Abstract
Objective: Assess clinical results using two different protocols, 10 years after ACL reconstruction surgery with the central third of quadriceps muscle tendon (QT). Method: Between November /1997 and April/1998, 25 patients were submitted to 25 ACL reconstructions with QT by transtibial technique. The bone portion of the graft was fixated on femoral tunnel with interference screw and the tendinous portion of tibial tunnel with screw with washer. Two patients injured the new when playing soccer. Six patients were not available for follow-up (24%). Seventeen patients were evaluated, 15 men and two women, with mean age at surgery time of 28.53 ± 6.64 years. All patients were examined at six months, one year, and ten years after surgery. Clinical evaluation was made by the Lysholm scale, and the knee evaluation, with the Hospital for Special Surgery scale. Results: The patients had their injuries operated after 9.87 ± 14.42 months of the accident. According to Lysholm scale, the results at the end of the first year were 98.71 ± 2.47 and, after 10 years, 97.35 ± 3.12. Using the Hospital for Special Surgery scale, the mean score was 95.07 ± 5.23 in one year, and 94.87 ± 4.16 in 10 years. All patients returned to their professional activities with the same previous status. Fifteen (88.24%) patients were able to return to their sports activities, one by modifying the practice, while another one switched to another sport. No patient complained of pain on the donor area in the medium and long term. The sports return rate was excellent, and no changes were found on the femoropatellar joint.
Keywords: Knee, Anterior cruciate ligament, Quadriceps muscle, Muscle skeletal
INTRODUCTION
Over the last decade, ACL reconstructive surgery has become one of the most common in orthopedics. Its long-term success rate is confirmed by good and excellent results, ranging from 75% to 95%, considering stability, relief of symptoms, and return to sports(1).
Sachs et al.(2) showed that loss of quadriceps strength, extension deficit, and pain in the anterior knee are the most frequent complications of ACL reconstruction. The incidence of these problems was greater when using the patellar tendon (PT), considered the gold standard for ACL reconstruction. Quadriceps strength deficits occurred in 60.8% of cases one year after ACL reconstruction with PT. Although rare, complications such as patellar fracture and PT rupture, crepitation, tendinitis, and decreased patellar motion were reported, findings confirmed by other authors3, 4. In 1975, Cho(5) described ACL reconstruction using the intra-articular semimembranosus tendon. The gracilis (FT) was later added. Proponents of this technique have reported a lower incidence of pain in the anterior knee, lower frequency of patellar tendinitis, less quadriceps weakness with decreased risk of an impaired range of motion (ROM) of the knee(2). Concerns about the strength and greater elasticity of tendons in relation to the ACL, combined with the difficulty of fixation and decreased strength of knee flexion, have not been verified over the years(6). The use of the quadriceps tendon (QT) has been popularized by Marshall et al. (7), but with some not very promising initial results. Fulkerson and Langeland(8), Howe et al. (9) and Staubli et al.(10), and Staubli and Jakob(11), with more consistent studies, showed that the QT has the adequate size and strength to replace the ACL with less morbidity at the donor site. Today, the QT is becoming more popular(12).
The objective of this study is to evaluate the clinical results of patients who underwent ACL reconstruction with QT using two different protocols 10 years after surgery.
METHODOLOGY
Between November 1997 and April 1998, 25 patients underwent 25 ACL reconstructions with the QT plus a patellar bone fragment using the transtibial technique. The bone portion of the graft was fixed in the femoral tunnel with a metal interference screw and the tendon portion was fixed in the tibial tunnel with two Ethibond 2 sutures and a cancellous screw (post) with a washer. The surgical technique and rehabilitation have been previously described(13).
Six patients were lost during follow-up. We excluded two patients who broke the QT graft in sprains during soccer practice three and six years after surgery and were reoperated. The study group had 17 patients. All were examined at six months, one year and 10 years after surgery. Clinical evaluation was performed with the Lysholm scale and the Hospital for Special Surgery scale for the knee.
Of the 17 patients, there were 15 men and two women (Table 1) with a mean age of 28.53 ± 6.64 years at the time of surgery. The lesions were operated 9.87 ± 14.42 months after the injury. Two injuries were caused by falls from motorcycles, one from a fall from standing height, and 13 from sprains while playing soccer. One patient had a prior arthroscopic resection of the ACL stump. Six lesions of the medial meniscus and a medial femoral chondral lesion with 1 cm were found perioperatively(2). There were no injuries to the patellofemoral joint. We conducted one full and five partial meniscectomies. Later, osteosynthesis was performed as treatment for a patellar fracture that occurred in a fall six months after surgery, arthroscopic release was performed as treatment of knee arthrofibrosis, there were four meniscectomies, two of which were full and two partial, and one removal of the tibial post screw.
Table 1.
