Abstract
The aim of this study was to evaluate the accuracy of simple radiography, ultrasound and magnetic resonance imaging (MRI) in diagnosing rotator cuff injuries, comparing their findings with open or arthroscopic surgery findings. Methods: Protocols of the Shoulder and Elbow Surgery Service for patients undergoing surgical treatment for rotator cuff injuries diagnosed by means of radiography, ultrasound and/or MRI between 2002 and 2007 were evaluated. Based on the data gathered, we analyzed the sensitivity, specificity, positive predictive value, negative predictive value and accuracy of these complementary examinations, compared with the findings during the surgical procedures. Results: This study included 147 patients with a mean age of 46.09 years. All the patients had undergone a radiography examination, 101 had undergone ultrasound examination and 72 had undergone MRI. We found sensitivity of 13.8%, specificity of 2.6% and accuracy of 30% with radiography; sensitivity of 57.6%, specificity of 29.6% and accuracy of 51.4% with ultrasound; and sensitivity of 86.6%, specificity of 22.2% and accuracy of 63.3% with MRI. Conclusion: Radiography was found to be a specific examination when the mirror sign was present. MRI and ultrasound were shown to be reliable methods with high accuracy for diagnosing rotator cuff injuries.
Keywords: Rotator Cuff, Ultrasonography, Magnetic Resonance Imaging, Diagnosis
INTRODUCTION
Rotator cuff injuries are a frequent cause of shoulder pain in individuals of all ages. This condition represents a spectrum of diseases, ranging from reversible acute tendinitis to massive lesions involving all of its components(1).
These injuries are diagnosed from the clinical history and physical examination, including by means of specific semiological maneuvers and infiltration of local anesthetic into the subacromial space in cases of diagnostic doubt (specific tests)(2).
Radiographic examinations help to define the cause of the impact and assess anatomical factors such as the shape and inclination of the acromion, presence of acromial spurs, presence of os acromiale and osteoarthrosis of the acromioclavicular joint. They show secondary alterations from the impact syndrome, such as subchondral cysts, sclerosis and irregularities of the greater tuberosity of the humerus. Radiographs also serve to identify tendinous and peritendinous calcifications(2).
The main noninvasive methods used in diagnosing rotator cuff injuries are ultrasound and magnetic resonance imaging (MRI)3, 4. Ultrasound is less expensive, but the sensitivity and specificity of its results vary because this is an “operator-dependent” examination4, 5, 6. MRI demonstrates the contrast between bone and soft tissues and presents degenerative lesions and tendon tears, along with other structural abnormalities that may be present7, 8.
There are few reports in the literature that compare the precision of ultrasound and MRI for diagnosing rotator cuff injuries, or for quantifying the lesion size. Both detecting and measuring the lesion may help in indicating whether open surgery or arthroscopy should be used as the therapeutic method, and in providing prognostic indications after these lesions have been repaired9, 10, 11.
The aim of this study was to evaluate the accuracy of simple radiography, ultrasound and MRI for diagnosing rotator cuff injuries of the shoulder, with comparisons with open or arthroscopic surgery as the standard.
METHODS
The protocols of the Shoulder and Elbow Surgery Service (Annex 1) of the Medical Residence Service over the years 2002 to 2007 were evaluated, by means of analysis on all the patients who underwent surgery to treat shoulder diseases. All the patients were operated by two orthopedic surgeons who are instructors within the Medical Residence Service.
ANNEX 1.
Protocol for the shoulder and elbow surgery service.
Adult patients of both sexes with a clinical and imaging diagnosis of rotator cuff injuries who were treated surgically after failed attempts at conservative treatment in accordance with the protocol of the service were included in this study.
The mean age of the patients evaluated was 46.09 years. The youngest patient was 20 years of age and the oldest was 69 years. Male patients were more prevalent: 83 males (56.5%) versus 64 women (43.5%).
All the patients underwent radiographic evaluation consisting of the true anteroposterior view, lateral scapular view and axillary view. The patients subsequently underwent ultrasound or MRI evaluations, or both.
