Abstract
Objective: To evaluate the efficacy of suprascapular nerve block in combination with infusion of anesthetic into the subacromial space, compared with interscalene block. Methods: Forty-five patients with small or medium-sized isolated supraspinatus tendon lesions who underwent arthroscopic repair were prospectively and comparatively evaluated through random assignation to three groups of 15, each with a different combination of anesthetic methods. The efficacy of postoperative analgesia was measured using the visual analogue scale for pain and the analgesic, anti-inflammatory and opioid drug consumption. Inhalation anesthetic consumption during surgery was also compared between the groups. Results: The statistical analysis did not find any statistically significant differences among the groups regarding anesthetic consumption during surgery or postoperative analgesic efficacy during the first 48 hours. Conclusion: Suprascapular nerve block with infusion of anesthetic into the subacromial space is an excellent alternative to interscalene block, particularly in hospitals in which an electrical nerve stimulating device is unavailable.
Keywords: Rotator cuff, Shoulder, Arthroscopy, Anesthesia, Nerve block
INTRODUCTION
After a surgical procedure on the shoulder joint, many patients report intense pain, especially during the first 48 hours, which has the consequence that most of them use large quantities of analgesics during this period1, 2.
With the advent of arthroscopic surgery, many of these operations have become outpatient procedures. However, pain is still a matter of concern among physicians and patients, given that controlling it outside of the hospital environment using intravenous analgesics becomes impracticable(3).
In most institutions, shoulder arthroscopy is performed under general anesthesia in combination with interscalene block(4). However, complications such as cardiac intoxication, pneumothorax and loss of consciousness through administration of anesthetic have been described(5). In addition, the efficacy of the anesthetic depends on the anesthesiologist's experience, given that in most Brazilian hospitals, electrical nerve stimulating devices are not yet available(6).
Recently, new anesthetic techniques have been studied, with evaluation of their intraoperative and postoperative efficacy, such as continuous infusion of ropivacaine into the subacromial space, intra-articular anesthesia and suprascapular nerve block2, 7, 8.
The objective of this study was to prospectively evaluate the intra and postoperative efficacy of suprascapular nerve block combined with infusion of anesthetic into the subacromial space, and to compare this with interscalene block, without using an electrical nerve stimulating device.
MATERIALS AND METHODS
Between January 2006 and November 2007, all of our patients with rotator cuff injuries were candidates for this study. We included 45 patients with small or medium-sized lesions in this study, out of a total of 157 arthroscopic procedures performed within our service to repair rotator cuff injuries during this period. The patients included were classified using magnetic resonance, had an indication for arthroscopic repair and did not have any histories of previous surgery on the affected shoulder. Patients with large or extensive lesions were excluded, as were those who did not agree to participate in the study. The patients were selected from among those who were referred to the Shoulder and Elbow Surgery Group of Mario Covas State Hospital, in Santo André, by primary care physicians in the ABC region.
The patients were divided randomly into three different groups. The randomization was performed using the minimization method, thus ensuring that the three groups presented similar numbers of patients. The patients in group A underwent arthroscopic repair of the rotator cuff injury under general anesthesia in combination with interscalene block, without using an electrical nerve stimulating device. The patients in group B underwent general anesthesia in combination with suprascapular nerve block and infusion of anesthetic into the subacromial space moments before the surgical procedure, and the patients in group C underwent the same arthroscopic procedure, but under general anesthesia alone, and only after the surgical procedure were suprascapular nerve block and infusion of anesthetic into the subacromial space performed, in order to evaluate the consumption of anesthetic during the surgical procedure, as a control group. All the anesthetic procedures were performed by a single experience anesthesiologist at the hospital.
Among the 45 patients, 32 were female and 13 were male. No patients were excluded during the period evaluated. The patients' ages ranged from 39 to 76 years (mean of 56 years), and the dominant side was affected in 33 patients.
In group A, 10 patients were female and five were male. Their mean age was 54 years (ranging from 39 to 65 years). The dominant shoulder was affected in 11 cases. In group B, 11 patients were female and four were male. Their mean age was 57 years (ranging from 45 to 69 years) and the dominant side was affected in 12 patients. In group C, 11 patients were female and four were male. Their mean age was 57 years (ranging from 47 to 76 years) and the dominant shoulder was affected in 10 patients.