Patient characteristics.
| Number of patients | ||
|---|---|---|
| Gender | Male | 15 |
| Female | 2 | |
| Side of injury | Right | 9 |
| Left | 8 | |
| Age at surgery (years) | 28.53 | |
| Time between injury and surgery (months) | 6.64 | |
| Time between surgery and evaluation (years) | 10 | |
| Associated injury | Chondral lesion | 2 |
| Medial meniscus | 7 | |
| Medial Collateral Ligament (not addressed) | 0 | |
| Lateral meniscus | 0 | |
| Type of trauma | Sprain | 13 |
| Hyperextension | 0 | |
| Fall while (snow) skiing | 1 | |
| Fall from standing height | 1 | |
| Fall from a motorcycle at a slow speed | 2 | |
| Surgery pre-reconstruction | ACL stump resection | 1 |
| Surgery post-reconstruction | Arthroscopic retinaculum release | 1 |
| Partial lateral meniscectomy | 1 | |
| Patelar osteosynthesis | 1 | |
| Medial meniscectomy | 3 | |
Source: Belo Horizonte Center for Orthopedics and Traumatology.
Radiological examination of three planes was conducted, with the operated knee in a support, after 10 years follow-up to assess the presence or absence of osteoarthritis (Figures 1, 2, and 3).
Figure 1.
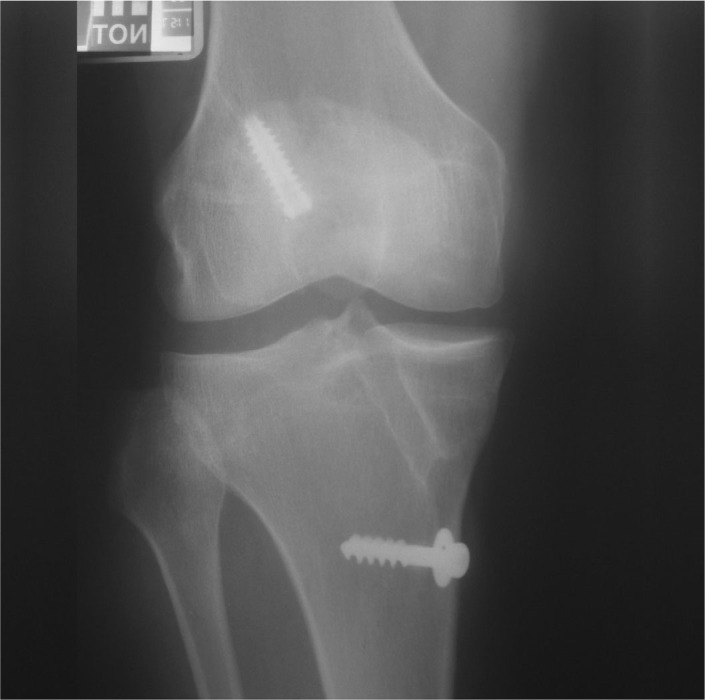
AP X-ray with the patient standing on one leg performed 10 years after ACL reconstruction
Figure 2.

Axial X-ray of the patella with knee flexed 30° performed 10 years after ACL reconstruction
Figure 3.

Lateral X-ray of the knee without weight-bearing performed 10 years after ACL reconstruction
RESULTS
According to the Lysholm scale (Table 2), the results after the first year were 98.71 ± 2.47 and 97.35 ± 3.12 after ten years. Using the Hospital for Special Surgery (HSS) scale (Table 3), the score was 95.07 ± 5.23 after one year and 94.87 ± 4.16 after 10 years (Table 4). The complaints that led to the largest loss of points on the Lysholm scale at the end of ten years were inconsistent and mild pain durings sports (17.65%-three patients), swelling after intense sports (11.76%-two patients), mild difficulty climbing stairs (17.65%-three patients), and mild and occasional difficulty in squatting (23.53%-four patients).
Table 2.
Lysholm scale results.