All the ultrasound and MRI examinations were performed in one of two specialized clinical located in the same city as the institution where this study was conducted. The data were analyzed and reported on by radiologists who were specialists in the musculoskeletal field.
The radiographs were evaluated by the surgeons themselves. The diagnostic impressions from analysis on the radiographs were divided as follows: 1) without alterations; 2) sclerosis and subchondral cysts in the region of the greater tuberosity; and 3) “mirror sign”, with osteophyte formation in the anteroinferior region of the acromion.
In evaluating the ultrasound examinations, the following criteria for diagnosing rotator cuff tears were used: failure to see one or more of the rotator tendons; lack of focal view of one of the tendons; and well-defined defect or discontinuity in the tendon that reaches both faces of the tendon (articular and bursal). To characterize the lesion seen on ultrasound, three possibilities were taken into consideration: 1) normal (no lesion); 2) partial lesion; and 3) total lesion of the tendon(s) of the rotator cuff.
In evaluating the MRI data, the criteria used for analyzing the rotator cuff were the same as described in the protocol of Slatkin. This method defines four stages of rotator cuff lesions seen on MRI: 0 – tendon with normal signal and morphology; 1 – increased signal intensity without irregularity or discontinuity; 2 – increased signal with irregularity and tapering of the tendon; and 3 – complete solution loss of the tendon(12). Based on the descriptive reports created through using this protocol, we distributed the patients into groups according to the MRI results: 1) normal (no lesion); 2) partial lesion; and 3) complete lesion of the tendon.
The surgical treatment was performed using an arthroscopic or mixed approach in lateral decubitus. In such cases, the lesion was evaluated arthroscopically, but the lesion was repaired as an open procedure. During the surgery, the rotator cuff was evaluated with the aim of identifying tears and degenerative alterations.
During the operation, the patients were classified as: 1) without tears or lesions; 2) with partial tears and lesions on which debridement was performed; and 3) complete lesions. Lesion repair was implemented when possible.
On the basis of the data gathered, we analyzed the sensitivity, specificity, positive predictive value, negative predictive value and accuracy of the simple radiography, ultrasound and MRI for diagnosing any lesion of the rotator cuff. We also analyzed the capacity of these three complementary examinations, through the abovementioned indicators, to make specific diagnoses of partial and complete lesions of the rotator cuff and to make diagnoses of absence of tendon lesions.
RESULTS
Analyses were conducted on 454 protocols from patients who underwent shoulder surgery between 2002 and 2007. Of these, 187 patients had a diagnosis of rotator cuff injury with surgical treatment indicated. Forty of these patients were excluded from the study because of incomplete data and 147 patients were included.
All the patients studied had undergone radiographic examination. Thirteen of them presented a “mirror sign” image (8.85%), three presented normal images (2.05%) and 131 (89.1%) presented some type of radiographic abnormality, such as sclerosis of the greater tuberosity or subchondral cysts (Figure 1).
Figure 1.
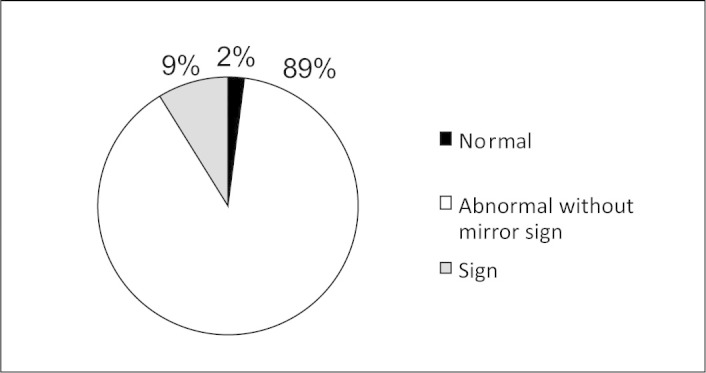
Patient distribution according to the presence of abnormalities on radiographs (approximate percentage values).
