Abstract
Background
During adolescence diabetes creates a juncture of very complex disease management demands with developmental needs, including the striving of adolescents for greater autonomy. Parents' concerns and fears about the teen's diabetes self-management abilities during this time can heighten parental attachment behavior and affect the parents' ability to support autonomy development necessary for effective self-care. Maternal parenting processes may be especially important for those adolescents who have Type 1 diabetes because mothers are the primary caregivers.
Purpose
Based on attachment theory, the aim was to test a model of the influence of mother-adolescent developmental conflict, maternal separation anxiety, and maternal inhibition of autonomy and relatedness on cognitive autonomy and self-care of adolescents with Type 1 diabetes.
Method
A total of 131 families with an adolescent, ages 11-15, contributed data annually across three waves. Mothers and adolescents completed paper-and-pencil measures and two interaction scenarios that were coded by trained staff from audio-tapes. The adolescent also completed a structured interview and questionnaire to assess self-care.
Results
Maternal separation anxiety when adolescents were 11-15 years of age directly predicted cognitive autonomy at one year follow-up, and that cognitive autonomy was directly related to self-care one year later, but did not mediate between separation anxiety and self-care.
Conclusions
Future investigation of the influence of separation anxiety of parents on adolescent autonomy development is warranted, as well as the contribution of autonomy development to diabetes self-management behaviors of adolescents.
Keywords: Chronic Illness, Diabetes, Maternal Influences, Parenting, Adolescence, Anxiety
In the United States T1DM is the predominant type of diabetes in youth, affecting about 1 in every 400-600 youth (National Institute of Diabetes and Digestive Diseases, 2005). During adolescence diabetes control worsens and disease management self-care behaviors decline ( Urbach et al, 2005; Pasquier-Fediaevsky, Chwalow, the PEDIAB Collaborative Group, & Tubian-Rufi, 2005); this contributes to long term diabetes complications (Silverstein, et al., 2005), and evokes fear and anxiety in parents (Gonder-Frederick et al., 2006; Streisand, et al. 2005). Further, T1DM is complex and demanding and must be integrated with the adolescents' quest for greater autonomy. Parents' concerns and fears about the teen's diabetes self-management abilities during this time can heighten parental attachment behavior and affect the parents' ability to support autonomy development necessary for effective self-care.
In this study, we test an attachment model of adolescent cognitive autonomy development in T1DM. We examine maternal processes that can be heightened through strong activation of maternal attachment to assess their influence on autonomy and self-care. These processes include maternal separation anxiety, mother-adolescent conflict, and maternal behaviors in interaction with the adolescent. Maternal parenting processes may be especially important for those adolescents who have T1DM as mothers have responsibility for one-third of the diabetes management task for early adolescents (Drotar & Ievers, 1994), while fathers have responsibility on the average for less than one task (Dashiff, 2003).
Attachment Theory and Autonomy
Exploration, which includes seeking autonomy, is highly active in adolescents (Allen & Land, 1999). In contrast, parental attachment and caregiving behaviors are primed to be active when there is danger or threat, leading parents to sometimes be anxious and want to protect and seek proximity to the adolescent (Bowlby, 1973). This separation anxiety may lead to conflict and communication styles which inhibit the development of autonomy (George & Solomon, 1999).
Autonomy
Cognitive autonomy is the type of autonomy that is most congruent with positive outcomes during adolescence. Cognitive autonomy is based on the ability to utilize relationships productively in reasoning for oneself, while also developing self-reliance and initiative (Greenberger, 1984; Allen & Land, 1999). Cognitive autonomy has high relevance for diabetes self-care during adolescence (Dashiff & Bartolucci, 2002), yet developing such autonomy may be a particular challenge for these families, related to parental perceptions that their child is vulnerable (Mullins et al., 2007).
Few studies of autonomy in self-management of diabetes during adolescence have been conducted. Autonomy was assessed in two studies by independence in the assumption of diabetes management responsibility (Wysocki et al, 1996; Wysocki, et al., 2006b). Palmer et al. (2004), in contrast, addressed cognitive autonomy and found that mothers did not transfer diabetes responsibility to adolescents across the adolescent developmental period based on this type of autonomy development. This was problematic for metabolic control of diabetes.
Parental Separation Anxiety
The most significant normative separation beyond childhood is believed to occur during adolescence (Berman & Sperling, 1991). Illness of offspring is one of several stressful conditions that elicit parental attachment behavior (Feeney, 1999) and anxiety that can thwart effective maternal caregiving (George & Solomon, 1999). However, few studies have addressed separation anxiety of parents of adolescents (e.g. Bartle-Haring, Brucker, & Hock, 2002; Soenens, Vansteenkise, Drulez, & Goossens, 2006). Although no study of parental separation anxiety in parents of adolescents with chronic illness was located, one study revealed that higher maternal trait anxiety was associated with greater maternal involvement in T1DM management and poorer adolescent disease self-management (Cameron, Young, & Wiebe, 2007).
Parent-Adolescent Conflict
Although adolescents tend to want more freedom, parents tend to reason about granting autonomy from more conservative perspectives (Eccles, et al., 1991). T1DM may further lead parents to dwell more intensely on issues of compliance that can heighten parent-adolescent conflict (Hock, Eberly, Bartle-Haring, Ellwanger, & Widaman, 2001). Higher levels of family conflict as experienced by young adolescents with T1DM (Anderson, Miller, Auslander, & Santiago, 1981; Hauser et. al, 1990; Miller-Johnson, 1994) and greater mother-daughter conflict (Bobrow, Avruskin, & Siller, 1985) have been associated with poorer self-care adherence.