| LYSHOLM |
|||
|---|---|---|---|
| Item | Response | Patients | % |
| Limp (5 points) | No (5) | 16 | 94.12 |
| Mildly or periodically (3) | 1 | 5.88 | |
| Intensely or constantly (0) | 0.00 | ||
| Support (5 points) | No (5) | 17 | 100.00 |
| Crutch or cane (2) | 0.00 | ||
| Weight-bearing impossible (0) | 0.00 | ||
| Locking (15 points) | No (15) | 16 | 94.12 |
| Catching sensation but no locking (10) | 1 | 5.88 | |
| Occasional locking (6) | 0.00 | ||
| Frequent locking (2) | 0.00 | ||
| Knee locked during exam (0) | 0.00 | ||
| Instability (25 points) | Never (25) | 17 | 100.00 |
| Rarely during severe exertion (20) | 0.00 | ||
| Frequently during severe exertion (15) | 0.00 | ||
| Occasionally during daily activities (10) | 0.00 | ||
| Frequently during daily activities (5) | 0.00 | ||
| All the time (0) | 0.00 | ||
| Pain (25 points) | No (25) | 14 | 82.35 |
| Intermittent or mild during severe exertion (20) | 3 | 17.65 | |
| Strong during severe exertion (15) | 0.00 | ||
| Strong after walking more than 2 km (10) | 0.00 | ||
| Strong after walking less than 2 km (5) | 0.00 | ||
| Constant (0) | 0.00 | ||
| Swelling (10 points) | No (10) | 15 | 88.24 |
| After severe exertion (6) | 2 | 11.76 | |
| After ordinary activities (2) | 0.00 | ||
| Constant (0) | 0.00 | ||
| Stair climbing (10 points) | No problems (10) | 14 | 82.35 |
| Slight problems (6) | 3 | 17.65 | |
| One step at a time (2) | 0.00 | ||
| Impossible (0) | 0.00 | ||
| Squatting (5 points) | No problems (5) | 13 | 76.47 |
| Slight problems (4) | 4 | 23.53 | |
| Not past 90 degrees (2) | 0.00 | ||
| Impossible (0) | 0.00 | ||
Source: Belo Horizonte Center for Orthopedics and Traumatology.
Table 3.
HSS Scale Results
| THE HOSPITAL FOR SPECIAL SURGERY KNEE LIGAMENT RATING FORM | |||
|---|---|---|---|
| Item | Response | Absolute value | % |
| Symptoms (5 points) | |||
| Edema | No = 2 | 17 | 100.00 |
| Yes = 0 | 0.00 | ||
| Locking | No = 3 | 17 | 100.00 |
| Yes = 0 | 0.00 | ||
| Popping or snapping (20 points) | |||
| Intensity | None = 10 | 17 | 100.00 |
| Transient = 8 | 0.00 | ||
| Recurs < 1 day = 6 | 0.00 | ||
| Recurs < 1 week = 2 | 0.00 | ||
| Recurs > 1 week = 0 | 0.00 | ||
| Frequency | None = 10 | 17 | 100.00 |
| 1 a year = 8 | 0.00 | ||
| 2-6 a year = 6 | 0.00 | ||
| 1 a month = 4 | 0.00 | ||
| 1 a week = 2 | 0.00 | ||
| Daily = 0 | 0.00 | ||
| Function (20 points) | |||
| Work | Complete resumption = 4 | 17 | 100.00 |
| Limited or change of work = 2 | 0.00 | ||
| Unable due to knee = 0 | 0.00 | ||
| Sports | Complete return = 4 | 15 | 88.24 |
| Resumption with modification = 3 | 1 | 5.88 | |
| Changed sport = 2 | 1 | 5.88 | |
| Did not return = 0 | 0.00 | ||
| Ability to | Slow down = 4 | 17 | 100.00 |
| Run from one side to the other = 4 | 17 | 100.00 | |
| Jump = 4 | 17 | 100.00 | |
| Examination (45 points) | |||
| ROM | Normal = 3 | 15 | 88.24 |
| Limited flexion or extension = 1 | 2 | 11.76 | |
| Both = 0 | 0.00 | ||
| Swelling | No = 4 | 16 | 94.12 |
| Yes = 0 | 1 | 5.88 | |
| Thigh circumference | Equal or discrepancy < 1 cm = 2 | 1 | 5.88 |
| Discrepancy > 1 cm = 0 | 16 | 94.12 | |
| Lachman (end point) | Negative = 4 | 13 | 76.47 |
| 1+ = 3 | 4 | 23.53 | |
| 2+ = 2 | 0.00 | ||
| 3+ = 0 | 0.00 | ||
| Anterior drawer test | Negative = 2 | 12 | 70.59 |
| 1+ = 2 | 5 | 29.41 | |
| 2+ = 0 | 0.00 | ||
| 3+ = 0 | 0.00 | ||
| Posterior drawer test | Negative = 5 | 17 | 100.00 |
| 1+ = 3 | 0.00 | ||
| 2+ = 2 | 0.00 | ||
| 3+ = 0 | 0.00 | ||
| Pivot Shift | Negative or symmetric = 10 | 13 | 76.47 |
| Light, without movement = 8 | 4 | 23.53 | |
| 1+, slight movement = 4 | 0.00 | ||
| 2+, definite movement = 2 | 0.00 | ||
| 3+, movement and locking = 0 | 0.00 | ||
| MCL | Normal = 5 | 17 | 100.00 |
| 1+ = 3 | 0.00 | ||
| 2+ = 2 | 0.00 | ||
| 3+ = 0 | 0.00 | ||
| LCL | Normal = 5 | 17 | 100.00 |
| 1+ = 3 | 0.00 | ||
| 2+ = 2 | 0.00 | ||
| 3+ = 0 | 0.00 | ||
| Reverse Pivot Shift | Negative = 5 | 17 | 100.00 |
| Positive = 0 | 0.00 | ||
| Functional exam (10 points) | |||
| Jump on one foot-difference between the lower limbs | 90-100% = 10 | 14 | 82.35 |
| 75-90% = 7 | 3 | 17.65 | |
| 50-75% = 5 | 0.00 | ||
| 50% = 0 | 0.00 | ||
| Deductions | |||
| External support | Due to insecurity = 2 | 0.00 | |
| Due to instability = 4 | 0.00 | ||
| Pain | None = 0 | 0.00 | |
| Occasional = 2 | 2 | 11.76 | |
| After severe exertion = 5 | 2 | 11.76 | |
| After daily activities = 8 | 0.00 | ||
| Continual = 10 | 0.00 | ||
Source: Belo Horizonte Center for Orthopedics and Traumatology
Table 4.
