Abstract
Background
For surgical treatment of thumb carpometacarpal (CMC) arthritis, current evidence suggests that simple trapeziectomy is as effective and may be safer than trapeziectomy and ligament reconstruction (LR) with or without tendon interposition (TI). We examined whether current practice patterns in the surgical treatment of thumb CMC arthritis reflect adoption of simple trapeziectomy as best practice. Furthermore, we investigated whether surgeon preferences and third-party payer patterns are associated with use of simple trapeziectomy.
Methods
We performed a retrospective cross-sectional study of 6776 surgical treatments for thumb CMC arthritis using the all-payer State Ambulatory Surgery Database (SASD) for Florida, during 2006–2009. We applied multinomial regression analysis to examine associations between covariates, describing surgeon and third-party payer factors and the type of procedure performed. We calculated an intra-class correlation coefficient (ICC) to determine how much of the difference in patient outcome (procedure type) is due to differences among surgeons.
Results
Across surgeon characteristics included in the analysis, patients’ outcome probabilities were over 90% in favor of treatment with trapeziectomy and LR with or without TI. Additionally, the level of intra-class correlation amongst patients clustered within a surgeon showed that individual surgeons contribute substantially to determining what procedure type a patient undergoes.
Conclusion
In this multi-year one state study, it appears that current evidence demonstrating the equivalent effectiveness of simple trapeziectomy compared to more involved alternatives did not result in wide adoption of the technique. This finding is consistent with studies in many clinical disciplines that highlight the difficulty of influencing clinical practice with available evidence.
Level of Evidence
III therapeutic
Keywords: CMC, arthritis, CMC, arthrodesis, CMC, synovectomy evidence, partial/complete trapeziectomy with, LR/LRTI, prosthetic arthroplasty, simple complete trapeziectomy, soft-tissue arthroplasty
INTRODUCTION
The thumb carpometacarpal (CMC) joint is the second most affected by osteoarthritis in the hand, and surgical treatments for thumb CMC arthritis are indicated for Eaton-Glickel stage II to IV disease refractory to pharmaceutical and other non-surgical treatments.1–4 However, there are up to 8 different procedures described to treat thumb CMC disease with outcomes that are comparable in terms of symptom relief, preservation of function and patient satisfaction.5–7 Much of current debate in the literature centers on the benefit of soft tissue arthroplasty techniques, including ligament reconstruction and tendon interposition in addition to excision of the trapezium.5–8
Gervis introduced simple complete trapeziectomy in 1949.9 However, surgeons reported debilitating weakness of the thumb following this procedure and theorized that this resulted from instability at the metacarpal base in the absence of the excised trapezium.10,11 Furthermore, they were concerned that unchecked subsidence of the metacarpal in the trapezial space put patients at risk for scapho-metacarpal arthritis.12
Subsequently, soft tissue arthroplasty techniques were devised to address concerns with simple complete trapeziectomy. These techniques include: flexor carpi radialis (FCR) tendon interposition in the trapezial space introduced by Froimson13; Burton and Pelligrini’s combined ligament reconstruction (LR) and tendon interposition (TI) also using half of the FCR tendon14; and Weilby’s suspensionplasty and tendon interposition using the abductor pollicis longus (APL) tendon.15,16 Many believed that these procedures addressed concerns about loss of thumb height and stability of the thumb metacarpal.14,17–20
However, accumulating evidence indicates that simple complete trapeziectomy, with or without technical modifications such as hematoma distraction arthroplasty, has similar outcomes compared to trapeziectomy with soft-tissue arthroplasty techniques.6,7, 21–25 Wajon et al’s 2 comprehensive Cochrane systematic reviews of 9 studies recommend simple complete trapeziectomy as an equivalently effective procedure with significantly fewer complications.6,7 Additionally, Li et al’s more recent 6 study systematic review also reported similar outcomes between simple trapeziectomy and trapeziectomy with soft-tissue arthroplasty techniques although unlike Wajon et al’s review, they did not find significantly less adverse events with simple trapeziectomy.26 Lastly, Gangopadhyay et al’s recent report on long-term follow-up of patients randomized to treatments including simple complete trapeziectomy and partial/complete trapeziectomy with LR/LRTI appear to support Wajon et al’s recommendations.27
In many clinical disciplines, it has been observed that best available evidence may not influence clinical practice.28–31 Evidence-based medicine experts estimate that the probability that any clinician responds to guidelines derived from available evidence is approximately 50 percent.32 As a result, investigators in several clinical disciplines have attempted to study reasons for the difficulty in adoption of available evidence into clinical practice.33–35 In the case of surgeons, some of the common explanations include continued adherence to techniques learned during training, the inertia of current practice and substantial reliance on anecdotal experience.33,36
In this study, we set out to examine the extent to which current evidence about the equivalent effectiveness of simple trapeziectomy, compared to trapeziectomy with soft-tissue arthroplasty techniques, is associated with practice patterns in surgical treatment of thumb CMC arthritis. Based on the established difficulty of influencing clinical practice with available evidence, we hypothesize that simple complete trapeziectomy is not a commonly used procedure for treating thumb CMC arthritis. Furthermore, we hypothesize that non-disease-related factors such as third-party payer status and surgeon preferences will be significantly associated with the lack of use of simple complete trapeziectomy.
MATERIALS AND METHODS
Data Source
We performed a cross-sectional analysis of the Healthcare Cost and Utilization (HCUP) Florida State Ambulatory Surgery Database (SASD) for the years 2006–2009. The database contains all-payer discharge-level records for all ambulatory procedures occurring in emergency departments, hospital-based surgical units and free standing ambulatory surgery centers statewide. We chose to examine data from Florida because the state has a high proportion of elderly patients, the demographic group most affected by thumb CMC arthritis. We examined data from 2006 and 2009 because they were the most recent data available that permitted consistently accurate assignation of patients to surgeons that treated them. The database is publicly available and de-identified; hence, our study was exempt from human subjects regulation by the University of Michigan Institutional Review Board.