Parent-Adolescent Interaction
Controlling communication that discounts or undermines adolescent autonomy is commonly identified as a problem in studies of adolescent's perceptions of parent-adolescent interactions about diabetes management (e.g., see Dashiff, Hardeman, & McLain, 2008),). Studies of the associations of observed parent-adolescent interaction with disease management outcomes in adolescents with T1DM are sparse, but indicate an association of parent-adolescent interaction with treatment adherence (Miller and Drotar, 2007; Wysocki et al., 2006a).
The Current Study
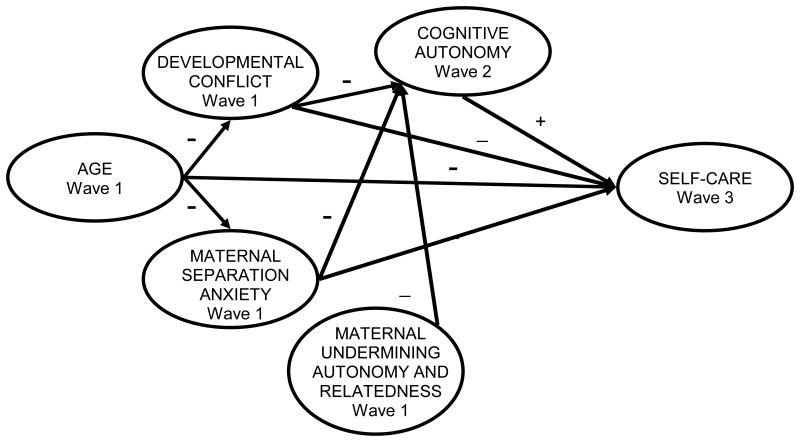
The primary aim was to test a model of the influence of maternal attachment processes on cognitive autonomy and self-care of adolescents with T1DM. Age was included in the model as a variable that could affect maternal processes and self-care. We hypothesized that (a) mothers' separation anxiety and developmental conflict with the adolescent would decrease with increased adolescent age, while adolescent self-care would worsen with increased adolescent age; (b) higher maternal separation anxiety, and developmental conflict with the adolescent would result in lower adolescent cognitive autonomy and self-care; (c) maternal behaviors inhibiting autonomy and relatedness in interactions would result in lower cognitive autonomy, and (d) relationships of maternal separation anxiety and developmental conflict with adolescent self-care would be mediated by adolescent cognitive autonomy. These hypotheses are reflected in the model depicted in Figure 1.
Figure 1. Full (Hypothesized) Causal Structural Equation Model. For these paths of interest, “+” indicates a positive expected value, “-” indicates a negative expected value.
Method
Sample and Procedures
Adolescents and their parents were recruited from a regional endocrinology clinic within a children's hospital in United States. Inclusion criteria were: (1) adolescents were between 11 and 15 years of age, (2) and diagnosed with T1DM for over a year, (3) the family must have lived together during the prior year, and (4) have facility with the English language sufficient to complete the study. Families were excluded if either the parent or teen had psychiatric symptomatology or developmental disability that would interfere with completion of the study. Data were collected in three annual waves.
A total of 161 families completed the first wave of data collection. The enrollment rate was 53% of those who were eligible. Wave 2 was completed by 129, and Wave 3 by 117 families. Overall attrition was 28% across two years. The primary reason given for not continuing in the study was that families did not have the time required to complete the measures. Attrition analysis indicated no significant differences between subjects who completed the study and those lost to attrition on demographic or study variables, other than that more female adolescents were lost to follow-up than males.
The research protocol was approved by a university institutional review board. Informed consent was obtained prior to screening for eligibility during a clinic visit. Data collection took place in the family home; adolescents and parents separately completed a series of paper-and-pencil measures, the adolescent completed a separate private interview, and parents and adolescents together participated in two audio-taped family interaction tasks, which were based on revealed difference tasks (Strodtbeck, 1951) focused on a diabetes issue (Rubin, Young-Hyman & Peyrot, 1989) and a developmental conflict (Prinz, Foster, Kent, & O'Leary, 1979). Each family received $120 equally divided among the participants.
Measures
Cognitive autonomy
The Individual Adequacy Subscale (IAS) of the Psychosocial Maturity Inventory (PMI)-Form B (Greenberger & Bond, 1984), was used to assess cognitive autonomy (Greenberger and Sorenson, 1974; Greenberger, 1984). The scale has good internal consistency reliability (Dashiff & Bartolucci, 2002) and support for predictive, concurrent and discriminant validity (Gavazzi, Anderson & Sabatelli, 1993; Greenberger, Josselson, Knerr & Knerr, 1975). Internal consistency of the total scale in the present study was .93.
Developmental conflict
The Issues Checklist (IC; (Prinz, Foster, Kent & O'Leary, 1979) was administered to mothers to assess the perceived conflict with the adolescent. The measure has good internal consistency reliability and validity (e.g., Grace, Kelley, & McCain, 1993; Robin & Foster, 1989; Robin & Weiss, 1980). In the current study, internal consistency reliability was Cronbach's alpha of .89 for mothers.
Inhibiting autonomy and relatedness
The Autonomy and Relatedness Coding System (ARCS; Allen et al., 1996) was used to code autonomy inhibiting and relatedness inhibiting maternal behaviors in interactions between parents and adolescents. The scale demonstrates acceptable interrater reliability (Allen et al., 1996) and construct validity (Allen et al, 1994; Allen & Hauser, 1996). In the present study the Pearson's correlation for two raters was .82 (p<.0001) and .75 (p<.0001) for mothers' inhibiting autonomy and inhibiting relatedness, respectively.
Maternal separation anxiety
The Parental Separation Anxiety Scale (PSAS; Dashiff & Weaver, 2008), was administered to mothers. The PSAS demonstrates good internal consistency reliability, short-term stability, and predictive validity (Dashiff & Weaver, 2008). Cronbach's alpha for the present study was .92.