Patient evolution according to scales used for evaluation.
| Summary of clinical evaluation |
||||
|---|---|---|---|---|
| Year 1 | Year 10 | |||
| Patients | Lysholm | HSS | Lysholm | HSS |
| 1 | 100 | 98 | 100 | 98 |
| 2 | 100 | 96 | 100 | 96 |
| 3 | 100 | 98 | 100 | 98 |
| 4 | 100 | 96 | 100 | 96 |
| 5 | 95 | 96 | 94 | 90 |
| 6 | 95 | 93 | 91 | 93 |
| 7 | 100 | 92 | 95 | 92 |
| 8 | 99 | 98 | 99 | 98 |
| 9 | 99 | 93 | 95 | 87 |
| 10 | 91 | 78 | 86 | 87 |
| 11 | 100 | 98 | 100 | 98 |
| 12 | 100 | 100 | 100 | 100 |
| 13 | 99 | 97 | 95 | 97 |
| 14 | 100 | 98 | 100 | 98 |
| 15 | 100 | 98 | 100 | 98 |
| 16 | 100 | 98 | 100 | 98 |
| 17 | 100 | 95 | 100 | 95 |
| Mean | 98.71 | 95.41 | 97.35 | 95.24 |
| Standard deviation | 2.57 | 4.99 | 4.11 | 4.02 |
| Variance | 6.48 | 24.87 | 16.40 | 16.19 |
Source: Belo Horizonte Center for Orthopedics and Traumatology.
In the HSS evaluation, all patients returned to work maintaining the same conditions as before the trauma. Fifteen (88.24%) patients returned to the same sport, one modifying the way it was practiced and another changed sports. Two patients who underwent total medial meniscectomy developed medial femorotibial osteoarthritis and a limited ROM. Among the patients, 16 had a thigh diameter 2 cm lower than the other leg. The Lachman test was negative in 13 patients (76.47%) and +/++++ in four. The anterior drawer test was negative in 12 patients (70.59%) and +/++++ in five. The pivot test was negative in 13 patients (76.47%) and light without movement in four.
No patient complained of pain at the graft donor site from four weeks after surgery until the final evaluation. Four patients had a contralateral ACL rupture during sports activities, three sprains while playing soccer (which occurred three, four, and ten years after surgery), and one while dancing three years after the procedure.
Three patients had some reduction of the medial femorotibial joint space in the radiological examination. These patients underwent meniscectomy. There were no decreases in the patellofemoral joint space, with the exception of one patient who suffered a fractured patella six months after surgery after falling from a ladder (Figure 4).
Figure 4.
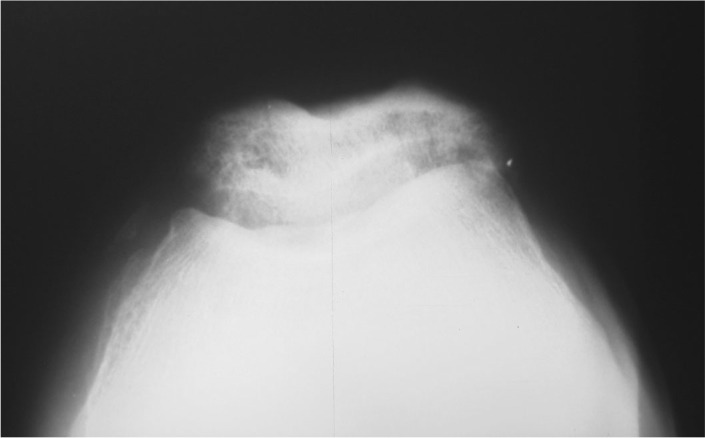
Axial radiograph of the patella in 30° of knee flexion after ACL reconstruction in a patient who suffered a fractured patella six months after surgery and underwent internal fixation with a tension band that has already been removed
DISCUSSION
ACL reconstruction aims to stabilize the knee. The restoration of kinematics minimizes the abnormal forces on the femorotibial interface. Recurrent episodes of instability after ACL rupture are often associated with meniscal lesions and premature osteoarthritis. Arthroscopies performed in patients with old and untreated ACL injuries show a large number of meniscal and chondral injuries. These joints have a high incidence of osteoarthritis, even after reconstruction14, 15.
