Abstract
Deep vein thrombosis (DVT) is a major health problem in pregnancy and postpartum period. Catheter-directed thrombolysis (CDT) is safe and effective in the management of symptomatic DVT. Value of CDT in postpartum DVT is not fully evaluated. We describe five patients presenting with acute iliofemoral DVT in their early postpartum period who were treated with mechanical thromboaspiration and CDT. The CDT was done using streptokinase infusion and unfractionated heparin. Percutaneous angioplasty was done in patients with symptomatic residual lesion following thrombolysis. Patients were discharged with oral anticoagulant and compression stockings. This approach was successful in all five cases. Percutaneous endovascular therapy using CDT, mechanical thromboaspiration, and balloon angioplasty is safe and effective in iliofemoral DVT in postpartum period.
Keywords: Angioplasty, Catheter-directed thrombolysis, Deep vein thrombosis, Mechanical thromboaspiration, Postpartum
1. Introduction
Worldwide, deep vein thrombosis (DVT) and venous thromboembolism (VTE) are major health problems with high mortality and morbidity in pregnancy and postpartum period.1 The high incidence of DVT and risk of VTE during pregnancy and postpartum period occurs due to hypercoagulable state.2 Catheter-directed thrombolysis (CDT) is a safe and effective method by lysing the thrombus and restoring the patency of the veins in proximal DVT.3 It reduces the incidence of post-thrombophlebitic syndrome (PTS) and improves the quality of life.3 Pregnancy and the postpartum period are considered as relative contraindications for thrombolysis.4 However, CDT of DVT may reduce long-term sequelae in these young patients by restoring early patency of veins.4 We share our experience of safety and efficacy of CDT in treatment of proximal DVT in postpartum period.
2. Case report
Eight patients were admitted to our hospital with proximal DVT in postpartum period in the last year. Among them, five patients were treated with CDT along with mechanical thromboaspiration, and the remaining three patients were treated with low molecular weight heparin and oral anticoagulant. The mean age of these patients was 22 years. The mean duration of symptoms before presentation was 9 (±4) days. Three patients had right lower limb DVT, one patient had left lower limb DVT, and another patient had bilateral lower limb DVT. Four patients had normal vaginal delivery, whereas one patient had second trimester abortion following trauma. All of these patients were primigravida and there was no family history of thrombotic disorder. Two patients had history of using oral contraceptive pills in the past. BMI was low or in normal range in these patients. All patients had iliofemoral DVT, three patients had extension into inferior vena cava (IVC), and one had additional renal vein thrombosis (RVT). After ruling out risk factors and contraindication for systemic thrombolysis, CDT was started locally through ipsilateral popliteal vein (PV). The mean duration of CDT was 128 (±16) h. Three patients had complete resolution of clot and another case had partial resolution. One case had received infusion of Urokinase after giving 2 days of Streptokinase infusion, as there was no significant improvement after giving streptokinase. In the patient with RVT with mild renal dysfunction, renal function was improved after CDT. Mechanical thromboaspiration was done by using a 7F multipurpose catheter (Cordis, Miami, Florida) and 50 cc syringe for aspiration. IVC filter was used in two patients prior to CDT and mechanical thromboaspiration. Percutaneous transluminal angioplasty (PTA) was done by using peripheral angioplasty balloon in patients for residual lesion in iliac veins. Three patients had minor bleeding from the local site; two patients required blood transfusion and two patients had thrombocytopenia which recovered gradually. In one patient, IVC filter could not be retrieved (Table 1). All patients improved symptomatically. At 6 months of follow-up, one patient had mild PTS. Three patients did not give consent for CDT. Table 1 describes the demographic, clinical features, and treatment outcome of these patients.
Table 1.