Self-care
Two measures were completed by the adolescent. The Self-Care Adherence Inventory (SCAI), a structured interview, was administered to measure the adherence to diabetes-related self-care activities (Hanson et al., 1996). The SCAI demonstrates good interrater and test-retest reliability, and predictive validity (e.g., Hanson, Henggeler, Harris, Burghen, & Moore, 1989; Hanson et al, 1992; Hanson et al., 1996). In the present study trained interviewers achieved 100% accuracy in recording responses to the highly structured guided format prior to data collection and retained this accuracy through periodic monitoring. The Denyes Self-Care Practice Instrument (DSCPI; Denyes, 1988), a self-report questionnaire was administered to assess health-related self-care. The measure demonstrates good internal consistency reliability (Dashiff, 1997; McCaleb & Edgil, 1994) and construct validity (Frey & Denyes, 1989). The Cronbach's alpha for the DSCPI was .84 in the present study.
Data Analyses
Potential background covariates were determined from a review of the literature and subsequent assessment of associations of age, gender, ethnicity, socioeconomic status, family structure, and diabetes duration with the outcome variable of self-care. Only age was significant and was included in the subsequent analysis. Paths were identified from age to variables in the model based on results of studies reported in the literature and previous studies by the investigators. Structural equation modeling (SEM) was applied because it permits simultaneous investigation of relationships between latent constructs comprised of multiple measures and directly observed variables while minimizing the effect of measurement error. SEM also permits relationships to emerge that may not be obvious in bivariate analyses due to suppressor effects.
Descriptive statistics and correlations were calculated using SPSS 12.0 (SPSS, 2002) and SEM was performed using LISREL 8.5 (Jöreskog & Sörbom, 1993). The longitudinal design was used to better explicate the causal relationships among factors over time. Age, maternal separation anxiety, mother-adolescent developmental conflict, and maternal undermining of autonomy and relatedness were extracted from Wave 1. Cognitive autonomy, a potential mediator, was extracted from Wave 2. Self-care was extracted from Wave 3. Cases were included if they had both Wave 1 data and either Wave 2 or Wave 3 data points. If data were missing for Wave 1, their corresponding Wave 2 or Wave 3 data were used, whichever one of these waves had the data and was most proximal to Wave 1. If data were missing for Wave 2, the average between Wave 1 and Wave 3 was used instead. If Wave 3 data were missing, then their corresponding Wave 2 data were used instead. This yielded a sample of 131 participants of which only 4.1% of data points were missing and imputed, which is below the 5% limit that is considered acceptable for data analysis (Little & Rubin, 1987).
Observed variables were used in the model for maternal separation anxiety, mother-adolescent developmental conflict, and cognitive autonomy. Latent variables were extracted for maternal undermining autonomy and relatedness across developmental and diabetes interactions (UA1, UA2, UR1, UR2) and adolescent selfcare (SCAI and DSCPI). The full causal model shown in Figure 1 was tested. Separation anxiety, developmental conflict, and cognitive autonomy were modeled as possible mediators of the effects of age on self-care. Cognitive autonomy was evaluated as a mediator of the effects of separation anxiety and developmental conflict on self-care.
To compare the fit of the models, standard fit indices were used, including goodness-of-fit (GFI) index and the adjusted goodness-of-fit (AGFI) index. A model is considered to fit the data well if the value of GFI or AGFI is equal to or exceeds 0.90. Other indices were used to judge parsimony and support these primary goodness-of-fit indices. The overly conservative chi-square test was used as the conventional overall test of fit (Jöreskog & Sörbom, 1993). T tests of the significance of each estimated path were examined, and non-significant paths were subsequently fixed to zero to improve parsimony and model fit. Standard Pearson correlations were estimated between the pairs of variables to estimate significance; however, the correlations were generated by LISREL. Violations of multivariate normality were explored. Skewness and kurtosis were detected; therefore, the data were analyzed by normalizing the data using the LISREL transformation option to correct for this (Jöreskog & Sörbom, 1993). Maximum likelihood was used to allow for all fit indices to be produced (Jöreskog & Sörbom, 1993). A covariance matrix generated from this procedure was used in SEM analysis.
Results
General descriptive characteristics of the sample of 131 participants are displayed in Table 1. Table 2 shows the correlation matrix for the variables. Anderson and Gerbing (1988) specified that SEM analysis should proceed in a logical sequence—baseline model, full causal (hypothesized) model, and trimmed model. First, the baseline model was constructed to confirm the stability of the latent variables, which were free to load on each other. All latent variables had significant loadings, meaning that stable latent variables were created and were appropriate to use in subsequent analyses (See Table 3).
Table 1. Demographics and Overall Score of Participants (n = 131).
