Abstract
Diaphyseal fractures of the femur and tibia in adults are mostly treated surgically, usually by means of intramedullary locked-nail osteosynthesis. Some comminuted and/or highly deviated shaft fractures may present a veritable technical challenge. Fracture (or orthopedic) tables, which enable vertical, horizontal and rotational instrumental stabilization of the limb, greatly facilitate reduction and implant placement maneuvers and are widely used by orthopedic surgeons. Humeral shaft fractures are mostly treated nonsurgically. However, some cases with indications that are well defined in the literature require surgical treatment. They can be fixed by means of plates or intramedullary nails, using anterograde or retrograde routes. In the humerus, fracture reduction and limb stabilization maneuvers for implantation of intramedullary nails are done manually, usually by two assistants. Because muscle fatigue may occur, this option may be less efficient. The aim of this paper is to present an external upper-limb traction device for use in anterograde intramedullary locked-nail osteosynthesis of humeral shaft fractures that enables vertical, horizontal and rotational stabilization of the upper limb, in a manner similar to the device used for the lower limbs. The device is portable, of simple construction, and can be installed on any operating table equipped with side rails. It was used for surgical treatment of 29 humeral shaft fractures using an anterograde locked intramedullary nail. Our experience was extremely positive. We did not have any complications relating to its use and we believe that it notably facilitated the surgical procedures.
Keywords: Humeral fractures/surgery, Diaphysis, Fracture fixation, intramedullary
METHOD
The device was used in surgically treating 29 humeral shaft fractures between April 2005 and June 2009.
The indications for surgical treatment were pathological fractures (n = 6); fractures that did not fulfill acceptable criteria for displacement and shortening after attempts to perform closed reduction (n = 5); fractures in obese patients and/or uncooperative patients and/or individuals incapable of tolerating functional treatment using a Sarmiento brace (n = 8); fractures in multiple trauma victims (n = 7); and cases of delayed consolidation (n = 3).
The device consists of three main parts, made of stainless steel, and it can be sterilized in an autoclave. There is a cushioned support for supporting and fixing the patient's head; a small radiotransparent table for supporting the arm; and the traction device per se (Figures 1a, 1b and 1c).
Figure 1A.

View of the device, consisting of three main parts, attached to the side rail of a standard surgical table: a headrest for supporting and fixing the head, a radiotransparent table and the traction device per se.
Figure 1B.

Proximal view of a patient positioned for the procedure.
Figure 1C.

Detail of the traction device, adapted to the distal side rail of the surgical table
TECHNIQUE
The patient is positioned in dorsal decubitus on the surgical table for administration of anesthesia. The cushioned support is adapted to the proximal extremity of the surgical table such that the patient can be placed fully laterally to it, so as to leave free all of the scapular belt, thereby facilitating the positioning of the image intensifier, which can be placed parallel, perpendicularly or obliquely to the surgical table. The headboard is elevated at between 30° and 40° and the head is fixed to the support, while maintaining alignment with the trunk, in order to avoid straining the neurovascular structures. Optionally, the patient can be positioned in strict dorsal decubitus. The patient's arm is place on the small radiotransparent table, which can be regulated for height and inclination and is adapted to the intermediate side rail of the surgical table (Figure 2). The traction device consists of a support of inverted (“reclining”) L shape, which is attached to the distal side rail of the table. This can take a piece that slides over its horizontal component and can be locked at any point on it. This piece, in turn, has an orifice through which a cylindrical rod can slide longitudinally, which can also be locked at any point. This rod connects to a stirrup-shaped device to which the patient's hand is attached by means of sterile bandaging. Thus, the arm with the elbow extended can be put under traction longitudinally and/or rotated around its own axis and locked in the desired position (Figure 3). Adduction and abduction movements of the arm take place by means of sliding the piece that grips the cylindrical rod, over the horizontal component of the inverted L-shaped support. Short flexion and extension movements are obtained by sliding the L-shaped support upwards and downwards (respectively towards the ceiling and floor of the surgical room), in relation to the distal side rail of the surgical table, which also has a locking mechanism.
Figure 2.