The quadriceps tendon is part of the knee extensor apparatus. It covers the femoral trochlea as the knee is bent. It consists of multiple layers of collagen that vary in shape and size. These layers overlap obliquely and longitudinally, forming a complex tension band. The most anterior part of the rectus femoris muscle creates an aponeurosis in front of the patella, which is called the prepatellar retinaculum14, 16. The most posterior part of the QT merges with the most anterior part of the synovial membrane. Suprapatellar fat covers its distal part.
Harris et al.(17) demonstrated that, on average, the QT is 1.8 times thicker than the PT. At a distance of 7 to 10 mm between the tendon and articular cartilage, it creates a safe area for graft removal without trauma to the articular surface of the patella. The QT is sufficiently wide (averaging 27 mm) for the withdrawal of grafts of 10 mm in diameter. It also presents asymmetric insertion with a slight lateral deviation of its fibers. It is suggested that removal of the graft should follow this direction(17).
Using a 10-mm central area of the QT and PT as its basis, studies by Staubli and Jakob(11) have shown that the QT has a length between 64.4 mm and 61.9 mm according to the type of preparation and the forces acting on the piece. The PT has a length between 36.8 mm and 34.5 mm under the same research conditions. They noted that the QT has a wide area of attachment on the patella. The most anterior fibers of the QT advance prior to the patella, forming an aponeurosis that creates a tension band system. The aponeurosis fuses with the most anterior fibers of the PT. In these cuts, the same authors showed that the myotendinous junction of the QT is located 85 mm proximal to the base of the patella. In PT cuts, the authors drew attention to the small area of insertion of the PT at the patella in relation to the QT.
According to Staubli and Jakob(11), the analysis of the tensile strength of grafts 10-mm thick taken from the central part of the QTs and PTs of young adults (mean age 24.9 years, ranging from 19 to 32 years) revealed that the breaking point for tendons without previous preparation is 2,173N (± 618N) for the QT and 1,953N (± 325N) for the PT. In studies of the cycles of resistance, when subjected to 200 cycles from 50 to 800N with a frequency of 0.5 Hz, the point of failure for the QT is 2,353N (± 495N) and 2,376N (± 152N) for the PT. Despite the size, thickness, shape, and area of the PT and QT being different at the beginning of testing, the breaking points and the energy required for failure were not significantly different. The 200N difference between the results has no clinical significance. Harris et al.(17), in their work on the strength of the QT showed that the failure of the suture occurred at 692N (± 181N) and the failure of the tendon occurred at 1,075N (± 449N). This breaking point was 1.36 times higher for the QT compared with the PT.
Discomfort in the anterior knee after ACL reconstruction remains unresolved. Many causes have been proposed, including limitations of the ROM after surgery, chondromalacia, an inadequate rehabilitation program, pain at the graft donor site, presence of fixed contracture, a reduction in the size of the TP, low patella, changes in glutamate and substance-P18, 19, 20, 21. Deehan et al.(16) found a low incidence (8%) of crepitation in the patellofemoral joint after ACL reconstruction with patellar tendon. McDaniel and Dameron(22) found 45%. Deehan et al.(16) also report that after five years of follow-up, 91% of their patients had no or mild pain in the patellar tendon. Pain was a persistent problem during squatting, with 44% of patients describing discomfort when kneeling five years after surgery. There was no pain in the graft donor site for the patients in this study. Patellar tendinitis was rare in the first six months postoperatively and showed rapid resolution with stretching exercises.
Because it is a technique that has been rarely used in the recent past, there are few studies reporting on long-term evaluation. Chen et al.(23) evaluated 34 patients with follow-up ranging from four to seven years, with an average of 62 months. There were 94% good and excellent results based on the Lysholm scale. The return to moderate or extreme sports occurred in 76% of patients. Ligament laxity of less than 2 mm was observed in 88 patients. Using the IKDC scale, 91% of patients had a normal or nearly normal knee. The authors conclude that the QT is a good choice for ACL reconstruction.
Lee et al.(24) clinically evaluated 67 patients with a mean follow-up of 41 months. Based on the Lysholm scale, patients progressed from 71 points preoperatively to 90 postoperatively (P < 0.05). In the IKDC scale, 94% of patients were grade A and B. Isokinetic peak torque in extension was 82% and 89% compared with the other knee at one and two years postoperatively, respectively. There were no changes in the Insall-Salvati index or in patellar congruence.