| Variable | Number (%) | M (SD) | Range |
|---|---|---|---|
| Adolescent Gender | |||
| Male | 70 (53%) | ||
| Female | 61 (47%) | ||
| Adolescent Ethnicity | |||
| African American | 24 (18) | ||
| White | 108 (82%) | ||
| Adolescent Adolescent Age (years) | 12.82 (1.48) | 11 – 15 | |
| Maternal Separation Anxiety | 65.54 (14.71) | 34 – 102 | |
| Mother-Adolescent Developmental Conflict | 2.18 (0.82) | 0.44- 4.52 | |
| Adolescent Cognitive Autonomy | 9.07 (0.92) | 5.58 – 10.95 | |
| Maternal Undermining Autonomy 1 | 2.06 (1.32) | 0 – 5.5 | |
| Maternal Undermining Autonomy 2 | 1.76 (1.30) | 0 – 5 | |
| Maternal Undermining Relatedness 1 | 0.72 (0.74) | 0 – 3.25 | |
| Maternal Undermining Relatedness 2 | 0.64 (0.71) | 0 – 3.75 | |
| Adolescent Diabetes-Related Self-Care | 25.67 (5.11) | 12 – 36 | |
| Adolescent Health-Related Self-Care | 75.01 (11.40) | 39.44 – 96.78 |
Table 2. Correlation Matrix Using Defined Variables from PRELIS.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Adolescent Age | |||||||||
| 2. Mother-Adolescent Developmental Conflict | -0.16† | ||||||||
| 3. Maternal Separation Anxiety | -0.24‡ | 0.05 | |||||||
| 4. Adolescent Cognitive Autonomy | -0.08 | 0.28‡ | -0.22† | ||||||
| 5. Maternal Undermining Autonomy 1a | 0.04 | 0.11 | 0.07 | 0.17‡ | |||||
| 6. Maternal Undermining Autonomy 2b | 0.03 | 0.24‡ | 0.01 | 0.31‡ | 0.58‡ | ||||
| 7. Maternal Undermining Relatedness 1a | -0.27‡ | 0.05 | -0.03 | 0.01 | 0.01 | -0.05 | |||
| 8. Maternal Undermining Relatedness 2b | 0.13 | -0.11 | -0.01 | -0.09 | 0.01 | 0.17 | -0.22† | ||
| 9. Adolescent Diabetes-Related Self-Care | -0.28‡ | -0.00 | 0.04 | 0.09 | 0.05 | 0.02 | 0.04 | 0.06 | |
| 10. Adolescent Health-Related Self-Care | -0.08 | -0.04 | 0.03 | 0.04 | 0.04 | 0.11 | 0.03 | 0.22† | 0.36‡ |
Developmental issue
Diabetes management issue
p < .05.
p < .01
Table 3. Fit Measures of Baseline, Causal, and Trimmed Models.
| χ2(df) | GFI | AGFI | PGFI | RMR | RMSEA | NFI | PNFI | RFI | |
|---|---|---|---|---|---|---|---|---|---|
| Baseline Model | 40.47 (24) | 0.94 | 0.86 | 0.41 | 0.06 | 0.08 | 0.79 | 0.42 | 0.61 |
| Full Causal Model | 51.46 (30) | 0.93 | 0.86 | 0.50 | 0.08 | 0.08 | 0.73 | 0.49 | 0.60 |
| Trimmed Model | 54.42 (33) | 0.92 | 0.87 | 0.55 | 0.08 | 0.07 | 0.72 | 0.53 | 0.62 |
Note. AGFI = Adjusted Goodness-of-Fit Index; df = degrees of freedom; GFI = Goodness-of-Fit Index; NFI = Normed Fit Index; PGFI = Parsimony Goodness-of-Fit Index; PNFI = Parsimony Normed Fit Index; RFI = Relative Fit Index; RMR = Standardized Root Mean Residual; RMSEA = Root Mean Square Error of Approximation; χ2= Chi-Square.
An independence model was tested and rejected, χ2 (45, N = 131) = 193.24, p < 0.001. The baseline model was tested next, and fit was improved, χ2 (24, N = 131) = 40.47, p < 0.001. A chi-square difference test revealed the improvement in fit was signficant, χ2diff (21, N = 131) = 152.97, p < 0.001. Testing of the full causal model (Figure 1) indicated a significant improvement in the fit relative to the independence model, χ2diff (15, N = 131) = 141.79, p < 0.001. A trimmed model (See Figure 2) was created by removing nonsignficant paths one at a time (based on the lowest t value) and recalculating model fit and parameters until only statistically significant paths remained in the model (p < 0.05).
Figure 2. Trimmed Structural Equation Model Predicting Self-Care (standardized solution). All solid lines represent significant paths (p < .05). Dotted lines represent hypothesized paths that were not significant.
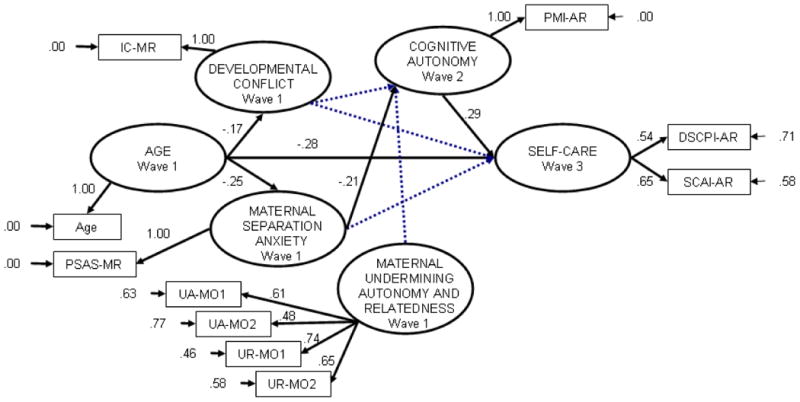
As can be seen by the standard fit indices (e.g., GFI = .92) in Table 3, the trimmed model also provided good fit to the observed data χ2 (33, N = 131) = 54.42, p < 0.001. A chi-square difference test with the full causal model revealed the improvement in fit was significant, χ2diff (3, N = 131) = 2.96, p < 0.05. The correlation between the causal model and the trimmed model estimates (Ullman, 1996) was strong (r = 0.99), indicative of stable parameter estimates for the statistically significant paths after deleting the non-significant paths. Modification indices for the trimmed model did not fit the model conceptually and were disregarded.