Lateral view of a patient positioned for the procedure
Figure 3.

If it is necessary to open up the fracture focus, the table can be used as a surgical table
Access to the subacromial space in order to introduce the guidewire is obtained with the arm maintained under traction and adduction, next to the chest. The magnitude of the longitudinal traction is regulated manually by the surgeon, in a manner similar to what is performed on lower limbs on a fracture table. This maneuver places the greater tubercle in a position that is lateral, distal and slightly anterior to the anterolateral acromion, thereby facilitating direct and radioscopic viewing (Figure 4). With the wide opening of subacromial space obtained, the guidewire, burrs and implant can easily be introduced in a non-traumatic manner, in line with the medullary canal of the humerus (Figures 5a, 5b and 5c).
Figure 4.

Radioscopic view of the subacromial space. On the left, opening obtained using the traction device
Figure 5A.
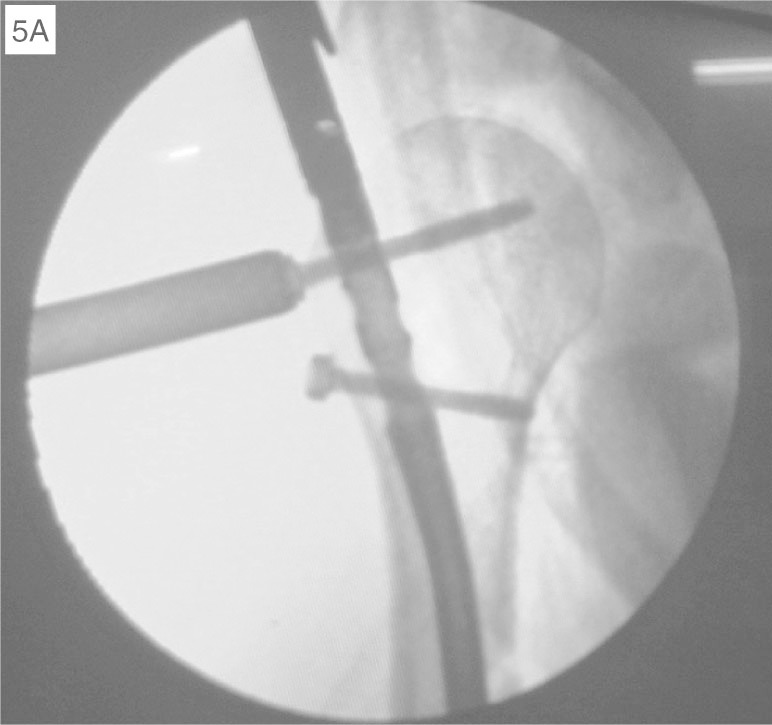
Radioscopic view of placement of proximal locking screws.
Figure 5B.

View of the construction of the entry orifice in the humeral head, after opening up the supraspinatus muscle.
Figure 5C.

View of supraspinatus, anatomically repaired at the end of the procedure
If the instrumental traction and manipulation of the main proximal and distal fragments is not enough to obtain sufficient alignment for the guidewire to be able to reach the medullary canal of the main distal fragment, the arm can be taken out of the device and manipulated over all simple and combined ranges of motion of the shoulder and elbow and/or be “hyperangled” at the level of the fracture focus. The arm can then be put back under traction again during the operation without difficulty (Figure 6).
Figure 6.

Demonstration of the ease of perioperatively removing the traction device, using a sterile technique
In this way, the surgeon has full control over positioning the arm and can easily adjust it throughout the procedure.
The tractioned arm is kept supported on the radiotransparent table in order to stabilize it in the horizontal plane (lateromedially) and vertical plane (superoinferiorly), respectively, thereby facilitating placement of proximal and distal locking screws, either using rigid guides or using a freehand technique (Figures 7a and 7b). If it is necessary to open up the fracture focus, the traction can be relaxed and the table can be used as a surgical table (Figure 8).
Figure 7A.

Perioperative view. The image intensifier can be placed parallel, perpendicularly or obliquely to the fracture table.
Figure 7B.

Perioperative view demonstrating the milling procedure in the medullary canal
Figure 8.