Among all the protocols analyzed, 101 presented data on ultrasound scans that had been carried out. Of these, there were 22 patients (21.8%) with normal examinations, 43 (42.6%) with partial lesions of the rotator cuff and 36 (35.6%) with diagnoses of complete/total cuff lesions (Figure 2).
Figure 2.
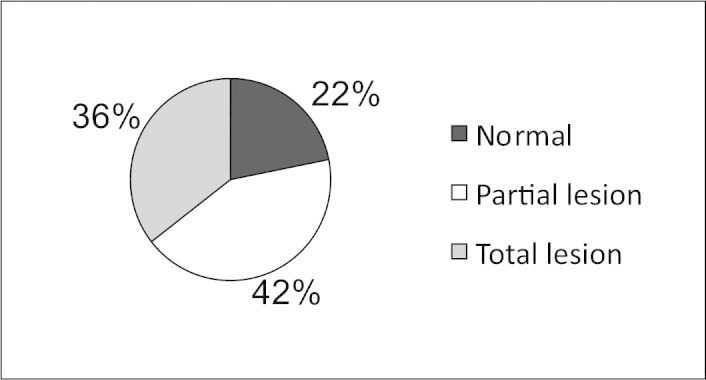
Patient distribution according to the presence of abnormalities on ultrasound (approximate percentage values).
Only 72 patients underwent MRI. Of these, 34 (47.2%) were found to present a complete lesion of the rotator cuff, 31 had a partial lesion (43%) and seven (9.8%) had normal reports (Figure 3).
Figure 3.
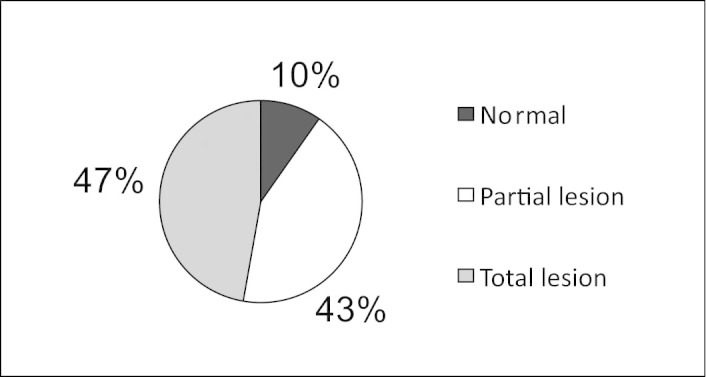
Patient distribution according to the presence of abnormalities on ultrasound (approximate percentage values).
During the 147 surgical procedures, we found that 38 patients did not have any rotator cuff injury (25.8%), 37 (25.2%) had a partial lesion and 72 (49%) had a total lesion.
In the statistical evaluation between radiography and the surgical procedure (gold standard), we found that out of the 131 patients who presented some abnormality on radiography, 34 (26%) had a partial cuff lesion and 60 (45.8%) had a complete lesion. Thus, for comparing partial lesions of the rotator cuff with images of abnormalities in the greater tuberosity, radiography presented sensitivity of 91.8% specificity of only 11.8%. Among the 13 patients with an anteroinferior image of osteophytes (“mirror sign”), all of them had some degree of tendon lesion: three (24%) with a partial lesion and 10 (76%) with a complete lesion. Thus, we found that when the radiograph presented a “mirror sign”, the sensitivity and specificity for complete lesion of the rotator cuff was 13.8% and 96%, respectively. Based on these data, we found sensitivity of 13.8%, specificity of 2.6% and accuracy of 30% when we compared the radiographic method with any type of rotator cuff lesion (Table 1).
Table 1.
Evaluation of findings suggestive of rotator cuff injuries seen on radiographs, in patients who underwent surgical treatment (gold standard), in absolute values.
 |
Source: data gathered between 2002 and 2007.
