Abstract
Hemoptysis as a sequelae of past tubercular infection of lungs is a known occurrence. Hemoptysis in such a patient can result from a number of etiologies like tubercular reactivation, bronchiectasis, aspergiloma and vascular complications like hypervascularity from bronchial arteries, arteriovenous fistula formation, pseudoaneurysms, etc. Massive hemoptysis in such a patient is usually treated by bronchial artery embolization and occasionally by surgical lobectomy. A rare source of bleeding in such a patient is from Rasmussen's aneurysm arising from the pulmonary arteries. We report a young patient of treated pulmonary tuberculosis who had recurrent hemoptysis. He was treated earlier with bronchial artery embolization. On recurrence of hemoptysis, he was reevaluated and was found to have multiple Rasmussen's aneurysms arising from the pulmonary arteries, which were successfully treated by coil embolization.
Keywords: Rasmussen's aneurysm, Hemoptysis, Coil embolization
1. Introduction
Rasmussen's aneurysm, named after Fritz Valdemar Rasmussen, is an aneurysm arising from the pulmonary artery adjacent to or within a tuberculous cavity. Although it is reported in 5% of autopsy series1 of patients with tubercular cavities, only a few clinical case reports exist in literature.2, 3, 4, 5, 6, 7, 8, 9, 10 In patients of tuberculosis after an active infective etiology of hemoptysis has been ruled out, the cause of hemoptysis is generally looked for in the bronchial arteries. Bronchial arteries in such a patient gets hypertrophied and enlarged and show rich broncho-pulmonary communications, which are the usual source of bleed. Bronchial artery embolization using various substances like gel foam, PVA embolization particles, coils, etc. have been used to control massive hemoptysis. If no abnormal bronchial arteries are found, then surgical lobectomy is considered for the control of life-threatening bleed. Rasmussen's aneurysm, if present, can be another treatable cause of hemoptysis in such patients. We report one such patient who had recurrent hemoptysis despite prior bronchial artery embolization procedure, and on evaluation by CT pulmonary artery angiogram was found to have multiple Rasmussen's aneurysms arising from the pulmonary arteries, which were then successfully treated by coil embolization.
2. Case report
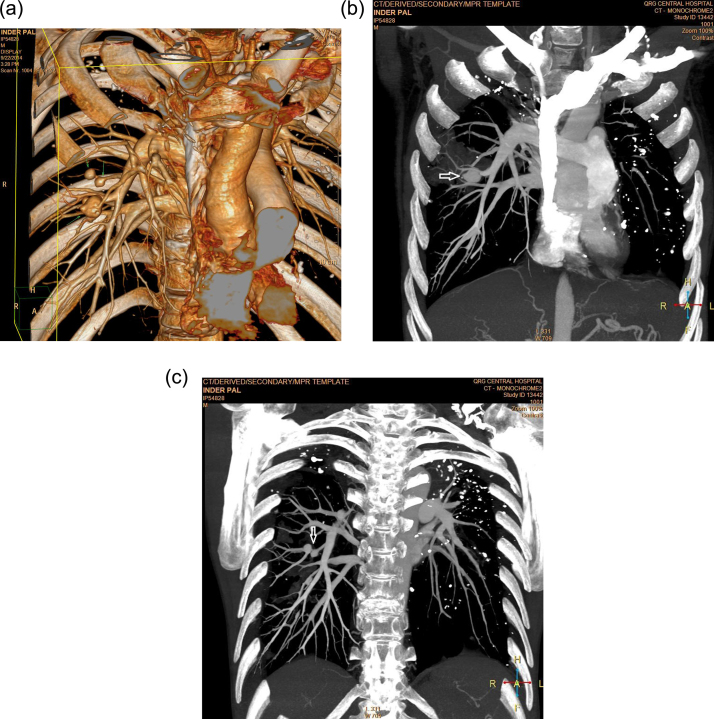
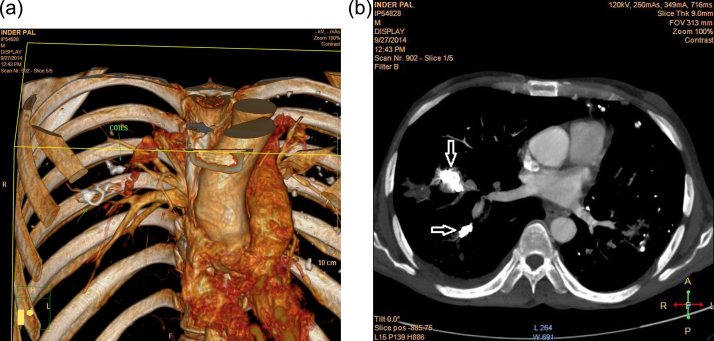
A 35-year-old male patient with a past history of tuberculosis of lung, which was treated earlier with anti-tubercular therapy, had presented with a history of recurrent hemoptysis. He had undergone bronchial artery embolization earlier at a different hospital. He, however, continued to have recurrent hemoptysis and was referred to us for evaluation and management. His evaluation revealed no evidence of active tuberculosis. He underwent CT pulmonary angiogram for evaluation of the cause of hemoptysis, which revealed three large Rasmussen's aneurysms arising from the branches of right pulmonary artery (Fig. 1a–c). In view of the reported literature of Rasmussen's aneurysm as a source of massive hemoptysis, he was taken up for the embolization procedure. His right pulmonary artery was selectively cannulated via right femoral venous approach. One large Rasmussen's