Cohort Selection
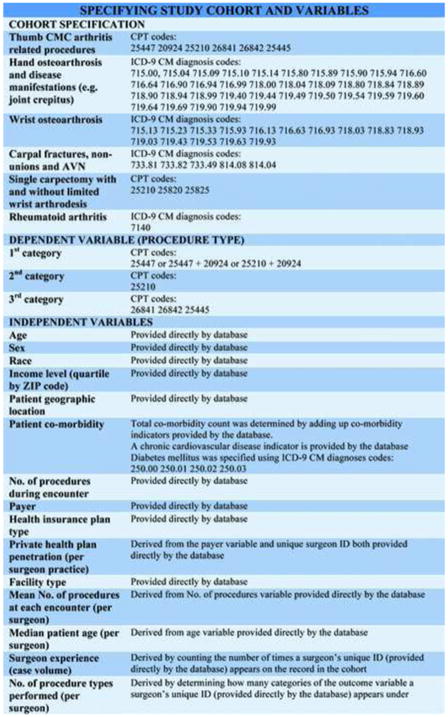
We defined our cohort using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9 CM) diagnostic codes and Current Procedural Terminology® (CPT) codes (Figure 1). Current Procedural Terminology® (CPT) procedure codes are more specific to the thumb CMC joint than ICD-9 CM diagnosis codes for most of the surgical treatments for thumb CMC arthritis included in this study.37 Hence, we used CPT procedure codes in the first step of specifying our study population.
Figure 1.
Specification of the study cohort and covariates using CPT (Current Procedure Terminology) codes, ICD-9 CM (International Classification of Diseases, 9th Revision, Clinical Modification) codes and variables provided by the database. CMC; carpometacarpal, AVN; avascular necrosis.
We included patients 40 years and older with documentation, by CPT code, of any one of 4 surgical treatments included in the study (Figure 1).37 To further specify our study population, we excluded patients without ICD-9 CM diagnoses codes for primary hand osteoarthrosis or manifestations of the disease such as arthralgia, degenerative disease of the articular cartilage, joint crepitus and joint instability (Figure 2). This exclusion ensured that only patients having documented diagnosis with ICD-9 CM codes and documented treatment with CPT codes were included in the study population. One of the CPT codes described procedures on the CMC joint and carpal bones but was not completely specific to the thumb. This CPT code is: 25210 (carpectomy, one bone, used for simple complete trapeziectomy).37 Hence, our next step was to address the incomplete specificity of the single carpectomy CPT code. We excluded patients with ICD-9 CM diagnosis codes for wrist and carpal conditions treated with procedures that involved excision of any single carpal bone. This exclusion eliminated patients who had any carpectomy other than trapeziectomy for hand osteoarthrosis. In order to accomplish this particular exclusion, we removed patients with ICD-9 CM diagnosis codes for wrist arthrosis along with CPT codes for excision of one carpal bone with or without limited wrist arthrodesis (Figure 2).38 We also excluded records with ICD-9 CM diagnosis codes for hamate and pisiform fractures along with CPT codes for excision of one carpal bone (Figure 2).39 Lastly, we excluded patients with ICD-9 CM diagnosis code for rheumatoid arthritis (Figure 2).
Figure 2.
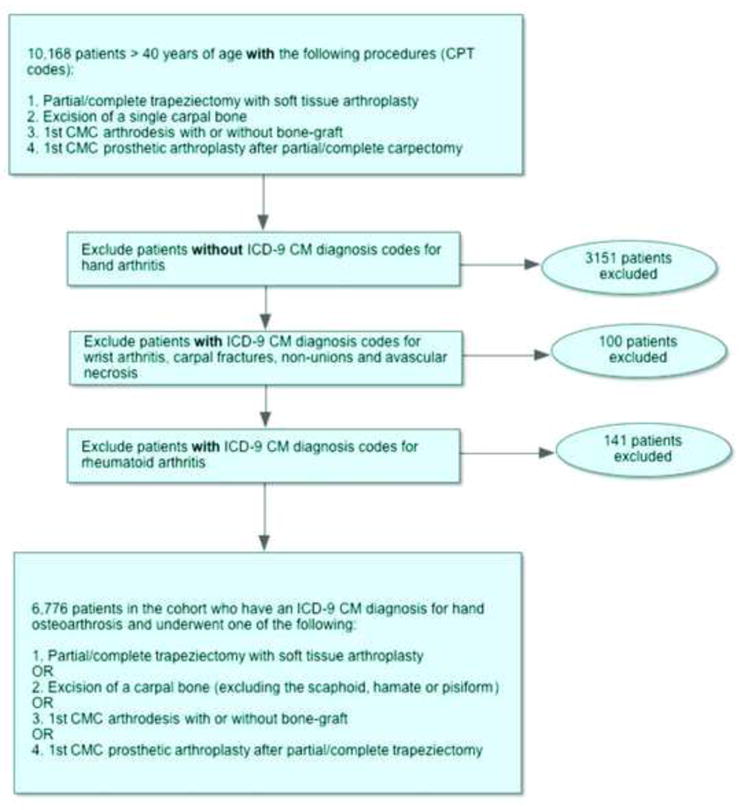
Algorithm for defining study cohort using the Florida State Ambulatory Surgery Database (SASD). CPT; current procedure terminology, CMC; carpometacarpal, ICD-9 CM; international classification of disease, 9th revision, clinical modification.
Our final study cohort included 6776 patients 40 years of age and older with both a diagnosis of hand osteoarthrosis and treatment with one of the following procedures: partial/complete trapeziectomy with tendon interposition with or without ligament reconstruction or with suspensionplasty; simple complete trapeziectomy; thumb CMC arthrodesis with or without bone graft; and thumb CMC prosthetic arthroplasty--interposition or total joint replacement (Figure 2). We chose these techniques because they have been relatively well reported on in the literature.5–8,18–27
Dependent, Control and Independent Variables
Our outcome variable was the method of surgical treatment for thumb CMC arthritis as specified by CPT codes. We defined the outcome variable in 3 categories. The first category was partial/complete trapeziectomy with any soft tissue arthroplasty. The second category was simple complete trapeziectomy. The third category was a combination of CMC arthrodesis and CMC prosthetic arthroplasty. We found it necessary to combine the last 2 procedures in order to have sufficient outcomes in that category for statistical analyses with reliable estimates.
For adjusted analyses, we included variables representing patient demographic and clinical characteristics. Patient demographic variables included age, gender, race/ethnicity, income level, and patient geographic location. Clinical characteristic variables included patient’s total co-morbidity count, diagnosis of chronic cardiovascular disease and diabetes mellitus, and the total number procedures performed at the time of treatment (e.g., carpal tunnel release and 1st dorsal compartment release, etc.). Our variables of interest included health system-related factors such as third-party payer (Medicare, private plans and other including Medicaid and self-pay) and the type of health plan (managed care vs. non-managed care plans). We also included surgeon-related variables such as the individual experience of surgeons in the dataset (case volume over the 4 years of the study), the number of different procedure types performed by each individual surgeon and the private health plan penetration (private plan payer as a proportion of all thumb CMC cases during the study period) in each individual surgeon’s practice. Other surgeon-related variables in the model including the median age of each surgeon’s panel of patients treated for thumb CMC arthritis, the mean number of procedures performed at the time of each patient encounter, and the type of facility in which they operated. We used variables provided directly by the database to derive some of these covariates (Figure 1).