For all the patients, the pre-anesthetic medication used was midazolam (3 mg), cefalotin (2 g) and ranitidine (50 mg). General anesthesia was induced using alfentanil (40 mg/kg), propofol (3 mg/kg) and rocuronium (0.6 mg/kg), and it was maintained using 3 l/min of 50% O2/NO2 plus 2% isofluorane. Interscalene block was performed using 2 mg/kg of 0.5% ropivacaine and suprascapular nerve block was performed using two thirds of 2 mg/kg of 0.5% ropivacaine. The remaining third was applied in the subacromial space. In all cases, the anesthesia was reversed using atropine (0.01 mg/kg) and prostigmine (0.02 mg/kg).
We calculated the consumption of inhalation anesthetic during the surgical procedure in order to compare it between the groups.
Arthroscopic procedures were performed to repair lesions to the supraspinal tendon using suture anchors, and to perform acromioplasty.
After the surgery, all the patients were immobilized using functional slings and received simple analgesics, opioid analgesics and anti-inflammatory agents, which were applied as requested by the patients. The quantities of drugs used in each group, over the first 48 hours, were compared between the three groups.
To evaluate the anesthetic efficacy in each group, comparisons of pain intensity during the postoperative period were made for each patient by means of visual pain scales (VAS) (Figure 1)(9). All the patients were questioned by a physician who was unaware of which anesthetic method had been administered. The evaluation was performed both preoperatively and postoperatively: immediately after the operation and after the first eight, 16, 24 and 48 hours after the surgery. Another parameter studied was the consumption of analgesic, anti-inflammatory and opioid drugs over the first 48 hours.
Figure 1.
Visual pain scale (VAS)
The statistical analysis was performed using the SPSS (Statistical Package for the Social Sciences) software, version 13.0, to compare the three groups. To analyze the parametric variables (age, weight, pain score and consumption of anesthetics and analgesics) and the nonparametric variables (sex and side affected) the Kruskal-Wallis and Mann-Whitney tests were used, and the results were taken to be significant when P < 0.05.
RESULTS
During the surgical procedure, the mean consumption of inhalation anesthetic (isofluorane) in group A was 32.2 ml (ranging from 9 to 65 ml). In group B, it was 40 ml (ranging from 20 to 65 ml) and in group C, it was 43.6 ml (ranging from 25 to 80 ml) (Figure 2).
Figure 2.
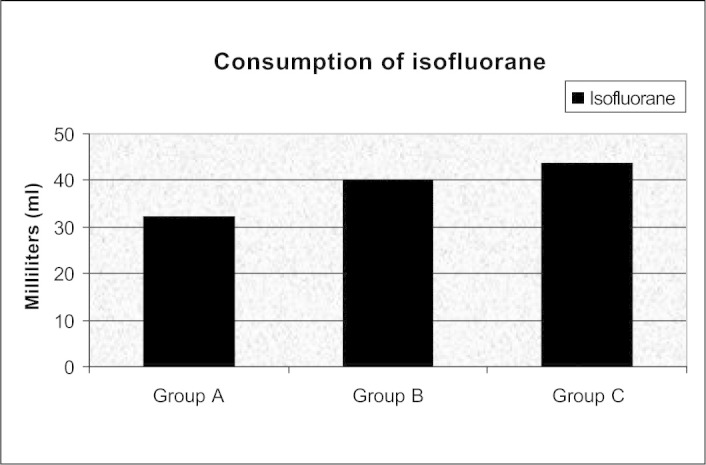
Mean consumption of inhalation anesthetics in milliliters in groups A, B and C
Before the operation, the mean pain intensity in group A was 7.6 (range: 5-10). During the immediate postoperative period, the mean pain intensity reported was 6.2 (range: 0-10). At the eight-hour postoperative evaluation, the reported mean was 5.6 (range: 0-10). After 16 hours, the patients reported a mean pain intensity of 4.5 (range: 0-8), and after 24 hours, the mean was 3.8 (range: 0-9). Finally, 48 hours after the operation, the reported mean pain intensity was 3.0 (range: 0-8).
In group B, the mean preoperative pain intensity was 6.6 (range: 5-9). During the immediate postoperative period, the reported mean pain intensity was 5.8 (range: 0-10), and at the eight-hour postoperative evaluation, the reported mean was 5.5 (range: 0-10). At the 16-hour postoperative evaluation, the patients reported a mean pain intensity of 5.8 (range: 2-10) and after 24 hours, the mean was 5.1 (range: 2-8). Finally, 48 hours after the operation, the reported mean pain intensity was 3.5 (range: 0-5) (Table 1).
Table 1.