Exploration of the radial nerve. The traction is relaxed and the radiotransparent table is used as a surgical table
COMMENTS
Humeral shaft fractures represent 1% to 3% of all fractures, and most of them can be successfully treated non-surgically1, 2. Surgical treatment can be performed by means of open reduction and internal fixation using a plate, or by means of closed reduction and intramedullary locked-nail fixation. It is indicated in specific situations: fractures presenting unacceptable displacement and/or shortening following closed reduction; fractures in very obese patients, uncooperative patients or individuals who are intolerant to functional treatment (Figures 9a, 9b, 9c and 9d); most pathological fractures; multiple trauma patients; exposed, segmental or bilateral fractures; floating elbow; or associations with vascular lesions that require surgical repair13, 5.
Figures 9A, B, C and D.
Segmental comminuted fracture of the humerus in a morbidly obese patient, fixed using a Seidel nail
Comminuted and/or greatly displaced diaphyseal fractures of the long bones of the upper and lower limbs may present veritable technical challenges for surgeons. Longitudinal traction of the limb facilitates alignment and reduction of the fragments of the fracture(4).
In cases of open reduction and internal fixation using plates and screws, on long bones of the upper and lower limbs, traction can be achieved when necessary by means of temporary perioperative external fixators(4).
In cases of closed reduction and internal fixation using intramedullary nails, in diaphyseal fractures of the femur and tibia, traction is traditionally obtained on a fracture table, which is widely used by orthopedic surgeons. In intramedullary osteosynthesis of humeral shaft fractures, traction is normally achieved manually with the aid of one or two assistants(5). Because muscle fatigue may occur, this method may be less efficient.
In cases of intramedullary fixation by means of an anterograde route, introduction of the guidewire, burrs and, finally, the nail must be done in a precise manner through divulsion of the supraspinatus muscle in the area adjacent to its insertion into the greater tubercle. It is very important to be able to adequately view the subacromial space. In this manner, the implant can be introduced into the correct position, thereby minimizing the trauma to the muscle and allowing its repair at the end of the procedure, as well as avoiding fracturing the greater tubercle, which could be catastrophic for shoulder functioning1, 3, 5, 13.
Passage of the guidewire for milling the medullary canal and introduction of the nail are facilitated by aligning the fracture through the longitudinal traction on the humerus. Manipulation and, possibly, “hyperangulation” of the fracture focus are sometimes necessary, in order to allow the guidewire to reach the medullary canal of the main distal fragment. Rotational displacement of the fracture, if present, should be corrected after passing the guidewire through and before milling the medullary canal.
The device described here enables excellent exposure of the subacromial space, which helps in introducing the intramedullary nail in a precise and non-traumatic manner.
The arm can be kept under traction and locked at any degree of rotation in a stable manner, and can also be taken out from the traction and manipulated as often as necessary.
Stable positioning of the arm in the vertical and horizontal planes facilitates placement of the proximal and distal locking screws of the intramedullary nail, which can be done by means of rigid guides or using a freehand technique. Opening up the fracture focus, if necessary (for example, when it is impossible to pass the guidewire through using the closed technique, as may be the case in situations of delayed consolidation, or for exploration of the radial nerve), may be done by means of relaxing the traction with the arm supported on the radiotransparent table.
Manual axial compression of the focus of short transverse or oblique fractures may be achieved by taking the arm out from the device after placement of the proximal locking screws and before placement of the distal screws.