Demographic, clinical features and treatment outcome of treated patients.
| Variable | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 |
|---|---|---|---|---|---|
| Age | 24 years | 22 years | 29 years | 20 years | 23 years |
| Risk factor | Postpartum, left leg polio | Postpartum | Abortion, left ankle fracture | Postpartum | Postpartum |
| Onset after delivery | 8 days | 7 days | 10 days | 7 days | 10 days |
| Presentation | Left leg swelling, renal angle tenderness | Right leg swelling | Bilateral leg swelling | Right leg swelling | Right leg swelling |
| Duplex venography | Left iliofemoral, IVC and RVT | Rt. Iliofemoral + IVC thrombosis | B/L iliofemoral + IVC thrombosis | Rt. Iliofemoral thrombosis | Rt. Iliofemoral thrombosis |
| Treatment | CDT | CDT | CDT | CDT | CDT |
| Duration of CDT | 120 h | 140 h | 144 h | 110 h | 120 h |
| Result of CDT | Partial lysis | Complete lysis | Complete lysis | Complete lysis | Complete lysis |
| Angioplasty | PTA done | PTA done + IVC filter | PTA done + IVC filter | PTA done | PTA done |
| Adverse events of therapy | Nil | Minor bleeding, anemia, IVC filter not retrieved | Minor bleeding, Thrombocytopenia, anemia | Minor bleeding, Thrombocytopenia, anemia | Minor bleeding, anemia |
| Symptoms at discharge | Pain and edema decreased | Pain and edema decreased | Pain and edema decreased | Pain and edema decreased | Pain and edema decreased |
| Follow-up at 6 months | Mild PTS | No PTS | No PTS | No PTS | No PTS |
Intervention: CDT was done using PV cannulation. PV sheath insertion (8F sheath) was performed under ultrasound guidance. One patient had bilateral PV sheath insertion. Peripheral venogram was done through PV sheath to assess the extent of thrombus. The thrombotic lesion was crossed with a 0.035′ angled Terumo guide wire with 6F multipurpose (MP) guiding catheter (Cordis, Miami, Florida) and IVC venogram was performed to assess the proximal level of thrombus (Fig. 1). Multiple holes were made in the distal 5–10 cm of the MP catheter and it was placed in the proximal part of the DVT. Injection streptokinase 100,000 units/h infusion was given of which two-third dose (70,000 units/h) was through catheter and one-third dose (30000 units/h) through sheath. Injection of unfractionated heparin (UFH) 800–1000 units/h was given through the sheath and activated plasma thromboplastin time (APTT) was monitored to maintain APTT between 60 and 90 s. Mechanical thromboaspiration was done using 8F MP catheter attached with a 50 ml syringe in those patients who did not show response to thrombolysis. Venogram was repeated after 24 h and infusion was continued till there was a satisfactory result or any sign of adverse events present. Percutaneous transluminal angioplasty (PTA) was performed if there was significant residual stenosis in the affected vein (Fig. 2). The treatment was considered successful if there was resolution of thrombus, good antegrade flow, and less than 30% residual luminal area narrowing (Fig. 3), along with complete or partial resolution of symptoms of DVT like lower extremity pain and edema. Following thrombolytic therapy, patients were discharged with graduated compression stockings, and anticoagulated with oral nicoumalone for 6 months a year (or lifelong in case of prothrombotic disorder) according to the American College of Chest Physician (ACCP) guidelines.4 The International Normalized Ratio (INR) was maintained between 2 and 3. During follow-up of 6 months, only one patient had mild PTS and the remaining were completely free of symptoms.
Fig. 1.

IVC venogram showing the proximal level of DVT with involvement of right common iliac vein and extending into IVC.
Fig. 2.