Joseph et al.(25) compared three different grafts for ACL reconstruction. They reported that patients in the QT group needed fewer analgesics and recovered active extension faster than the group in which the patellar ligament was used.
In our country, Coelho et al.(26), Cortellazo et al.(27), and Guimarães et al.13, 28, 29 have published studies on the use of the QT graft in ACL reconstruction.
The QT has been successfully used for revision surgery for ACL reconstruction and dual-band reconstruction of the ACL30, 31, 32. Antonogiannakis et al.(33) studied the QT in ACL reconstructive surgery without the patellar bone block, with good results.
Pigozzi et al.(34) compared the isokinetic evolution of patients operated with the PL and the QT. They concluded that the strength deficit in the QT group was smaller and that good recovery of strength in this group after six months postoperatively should encourage the use of the QT in ACL reconstructions.
One indicator of successful ACL reconstruction is the rate of return to sports. Such an event may be influenced by the preoperative status of the individual, expectations, patient safety, rehabilitation, and the type of sport. Gobbi and Francisco(35) evaluated 100 athletes who underwent ACL reconstruction with the PT (n = 50) and flexor tendons (n = 50). They observed that 64% returned to the same sport at the same level, 24% changed their sport, and 11% stopped sports activity. There was no difference between the two groups of patients. Patients in this study showed a greater return to sport compared with the findings of Gobbi and Francisco(35).
The importance of preserving the meniscus for patients with ligament injury requires our attention. Gillquist and Messner(36) reported that concomitant injuries of the ACL and meniscus increase the incidence of degenerative changes in the knee. Cohen et al.(37) showed the negative association between meniscectomy, patients with ACL injury who have undergone surgery, and osteoarthritis in the long term. Carvalho Junior et al.(38) showed the effects of meniscectomy on the results of ACL reconstruction. In this study, the three patients with the worst scores underwent total meniscectomy, one during the primary surgery and the other two, years later.
It was observed that, even with stable knees, many patients required further interventions to correct a meniscus and/or chondral injury. The authors believe that secondary lesions associated with ACL injury continue to deteriorate the knee over time, although stability has been restored. Fithian et al.(39) showed a high incidence of delayed degeneration in patients undergoing ACL reconstruction. It would be desirable that patients with major meniscal injuries be discouraged from returning to certain sports.
Another important factor was the high rate of contralateral ACL injury observed (17.65%). There are several theories to explain this finding. One of them links this observation to the deficit in isokinetic evaluation of the contralateral (non-operated) limb, a fact already observed by Guimarães et al.(28)
This article has limitations. The principal author has the use of the QT as his first option for ACL reconstruction. This made a comparative study between two different types of grafts unfeasible. The number of patients studied is small. Annual assessments would be important to provide details of the patients' evolution. Preoperative clinical patient data were missing, lost in the files.
CONCLUSION
The QT graft is a good choice for ACL reconstruction, even 10 years after surgery. There was no pain at the donor graft site in the medium and long term. The rate of return to sport was excellent and there were no changes in the patellofemoral joint.
Footnotes
Study completed at the Center for Orthopedics and Traumatology, Belo Horizonte, MG.
REFERENCES
- 1.Wetzler MJ, Bartolozzi AR, Gillespie MJ. Revision anterior cruciate ligament reconstruction. Oper Tech Orthop. 1996;6:181–189. [Google Scholar]
- 2.Sachs RA, Daniel DM, Stone ML, Garfein RF. Patellofemoral problems after anterior cruciate ligament reconstruction. Am J Sports Med. 1989;17(6):760–765. doi: 10.1177/036354658901700606. [DOI] [PubMed] [Google Scholar]