The final trimmed model demonstrated that age, maternal separation anxiety, and cognitive autonomy contributed to self-care. Age exerted a direct influence on developmental conflict (standardized coefficient = -0.17); specifically, the older the adolescent, the less conflict mothers reported. Age also had a direct relationship to maternal separation anxiety (standardized coefficient = -0.25) and self-care (-0.28); the older the adolescent, the less maternal separation anxiety and adolescent self-care were reported. Maternal separation anxiety had a direct relationship with cognitive autonomy (-0.21); those who reported less maternal separation anxiety had adolescents who exhibited higher levels of cognitive autonomy. Finally, cognitive autonomy had a direct relationship to self-care (0.29); those adolescents who reported more cognitive autonomy exhibited higher levels of self-care. The indirect causal path from age to self-care through maternal separation anxiety and cognitive autonomy (0.02) was not significant; neither was the indirect causal path from maternal separation anxiety to self-care (-0.06). The trimmed model explained 15% of the variance in self-care.
Discussion
The purpose of this study was to determine whether certain attachment-related parental processes inhibited one type of autonomy, termed cognitive autonomy, and whether cognitive autonomy contributed to self-care and mediated the relationship of parental processes with self-care. Our findings indicated that only maternal separation anxiety when adolescents were 11-15 years of age directly predicted cognitive autonomy at one year follow-up, and that cognitive autonomy was directly related to self-care one year later, but did not mediate between maternal separation anxiety and self-care over this longitudinal period. These findings are congruent with Allen et al. (1994), who suggested that parents who are more preoccupied with attachment relationships may have the most difficulty with their adolescents' autonomy, and Cameron et al. (2007), who found maternal trait anxiety was associated with autonomous motivation of older adolescents with T1DM.
Significant declines in parent-adolescent conflict of more usual and developmental nature based on adolescent age were found in this study. These findings are consistent with findings from a meta-analysis of studies of conflict between parents and adolescents without diabetes across adolescence, which demonstrated that developmental conflict was highest between parents and10-12 year old youth and decreased during the 13-15 year age span (Laursen, Coy, & Collins, 1998). Moreover, in other analyses we found mothers' reports of developmental conflict with their teens with T1DM were quite similar to those of mothers of adolescents without chronic illness (Viikinsalo, Crawford, Kimbrel, Long, & Dashiff, 2005). The absence of a relationship of these more mundane day to day conflicts in the lives of adolescents and their mothers with cognitive autonomy indicates that these household disagreements over such things as doing chores and getting along with siblings may not provide sufficient challenge to affect cognitive autonomy development at this earlier stage of adolescence. These usual conflicts may also not be useful indicators of heightened activation of maternal attachment.
Our failure to find a relationship of maternal undermining autonomy and relatedness with cognitive autonomy is especially noteworthy. There are several possible interpretations of this unexpected result. Firstly, some teens with diabetes may view undermining behaviors as an indication of parental caring rather than intrusion (Kyngas & Barlow, 1995; McElhaney and Allen, 2001). Second, we did not examine maternal behaviors that supported autonomy and relatedness. Thus, undermining autonomy and relatedness by mothers in this study may have been outweighed by autonomy supportive behaviors, explaining our failure to find significance of undermining behaviors in the overall model. The overall context of the parent-teen relationship should be taken into account in future studies. Third, fathers may have a greater role in the development of autonomy than mothers (Allen et. al., 1994; Allen & Hauser, 1991). Therefore, whether fathers' undermining behaviors influence adolescent autonomy development and self-care also deserves exploration.
Parental separation anxiety, conflict, and self-care adherence were directly predicted by adolescent age, indicating developmental trends in these processes through adolescence. In contrast, parental undermining of autonomy and relatedness were not responsive to age, suggesting stability of these behaviors across early adolescence, at least among adolescents with T1DM. Declining maternal separation anxiety and declining mother-adolescent developmental conflict may indicate a potential for improved maternal well-being as adolescents with T1DM get older. Although cognitive autonomy did not mediate between parental variables and self-care, it was directly related to self-care, supporting its relevance for health outcomes among adolescents with T1DM. The failure to find a mediating relationship of cognitive autonomy in this study may be related to the measure of cognitive autonomy which was not domain specific to illness management and self-care issues.
The trimmed model explained only 15% of the variance in self-care based on adolescent age, parental separation anxiety, and cognitive autonomy. This indicates that other variables that were not included in the model may be important in considering how autonomy and self-care are enhanced during adolescence and their inclusion may produce a more robust model. Other variables indicated in the literature include adolescent variables, such as self-efficacy (Grey, Boland, Yu, Sullivan-Bolyai, & Tamborlane, 1998), and illness representations (Skinner, Hampson, & Fife-Schaw, 2002), and parental variables, such as maternal autonomy supportiveness and self-efficacy (Leonard, Skay, & Rheinberger, 1998). Moreover, this analysis addressed only maternal processes and one aspect of autonomy development. While cognitive autonomy has been associated with advances in maturity among youth, the role of other types of autonomy in mediating between parenting processes and self-care should be investigated (Ryan & Lynch, 1989), as well as the role of these processes in models of father-adolescent relationships. Finally, the study findings are limited by the sample size and imputation of missing data. However, the results indicate that parental separation anxiety and cognitive autonomy warrant further study during the adolescent period as contributors to self-management of a chronic illness.
Key Messages.
Mothers who are more anxious about separation from their young adolescent with Type 1 diabetes may have more difficulty stimulating cognitive autonomy.
Separation anxiety among mothers of young adolescents with diabetes may be germane to the development of adolescent autonomy.
Associations of maternal separation anxiety and parent-adolescent conflict about developmental issues with adolescent age may indicate potential for improved well-being.
Future research should focus on autonomy-supportive maternal behavior as a predictor of cognitive autonomy.
Interventions to stimulate cognitive autonomy of adolescents with Type 1 diabetes may enhance self-care.
Acknowledgments
This research was supported by grant NR04948 from NIH/NINR awarded to Dashiff.