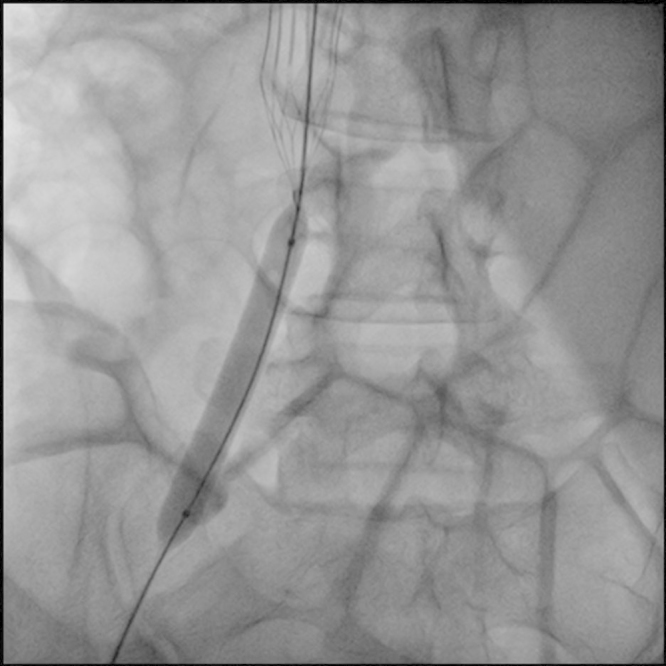
Peripheral venous angioplasty of right common iliac vein.
Fig. 3.

Venogram demonstrating >90% resolution of venous clot and IVC filter was also implanted in this patient.
3. Discussion
Pregnancy and postpartum period are associated with an overall 5–10 fold increased risk of VTE.5 The absolute risk is highest during and shortly after delivery. Furthermore, during the puerperium, the risk of developing DVT is significantly higher than antepartum.6, 7 In majority of the cases, DVT arises in left lower extremity due to a relative stenosis of the left common iliac vein where it lies between the lumbar vertebral body and the right common iliac artery.5 But in our cases, involvement of right leg was more than left leg without any obvious reason. The treatment of VTE has advanced significantly in recent years, but major challenges remain. Despite use of standard therapies, VTE continues to a significant risk factor for death or major disability.8 Significant portion of patients develop post-thrombophlebitic syndrome despite adequate anticoagulation therapy.9 In venous thromboembolic disease, CDT with or without assisted mechanical thrombolysis is becoming the standard of medical care in the treatment of acute DVT.10 Anticoagulation therapy is ineffective at removing thrombus of the deep venous system, and when extensive, DVT carries a high risk of developing PTE and PTS.11 To avoid PTS, aggressive therapy to remove venous thrombus/venous obstruction must be undertaken before irreversible valvular damage occurs.12 Nevertheless, during the last decade, advances in minimally invasive technologies have spurred a renaissance in the aggressive treatment of DVT using percutaneous techniques.11 Endovascular management using percutaneous mechanical thrombectomy alone or in combination with pharmacological thrombolytic agents has recently received much attention in the literature as a safe and effective means for the treatment of acute DVT.12 Fibrinolysis is relatively contraindicated during pregnancy and postpartum period due to high incidence of bleeding risk.4 A few studies which showed that CDT can be safely used in postpartum period.4, 7 Successful CDT in our patients also confirmed the same. But there are some differences between previous studies and treatment pattern in our patients. We have used streptokinase through popliteal vein approach of same side, whereas the previous study used alteplase as fibrinolytic agent. In a previous study, CDT with alteplase was used for a maximum period of 4 days,4 whereas, another study12 had used streptokinase for CDT through PV, similar to what we have done in our cases. We have used streptokinase for up to 6 days in our patients and all patients underwent mechanical thromboaspiration. The complications of CDT seen our cases were anemia (due to mechanical thromboaspiration), thrombocytopenia (heparin induced), minor bleeding, and nonretrieval of IVC filter. These were more than the previous study may be due to longer duration of CDT. But these adverse events were mild, nonlife threatening with the benefit of complete lysis. Thrombophilia screening was not performed in every case.
4. Conclusion
Our prospective case analysis demonstrated that percutaneous endovascular therapy consisting of CDT with PTA and/or stenting in selected cases may be safe and effective in iliofemoral DVT during post-partum period; however, larger studies are required to confirm the results.
Contributors
Srinivas BC was the primary operator in all these cases. Soumya Patra, Nagesh CM and Babu Reddy were also involved in the management of the patients. Soumya Patra reviewed the literatures and drafted the manuscript. Srinivas BC and Manjunath CN corrected the manuscript. All authors approved the final version of the manuscript.