aneurysm, which was arising from the anterior division of the inferior branch of right pulmonary artery, was selectively cannulated using a MicroFerret catheter (Cook Medical, Denmark). As this was a large aneurysm measuring 22 mm × 16 mm with a narrow neck, it was embolized with two soft MicroNester Coils (Cook Medical, Bloomington, IN, USA) released inside the aneurysm cavity and almost completely obliterating the aneurysmal cavity. The other two aneurysms (measuring 8 mm × 7 mm and 6 mm × 6 mm) were arising sequentially from the posterior division of the inferior branch of right pulmonary artery. There was a long normal segment of this feeding branch prior to the aneurysms. This branch was occluded by releasing two Hilal coils (Cook Medical, Bloomington, IN, USA) in the feeding portion of this branch prior to the aneurysms and thus occluding both of them. Repeat CT pulmonary angiogram confirmed the complete occlusion of all the aneurysms (Fig. 2a and b). This also resulted in successful control of hemoptysis.
Fig. 1.
Rasmussen's aneurysms, one large arising from anterior division and two smaller (marked by arrows) arising from posterior division of right inferior pulmonary artery as seen in (a) 3D virtually rendered image and (b and c) maximum intensity projections of CT pulmonary angiogram.
Fig. 2.
Complete occlusion of aneurysms by coils (marked by arrows) as seen in (a) 3D virtually rendered image and (b) maximum intensity transverse section projection of repeat CT pulmonary angiogram.
3. Discussion
Hemoptysis is a known complication of active or old burnt-out pulmonary tuberculosis. Mild hemoptysis in a patient with history of old treated tuberculosis of lungs is usually secondary to tubercular reactivation or secondary bacterial or Aspergillus infection of a tuberculous cavity. Chronic bronchitis or bronchiectasis in such patients could also be responsible for hemoptysis. Massive hemoptysis in them is often secondary to a vascular complication. Such massive hemoptysis usually originates from the bronchial circulation (95%) rather than pulmonary circulation.1 Bronchial arteries in such patients with chronic inflammation get hypertrophied and lead to development of broncho-pulmonary and arterio-venous communications, which are the common sources of bleed. Bronchial artery embolization has rightfully become the usual way to treat such patients with massive hemoptysis. Rasmussen's aneurysm in patients with cavitary tuberculosis is caused due to gradual weakening of adjacent pulmonary arterial wall. The granulation tissue replaces the adventitia and media of the pulmonary arterial wall, which is in turn replaced by fibrin, leading to thinning and pseudoaneurysm formation.11 In a study, 38% of patients who re-bled after successful bronchial artery embolizations for hemoptysis had Rasmussen aneurysms.5 Being rare, Rasmussen's aneurysms are not looked for and so are often missed. CT pulmonary angiography is the investigation of choice to diagnose them and should be done in patients with recurrent hemoptysis, especially if there is recurrence after prior bronchial artery embolization. Our case emphasizes this fact, as CT pulmonary angiography in this case was crucial in diagnosing Rasmussen's aneurysm, which would have been otherwise missed.