Missing Data
In order to include observations that had missing data for control variables in the final analysis, we created “missing” categories within variables that had more than 1% of the data missing: for race/ethnicity (1.4% missing) and patient income level (2.2% missing).
Statistical Analyses
We used descriptive statistics to summarize current trends in surgical treatment of thumb CMC arthritis in the state of Florida over 4 most recent years of publicly available data (2006–2009). Then we applied multinomial regression analysis to examine the associations between independent variables and the choice of procedure for surgical treatment of CMC arthritis.
We performed the regression analysis with adjustment for the clustered nature of our data (i.e., patients cluster within surgeons, and therefore the observations are not independent of each other at the surgeon level). We then calculated the intra-class correlation coefficient (ICC) to ascertain how much of the explanation of a patient’s outcome may be ascribed to clustering under a particular surgeon’s care. Lastly, we used regression estimates to generate marginal adjusted probabilities of undergoing one procedure versus alternatives, which are all reported with 95% confidence intervals.
RESULTS
Characteristics of Patients and Encounters in the Study Sample
Of the 6776 encounters in the sample, 6,240 patients (92.1%) underwent partial/complete trapeziectomy with soft tissue arthroplasty, 291 (4.3%) underwent simple complete trapeziectomy and 245 (3.6%) underwent CMC arthrodesis, or prosthetic arthroplasty (Table 1). Socio-demographic and clinical characteristics of patient encounters in the sample are presented in Table 1.
Table 1.
| Trapeziectomy with soft tissue arthroplasty | Simple complete trapeziectomy | CMC arthrodesis and Prosthetic CMC arthroplasty | |
|---|---|---|---|
| No. of patients (%) | 6240 (92.1) | 291 (4.3) | 245 (3.6) |
| Demographics | |||
| Mean age (SD) | 63 (9.3) | 61 (9.9) | 61 (10.1) |
| Sex††, % | |||
| Male | 20.7 | 25.4 | 27.3 |
| Female | 79.3 | 74.6 | 72.6 |
| Race††, n (%) | |||
| White | 5758 (92.3) | (92.0) | (88.2) |
| Non-white | 388 (6.2) | (8.0) | (11.8) |
| Missing | 94 (1.5) | - | - |
| Income quartile†† (per ZIP), n (%) | |||
| 1st quartile | 1148 (18.4) | (14.2) | (23.2) |
| 2nd quartile | 1598 (25.6) | (19.8) | (27.8) |
| 3rd quartile | 1655 (26.5) | (35.3) | (21.9) |
| 4th quartile | 1703 (27.3) | (30.7) | (27.1) |
| Missing | 136 (2.2) | - | - |
| Patient location††, % | |||
| Large metro. | 38.6 | 63.8 | 47.8 |
| Small metro. | 50.9 | 26.2 | 41.2 |
| Micropolitan | 6.6 | 7.2 | 7.8 |
| Non Metro | 3.9 | 2.8 | 3.2 |
| Clinical | |||
| Total co-morbidity count | |||
| Mean (SD) | 1.8 (1.3) | 1.3 (0.76) | 2.0 (1.5) |
| Chronic CV disease, n (%) | 1111 (17.8) | 13 (4.5) | 45 (118.4) |
| Diabetes Mellitus, n (%) | 247 (4.0) | - | - |
| No. of procedures during encounter | |||
| Mean (SD) | 3.4 (2.2) | 2.8 (1.6) | 3.1 (2.6) |
| Healthcare system | |||
| Payer, n (%) | |||
| Medicare | 2655 (42.6) | 104 (35.7) | 88 (35.9) |
| Private | 3113 (49.9) | 157 (54.0) | 132 (53.9) |
| Other | 469 (7.5) | 30 (10.3) | 25 (10.2) |
| Health insurance plan type, n (%) | |||
| Managed | 2296 (36.8) | 74 (25.4) | 110 (44.9) |
| Non-managed | 3504 (56.2) | 188 (64.6) | 112 (45.7) |
| Other | 437 (7.0) | 29 (10.0) | 23 (9.4) |
CMC arthrodesis, and prosthetic arthroplasty (right column) were combined into one outcome category in order to have sufficient outcomes for reliable estimates from statistical analysis.
In order to protect identity of patients who contribute personal health information to its databases, the Agency for Healthcare Research and Quality (AHRQ prohibits reporting summary statistics on patient characteristics in variable categories containing ≤10 observations. We have taken the following steps to comply with AHRQ rules:
Sex: one of the outcome categories contains 2 observations with missing data for this variable; hence we described this patient characteristic as percentages of non-missing data.
Race: two of the outcome categories contained 4 observations with missing data for this variable; hence we described this patient characteristic for those two outcome categories as percentages of non-missing data.
Income quartile (per ZIP): two of the outcome categories contained 16 observations (≤10 observations each) with missing data for this variable; hence we described this patient characteristic for those two outcome categories as percentages of non-missing data.
Patient location: two of the outcome categories contained 6 observations with missing data for this variable; hence we described this patient characteristic as percentages of non-missing data.
Diabetes Mellitus: two of the outcome categories contained ≤10 observations and no missing data; hence we are prohibited by AHRQ rules from reporting summary statistics for those 2 outcome categories.
CMC; carpometacarpal, SD; standard deviation, CV; cardiovascular.
Of 328 surgeons who performed thumb CMC procedures for patients in the study sample, 64% performed only 1 procedure type. Most of the surgeons (89%) performed 1 or 2 procedure types, and these surgeons performed the majority (71%) of cases in the sample. Table 2 displays characteristics of surgeons in the study.
Table 2.