Mean pain score according to the visual pain scale (VAS) in each group
| Observation time | Group A | Group B | Group C |
|---|---|---|---|
| Pre-op | 7.67 | 6.6 | 7.13 |
| Immediate post-op | 6.27 | 5.87 | 6.07 |
| 8H post-op | 5.67 | 5.53 | 5.4 |
| 16H post-op | 4.53 | 5.8 | 4.67 |
| 24H post-op | 3.8 | 5.13 | 4.33 |
| 48H post-op | 3 | 3.53 | 2.33 |
Legend: Pre-op - preoperative period, Post-op - postoperative period, H - Hours
Source: Hospital Medical Archives Service
In group C, the mean preoperative pain intensity was 7.1 (range: 0-10). During the immediate postoperative period, the reported main pain intensity was 6.0 (range: 0-10), and at the eight-hour postoperative evaluation, the reported mean was 5.4 (range: 0-10). At the 16-hour postoperative evaluation, the patients reported a mean pain intensity of 4.6 (range: 0-7) and after 24 hours, the mean was 4.3 (range: 0-10). Finally, 48 hours after the operation, the reported mean pain intensity was 2.5 (range: 0-6).
In the analysis on drug consumption in group A, the consumption was 5.4 ampoules of analgesics, 2.7 ampoules of anti-inflammatory agents and 0.8 ampoules of opioids. In group B, the consumption was 3.1 ampoules of analgesics, 1.05 ampoules of anti-inflammatory agents and 1.2 ampoules of opioids. In group C, the consumption was 4.2 ampoules of analgesics, 2.2 ampoules of anti-inflammatory agents and one ampoule of morphine (Figure 3).
Figure 3.
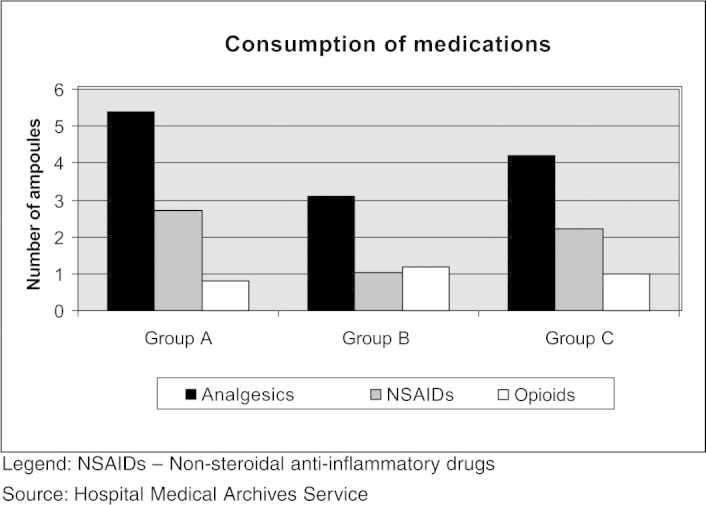
Mean number of ampoules of analgesics, anti-inflammatory agents and opioids consumed in each group after the operation
According to the statistical analysis, no statistically significant differences (p > 0.05) were found in relation to the patient sample (age, weight, sex and side affected), in comparisons between the three groups. The consumption of inhalation anesthetic during the surgery did not show any statistically significant difference between the three groups, according to the Kruskal-Wallis test (P = 0.216) (Figure 2), although on average there was 7.8 ml less consumption in group A than in group B, and 11.4 ml less than in group C.
With regard to the pain evaluation, the three groups showed similar analgesic efficacy during the postoperative period. There were no statistical differences according to the Kruskal-Wallis test at any time of asking about the pain intensity: preoperative period, P = 0.140; immediate postoperative period, P = 0.872; eight hours after the operation, P = 0.969; 16 hours after the operation, P = 0.383; 24 hours after the operation, P = 0.203; and 48 hours after the operation, P = 0.260 (Table 1).
In relation to analgesic and anti-inflammatory drug consumption, according to the Kruskal-Wallis test, there was also no statistically significant difference between the three groups (analgesics: P = 0.073; opioids: P = 0.88; and anti-inflammatory agents: P = 0.880) (Figure 3), thus showing that the efficacy of the different types of anesthesia used was similar.
DISCUSSION
General anesthesia in combination with interscalene block is widely used as an anesthetic method for shoulder surgery, including arthroscopic procedures4, 10. However, in Brazil and many developing countries, only certain private hospitals and a minority of public hospitals have electrical nerve stimulating devices for performing anesthetic block. The number of complications may increase when this technique is performed without using a stimulator, as reported by Weber and Jain(5), who found intercurrences such as episodes of cardiovascular collapse, severe respiratory depression, neurological abnormalities persisting for up to six weeks and persistent postoperative pain(11).