The device functions as a fracture table similar to those used for the lower limbs. It enables intermittent or continuous traction of the arm and helps in reducing and fixing humeral shaft fractures using an anterograde intramedullary nail. The image intensifier can easily be positioned parallel, perpendicularly or obliquely to the fracture table. When traction is unnecessary, the device functions as an arm holder, thereby facilitating the surgeon's work.
Application of this traction device to cases of anterograde intramedullary locked-nail fixation of humeral shaft fractures, which was derived from our experience of its use in arthroscopic and open surgery on the shoulder in a semi-seated position (deckchair position) (14), was extremely useful and enormously facilitated the reduction and fixation of fractures. We did not have any complications relating to its use, and we are using it routinely in cases of anterograde intramedullary locked-nail osteosynthesis of humeral shaft fractures.
Footnotes
Work performed at Hospital Madre Teresa, Belo Horizonte, Minas Gerais.
We declare that thers is no confilct of interests in this article
REFERENCES
- 1.Wolf JM, Athwal GS, Shin AY, Dennison DG. Acute trauma to the upper extremity: what to do and when to do it. J Bone Joint Surg Am. 2009;91(5):1240–1252. [PubMed] [Google Scholar]
- 2.Anglen JO, Archdeacon MT, Cannada LK, Herscovici D., Jr Avoiding complications in the treatment of humeral fractures. J Bone Joint Surg Am. 2008;90(7):1580–1589. [PubMed] [Google Scholar]
- 3.Chapman JR, Henley MB, Agel J, Benca PJ. Randomized prospective study of humeral shaft fracture fixation: intramedullary nails versus plates. J Orthop Trauma. 2000;14(3):162–166. doi: 10.1097/00005131-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Boykin RE, Baskies MA, Harrod CC, Jupiter JB. Intraoperative distraction in the upper extremity. Tech Hand Up Extrem Surg. 2009;13(2):75–81. doi: 10.1097/BTH.0b013e31818f0730. [DOI] [PubMed] [Google Scholar]
- 5.Lin J, Hou SM. Locked nailing of severely comminuted or segmental humeral fractures. Clin Orthop Relat Res. 2003;(406):406–407. doi: 10.1097/01.blo.0000038052.29678.ec. [DOI] [PubMed] [Google Scholar]
- 6.Gaultier O, Rebai L, Dunaud JL, Moughabghab M, Benaissa M. Treatment of humeral shaft fractures with the seidel nail. A study of 23 cases with rotator cuff evaluation J Bone Joint Surg Br. 2000;82(Suppl 2):118. [Google Scholar]
- 7.Johnson EC, Strauss E. Recent advances in the treatment of gunshot fractures of the humeral shaft. Clin Orthop Relat Res. 2003;(408):408–432. doi: 10.1097/00003086-200303000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Blum J, Janzing H, Gahr R, Langendorff HS, Rommens PM. Clinical performance of a new medullary humeral nail: antegrade versus retrograde insertion. J Orthop Trauma. 2001;15(5):342–349. doi: 10.1097/00005131-200106000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Schoots IG, Simons MP, Nork SE, Chapman JR, Henley MB. Antegrade locked nailing of open humeral shaft fractures. Orthopedics. 2007;30(1):49–54. doi: 10.3928/01477447-20070101-02. [DOI] [PubMed] [Google Scholar]
- 10.Cox MA, Dolan M, Synnott K, McElwain JP. Closed interlocking nailing of humeral shaft fractures with the Russell-Taylor nail. J Orthop Trauma. 2000;14(5):349–353. doi: 10.1097/00005131-200006000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Scheerlinck T, Handelberg F. Functional outcome after intramedullary nailing of humeral shaft fractures: comparison between retrograde Marchetti-Vicenzi and unreamed AO antegrade nailing. J Trauma. 2002;52(1):60–71. doi: 10.1097/00005373-200201000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Cheng HR, Lin J. Prospective randomized comparative study of antegrade and retrograde locked nailing for middle humeral shaft fracture. J Trauma. 2008;65(1):94–102. doi: 10.1097/TA.0b013e31812eed7f. [DOI] [PubMed] [Google Scholar]
- 13.Lin J, Shen PW, Hou SM. Complications of locked nailing in humeral shaft fractures. J Trauma. 2003;54(5):943–949. doi: 10.1097/01.TA.0000032252.57947.47. [DOI] [PubMed] [Google Scholar]
- 14.Correa MC, Gongalves LB, Andrade RP, Carvalho LH., Jr Beach chair position with instrumental distraction for arthroscopic and open shoulder surgeries. J Shoulder Elbow Surg. 2008;17(2):226–230. doi: 10.1016/j.jse.2007.08.009. [DOI] [PubMed] [Google Scholar]