- 3.Langan P, Fontanetta AP. Rupture of patellar tendon after use of its central third. Orthop Rev. 1987;16(3):317–321. [PubMed] [Google Scholar]
- 4.Rosenberg TD, Franklin JL, Baldwin GN, Nelson KA. Extensor mechanism function after patellar tendon graft harvest for anterior cruciate ligament reconstruction. Am J Sports Med. 1992;20(5):519–525. doi: 10.1177/036354659202000506. [DOI] [PubMed] [Google Scholar]
- 5.Cho KO. Reconstruction of the anterior cruciate ligament by semitendinosus tenodesis. J Bone Joint Surg Am. 1975;57:608–612. [PubMed] [Google Scholar]
- 6.Eriksson K, Anderberg P, Hamberg P, Lofgren AC, Bredenberg M, Westman I, Wredmark T. A comparison of quadruple semitendinosus and patellar tendon grafts in reconstruction of anterior cruciate ligament. J Bone Joint Surg. 2001;83:348–354. doi: 10.1302/0301-620x.83b3.11685. [DOI] [PubMed] [Google Scholar]
- 7.Marshall JL, Warren RF, Wickiewicz TL, Reider B. The anterior cruciate ligament: a technique for repair and reconstruction. Clin Orthop Relat Res. 1979;(143):97–106. [PubMed] [Google Scholar]
- 8.Fulkerson JP, Langeland R. An alternative cruciate reconstruction graft: the central quadriceps tendon. Arthroscopy. 1995;11(2):252–254. doi: 10.1016/0749-8063(95)90078-0. [DOI] [PubMed] [Google Scholar]
- 9.Howe JG, Johnson RJ, Kaplan MJ, Fleming B, Jarvinen M. Anterior cruciate ligament reconstruction using quadriceps patellar tendon graft. Part I. Long-term followup. Am J Sports Med. 1991;19(5):447–457. doi: 10.1177/036354659101900505. [DOI] [PubMed] [Google Scholar]
- 10.Staubli HU, Schatzmann L, Brunner P, Rincon L, Nolte LP. Quadriceps tendon and patellar ligament: cryosectional anatomy and structural properties in young adults. Knee Surg Sports Traumatol Arthrosc. 1996;4(2):100–110. doi: 10.1007/BF01477262. [DOI] [PubMed] [Google Scholar]
- 11.Staubli HU, Jakob RP. Central quadriceps tendon for anterior cruciate ligament reconstruction. Part I: morphometric and biochemical evaluation. Am J Sports Med. 1997;25(5):725–727. [PubMed] [Google Scholar]
- 12.Almazan Diaz A, Cruz Lopez F, Perez Jimenez FX, Ibarra Ponce de Leon JC. Minimally invasive quadriceps tendon harvest. Arthroscopy. 2006;22(6):679.e1–679.e3. doi: 10.1016/j.arthro.2005.09.022. [DOI] [PubMed] [Google Scholar]
- 13.Guimaraes MV. Reconstrução artroscópica do ligamento cruzado anterior: estudo comparativo entre os enxertos de ligamento patelar e de tendão do quadríceps. Rev Bras Ortop. 2004;39(2):130–141. [Google Scholar]
- 14.Jomha NM, Borton DC, Clingeleffer AJ, Pinczewski LA. Long-term osteoarthritic changes in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res. 1999;(358):358–393. [PubMed] [Google Scholar]
- 15.Dandy DJ, Hobby JL. Anterior cruciate ligament reconstruction. J Bone Joint Surg Br. 1998;80(2):189–190. doi: 10.1302/0301-620x.80b2.8582. [DOI] [PubMed] [Google Scholar]
- 16.Deehan DJ, Salmon LJ, Webb VJ, Davies A, Pinczewski LA. Endoscopic reconstruction of the anterior cruciate ligament with an ipsilateral patellar tendon autograft. A prospective longitudinal five-year study. J Bone Joint Surg Br. 2000;82(7):984–991. doi: 10.1302/0301-620x.82b7.10573. [DOI] [PubMed] [Google Scholar]
- 17.Harris NL, Smith DA, Lamoreaux L, Purnell M. Central quadriceps tendon for anterior cruciate ligament reconstruction. Part I: Morphometric and biomechanical evaluation. Am J Sports Med. 1997;25(1):23–28. doi: 10.1177/036354659702500105. [DOI] [PubMed] [Google Scholar]
- 18.Aglietti P, Buzzi R, D'Andria S, Zaccherotti G. Patellofemoral problems after intraarticular anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 1993;(288):288–294. [PubMed] [Google Scholar]
- 19.Shino K, Nakagawa S, Inoue M, Horibe S, Yoneda M. Deterioration of patellofemoral articular surfaces after anterior cruciate ligament reconstruction. Am J Sports Med. 1993;21(2):206–211. doi: 10.1177/036354659302100208. [DOI] [PubMed] [Google Scholar]
- 20.Hantes ME, Zachos VC, Bargiotas KA, Basdekis GK, Karantanas AH, Malizos KN. Patellar tendon length after anterior cruciate ligament reconstruction: a comparative magnetic resonance imaging study between patellar and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc. 2007;15(6):712–719. doi: 10.1007/s00167-006-0272-x. [DOI] [PubMed] [Google Scholar]