Laurila et al(12) compared interscalene block with infiltration of 15 ml of ropivacaine (5 mg/ml) into the subacromial space, immediately after introducing the arthroscope into the shoulder. They reported that this method did not reduce the postoperative pain or the consumption of oxycodone, compared with interscalene block.
Harvey et al(6) conducted a double-blind study to evaluate analgesia after arthroscopic acromioplasty. They compared continuous infusion of 0.2% ropivacaine into the subacromial space with infusion of 0.9% saline solution, which was used as a control group. From the visual pain scale (VAS), they noted that the group that received ropivacaine reported 34% less postoperative pain (46% on the first day and 22% on the second), with a statistically significant difference.
In another study, Muittari et al(13) found that the analgesia was better among patients who, after open acromioplasty procedures under general anesthetic, received 10 ml of 0.5% bupivacaine in the subacromial space, compared with patients who received 10 ml of oxycodone in the subacromial space and 5 mg intramuscularly.
Almeida et al(14) analyzed three groups of patients who underwent arthroscopic repair of the rotator cuff under general anesthesia. One of the groups underwent interscalene block, the second group received interscalene block combined with 150 mg of clonidine and the third group received infiltration at the ports with 10 ml of ropivacaine and 20 ml in the subacromial space after the surgery, after continuous administration of 0.2% ropivacaine. A pain intensity evaluation using a VAS 24 hours after the operation showed that the third group presented greater analgesic efficacy than the other two groups (p < 0.001). However, the interscalene block was performed without an electrical stimulator.
In a randomized double-blind study, Singelyn et al(15) compared the efficacy of intra-articular anesthesia with suprascapular nerve block and with interscalene block with an electrical stimulator, to perform arthroscopic acromioplasty on 120 patients. The authors found that the suprascapular nerve block and interscalene block groups presented less postoperative pain than shown by the intra-articular anesthesia group, although there was no statistical difference. They also found that the suprascapular nerve block group had the lowest morphine consumption and fewest adverse effects. They concluded that interscalene block was the most effective technique for performing arthroscopic acromioplasty and that when interscalene block was contraindicated, suprascapular nerve block was an efficient alternative.
In comparing our results with the study by Laurila et al(12), we saw that the latter also did not note any difference in analgesia between interscalene block and infiltration of bupivacaine into the subacromial space. However, they did not perform suprascapular nerve block. On the other hand, Almeida et al(l4) found that there was greater analgesic efficacy with infiltration of anesthetic into the subacromial space, thus differing from our results. The latter also did not perform suprascapular nerve block, while, as in our study, interscalene block was performed without an electrical stimulator. In the study by Singelyn et al(15), like in our study, there was no statistical difference between the groups, i.e. similar to what we found in the literature.
In this preliminary study, we compared analgesic efficacy between the technique of interscalene block using 2 mg/kg of 0.5% ropivacaine and the technique of suprascapular nerve block using two thirds of 2 mg/ kg of 0.5% ropivacaine in combination with infusion of the remaining one third into the subacromial space, moments before the surgery, and also the same suprascapular nerve block technique applied immediately after the procedure. We observed that the three techniques used presented similar analgesic efficacy, given that there were no statistically significant differences between the groups in relation to medication consumption and pain evaluation, thus showing that in this small sample of 45 patients, suprascapular nerve block combined with infusion of anesthetic into the subacromial space was an effective technique.
One of the failings of our study may be the size of the patient sample in each group, given that we did not obtain statistically significant differences between the groups and we do not know whether we could have had different results with a bigger sample. However, we now have important data that may assist in calculating the sample size needed for a study with greater statistical power, which will certainly involve a greater number of patients in each group. Moreover, we believe that this study might demonstrate, for hospitals in which a stimulator is not yet available, that suprascapular nerve block may be a good option, since it may reduce the chances of complications while presenting postoperative analgesic efficacy similar to that of interscalene block.
On the other hand, since we did not use an electrical stimulator, the failure rate for nerve block may have been higher, with greater mean consumption of anesthetic during the surgery and analgesic after the operation.
CONCLUSION
We observed similar efficacy between suprascapular nerve block combined with infusion of anesthetic into the subacromial space and interscalene block of the brachial plexus.
Footnotes
Work performed in the Discipline of Locomotor Apparatus Diseases, ABC School of Medicine, and in Mario Covas State Hospital.