Characteristics of Surgeons† in the Study
| No. of procedure types performed by surgeon: | No. of surgeons n (%): |
| 1 procedure | 210 (64.0) |
| 2 procedures | 83 (25.3) |
| 3 procedures | 32 (9.8) |
| 4 procedures | 3 (0.9) |
|
| |
| No. of procedure types performed by surgeon: | No. of encounters, n (%): |
| 1 procedure | 2521 (37.2) |
| 2 procedures | 2272 (33.5) |
| 3 procedures | 1862 (27.5) |
| 4 procedures | 121 (1.9) |
|
| |
| Surgeon case volume summary statistics during 4-year study period: | |
| Mean (SD) | 84.0 (66.8) |
| 1st quartile | < 31 cases |
| 2nd quartile | 31–67 cases |
| 3rd quartile | 67–120 cases |
| 4th quartile | > 120 cases |
|
| |
| Surgeon case volume during 4-year study period: | No. of surgeons, n (%): |
| 1st quartile (< 28 cases) | 100 (30.5) |
| 2nd quartile (28–67 cases) | 68 (20.7) |
| 3rd quartile (67–120 cases) | 79 (24.1) |
| 4th quartile (> 120 cases) | 81 (24.7) |
|
| |
| Private health plan penetration (per surgeon practice) | |
| Mean (SD) | |
| 1st quartile | 0.50 (0.17) |
| 2nd quartile | < 0.39 |
| 3rd quartile | 0.39–0.50 |
| 4th quartile | 0.50–0.62 |
| > 0.62 | |
|
| |
| Medicare penetration (per surgeon practice) | |
| Mean (SD) | |
| 1st quartile | 0.42 (0.17) |
| 2nd quartile | < 0.31 |
| 3rd quartile | 031–0.39 |
| 4th quartile | 0.39–0.52 |
| > 0.52 | |
|
| |
| Proportion of cases in freestanding ASC (per surgeon practice) | |
| Mean (SD) | 0.66 (0.39) |
| 1st quartile | < 0.35 |
| 2nd quartile | 0.35–0.87 |
| 3rd quartile | 0.87–0.99 |
| 4th quartile | > 0.99 |
328 surgeons in the study
SD; standard deviation, ASC; ambulatory surgery center
Effect of Predictors of Interest
Tables 3a and 3b show the results of the cluster-adjusted multinomial regression analysis with partial/complete trapeziectomy with soft-tissue arthroplasty (1st outcome variable category) as the reference group. In the comparisons of the 2nd (Table 3a) and 3rd outcome variable categories (Table 3b) to the reference group, the number of distinct procedure types performed by a given surgeon was significantly associated with a patient undergoing a procedure other than partial/complete trapeziectomy with soft-tissue arthroplasty. In addition, surgeon overall case volume was significantly associated with a patient’s outcome in the comparison of the 3rd outcome category to the reference group (Table 3b). The intra-class correlation among surgeons in the sample was 0.67.
Table 3.
| Tables 3a. Adjusted Relative Risk of Performing Simple Complete Trapeziectomy Versus Trapeziectomy with Soft-Tissue Arthroplasty.
| ||||
|---|---|---|---|---|
| RRR‡ | 95% CI | p | ||
|
| ||||
| Trapeziectomy w/ soft-tissue arthroplasty (reference group) | ||||
|
| ||||
| Simple complete trapeziectomy | ||||
|
| ||||
| Patient demographics | ||||
|
| ||||
| Age | 0.85† | 0.73–0.99 | 0.03 | |
|
| ||||
| Sex | ||||
| Male | Reference group | |||
| Female | 0.76 | 0.53–1.10 | 0.15 | |
|
| ||||
| Race | ||||
| Non-white | Reference group | |||
| White | 1.15 | 0.67–1.99 | 0.62 | |
| Unspecified | 0.31 | 0.05–1.89 | 0.20 | |
|
| ||||
| Income level (ZIP code) | ||||
| 1st quartile | Reference group | |||
| 2nd quartile | 0.94 | 0.63–1.42 | 0.80 | |
| 3rd quartile | 1.96† | 1.28–3.01 | 0.02 | |
| 4th quartile | 1.28 | 0.77–2.14 | 0.35 | |
| Unspecified | 1.35 | 0.53–3.39 | 0.53 | |
|
| ||||
| Patient location | ||||
| Large metropolitan | Reference group | |||
| Small metropolitan | 0.19† | 0.10–0.35 | < 0.01 | |
| Micropolitan | 0.43 | 0.14–1.33 | 0.14 | |
| Non-metropolitan | 0.19† | 0.04–0.79 | 0.02 | |
|
| ||||
| Surgeon | ||||
|
| ||||
| Proportion of patients with private insurance | 0.27 | 0.01–7.82 | 0.49 | |
|
| ||||
| Proportion of cases in freestanding ambulatory surgery center | 2.58 | 0.57–11.76 | 0.22 | |
|
| ||||
| Mean No. of procedures at each encounter | 1.12 | 0.76–1.65 | 0.56 | |
|
| ||||
| Median age of patients in surgeon’s practice treated for thumb CMC arthritis | 0.98 | 0.85–1.13 | 0.77 | |
|
| ||||
| Total volume of cases | 1.00 | 1.00–1.01 | 0.33 | |
|
| ||||
| No. of procedure types performed | 2.85† | 1.87–4.37 | < 0.01 | |
|
| ||||
| Clinical | ||||
|
| ||||
| Total co-morbidity count | 0.48† | 0.30–0.76 | 0.02 | |
|
| ||||
| Chronic cardiovascular disease | ||||
| No | Reference group | |||
| Yes | 0.81 | 0.31–2.11 | 0.66 | |
|
| ||||
| Diabetes Mellitus | ||||
| No | Reference group | |||
| Yes | 2.39 | 0.73–7.86 | 0.15 | |
|
| ||||
| Total No. of procedures during encounter | 0.93 | 0.80–1.08 | 0.33 | |
|
| ||||
| Healthcare system | ||||
|
| ||||
| Payer | ||||
| Medicare | Reference group | |||
| Private | 1.03 | 0.69–1.54 | 0.89 | |
| Other (Medicaid, self-pay etc.) | 0.97 | 0.23–4.04 | 0.97 | |
|
| ||||
| Health insurance plan type | ||||
| Managed | Reference group | |||
| Non-managed | 1.29 | 0.81–2.06 | 0.29 | |
| Other (self-pay, worker’s comp. etc.) | 1.28 | 0.28–5.90 | 0.75 | |
| Tables 3b. Adjusted Relative Risk of Performing Arthrodesis or Prosthetic Arthroplasty Versus Trapeziectomy with Soft-Tissue Arthroplasty.
