Abstract
Objective: To evaluate the clinical and radiographic results from 30 cases of revision of total hip arthroplasty using a modular cementless distal fixation prosthesis: the ZMR® Hip System. Method: Between July 2005 and December 2008, 30 operations were performed, on 14 men and 14 women. Two male patients had bilateral surgery. The mean age was 59.2 years (29-81 years), with a mean follow-up of 24 months. The Paprosky classification was used for periprosthetic bone loss, and the Harris Hip Score (HHS) was used to evaluate clinical results. On radiographs, distal migration of the femoral stem was defined in accordance with Sporer. Proximal bone remodeling was classified using the Callaghan criteria. Results: The mean preoperative HHS was 39, and there was a significant increase to 93 points in the final evaluation, which indicated excellent clinical results. No femoral stem migration greater than 5 mm (Sporer) was observed on radiographs, thus suggesting that all the femoral prostheses presented osseointegration and remained stable from the time of the surgery until the final evaluation. The proximal femoral remodeling was either type B or type C in 29 hips, according to Callaghan. Seven patients had complications, but without interfering with osseointegration of the femoral components. Conclusion: Our results from revision of total hip arthroplasty using the ZMR® Hip System were extremely encouraging, and all the components became osseointegrated and remained fixed at the time of the final evaluation.
Keywords: Arthroplasty, hip; Hip prosthesis; Retrospective studies; Adult
INTRODUCTION
The large increases in the numbers of primary hip arthroplasty procedures performed over recent decades has also led to an increase in the importance of defining better techniques and implants for revision surgery2, 2.
The main challenges of femoral revision are the following: (1) excessive periprosthetic bone loss; (2) removal of the femoral component and the cement without causing iatrogenic bone loss; (3) achieving stable fixation for the new implant and maintaining this(3).
The first femoral revisions were performed as an “extension of the primary surgery”, in which long-stem cemented femoral components were used. However, the length of the femoral canal did not provide sufficient fixation for the implant, thus leading to mobility at the bone-cement interface and formation of debris, which then led to early loosening4, 5, 6, 7.
Cementless stems with proximal fixation present excellent results in primary arthroplasties, but their use is very limited in revisions because good metaphyseal bone stock is needed in order to achieve sufficient stabilization of the implant and consequent osseointegration. Since in most cases there is extensive proximal femoral bone loss and the remaining bone is weak and poorly vascularized, use of these implants in revision surgery presents unsatisfactory results8, 9, 10, 11.
The technique using an impacted bone graft and a cemented polished femoral component that was developed in Exeter (England), presents good results12, 13. However, it is difficult to reproduce it in different surgical services because of its complicated “learning curve” and because of the need for a large volume of homologous bone tissue, which is required for reconstruction of the femur.
With the aim of achieving initial stability of the implant, even in cases of extensive proximal femoral losses, cementless femoral components with distal fixation have been developed, with a variety of designs and materials. Milling of the diaphyseal bone and tight impaction of the prosthesis with the femoral cortical bone provides sufficient fixation until osseointegration of the implant occurs14, 15, 16, 17, 18, 19, 20, 21.
Modular cementless prostheses with distal fixation were introduced by Konstantin Sivash, a Russian orthopedist, in 1956. This implant underwent many modifications until reaching his most famous model: the S-ROM (Sivash-Range of Motion). The modular design of the implant allowed surgeons to adapt it to different metaphyseal/diaphyseal diameters, choose different stem lengths and modify the anteversion and offset angles3, 14, 22, 23, 24, 25, 26, 27, 28, 29.
The aim of this study was to evaluate the clinical and radiographic results from 30 cases of revision of total hip arthroplasty using the ZMR® (Zimmer Modular Revision) modular cementless distal fixation prosthesis.
METHODS
Between July 2005 and December 2008, 30 revision operations were performed on cases of total hip arthroplasty (THA) using the ZMR® modular cementless distal fixation prosthesis. These procedures were performed on 14 men and 14 women: two of the men underwent bilateral surgery. The mean age was 59.2 years (29-81 years). The mean duration of the follow-up was 24 months, and no cases were lost or excluded. The operations were performed at Hospital de Caridade and Hospital Governador Celso Ramos, in Florianópolis, SC, Brazil. All the operations were performed by the same surgeon (RPC).