Conflicts of interest
The authors have none to declare.
References
- 1.Ray J.G., Chan W.S. Deep vein thrombosis during pregnancy and the puerperium: a meta-analysis of the period of risk and the leg of presentation. Obstet Gynecol Surv. 1999;54:265–271. doi: 10.1097/00006254-199904000-00023. [DOI] [PubMed] [Google Scholar]
- 2.O’Connor D.J., Scher L.A., Gargiulo N.J., III, Jang J., Suggs W.D., Lipsitz E.C. Incidence and characteristics of venous thromboembolic disease during pregnancy and the postnatal period: a contemporary series. Ann Vasc Surg. 2011;25:9–14. doi: 10.1016/j.avsg.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 3.Jacobsen A.F., Drolsum A., Klow N.E., Dahl G.F., Qvigstad E., Sandset P.M. Deep vein thrombosis after elective cesarean section. Thromb Res. 2004;113:283–288. doi: 10.1016/j.thromres.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 4.Acharya G., Singh K., Hansen J.B., Kumar S., Maltau J.M. Catheter-directed thrombolysis for the management of postpartum deep venous thrombosis. Acta Obstet Gynecol Scand. 2005;84:155–158. doi: 10.1111/j.0001-6349.2005.00565.x. [DOI] [PubMed] [Google Scholar]
- 5.Gader A.A., Haggaz A.E., Adam I. Epidemiology of deep venous thrombosis during pregnancy and puerperium in Sudanese women. Vasc Health Risk Manag. 2009;5:85–87. [PMC free article] [PubMed] [Google Scholar]
- 6.McLintock C., Brighton T., Chunilal S., Dekker G. Recommendations for the diagnosis and treatment of deep venous thrombosis and pulmonary embolism in pregnancy and the postpartum period. Aust N Z J Obstet Gynaecol. 2012;52:14–22. doi: 10.1111/j.1479-828X.2011.01361.x. [DOI] [PubMed] [Google Scholar]
- 7.Virkus R.A., Jørgensen M., Broholm R., Bergholt T. Successful treatment of massive deep vein thrombosis using catheter-directed thrombolysis and inferior vena cava filter in a puerperal woman. Acta Obstet Gynecol Scand. 2012;91:269–270. doi: 10.1111/j.1600-0412.2011.01294.x. [DOI] [PubMed] [Google Scholar]
- 8.Anthony J.C. The ATTRACT Trial: rationale for early intervention for iliofemoral DVT. Perspect Vasc Surg Endovasc Ther. 2009;21:221–225. doi: 10.1177/1531003509359311. [DOI] [PubMed] [Google Scholar]
- 9.Camerota A.J., Paolini D. Treatment of acute iliofemoral deep venous thrombosis: a strategy of thrombus removal. Eur J Vasc Endovasc Surg. 2007;33:351–356. doi: 10.1016/j.ejvs.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 10.Benjamin O.P., Robert H., Ian M.L., Matt M.T., Peter J.E.H. Indications for catheter-directed thrombolysis in the management of acute deep venous thrombosis. Arterioscler Thromb Vasc Biol. 2010;30:669–674. doi: 10.1161/ATVBAHA.109.200766. [DOI] [PubMed] [Google Scholar]
- 11.Enden T., Haig Y., Kløw N.E., Slagsvold C.E. Long-term outcome after additional catheter-directed thrombolysis versus standard treatment for acute iliofemoral deep vein thrombosis (the CaVenT study): a randomised controlled trial. Lancet. 2012;379:31–38. doi: 10.1016/S0140-6736(11)61753-4. [DOI] [PubMed] [Google Scholar]
- 12.Elsharawy M., Elzayat E. Early results of thrombolysis vs anticoagulation in iliofemoral venous thrombosis, A randomised clinical trial. Eur J Vasc Endovasc Surg. 2002;24:209–214. doi: 10.1053/ejvs.2002.1665. [DOI] [PubMed] [Google Scholar]