| ||||
|---|---|---|---|---|
| RRR‡ | 95% CI | p | ||
|
| ||||
| Trapeziectomy w/ soft-tissue arthroplasty (reference group) | ||||
|
| ||||
| Arthrodesis and prosthetic arthroplasty | ||||
|
| ||||
| Demographics | ||||
|
| ||||
| Age | 0.81† | 0.72–0.92 | < 0.01 | |
|
| ||||
| Sex | ||||
| Male | Reference group | |||
| Female | 0.68† | 0.51–0.91 | 0.01 | |
|
| ||||
| Race | ||||
| Non-white | Reference group | |||
| White | 0.76 | 0.48–1.22 | 0.26 | |
| Unspecified | 0.37 | 0.08–1.81 | 0.22 | |
|
| ||||
| Income level (ZIP code) | ||||
| 1st quartile | Reference group | |||
| 2nd quartile | 0.92 | 0.58–1.46 | 0.72 | |
| 3rd quartile | 0.65 | 0.37–1.14 | 0.13 | |
| 4th quartile | 0.76 | 0.43–1.34 | 0.34 | |
| Unspecified | 1.17 | 0.51–2.68 | 0.71 | |
|
| ||||
| Patient location | ||||
| Large metropolitan | Reference group | |||
| Small metropolitan | 0.77 | 0.44–1.34 | 0.36 | |
| Micropolitan | 0.91 | 0.48–1.74 | 0.78 | |
| Non-metropolitan | 0.59 | 0.26–1.35 | 0.21 | |
|
| ||||
| Surgeon | ||||
|
| ||||
| Proportion of patients with private insurance | 0.72 | 0.12–4.22 | 0.71 | |
|
| ||||
| Proportion of cases in freestanding ambulatory surgery center | 0.74 | 0.37–1.47 | 0.34 | |
|
| ||||
| Mean No. of procedures at each encounter | 0.98 | 0.74–1.30 | 0.89 | |
|
| ||||
| Median age of patients in surgeon’s practice treated for thumb CMC arthritis | 1.04 | 0.95–1.13 | 0.44 | |
|
| ||||
| Total volume of cases | 0.98† | 0.97–0.99 | < 0.01 | |
|
| ||||
| No. of procedure types performed | 2.58† | 1.99–3.35 | < 0.01 | |
|
| ||||
| Clinical | ||||
|
| ||||
| Total co-morbidity count | 1.02 | 0.75–1.41 | 0.86 | |
|
| ||||
| Chronic cardiovascular disease | ||||
| No | Reference group | |||
| Yes | 0.81 | 0.45–1.45 | 0.47 | |
|
| ||||
| Diabetes Mellitus | ||||
| No | Reference group | |||
| Yes | 0.50 | 0.21–1.18 | 0.11 | |
|
| ||||
| Total No. of procedures during each encounter | 0.89 | 0.74–1.07 | 0.21 | |
|
| ||||
| Healthcare system | ||||
|
| ||||
| Payer | ||||
| Medicare | Reference group | |||
| Private | 0.91 | 0.57–1.46 | 0.70 | |
| Other (Medicaid, self-pay etc.) | 1.06 | 0.22–5.00 | 0.94 | |
|
| ||||
| Health insurance plan type | ||||
| Managed | Reference group | |||
| Non-managed | 0.62 | 0.38–1.00 | 0.05 | |
| Other (self-pay, worker’s comp. etc.) | 0.78 | 0.16–3.70 | 0.75 | |
Relative risk ratio, which is the measure of effect size in multinomial regression analysis. It is similar to odds ratio in logistic regression
Significant relative risk ratios
Adjusted Predictive Probabilities from the Cluster Adjusted Regression Analysis
In analyses adjusted for patient, surgeon, and practice covariates, the marginal probability that any patient in our study was treated with partial/complete trapeziectomy with soft tissue arthroplasty was 96.6% (95.6%–97.6%), compared with 1.9% (1.1%–2.6%) for simple complete trapeziectomy and 1.5% (0.7%–2.3%) combined for arthrodesis, and prosthetic arthroplasty.
Furthermore, the probability for any patient in the study to undergo partial/complete trapeziectomy with soft tissue arthroplasty if treated by a surgeon who performs only one of the four procedures is 97.3% (96.2%–98.3%) (Figure 3a). With surgeons who perform two or more of the procedures for thumb CMC arthritis, the patient’s probability of treatment with partial/complete trapezietomy with soft tissue arthroplasty progressively decreases (Figure 3a).
Figure 3.
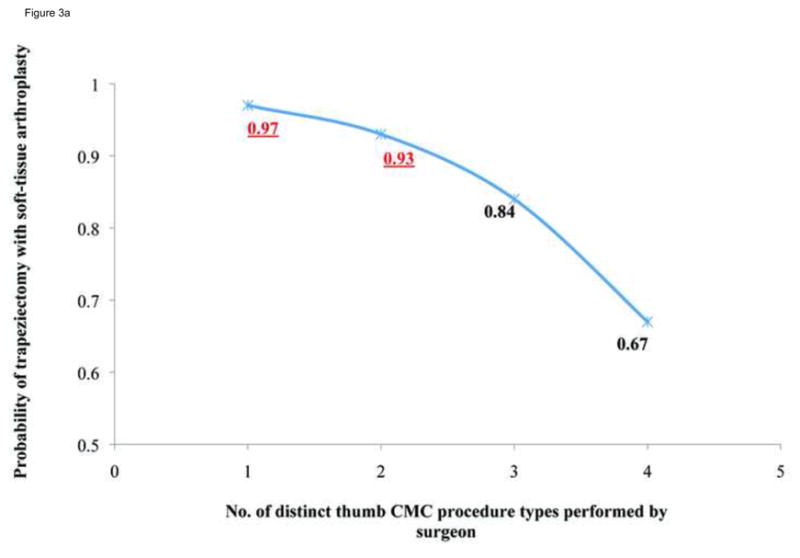
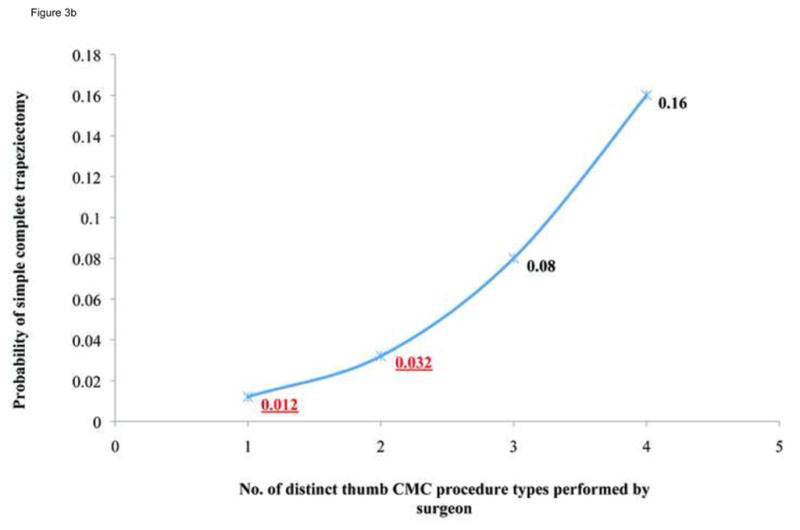
Figure 3a: Association between the number of procedure types a surgeon performs and a patient’s likelihood of undergoing partial/complete trapeziectomy with soft-tissue arthroplasty for thumb CMC arthritis. The numbers highlighted in red (top left) represent the most common probabilities of treatment with partial/complete trapeziectomy with soft-tissue arthroplasty given that surgeons that performed 1 or 2 procedures treated > 70% of patients.