Comparison between ultrasound and the surgical procedure showed that out of the 43 patients with a partial lesion on ultrasound, 14 (32.5%) were found to have the same partial lesion during the surgery, and another 14 of them had a complete lesion. Thus, in analyzing the patients with partial lesions diagnosed by means of ultrasound and evaluated subsequently during the surgical procedure, we found sensitivity of 63.6% and specificity of 63.2%. However, among the 36 patients with reports of complete lesions seen on ultrasound, 30 (83.5%) were found to have a lesion with complete tearing of the rotator cuff during the surgical procedure, while four did not present any abnormalities and two had partial lesions. Analysis on the relationship between complete cuff tearing on ultrasound and proof of this in the procedure showed sensitivity of 57.6% and specificity of 87.7%. Based on these results, this method presented sensitivity of 57.6%, specificity of 29.6% and accuracy of 51.4% when we compared all of the data with the existence of any type of rotator cuff lesion (Table 2).
Table 2.
Evaluation of findings suggestive of rotator cuff injuries seen on ultrasound, in patients who underwent surgical treatment (gold standard), in absolute values.
 |
Source: data gathered between 2002 and 2007.
Analysis on the results from comparing MRI with surgery showed that out of the seven patients for whom the conclusion from the examination was that they did not have any lesions, we found four patients (57%) with undamaged rotator cuffs during the surgery, two (28.5%) with partial lesions and one (14.5%) with a complete lesion. Thus, we found sensitivity of 22.2% and specificity of 94.3% when the MRI report regarding cuff lesions was “normal”. Regarding the 30 patients whose MRI reports showed partial cuff lesion, there were 12 (38.7%) without a lesion seen during the operation, 15 (48.3%) with a confirmed partial lesion and three (13%) with a complete lesion. Based on these data, we found sensitivity of 65.2% and specificity of 68.7% for MRI with partial rotator cuff lesion. Analysis on the 34 patients with complete lesion presented on MRI showed that there were two patients (6%) with tendons without abnormalities, six (17.6%) with confirmed partial lesions and 26 (76.4%) with complete lesions. Therefore, the results obtained demonstrated sensitivity of 86.6% and specificity of 80.4% when the MRI diagnosis consisted of a complete cuff tear. Thus, analysis on these data revealed sensitivity of 86.6%, specificity of 22.2% and accuracy of 63.3% for this method compared with the gold standard, with regard to any degree of rotator cuff lesion or when the result from MRI is normal for this condition (Table 3).
Table 3.
Evaluation of findings suggestive of rotator cuff injuries seen on magnetic resonance imaging, in patients who underwent surgical treatment (gold standard), in absolute values.
 |
Source: Dados coletados de 2002-2007.
The results from the statistical analyses can be seen in the graph of Figure 4, with comparisons of sensitivity, specificity, accuracy and other indices with the three diagnostic methods (Figure 4).
Figure 4.
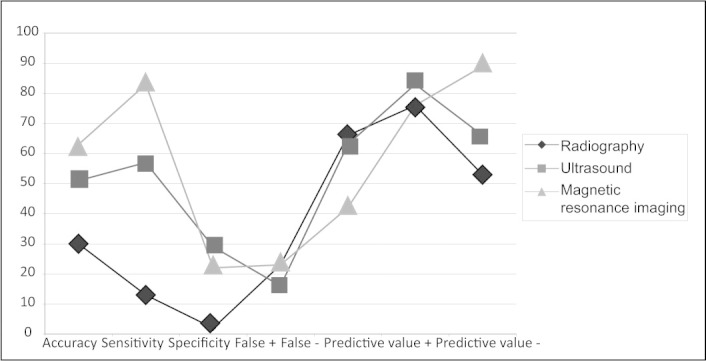
Bilateral TKA showing adequate alignment and complete extension.
DISCUSSION
Approximately 60% of all shoulder diseases are attributed to rotator cuff injuries. Arthroscopic studies have suggested that 10% of the cases of painful shoulder are due to lesions affecting the entire thickness, while the remaining 90% are due to partial lesions(13).