Contributor Information
Carol Dashiff, Email: dashiffc@uab.edu, NB 323, School of Nursing, University of Alabama at Birmingham, 1530 3rd Ave. South, Birmingham, AL 35294-1210, (205) 996-6110.
David Vance, Hussein Abdullatif, MD, Associate Professor, Jan Wallander, PhD, Professor, University of Alabama at Birmingham.
Reference List
- Allen JP, Hauser S. Predictions of adult attachment representations, psychological distress, and competence from family interactions in adolescence. Paper presented at the 1991 meeting of the Society for Research in Child Development; Kansas City, MO. 1991. [Google Scholar]
- Allen JP, Hauser ST. Autonomy and relatedness in adolescent-family interactions as predictors of young adults' states of mind regarding attachment. Development and Psychopathology. 1996;8:793–809. [Google Scholar]
- Allen JP, Hauser ST, Bell KL, O'Connor TG. Longitudinal assessment of autonomy and relatedness in adolescent-family interactions as predictors of adolescent ego development and self-esteem, Child Development. 1994;65:179–194. doi: 10.1111/j.1467-8624.1994.tb00743.x. [DOI] [PubMed] [Google Scholar]
- Allen JP, Hauser ST, O'Connor TG, Bell KL, Eickholt C. The connection of observed hostile family conflict to adolescents' developing autonomy and relatedness with parents. Development and Psychopathology. 1996;8:425–442. [Google Scholar]
- Allen JP, Land D. Attachment in adolescence. In: Cassidy J, Shaver PR, editors. Handbook of attachment: Theory, research, and clinical applications. New York: Guilford Press; 1999. pp. 319–355. [Google Scholar]
- Anderson BJ, Miller JP, Auslander W, Santiago J. Family characteristics of diabetic adolescents: Relations to metabolic control. Diabetes Care. 1981;4:586–594. doi: 10.2337/diacare.4.6.586. [DOI] [PubMed] [Google Scholar]
- Anderson JC, Gerbing DW. Structural equation modeling in practice: a review and recommended two-step approach. Psychological Bulletin. 1988;103:411–423. [Google Scholar]
- Bartle-Haring S, Brucker P, Hock E. The impact of parental separation anxiety on identity development in late adolescence and early adulthood. Journal of Adolescent Research. 2002;17:439–450. [Google Scholar]
- Berman WH, Sperling MB. Parental attachment and emotional distress in the transition to college. Journal of Youth and Adolescence. 1991;20:427–440. doi: 10.1007/BF01537184. [DOI] [PubMed] [Google Scholar]
- Bobrow ES, Avruskin TW, Siller J. Mother-daughter interaction and adherence to diabetes regimens. Diabetes Care. 1985;8:146–151. doi: 10.2337/diacare.8.2.146. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss: Vol 2 Attachment. New York: Basic Books; 1973. [Google Scholar]
- Cameron LD, Young MJ, Wiebe DJ. Maternal trait anxiety and diabetes control in adolescents with type 1 diabetes. Journal of Pediatric Psychology. 2007;32:733–744. doi: 10.1093/jpepsy/jsl053. [DOI] [PubMed] [Google Scholar]
- Dashiff C. Parents' perceptions of the impact on the family of diabetes in adolescent daughters. Journal of Pediatric Nursing. 1993;8:361–369. [PubMed] [Google Scholar]
- Dashiff CJ. Self- and dependent-care responsibility of adolescents with IDDM and their parents. Journal of Family Nursing. 2003;9:166–183. [Google Scholar]
- Dashiff CJ. Young adolescents with IDDM: Family processes, autonomy development and health. Quality Nursing. 1997;3:19–28. [Google Scholar]
- Dashiff C, Bartolucci A. Autonomy development in adolescents with Insulin Dependent Diabetes Mellitus. Journal of Pediatric Nursing. 2002;17:96–105. doi: 10.1053/jpdn.2002.124127. [DOI] [PubMed] [Google Scholar]
- Dashiff C, Hardeman T, McLain R. Parent-adolescent communication and diabetes: An integrative review. Journal of Advanced Nursing. 2008;62:140–162. doi: 10.1111/j.1365-2648.2007.04549.x. [DOI] [PubMed] [Google Scholar]
- Dashiff CJ, Weaver M. Development and Testing of a Scale to Measure Separation Anxiety of Parents of Adolescents. Journal of Nursing Measurement. 2008;16 doi: 10.1891/1061-3749.16.1.61. in press. [DOI] [PubMed] [Google Scholar]
- Denyes MJ. Orem's model used for health promotion: Directions for research. Advances in Nursing Science. 1988;11:13–21. doi: 10.1097/00012272-198810000-00003. [DOI] [PubMed] [Google Scholar]
- Drotar D, Ievers C. Age differences in parent and child responsibilities for management of cystic fibrosis and insulin-dependent diabetes mellitus. Journal of Developmental and Behavioral Pediatrics. 1994;13:265–272. [PubMed] [Google Scholar]
- Eccles JS, Buchanan CM, Flanagan C, Fulgini A, Midgley C, Yee D. Control versus autonomy during early adolescence. Journal of Social Issues. 1991;47:53–68. [Google Scholar]
- Feeney JA. Adult romantic attachment and couple relationships. In: Cassidy J, Shaver PR, editors. Handbook of attachment: Theory, research, and clinical applications. New York: Guilford Press; 1999. pp. 355–377. [Google Scholar]
- Frey MA, Denyes MJ. Health and illness self-care in adolescents with IDDM: A test of Orem's theory. Advances in Nursing Science. 1989;12:67–75. doi: 10.1097/00012272-198910000-00009. [DOI] [PubMed] [Google Scholar]