Figure 3b: Association between number of procedures types a surgeon performs and a patient’s likelihood of undergoing simple complete trapeziectomy. The numbers highlighted in red (bottom left) represent the most common probabilities of treatment with simple complete trapeziectomy, given that surgeons that performed 1 or 2 procedures treated > 70% of patients.
On the other hand, the probability of undergoing simple complete trapeziectomy if treated by a surgeon who performs only one of the four procedures is 1.2% (0.4%–2.0%) (Figure 3b). With surgeons who perform two or more of the procedures, the probability of treatment with simple complete trapeziectomy progressively increases, although the maximum is 16.2% (5.8%–26.5%) (Figure 3b).
Patients treated by surgeons in the lowest quartile for case volume (8 cases/year) had a 6.6% (5.2%–8.1%) probability of undergoing procedures in the 3rd outcome category (arthrodesis and prosthetic arthroplasty). When treated by surgeons in the highest quartile for case volume (≥30 cases/year), the probability of undergoing procedures in the 3rd outcome category is negligible (< 1%).
DISCUSSION
In this cross-sectional study of recent patterns of surgical treatment for thumb CMC arthritis in the state of Florida, our findings indicate that simple complete trapeziectomy is not a widely performed procedure, despite level 1 evidence to indicate that this is a clinically acceptable procedure that is simpler than alternatives.23,24,27 In fact, the most common surgical treatment in this sample is partial/complete trapeziectomy with soft tissue arthroplasty. These findings should be considered in the context of current evidence that demonstrates the equivalent effectiveness of simple complete trapeziectomy compared to the more involved partial/complete trapeziectomy with soft tissue arthroplasty techniques.6,7,21–27
Much has been written about the difficulty of influencing clinical practice with available evidence, across many clinical disciplines including surgery.28–31,40 Entrenched practice patterns among clinicians based on such factors as anecdotal experience, inertia of current practice, tradition of techniques learned in training programs–and differing views on the relevance of current evidence have been described as contributors to non-adoption of experimental evidence.29,33,36,41. Two findings in this study lend credence to the idea of entrenched practice patterns in the surgical treatment of thumb CMC arthritis. First, the most widely practiced technique is at odds with current evidence. Second, we found that the intra-class correlation among encounters for the same surgeon is quite high, indicating that the procedure a patient gets is highly dependent on which surgeon treats them.
In fact, among variables significantly associated with the risk of having specific thumb CMC procedures, the effect sizes were of greatest magnitude for surgeon-level factors, rather than patient-level factors. This is attributable to the observations that most surgeons in the study (89%) performed 1 or 2 types of thumb CMC procedures, and patients treated by these surgeons had a 97% and 93% probability, respectively, of being treated with partial/complete trapeziectomy with soft tissue arthroplasty. The equivalent probabilities were only 1.2% and 3.2%, respectively, for treatment with simple complete trapeziectomy.
Although our data and study design do not permit us to determine specific reasons for entrenched practice patterns, the literature regarding surgical treatments for thumb CMC arthritis offers some insight. Early concerns raised about simple complete trapeziectomy fueled efforts to improve on this technique. Hence, between 1949 and 1986, many of the different techniques used in current practice were devised (figure 4).13–16,42,43 Of all the alternatives, soft tissue arthroplasty techniques were consistently reported as producing good outcomes with relatively lower complication rates compared to alternatives such as CMC arthrodesis and prosthetic arthroplasty.14,18–20,44,45 Davis et al’s 1997 randomized controlled trial and subsequent studies reintroducing simple complete trapeziectomy as an effective alternative to trapeziectomy with soft-tissue arthroplasty techniques were published after the latter techniques were widely established as the procedures of choice.21–27 Therefore, it seems likely that techniques that hand surgeons learned in training programs combined with inertia of a current practice that produces acceptable results–contribute to the high prevalence of partial/complete trapeziectomy with soft tissue arthroplasty in this study. Additionally, EBM experts point out that clinicians may remain entrenched in their practice patterns because they do not believe that current evidence addresses concerns specific to their patients and practices.33,35 For example, much of the literature demonstrating equivalent outcomes from simple trapeziectomy and soft tissue arthroplasty techniques have short average follow-up durations.27, This relatively short duration of follow-up may not be sufficient to allay concerns about long-term outcome, hence, surgeons might be inclined to carry on with current practice.33,35
Figure 4.
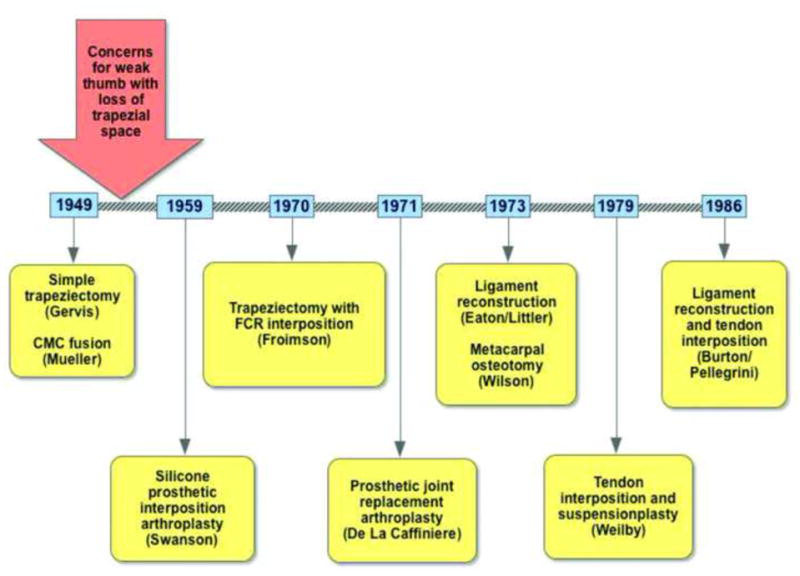
Timeline of procedures devised to treat thumb carpometarcarpal arthritis. CMC; carpometacarpal, FCR; flexor carpi radialis.
Our study has limitations common to administrative data analyses. First, it is a retrospective cross-sectional study that lacks some clinical data that would ideally be included in adjusted analyses, to account for disease stage as defined by the Eaton-Glickel classification.3,4 However, all of the procedures analyzed in this study are indicated for Eaton-Glickel stage II to IV disease.3,4,46 Hence, our finding of over 90% probability of treatment with partial/complete trapeziectomy with soft tissue arthroplasty amongst surgeons who treated most patients is not likely to be due solely to decision-making with the Eaton-Glickel classification. Lastly, our study findings are limited to the state of Florida and must be generalized with caution to practice patterns in other states. However, Florida is a populous state that contains a large proportion of patients in the demographic with the highest risk of thumb CMC arthritis. Thus, it is a suitable location in which to study trends that will inform future studies on utilization of resources and variations in practice for thumb CMC treatment in broader contexts.