The ZMR® Hip System consists of a conical modular cementless femoral prosthesis with distal fixation that is made of an alloy of titanium, aluminum and vanadium. The proximal component (body) has different possible lengths (75, 80, 90 and 100 mm) and diameters (AA, A, B, C, D, E and F), with a cervicodiaphyseal angle of 135°. The possibilities for the distal component (taper stem) are lengths of 135, 185 and 235 mm and diameters of 14 to 22 mm. For the offset, the choices are 36, 40 and 46 mm, and there are five possibilities for the femoral head (from −3.5 to 10 mm). In addition to the conical design of the implant, with an angle of 3.5° from proximal to distal, which promotes axial stability, there are sharp splines of 0.75 mm to ensure anchoring in the femoral canal and rotational stabilization. At the distal extremity of the stem, there is also anterior chamfering that is designed to adapt to the anterior curvature of the femur, thereby diminishing the impact on and possible perforation of the cortical bone, especially in relation to long stems (Figure 1).
Figure 1.
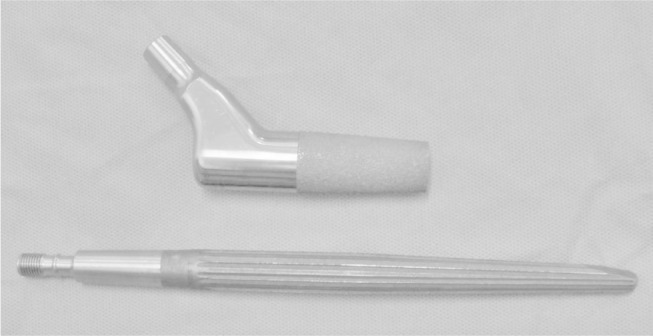
ZMR® modular cementless distal fixation prosthesis
The modular design of the implant provides surgeons with the choice of 12 different lengths (210 to 335 mm) and also different degrees of version of the proximal component, thereby facilitating correction of anatomical abnormalities of the femur or acetabular positioning, and increasing the stability of the implant, in which the connection is made in a Morse cone with a nut for additional locking.
The indications for femoral revision were aseptic loosening (26 cases), periprosthetic fracture (three cases) and septic loosening (one case). The classification of Valle and Paprosky(19) was used for the periprosthetic bone loss (Box 1). In only one case was the acetabular component not revised: this case did not present signs of loosening and the cementation technique was adequate. In another case, a polyethylene component was cemented to the metal cupola, which was found to be fixed. In the other 28 cases, the entire acetabular component was revised.
Box 1.
Periprosthetic bone loss (Paprosky classification)
| Paprosky | Patients |
|---|---|
| I | 0 |
| II | 7 |
| IIIA | 15 |
| IIIB | 5 |
| IV | 3 |
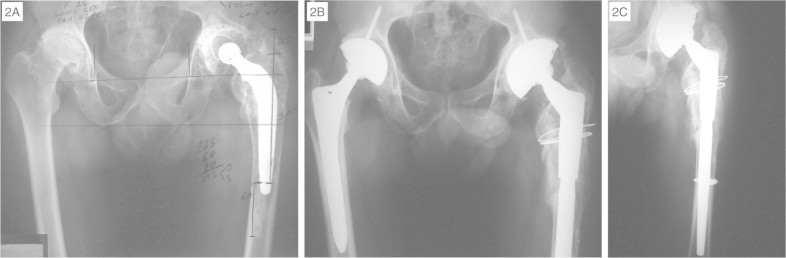
It was necessary to use a bone graft in 13 cases. In nine cases, homologous bone tissue supplied by the Musculoskeletal Tissue Bank of Curitiba, PR, was used. In another four cases, use of autologous tissue for reconstruction of bone losses was indicated: in three cases, this was taken from the iliac crest, and in one case from the contralateral femoral head, which was taken for primary THA within the same operation (Figures 2a, 2b and 2c).
Figure 2.
A) Patient GM, presenting arthrosis in the right hip secondary to rheumatoid arthritis and loosening of the left-hip prosthesis. B) The patient underwent right-side THA and revision of the left-side THA during the same operation, using the femoral head for an autologous bone graft. C) Control radiograph 15 months after the operation, showing proximal bone remodeling
All the patients underwent radiographic examinations for preoperative planning using templates supplied by the manufacturer. It was essential to define the length and width of the modular femoral component prior to the surgical procedure, in order to achieve initial stabilization of the prosthesis. Through this, osseointegration of the implant would be promoted. For impaction of the stem, 5 to 7 cm of diaphyseal bone would be needed.