- Gavazzi SM, Anderson SA, Sabatelli RM. Family differentiation, peer differentiation, and adolescent adjustment in clinical sample. Journal of Adolescent Research. 1993;8:205–225. [Google Scholar]
- George C, Solomon J. Attachment and caregiving: The caregiving behavioral system. In: Cassidy J, Shaver PR, editors. Handbook of attachment: Theory, research, and clinical applications. New York: Guilford Press; 1999. pp. 649–670. [Google Scholar]
- Gonder-Frederick LA, Fisher CD, Ritterband LM, Cox DJ, Hou L, DasGupta AA, Clark WL. Predictors of fear of hypoglycemia in adolescents with type 2 diabetes and their parents. Pediatric Diabetes. 2006;7:215–222. doi: 10.1111/j.1399-5448.2006.00182.x. [DOI] [PubMed] [Google Scholar]
- Grace NC, Kelley ML, McCain AP. Attribution processes in mother-adolescent conflict. Journal of Abnormal Child Psychology. 1993;21:199–211. doi: 10.1007/BF00911316. [DOI] [PubMed] [Google Scholar]
- Greenberger E. Defining psychosocial maturity in adolescence. In: Karoly P, Stefen J, editors. Adolescent behavior disorders: Foundations and contemporary concerns. Lexingon, MA: Heath; 1984. pp. 54–81. [Google Scholar]
- Greenberger E, Bond L. User's manual for the psychosocial maturity inventory. E Greenberger, Program in Social Ecology; University of California, Irvine: 1984. [Google Scholar]
- Greenberger E, Jossselson R, Knerr C, Knerr B. The measurement and structure of psychosocial maturity. Journal of Youth and Adolescence. 1975;4:127–143. doi: 10.1007/BF01537437. [DOI] [PubMed] [Google Scholar]
- Greenberger E, Sorenson A. Toward a concept of psychosocial maturity. Journal of Youth and Adolescence. 1974;3:329–358. doi: 10.1007/BF02214746. [DOI] [PubMed] [Google Scholar]
- Grey M, Boland EA, Yu C, Sullivan-Bolyai S, Tamborlane WV. Personal and family factors associated with quality of life in adolescents with diabetes. Diabetes Care. 1998;21:909–914. doi: 10.2337/diacare.21.6.909. [DOI] [PubMed] [Google Scholar]
- Hanson CL, De Guire MJ, Schinkel AM, Henggeler SW. Comparing social learning and family systems correlates of adaptation in youths with IDDM. Journal of Pediatric Psychology. 1992;17:555–572. doi: 10.1093/jpepsy/17.5.555. [DOI] [PubMed] [Google Scholar]
- Hanson CL, De Guire MJ, Schinkel AM, Kolterman OG, Goodman JP, Buckingham BA. Self-care behaviors in insulin-dependent diabetes: Evaluative tools and their association with glycemic control. Journal of Pediatric Psychology. 1996;21:467–482. doi: 10.1093/jpepsy/21.4.467. [DOI] [PubMed] [Google Scholar]
- Hanson CL, Henggeler SW, Harris MA, Burghen GA, Moore M. Family system variables and the health status of adolescents with insulin-dependent diabetes mellitus. Heath Psychology. 1989;8:239–253. doi: 10.1037//0278-6133.8.2.239. [DOI] [PubMed] [Google Scholar]
- Hauser ST, Jacobson AM, Lavori P, Wolfsdorf JI, Herskowitz RD, Wertlieb D, Stein J. Adherence among children and adolescents with insulin-dependent diabetes mellitus over a four-year longitudinal follow-up: II. Immediate and long-term linkages with the family milieu. Journal of Pediatric Psychology. 1990;15:527–542. doi: 10.1093/jpepsy/15.4.527. [DOI] [PubMed] [Google Scholar]
- Hock E, Eberly M, Bartle-Haring S, Ellwanger P, Widaman KF. Separation anxiety in parents of adolescents: Theoretical significance and scale development. Child Development. 2001;72:284–298. doi: 10.1111/1467-8624.00279. [DOI] [PubMed] [Google Scholar]
- Jöreskog KG, Sörbom D. LISREL 8: the SIMPLIS command language. Chicago, IL: SPSS; 1993. [Google Scholar]
- Kenny ME. The extent and function of parental attachments among first-year college students. Journal of Youth and Adolescents. 1987;16:17–29. doi: 10.1007/BF02141544. [DOI] [PubMed] [Google Scholar]
- Kyngas H, Barlow J. Diabetes: An adolescent's perspective. Journal of Advanced Nursing. 1995;22:941–947. doi: 10.1111/j.1365-2648.1995.tb02646.x. [DOI] [PubMed] [Google Scholar]
- Laursen B, Coy KC, Collins WA. Reconsidering changes in parent-child conflict across adolescence: A meta-analysis. Child Development. 1998;69:817–832. [PMC free article] [PubMed] [Google Scholar]
- Leonard BJ, Skay CL, Rheinberger JD. Self-management development in children and adolescents with diabetes: The role of maternal self-efficacy and conflict. Journal of Pediatric Nursing. 1998;13:224–233. doi: 10.1016/S0882-5963(98)80049-3. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. John Wiley & Sons; New York: 1987. [Google Scholar]
- McCaleb A, Edgil A. Self-concept and self-care practices of healthy adolescents. Journal of Pediatric Nursing. 1994;9:233–238. [PubMed] [Google Scholar]
- McElhaney KB, Allen JP. Autonomy and adolescent social functioning: the moderating effect of risk. Child Development. 2001;72:220–235. doi: 10.1111/1467-8624.00275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller VA, Drotar D. Decision making competence and adherence to treatment in adolescents with diabetes. Journal of Pediatric Psychology. 2007;32:178–188. doi: 10.1093/jpepsy/jsj122. [DOI] [PubMed] [Google Scholar]