In conclusion, today’s rapid advances in healthcare reform require enhanced justification for resource utilization. Hence, hand surgeons must be at the vanguard of implementing best, cost-effective and safe practices based on available evidence. If available evidence is judged inadequate to alter clinical practice, the onus remains on hand surgeons to improve the level of evidence with rigorously performed studies. Institutions of healthcare reform such as the newly formed Patient Centered Outcomes Research Institute, established under the Patient Protection and Affordable Care Act to conduct and recommend findings from comparative effectiveness studies, can be critical partners in the effort to establish best practices based on soundly generated evidence.47
Acknowledgments
Support for this study was provided by the Robert Wood Johnson Foundation Clinical Scholars Program/VA Scholar and with a grant from the National Endowment for Plastic Surgery (to Dr. Oluseyi Aliu). This study is also supported in part by a Midcareer Investigator Award in Patient-Oriented Research (K24AR053120) and 2R01AR047328 - 06 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), and R01AR062066 from NIAMS and the National Institute on Aging (to Dr. Kevin C. Chung).
References
- 1.Haugen IK, Englund M, Aliabadi P, et al. Prevalence, incidence and progression of hand osteoarthritis in the general population: the Framingham Osteoarthritis Study. Ann Rheum Dis. 2011;70:1581–1586. doi: 10.1136/ard.2011.150078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang Y, Niu J, Kelly-Hayes M, et al. Prevalence of symptomatic hand osteoarthritis and its impact on functional status among the elderly: The Framingham Study. Am J Epidemiol. 2002;156:1021–1027. doi: 10.1093/aje/kwf141. [DOI] [PubMed] [Google Scholar]
- 3.Matullo KS, Ilyas A, Thoder JJ. CMC arthroplasty of the thumb: a review. Hand (N Y) 2007;2:232–239. doi: 10.1007/s11552-007-9068-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Heest AE, Kallemeier P. Thumb carpal metacarpal arthritis. J Am Acad Orthop Surg. 2008;16:140–151. doi: 10.5435/00124635-200803000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Vermeulen GM, Slijper H, Feitz R, et al. Surgical management of primary thumb carpometacarpal osteoarthritis: a systematic review. J Hand Surg Am. 2011;36:157–169. doi: 10.1016/j.jhsa.2010.10.028. [DOI] [PubMed] [Google Scholar]
- 6.Wajon A, Carr E, Edmunds I, Ada L. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database Syst Rev. 2009;(4):CD004631. doi: 10.1002/14651858.CD004631.pub3. [DOI] [PubMed] [Google Scholar]
- 7.Wajon A, Ada L, Edmunds I. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database Syst Rev. 2005;(4):CD004631. doi: 10.1002/14651858.CD004631.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Martou G, Veltri K, Thoma A. Surgical treatment of osteoarthritis of the carpometacarpal joint of the thumb: a systematic review. Plast Reconstr Surg. 2004;114:421–432. doi: 10.1097/01.prs.0000131989.86319.b1. [DOI] [PubMed] [Google Scholar]
- 9.Gervis WH. Excision of the trapezium for osteoarthritis of the trapezio-metacarpal joint. J Bone Joint Surg Br. 1949;31B:537–539. [PubMed] [Google Scholar]
- 10.Murley AH. Excision of the trapezium and osteoarthritis of the first carpo-metacarpal joint. J Bone Joint Surg Br. 1960;42:502–507. [Google Scholar]
- 11.Iyer KM. The results of excision of the trapezium. Hand. 1981;13:246–250. doi: 10.1016/s0072-968x(81)80004-6. [DOI] [PubMed] [Google Scholar]
- 12.Conolly WB, Rath S. Revision procedures for complications of surgery for osteoarthritis of the carpometacarpal joint of the thumb. J Hand Surg Br. 1993;18:533–539. doi: 10.1016/0266-7681(93)90166-d. [DOI] [PubMed] [Google Scholar]
- 13.Froimson AI. Tendon arthroplasty of the trapeziometacarpal joint. Clin Orthop Relat Res. 1970;70:191–199. [PubMed] [Google Scholar]
- 14.Burton RI, Pellegrini VD., Jr Surgical management of basal joint arthritis of the thumb. Part II. Ligament reconstruction with tendon interposition arthroplasty. J Hand Surg Am. 1986;11:324–332. doi: 10.1016/s0363-5023(86)80137-x. [DOI] [PubMed] [Google Scholar]
- 15.Weilby A. Resection arthroplasty of the first carpometacarpal joint. J Hand Surg. 1979;4:586. [Google Scholar]
- 16.Chang EY, Chung KC. Outcomes of trapeziectomy with a modified abductor pollicis longus suspension arthroplasty for the treatment of thumb carpometacarpal joint osteoarthritis. Plast Reconstr Surg. 2008;122:505–515. doi: 10.1097/PRS.0b013e31817d5419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Magnusson A, Bertheussen K, Weilby A. Ligament reconstruction of the thumb carpometacarpal joint using a modified Eaton and Littler technique. J Hand Surg Br. 1985;10:115–116. doi: 10.1016/s0266-7681(85)80036-x. [DOI] [PubMed] [Google Scholar]
- 18.Froimson AI. Tendon interposition arthroplasty of carpometacarpal joint of the thumb. Hand Clin. 1987;3:489–505. [PubMed] [Google Scholar]
- 19.Tomaino MM, Pellegrini VD, Jr, Burton RI. Arthroplasty of the basal joint of the thumb. Long-term follow-up after ligament reconstruction with tendon interposition. J Bone Joint Surg Am. 1995;77:346–355. doi: 10.2106/00004623-199503000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Tomaino MM. Ligament reconstruction tendon interposition arthroplasty for basal joint arthritis. Rationale, current technique, and clinical outcome. Hand Clin. 2001;17:207–221. [PubMed] [Google Scholar]
- 21.Belcher HJ, Nicholl JE. A comparison of trapeziectomy with and without ligament reconstruction and tendon interposition. J Hand Surg Br. 2000;25:350–356. doi: 10.1054/jhsb.2000.0431. [DOI] [PubMed] [Google Scholar]