Currently, both ultrasound and magnetic resonance are methods used for diagnosing rotator cuff injuries, and there is no clearly preferable method3, 14. However, the improvements in transducers and the more accessible price of ultrasound have made this a good initial investigational method for patients with shoulder pain and suspected disease4, 15.
From reviewing the literature, it can be seen that there is great variation in the results from ultrasonography, with regard to identifying torn rotator cuff tendons, with reports of sensitivity greater than 90% in some studies, while the results from some other studies have been much less notable16, 17, 18, 19, 20. These differences have been due to changes in ultrasound devices, differences between the populations studied and differences in ultrasound operators' experience. In our study, we found that the general sensitivity was 57.6% and the general specificity was 29.6%. However, specifically for complete lesions, this method presented sensitivity of 57.6% and specificity of 87.7%; while for partial lesions, the sensitivity was 63.6% and the specificity was 63.2%. We are aware of the greater difficulty in diagnosing partial lesions, and of the sensitivity limitations of the method(21), but we believe that these results are in agreement with the literature that we consulted.
The risk in using a method with low sensitivity rates, as found through using ultrasound, is that surgical treatment may not be indicated because of false negatives(22).
In massive injuries to the rotator cuff, the tendons retract below the acromion and there is direct contact between the humeral head and the deltoid. However, when the subacromial bursa and peribursal region are very thick, this may be interpreted from ultrasound as an undamaged tendon, i.e. leading to a false negative13, 23, 24. Our positive predictive value was 83.3% and our negative predictive value was 66.1%, which were similar to other authors' data24, 25.
MRI is an examination of limited use when dealing with obese patients. In such cases, there are artifacts caused by mobility and by non-tolerance by claustrophobic patients, along with certain restrictions when there is a metallic implant. It has also been reported that the accuracy in diagnosing partial lesions is lower than for lesions affecting the complete thickness(26). In our study, we found sensitivity of 86.6% and specificity of 80.4% with regard only to patients with a completely torn rotator cuff, resulting in accuracy of 83.09%. Among patients diagnosed with a partial lesion, the sensitivity was 65.2% and the specificity was 68.7%, with accuracy of 67.5%. The literature presents sensitivity results ranging from 82% to 100% and specificity ranging from 79 to 100%, for complete tendon lesions7, 16, 19.
Martín-Hervás et al(22) found high sensitivity (100%) in diagnosing partial lesions using magnetic resonance, but with low specificity (29.8%), which resulted in few false negatives. However, when a lesion was present in an examination, this presence was uncertain and the false positive rate was high, with a positive predictive value of 19.5%. In our study, we found higher specificity rates for partial lesions, with a positive predictive value of 50%. The positive predictive value for performing MRI for any patient in this study, i.e. taking into consideration the presence or absence of any lesion, was 76.4%.
MRI was shown to be superior to the other examinations in assessing the quality of the rotator cuff tendons, since it demonstrated the degree of retraction and atrophy of the tendons.
Evaluations on patients with diagnoses of a completely torn rotator cuff produced similar results, with sensitivity of 86.6% from MRI versus 57.6% from ultrasound, while the specificity was 80.4% and 87.7%, respectively. Thus, it may be supposed that among the patients studied, in cases of completely torn rotator cuffs, MRI had a greater capacity to diagnose the condition, whereas ultrasound was better for ruling out cases that did not present a complete lesion. Comparison of the accuracy of the two methods in relation to completely torn rotator cuffs showed a value of 83.09% for MRI versus 67.3% for ultrasound. These data are similar to what is seen in reports in the literature(22).
Analysis on partial tears among our sample, with the same comparison between the methods, showed sensitivity of 63.6% for ultrasound versus 65.2% for MRI. For specificity, the values were 63.2% and 68.7%, respectively. These data showed a smaller difference between the two complementary examinations in favor of MRI, compared with the analysis on complete tears presented above.