REFERENCES
- 1.Boss AP, Maurer T, Seiler S, Aeschbach A, Hintermann B, Strebel S. Continuous subacromial infusion for postoperative analgesia after open acromioplasty and rotator cuff repair: preliminary results. J Shoulder Elbow Surg. 2004;13(6):630–634. doi: 10.1016/j.jse.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 2.Barber FA. Suprascapular nerve block for shoulder arthroscopy. Arthroscopy. 2005;21(8):e1–e4. doi: 10.1016/j.arthro.2005.05.033. [DOI] [PubMed] [Google Scholar]
- 3.Scoggin JF, III, Mayfield G, Awaya DJ, Pi M, Prentiss J, Takahashi J. Subacromial and intra-articular morphine versus bupivacaine after shoulder arthroscopy. Arthroscopy. 2002;18(5):464–468. doi: 10.1053/jars.2002.29895. [DOI] [PubMed] [Google Scholar]
- 4.Karkabi S, Besser M, Zinman C. Arthroscopic subacromial decompression performed under local anesthesia. Arthroscopy. 2005;21(11):1404:e1–11404e2. doi: 10.1016/j.arthro.2005.08.029. [DOI] [PubMed] [Google Scholar]
- 5.Weber SC, Jain R. Scalene regional anesthesia for shoulder surgery in a community setting: an assessment of risk. J Bone Joint Surg Am. 2002;84(5):775–779. doi: 10.2106/00004623-200205000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Harvey GP, Chelly JE, AlSamsam T, Coupe K. Patient-controlled ropivacaine analgesia after arthroscopic subacromial decompression. Arthroscopy. 2004;20(5):451–455. doi: 10.1016/j.arthro.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 7.Arciero RA, Taylor DC, Harrison SA, Snyder RJ, Leahy KE, Uhorchak JM. Interscalene anesthesia for shoulder arthroscopy in a community-sized military hospital. Arthroscopy. 1996;12(6):715–719. doi: 10.1016/s0749-8063(96)90176-0. [DOI] [PubMed] [Google Scholar]
- 8.Savoie FH, Field LD, Jenkins N, Mallon WJ, Phelps RA., 2nd The pain control infusion pump for postoperative pain control in shoulder surgery. Arthroscopy. 2000;16(4):339–342. doi: 10.1016/s0749-8063(00)90076-8. [DOI] [PubMed] [Google Scholar]
- 9.Jensen MK, Karoly P. Self-report scales and procedures for accessing pain in adults. In: Turk DC, Melzack R, editors. Handbook of pain assessment. Guilford Press; New York: 1992. pp. 135–151. [Google Scholar]
- 10.Horn EP, Schroeder F, Wilhelm S, Wappler F, Sessler DI, Uebe B. Wound infiltration and drain lavage with ropivacaine after major shoulder surgery. Anesth Analg. 1999;89(6):1461–1466. doi: 10.1097/00000539-199912000-00027. [DOI] [PubMed] [Google Scholar]
- 11.Mallon WJ, Thomas CW. Patient-controlled lidocaine analgesia for acromioplasty surgery. J Shoulder Elbow Surg. 2000;9(2):85–88. [PubMed] [Google Scholar]
- 12.Laurila PA, Löppönen A, Kanga-Saarela T, Flinkkilä T, Salomäki TE. Interscalene brachial plexus block is superior to subacromial bursa block after arthroscopic shoulder surgery. Acta Anaesthesiol Scand. 2002;46(8):1031–1036. doi: 10.1034/j.1399-6576.2002.460818.x. [DOI] [PubMed] [Google Scholar]
- 13.Muittari PA, Nelimarkka O, Seppälä T, Kanto JH, Kirvelä OA. Comparison of the analgesic effects of intrabursal oxycodone and bupivacaine after acromiplasty. J Clin Anesth. 1999;11(1):11–16. doi: 10.1016/s0952-8180(98)00122-6. [DOI] [PubMed] [Google Scholar]
- 14.Almeida A, Roveda G, Valin MR, Valin MCS, Almeida NC, Agostini AP. Analgesia para a sutura artroscópica do manguito rotador: estudo comparativo entre o bloqueio interescalênico do plexo braquial e o bloqueio da bursa subacromial contínuo. Rev Bras Ortop. 2007;42(10):324–332. [Google Scholar]
- 15.Singelyn FJ, Lhotel L, Fabre B. Pain relief after arthroscopic shoulder surgery: a comparison of intra-articular analgesia, suprascapular nerve block, and interscalene brachial plexus block. Anesth Analg. 2004;99(2):589–592. doi: 10.1213/01.ANE.0000125112.83117.49. [DOI] [PubMed] [Google Scholar]