Embolization procedure technique for treating Rasmussen's aneurysm needs special care, as being pseudoaneurysm, they are very prone to rupture and bleeding during the procedure. Many commercially available substances including embospheres, coils, glue, gel foam, detachable balloons, stent grafts, etc. can be used for embolization. However, in view of their tendency to rupture, glue is considered preferable.10 In our case, we had used a soft MicroNester Coil (Cook Medical) to embolize the larger aneurysm. This coil is very soft and takes the shape of the aneurysm easily and without putting pressure on the wall, and that is why, this coil is also used for embolization in the intracranial vascular aneurysms. For the other aneurysm in our case, as there was a long feeding pulmonary artery branch, it could easily be occluded using the common Hilal coil (Cook Medical) without touching the Rasmussen's aneurysms.
4. Conclusions
Rasmussen's aneurysm is a rare and often missed cause of hemoptysis in patients with tubercular lung cavities. CT pulmonary angiography is the best investigation to confirm their existence and should be done in patients with recurrent hemoptysis, especially if it happens after bronchial arteries have been successfully embolized. Special care should be taken for embolization of Rasmussen's aneurysms, as they are very prone to rupture and bleeding.
Conflicts of interest
The authors have none to declare.
References
- 1.Santelli E.D., Katz D.S., Goldschmidt A.M., Thomas H.A. Embolization of multiple Rasmussen aneurysms as a treatment of haemoptysis. Radiology. 1994;193:396–398. doi: 10.1148/radiology.193.2.7972750. [DOI] [PubMed] [Google Scholar]
- 2.Kim H.Y., Song K.S., Goo J.M., Lee J.S., Lee K.S., Lim T.H. Thoracic sequelae and complications of tuberculosis. Radiographics. 2001;21:839–860. doi: 10.1148/radiographics.21.4.g01jl06839. [DOI] [PubMed] [Google Scholar]
- 3.Pantankar T., Prasad S., Deshmukh H., Mukherji S.K. Fatal haemoptysis caused by giant Rasmussen's aneurysm. Am J Roentgenol. 2000;174:262–263. doi: 10.2214/ajr.174.1.1740262. [DOI] [PubMed] [Google Scholar]
- 4.Remy J., Lemaitre L., Lafitte J.J., Vilain M.O., Saint Michel J., Steenhouwer F. Massive haemoptysis of pulmonary arterial origin: diagnosis and treatment. Am J Roentgenol. 1984;143:963–969. doi: 10.2214/ajr.143.5.963. [DOI] [PubMed] [Google Scholar]
- 5.Sanyika C., Corr P., Royston D., Blyth D.F. Pulmonary angiography and embolization for severe haemoptysis due to cavitary pulmonary tuberculosis. Cardiovasc Intervent Radiol. 1999;22:457–460. doi: 10.1007/s002709900432. [DOI] [PubMed] [Google Scholar]
- 6.Picard C., Parrot A., Boussaud V. Massive haemoptysis due to Rasmussen aneurysm: detection with helicoidal CT angiography and successful steel coil embolization. Intensive Care Med. 2003;29:1837–1839. doi: 10.1007/s00134-003-1912-y. [DOI] [PubMed] [Google Scholar]
- 7.Jayet P.Y., Denys A., Zellweger J.P. Successful embolization of Rasmussen's aneurysm for severe hemoptysis. Swiss Med Wkly. 2004;134:705–706. doi: 10.4414/smw.2004.10831. [DOI] [PubMed] [Google Scholar]
- 8.Hamano J., Shiotani S., Yamazaki K., Suzuki M., Ishikawa H. Postmortem computed tomographic (PMCT) demonstration of fatal haemoptysis by pulmonary tuberculosis – radiological-pathological correlation in a case of rupture of Rasmussen's aneurysm. Radiat Med. 2004;22:120–122. [PubMed] [Google Scholar]
- 9.van den Heuvel M.M., van Rensburg J.J. Images in clinical medicine: Rasmussen's aneurysm. N Engl J Med. 2006;355:e17. doi: 10.1056/NEJMicm050783. [DOI] [PubMed] [Google Scholar]
- 10.Keeling A.N., Costello R., Lee M.J. Rasmussen's aneurysm: a forgotten entity. Cardiovasc Intervent Radiol. 2008;31:196–200. doi: 10.1007/s00270-007-9122-6. [DOI] [PubMed] [Google Scholar]
- 11.Yoon W., Kim J.K., Kim Y.H., Chung T.W., Kang H.K. Bronchial and nonbronchial systemic artery embolization for life threatening hemoptysis: a comprehensive review. Radiographics. 2002;22:1399–1409. doi: 10.1148/rg.226015180. [DOI] [PubMed] [Google Scholar]