In evaluating the accuracy of the two methods, we found that both ultrasound and MRI presented high accuracy, with results that were little more notable for one than for the other. Radiography is a method that presented less favorable results, and its use became important when the mirror sign was present. The latter situation presented 96% specificity for complete tearing. This indicates that when we found osteophytes in the anteroinferior region of the acromion, there was a high probability that the patient would present a lesion affecting the complete thickness of the rotator cuff. In this way, radiography has importance in investigating painful shoulders with suspected rotator cuff injuries.
CONCLUSION
MRI and ultrasound were shown to be reliable methods presenting high accuracy for diagnosing rotator cuff injuries.
Radiography was shown to be a specific examination when the mirror sign was presented. It is an easily accessible tool and remains recommended for diagnosing rotator cuff injuries.
Footnotes
Work performed at the Institute of Orthopedics and Traumatology (IOT), Joinville, SC.
Declaramos inexistência de conflito de interesses neste artigo
REFERENCES
- 1.Andrade RP, Corra Filho MR, Queiroz BC. Lesões do manguito rotador. Rev Bras Ortop. 2004;39:621–636. [Google Scholar]
- 2.Volpon JB, Erdmann K, Nisiyama CY, Monteiro CR. Ruptura do manguito rotador do ombro em pacientes com pinçamento crônico. Rev Bras Ortop. 1989;24(4):111–114. [Google Scholar]
- 3.Bachmann GF, Melzer C, Heinrichs CM, Möhring B, Rominger MB. Diagnosis of rotator cuff lesions: comparison of US and MRI on 38 joint specimens. Eur Radiol. 1997;7(2):192–197. doi: 10.1007/s003300050133. [DOI] [PubMed] [Google Scholar]
- 4.Read JW, Perko M. Shoulder ultrasound: diagnostic accuracy for impingement syndrome, rotator cuff tear, and biceps tendon pathology. J Shoulder Elbow Surg. 1998;7(3):264–271. doi: 10.1016/s1058-2746(98)90055-6. [DOI] [PubMed] [Google Scholar]
- 5.Paavolainen P, Ahovuo J. Ultrasonography and arthrography in the diagnosis of tears of the rotator cuff. J Bone Joint Surg Am. 1994;76(3):335–340. doi: 10.2106/00004623-199403000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Teefey SA, Middleton WD, Yamaguchi K. Shoulder sonography. State of the art. Radiol Clin North Am. 1999;37(4):767–785. doi: 10.1016/s0033-8389(05)70128-7. [DOI] [PubMed] [Google Scholar]
- 7.Iannotti JP, Zlatkin MB, Esterhai JL, Kressel HY, Dalinka MK, Spindler KP. Magnetic resonance imaging of the shoulder. Sensitivity, specificity, and predictive value. J Bone Joint Surg Am. 1991;73(1):17–29. [PubMed] [Google Scholar]
- 8.Uri DS. MR imaging of shoulder impingement and rotator cuff disease. Radiol Clin North Am. 1997;35(1):77–96. [PubMed] [Google Scholar]
- 9.Yamaguchi K. Mini-open rotator cuff repair: an updated perspective. Instr Course Lect. 2001;50:53–61. [PubMed] [Google Scholar]
- 10.Yamaguchi K, Levine WN, Marra G, Galatz LM, Klepps S, Flatow EL. Transitioning to arthroscopic rotator cuff repair: the pros and cons. Instr Course Lect. 2003;52:81–92. [PubMed] [Google Scholar]
- 11.Warner JJ, Goitz RJ, Irrgang JJ, Groff YJ. Arthroscopic-assisted rotator cuff repair: patient selection and treatment outcome. J Shoulder Elbow Surg. 1997;6(5):463–472. doi: 10.1016/s1058-2746(97)70054-5. [DOI] [PubMed] [Google Scholar]