- Miller-Johnson S, Emery RE, Marvin RS, Clarke W, Lovinger R, Martin M. Parent-child relationships and the management of insulin-dependent diabetes mellitus. Journal of Consulting and Clinical Psychology. 1994;62:603–610. doi: 10.1037//0022-006x.62.3.603. [DOI] [PubMed] [Google Scholar]
- Mullins LL, Wolfe-Christensen C, Hoff Pai AL, Carpentier MY, Gillaspy S, Cheek J, Page M. The relationship of parental overprotection, perceived child vulnerability, and parenting stress to uncertainty in youth with chronic illness. Journal of Pediatric Psychology. 2007;32:973–982. doi: 10.1093/jpepsy/jsm044. [DOI] [PubMed] [Google Scholar]
- National Institute of Diabetes and Digestive Diseases. National Diabetes Statistics fact sheet: general information and national estimates on diabetes in the United States, 2005. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health; 2005. [Google Scholar]
- Palmer DL, Berg CA, Wiebe DJ, Beveridge RM, Korbel CD, Upchurch R, Swinyard MT, Lindsay R, Donaldson DL. The role of autonomy and pubertal status in understanding age differences in maternal involvement in diabetes responsibility across adolescence. Journal of Pediatric Psychology. 2004;29:35–46. doi: 10.1093/jpepsy/jsh005. [DOI] [PubMed] [Google Scholar]
- Pasquier-Fediaevsky LD, Chwalow AJ the PEDIAB Collaborative Group, & Tubiana-Rufi, N. Is the relationship between adherence behaviors and glycaemic control bi-directional at adolescence? A longitudinal cohort study. Diabetic Medicine. 2005;22:427–433. doi: 10.1111/j.1464-5491.2005.01429.x. [DOI] [PubMed] [Google Scholar]
- Prinz RJ, Foster S, Kent RN, O'Leary D. Multivariate assessment of conflict in distressed and nondistressed mother-adolescent dyads. Journal of Applied Behavior Analysis. 1979;2:691–700. doi: 10.1901/jaba.1979.12-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robin AL, Foster SL. Negotiating parent-adolescent conflict: A behavioral approach. New York: Guilford Press; 1989. [Google Scholar]
- Robin AL, Weiss JG. Criterion related validity of behavioral and self-report measures of problem solving communication skills in distressed and non-distressed parent adolescent dyads. Behavioral Assessment. 1980;2:339–352. [Google Scholar]
- Rubin RR, Young-Hyman D, Peyrot M. Parent-child responsibility and conflict in diabetes care. Diabetes. 1989;38(suppl. 2):28A. (abtract) [Google Scholar]
- Ryan RM, Lynch JH. Emotional autonomy versus detachment: Revisiting the vicissitudes of adolescence and young adulthood. Child Development. 1989;60:340–356. doi: 10.1111/j.1467-8624.1989.tb02720.x. [DOI] [PubMed] [Google Scholar]
- Silverstein J, Klingensmith G, Copeland K, Plotnick L, et al. Care of children and adolescents with type 1 diabetes: A statement of the American Diabetes Association. Diabetes Care. 2005;28:186–213. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- Skinner TC, Hampson SE, Fife-Schaw C. Personality, personal model beliefs, and self-care in adolescents and young adults with Type 1 diabetes. Health Psychology. 2002;21:61–70. [PubMed] [Google Scholar]
- Soenens B, Elliot AJ, Goosens L, Vansteenkiste M, Luyten P, Duriez B. The intergenerational transmission of perfectionism: Parents' psychological control as an intervening variable. Journal of Family Psychology. 2005;19:358–366. doi: 10.1037/0893-3200.19.3.358. [DOI] [PubMed] [Google Scholar]
- Streisand R, Swift E, Strodtbeck F. Husband-wife interaction over revealed differences. American Sociology Review. 1951;16:463–473. [Google Scholar]
- Ullman JB. Structural equation modeling. In: Tabachnick BG, Fidell LS, editors. Using multivariate statistics. New York: Harper Collins; 1996. pp. 709–811. [Google Scholar]
- Urbach SL, LaFranchi S, Lambert L, Lapidus JA, Daneman D, Becker TM. Predictors of glucose control in children and adolescents with type 1 diabetes mellitus. Pediatric Diabetes. 2005;6:69–74. doi: 10.1111/j.1399-543X.2005.00104.x. [DOI] [PubMed] [Google Scholar]
- Viikinsalo MK, Crawford DM, Kimbrel H, Long AE, Dashiff C. Conflicts between young adolescents with Type 1 Diabetes and their parents. Journal of the Society of Pediatric Nurses. 2005;10:69–80. doi: 10.1111/j.1744-6155.2005.0015a.x. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Harris MA, Buckloh LM, Mertlich D, Lochrie AS, Taylor A, et al. Effects of behavioral family systems therapy for diabetes on adolescents' family relationships, treatment adherence, and metabolic control. Journal of Pediatric Psychology. 2006a;31:928–938. doi: 10.1093/jpepsy/jsj098. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Harris MA, Buckloh LM, Wilkinson K, Sadler M, Mauras N, White N. Self-care autonomy and outcomes of intensive therapy or usual care in youth with Type 1 diabetes. Journal of Pediatric Psychology. 2006b;31:1036–1035. doi: 10.1093/jpepsy/jsj017. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Taylor A, Hough BS, Linscheid TR, Yates KO, Naglieri JA. Deviation from developmentally appropriate self-care autonomy: Association with diabetes outcomes. Diabetes Care. 1996;19:119–125. doi: 10.2337/diacare.19.2.119. [DOI] [PubMed] [Google Scholar]