- 21.Witonski D, Wagrowska-Danielewicz M. Distribution of substance-P nerve fibers in the knee joint in patients with anterior knee pain syndrome. A preliminary report. Knee Surg Sports Traumatol Arthrosc. 1999;7(3):177–183. doi: 10.1007/s001670050144. [DOI] [PubMed] [Google Scholar]
- 22.McDaniel WJ, Jr, Dameron TB., Jr Untreated ruptures of the anterior cruciate ligament. A follow-up study. J Bone Joint Surg Am. 1980;62(5):696–705. [PubMed] [Google Scholar]
- 23.Chen CH, Chuang TY, Wang KC, Chen WJ, Shih CH. Arthroscopic anterior cruciate ligament reconstruction with quadriceps tendon autograft: clinical outcome in 4-7 years. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1077–1085. doi: 10.1007/s00167-006-0111-0. [DOI] [PubMed] [Google Scholar]
- 24.Lee S, Seong SC, Jo H, Park YK, Lee MC. Outcome of anterior cruciate ligament reconstruction using quadriceps tendon autograft. Arthroscopy. 2004;20(8):795–802. doi: 10.1016/j.arthro.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 25.Joseph M, Fulkerson J, Nissen C, Sheehan TJ. Short-term recovery after anterior cruciate ligament reconstruction: a prospective comparison of three autografts. Orthopedics. 2006;29(3):243–248. doi: 10.3928/01477447-20060301-14. [DOI] [PubMed] [Google Scholar]
- 26.Coelho MG, Souza JMG, Caldas MTL. Reconstrução “all-inside” do ligamento cruzado anterior do joelho com enxerto da parte central do tendão quadricipital. Descrição técnica. Rev Bras Ortop. 1998;33(5):357–362. [Google Scholar]
- 27.Cortelazo MJ, Cohen M, Mestriner LA, Carneiro FM. Reconstrução artroscópica do ligamento cruzado anterior com enxerto do tendão quadricipital: estudo das características dimensionais do tendão e da técnica. Nota preliminar. Rev Bras Ortop. 2002;37(6):247–255. [Google Scholar]
- 28.Guimarães MV, Cunha FM, Silva WN. Reconstrução do ligamento cruzado anterior utilizando enxerto de tendão do quadríceps: avaliação clínica e isocinética. Rev Bras Ortop. 2005;40(4):182–192. [Google Scholar]
- 29.Guimaraes MV, Murta Filho JB, Baumfeld DS, Da Silva WN. Ensanchamiento del tunel tibial tras reconstruir LCA con injerto de tendon cuadriceps: comparacion entre tres tecnicas de fijacion. Artrosc. (B. Aires) 2007;14(2):111–118. [Google Scholar]
- 30.Garofalo R, Djahangiri A, Siegrist O. Revision anterior cruciate ligament reconstruction with quadriceps tendon-patellar bone autograft. Arthroscopy. 2006;22(2):205–214. doi: 10.1016/j.arthro.2005.08.045. [DOI] [PubMed] [Google Scholar]
- 31.Noronha JC. Reconstruction of the anterior cruciate ligament with quadriceps tendon. Arthroscopy. 2002;18(7):E37. doi: 10.1053/jars.2002.30063. [DOI] [PubMed] [Google Scholar]
- 32.Kim SJ, Jung KA, Song DH. Arthroscopic double-bundle anterior cruciate ligament reconstruction using autogenous quadriceps tendon. Arthroscopy. 2006;22(7):797. doi: 10.1016/j.arthro.2005.09.027. [DOI] [PubMed] [Google Scholar]
- 33.Antonogiannakis E, Yiannakopoulos CK, Hiotis I, Karabalis C, Babalis G. Arthroscopic anterior cruciate ligament reconstruction using quadriceps tendon autograft and bioabsorbable cross-pin fixation. Arthroscopy. 2005;21(7):894. doi: 10.1016/j.arthro.2005.04.099. [DOI] [PubMed] [Google Scholar]
- 34.Pigozzi F, Di Salvo V, Parisi A, Giombini A, Fagnani F, Magini W. Isokinetic evaluation of anterior cruciate ligament reconstruction: quadriceps tendon versus patellar tendon. J Sports Med Phys Fitness. 2004;44(3):288–293. [PubMed] [Google Scholar]
- 35.Gobbi A, Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg Sports Traumatol Arthrosc. 2006;14(10):1021–1028. doi: 10.1007/s00167-006-0050-9. [DOI] [PubMed] [Google Scholar]
- 36.Gillquist J, Messner K. Anterior cruciate ligament reconstruction and the long-term incidence of gonarthrosis. Sports Med. 1999;27(3):143–156. doi: 10.2165/00007256-199927030-00001. [DOI] [PubMed] [Google Scholar]
- 37.Cohen M, Amaro JT, Ejnisman B, Carvalho RT, Nakano KK, Peccin MS. Anterior cruciate ligament reconstruction after 10 to 15 years: association between meniscectomy and osteoarthrosis. Arthroscopy. 2007;23(6):629–634. doi: 10.1016/j.arthro.2007.03.094. [DOI] [PubMed] [Google Scholar]
- 38.Carvalho Junior LH, Pidner Neto H, Schuffner FA. Efeitos da meniscectomia no resultado da reconstrução do ligamento cruzado anterior. Rev Bras Ortop. 2004;39(7):357–362. [Google Scholar]