- 12.Zlatkin MB, Iannotti JP, Roberts MC, Esterhai JL, Dalinka MK, Kressel HY. Rotator cuff tears: diagnostic performance of MR imaging. Radiology. 1989;172(1):223–229. doi: 10.1148/radiology.172.1.2740508. [DOI] [PubMed] [Google Scholar]
- 13.Van Holsbeeck MT, Craig JG. Bouffard JA, Shirazi KK. Shoulder pain. Radiol Soc North Am. 1996:117–123. [Google Scholar]
- 14.Torstensen ET, Hollinshead RM. Comparison of magnetic resonance imaging and arthroscopy in the evaluation of shoulder pathology. J Shoulder Elbow Surg. 1999;8(1):42–45. doi: 10.1016/s1058-2746(99)90053-8. [DOI] [PubMed] [Google Scholar]
- 15.Erickson SJ. High-resolution imaging of the musculoskeletal system. Radiology. 1997;205(3):593–618. doi: 10.1148/radiology.205.3.9393511. [DOI] [PubMed] [Google Scholar]
- 16.Burk DL, Jr, Karasick D, Kurtz AB, Mitchell DG, Rifkin MD, Miller CL. Rotator cuff tears: prospective comparison of MR imaging with arthrography, sonography, and surgery. AJR Am J Roentgenol. 1989;153(1):87–92. doi: 10.2214/ajr.153.1.87. [DOI] [PubMed] [Google Scholar]
- 17.Crass JR, Craig EV, Thompson RC, Feinberg SB. Ultrasonography of the rotator cuff: surgical correlation. J Clin Ultrasound. 1984;12(8):487–491. doi: 10.1002/jcu.1870120806. [DOI] [PubMed] [Google Scholar]
- 18.Mack LA, Matsen FA, 3rd, Kilcoyne RF, Davies PK, Sickler ME. US evaluation of the rotator cuff. Radiology. 1985;157(1):205–209. doi: 10.1148/radiology.157.1.3898216. [DOI] [PubMed] [Google Scholar]
- 19.Nelson MC, Leather GP, Nirschl RP, Pettrone FA, Freedman MT. Evaluation of the painful shoulder. A prospective comparison of magnetic resonance imaging, computerized tomographic arthrography, ultrasonography, and operative findings. J Bone Joint Surg Am. 1991;73(5):707–716. [PubMed] [Google Scholar]
- 20.Middleton WD, Reinus WR, Totty WG, Melson CL, Murphy WA. Ultrasonographic evaluation of the rotator cuff and biceps tendon. J Bone Joint Surg Am. 1986;68(3):440–450. [PubMed] [Google Scholar]
- 21.Brenneke SL, Morgan CJ. Evaluation of ultrasonography as a diagnostic technique in the assessment of rotator cuff tendon tears. Am J Sports Med. 1992;20(3):287–289. doi: 10.1177/036354659202000309. [DOI] [PubMed] [Google Scholar]
- 22.Martín-Hervás C, Romero J, Navas-Acién A, Reboiras JJ, Munuera L. Ultrasonographic and magnetic resonance images of rotator cuff lesions compared with arthroscopy or open surgery findings. J Shoulder Elbow Surg. 2001;10(5):410–415. doi: 10.1067/mse.2001.116515. [DOI] [PubMed] [Google Scholar]
- 23.Middleton WD. Ultrasonography of the shoulder. Radiol Clin North Am. 1992;30(5):927–940. [PubMed] [Google Scholar]
- 24.Thain LF, Adler RS. Shoulder: rotator cuff and long head of biceps tendons. In: Chhem RK, Cardinal E, editors. Guidelines and gamuts in musculoskeletal ultrasound. Wiley-Liss; New York: 1999. pp. 39–72. [Google Scholar]
- 25.Swen WA, Jacobs JW, Algra PR, Manoliu RA, Rijkmans J, Willems WJ. Sonography and magnetic resonance imaging equivalent for the assessment of full-thickness rotator cuff tears. Arthritis Rheum. 1999;42(10):2231–2238. doi: 10.1002/1529-0131(199910)42:10<2231::AID-ANR27>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 26.Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res. 1997;(344):344–383. [PubMed] [Google Scholar]