008.09.006. vii. [DOI] [PubMed] [Google Scholar]
- 12.Scheurer ME, Tortolero-Luna G, Adler-Storthz K. Human papillomavirus infection: Biology, epidemiology, and prevention. Int J Gynecol Cancer. 2005;15:727–46. doi: 10.1111/j.1525-1438.2005.00246.x. [DOI] [PubMed] [Google Scholar]
- 13.Yu XM, Pan YP, Wang J. A comparative study on pubertal development and sexual behaviors among middle school students in Beijing and Tianjin (in Chinese) Chin J Sch Health. 2002;4:292–3. [Google Scholar]
- 14.Cheng Y, Kang H. Study of the influence factors on the adolescent's productive health (in Chinese) J Maternal Child Health Care Chin. 2002;17:744–6. [Google Scholar]
- 15.Petignat P, Faltin D, Goffin F. Age-related performance of human papillomavirus testing used as an adjunct to cytology for cervical carcinoma screening in a population with a low incidence of cervical carcinoma. Cancer. 2005;103:126–32. doi: 10.1002/cncr.21060. [DOI] [PubMed] [Google Scholar]
- 16.Bosch FX, Manos MM, Muñoz N, Sherman M, Jansen AM, Peto J, et al. Prevalence of human papillomavirus in cervical cancer: A worldwide perspective. International biological study on cervical cancer (IBSCC) Study Group. J Natl Cancer Inst. 1995;87:796–802. doi: 10.1093/jnci/87.11.796. [DOI] [PubMed] [Google Scholar]
- 17.Wu MH, Zhang SW, Zhang WY, Zhou BL, Xie Z, Wang JD, et al. Study on the relations between high risk human papillomavirus and cervical intraepithelial neoplasia in married women from Beijing (in Chinese) Chin J Epidemiol. 2010;31:133–7. [PubMed] [Google Scholar]
- 18.Wang X, Gu D, Lou B, Xu B, Qian F, Chen Y. Hospital-based prevalence of high-risk cervical HPV types infecting the general population and female sex workers in Huzhou, China. Int J Gynaecol Obstet. 2013;120:37–41. doi: 10.1016/j.ijgo.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 19.Anttila A, Ronco G, Clifford G, Bray F, Hakama M, Arbyn M, et al. Cervical cancer screening programmes and policies in 18 European countries. Br J Cancer. 2004;91:935–41. doi: 10.1038/sj.bjc.6602069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chiu WA, Jinot J, Scott CS, Makris SL, Cooper GS, Dzubow RC, et al. Human health effects of trichloroethylene: Key findings and scientific issues. Environ Health Perspect. 2013;121:303–11. doi: 10.1289/ehp.1205879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fahs MC, Plichta SB, Mandelblatt JS. Cost-effective policies for cervical cancer screening. An international review. Pharmacoeconomics. 1996;9:211–30. doi: 10.2165/00019053-199609030-00004. [DOI] [PubMed] [Google Scholar]