- 22.Field J, Buchanan D. To suspend or not to suspend: a randomised single blind trial of simple trapeziectomy versus trapeziectomy and flexor carpi radialis suspension. J Hand Surg Eur Vol. 2007;32:462–466. doi: 10.1016/J.JHSB.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 23.Davis TRC, Brady O, Dias JJ. Excision of the trapezium for osteoarthritis of the trapeziometacarpal joint: a study of the benefit of ligament reconstruction or tendon interposition. J Hand Surg Am. 2004;29:1069–1077. doi: 10.1016/j.jhsa.2004.06.017. [DOI] [PubMed] [Google Scholar]
- 24.Davis TR, Brady O, Barton NJ, Lunn PG, Burke FD. Trapeziectomy alone, with tendon interposition or with ligament reconstruction? J Hand Surg Br. 1997;22:689–694. doi: 10.1016/s0266-7681(97)80426-3. [DOI] [PubMed] [Google Scholar]
- 25.Davis TRC, Pace A. Trapeziectomy for trapeziometacarpal joint osteoarthritis: is ligament reconstruction and temporary stabilisation of the pseudarthrosis with a Kirschner wire important? J Hand Surg Eur Vol. 2009;34:312–321. doi: 10.1177/1753193408098483. [DOI] [PubMed] [Google Scholar]
- 26.Li YK, White C, Ignacy TA, Thoma A. Comparison of trapeziectomy and trapeziectomy with ligament reconstruction and tendon interposition: a systematic review. Plast Reconstr Surg. 2011;128:199–207. doi: 10.1097/PRS.0b013e318217435a. [DOI] [PubMed] [Google Scholar]
- 27.Gangopadhyay S, McKenna H, Burke FD, Davis TRC. Five- to 18-year follow-up for treatment of trapeziometacarpal osteoarthritis: a prospective comparison of excision, tendon interposition, and ligament reconstruction and tendon interposition. J Hand Surg Am. 2012;37:411–417. doi: 10.1016/j.jhsa.2011.11.027. [DOI] [PubMed] [Google Scholar]
- 28.Burstin HR, Conn A, Setnik G, et al. Benchmarking and quality improvement: the Harvard Emergency Department Quality Study. Am J Med. 1999;107:437–449. doi: 10.1016/s0002-9343(99)00269-7. [DOI] [PubMed] [Google Scholar]
- 29.Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 30.Armstrong D. Clinical autonomy, individual and collective: the problem of changing doctors’ behaviour. Soc Sci Med. 2002;55:1771–1777. doi: 10.1016/s0277-9536(01)00309-4. [DOI] [PubMed] [Google Scholar]
- 31.Grol R. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care. 2001;39:II46–54. doi: 10.1097/00005650-200108002-00003. [DOI] [PubMed] [Google Scholar]
- 32.Grilli R, Lomas J. Evaluating the message: the relationship between compliance rate and the subject of a practice guideline. Med Care. 1994;32:202–213. doi: 10.1097/00005650-199403000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Kitto S, Petrovic A, Gruen RL, Smith JA. Evidence-based medicine training and implementation in surgery: the role of surgical cultures. J Eval Clin Pract. 2011;17:819–826. doi: 10.1111/j.1365-2753.2010.01526.x. [DOI] [PubMed] [Google Scholar]
- 34.Timmermans S. From autonomy to accountability: the role of clinical practice guidelines in professional power. Perspect Biol Med. 2005;48:490–501. doi: 10.1353/pbm.2005.0096. [DOI] [PubMed] [Google Scholar]
- 35.Hay MC, Weisner TS, Subramanian S, et al. Harnessing experience: exploring the gap between evidence-based medicine and clinical practice. J Eval Clin Pract. 2008;14:707–713. doi: 10.1111/j.1365-2753.2008.01009.x. [DOI] [PubMed] [Google Scholar]
- 36.Meakins JL. Evidence-based surgery. Surg Clin North Am. 2006;86:1–16. doi: 10.1016/j.suc.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 37.Benson LS. Thumb CMC arthritis: A challenge to code. Hand Surgery Quarterly. 2003 Autumn; [Google Scholar]
- 38.Stanley J. Arthroplasty and arthrodesis of the wrist. In: Wolfe SW, Hotchkiss RN, Green DP, editors. Green’s operative hand surgery. 6. Vol. 1. Philadelphia, PA: Elsevier Churchill Livingstone; 2011. pp. 429–464. [Google Scholar]
- 39.Geissler WB, Slade JF. Fractures of the carpal bones. In: Wolfe SW, Hotchkiss RN, Green DP, editors. Green’s operative hand surgery. 6. Vol. 1. Philadelphia, PA: Elsevier Churchill Livingstone; 2011. pp. 639–708. [Google Scholar]
- 40.Wasey N, Baughan J, de Gara CJ. Prophylaxis in elective colorectal surgery: the cost of ignoring the evidence. Can J Surg. 2003;46:279–284. [PMC free article] [PubMed] [Google Scholar]
- 41.Timmermans S, Mauck A. The promises and pitfalls of evidence-based medicine. Health Aff (Millwood) 2005;24:18–28. doi: 10.1377/hlthaff.24.1.18. [DOI] [PubMed] [Google Scholar]
- 42.Mueller GM. Arthrodesis of the trapezio-metacarpal joint for osteoarthritis. J Bone Joint Surg Br. 1949;31B:540–542. [PubMed] [Google Scholar]
- 43.Swanson AB. Finger joint replacement by silicone rubber implants and the concept of implant fixation by encapsulation. Ann Rheum Dis. 1969;28:47–55. [PMC free article] [PubMed] [Google Scholar]
- 44.Pellegrini VD, Jr, Burton RI. Surgical management of basal joint arthritis of the thumb. Part I. Long-term results of silicone implant arthroplasty. J Hand Surg Am. 1986;11:309–324. doi: 10.1016/s0363-5023(86)80136-8. [DOI] [PubMed] [Google Scholar]
- 45.Taylor EJ, Desari K, D’Arcy JC, Bonnici AV. A comparison of fusion, trapeziectomy and silastic replacement for the treatment of osteoarthritis of the trapeziometacarpal joint. J Hand Surg Br. 2005;30:45–49. doi: 10.1016/j.jhsb.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 46.Barron OA, Catalano LW. Thumb basal joint arthritis. In: Wolfe SW, Hotchkiss RN, Green DP, editors. Green’s operative hand surgery. 6. Vol. 1. Philadelphia, PA: Elsevier Churchill Livingstone; 2011. pp. 407–428. [Google Scholar]
- 47.Clancy C, Collins FS. Patient-Centered Outcomes Research Institute: the intersection of science and health care. Sci Transl Med. 2010;2:37. doi: 10.1126/scitranslmed.3001235. [DOI] [PubMed] [Google Scholar]