OPERATIVE TECHNIQUE
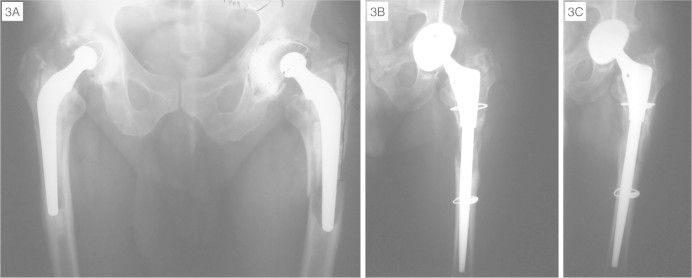
The surgical access chosen in all cases was posterolateral and it was combined with extended trochanteric osteotomy in 26 cases. After the implant, cement and periprosthetic fibrous tissue had been removed, the femoral canal was milled using specific tools, increasing the diameter millimeter by millimeter until reaching the predetermined size. The prosthesis test and reduction components were then used to check for discrepancies between the lower limbs and test the joint stability. After defining which components would be used but before performing stem impaction, a loop of steel wire was fashioned on the distal femur (Figures 3 a, 3b and 3c). This would serve as protection against possible femoral fracture upon insertion of the prosthesis, thereby avoiding displacement of fragments that might lead to instability and failure of the distal fixation. Through impaction of the definitive stem, reduction of the implant and joint stability tests, osteosynthesis on the femurs that underwent extended trochanteric osteotomy was achieved using one or two steel wires, positioning a suction drain and suturing of the wound.
Figure 3.
A) Patient RF, presenting a periprosthetic fracture in the left femur. B) Postoperative control with steel wire on the diaphysis to prevent femoral fracturing during the operation. C) Control radiograph two years after the operation, showing proximal bone remodeling without using a graft
During the postoperative period, physiotherapy was started on the first day, with ankle mobilization exercises and isometric exercises for the quadriceps. On the second postoperative day, the section drain was removed and the patient was encouraged to walk with partial offloading of weight by means of a walking frame or a pair of crutches. This continued for eight weeks and was followed by use of a contralateral crutch until the patient felt secure enough to walk without support. Administration of intravenous antibiotics was maintained until we had received the results from cultures on periprosthetic tissue that was removed during the operation, and the antibiotics were continued thereafter if necessary. In addition to early mobilization and use of elastic stockings for prevention of pulmonary thromboembolism, low molecular weight heparin was also prescribed. This started on the first postoperative day and was maintained for 30 days.
The patients were instructed to return for follow-ups three weeks, two months, four months, six months and twelve months after the surgery, and annually thereafter. They were evaluated using the Harris Hip Score(30) (HHS) before the operation and at all the postoperative follow-ups. On this scale, scores less than 70 are defined as poor results; between 70 and 79, as reasonable; between 80 and 89, as good; and greater than 90, as excellent. On radiographs, occurrences of distal migration of the femoral stem were defined as movements greater than 5 mm, in accordance with Sporer and Paprosky(21). The references for this were the distances from the center of the femoral head and from the small trochanter, measured on radiographs produced just after the surgery and repeated until the last evaluation. Proximal bone remodeling was evaluated quantitatively on anteroposterior and lateral radiographs during the outpatient follow-up, using the cortical diameter on the femoral diaphysis, 1 cm distally to the small trochanter. This was classified in accordance with Callaghan et al(31), with the following criteria: A – increased defect or no remodeling; B – small degree of remodeling; and C – significant bone remodeling. Our still modest number of operated cases was insufficient for statistical analysis, and only descriptive analysis could be performed.
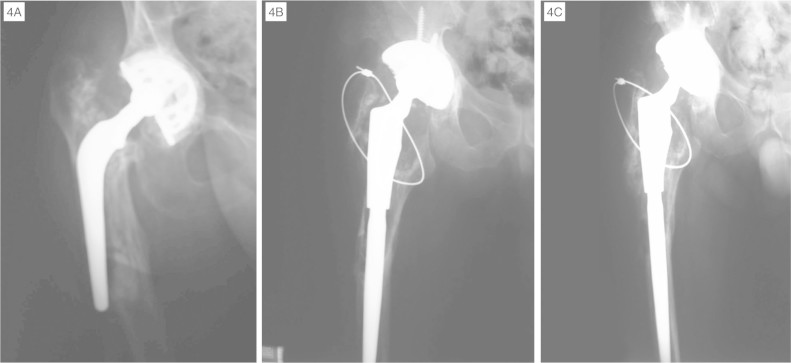
RESULTS
The mean preoperative HHS was 39, and this showed significant increases, reaching 93 points at the last evaluation, thus indicating that the clinical result was excellent. The radiographs were evaluated in accordance with the migration criteria described by Sporer and Paprosky(21) and, from this, no cases of femoral stem migration greater than 5 mm were observed. This suggests that all the femoral prostheses presented osseointegration and remained stable from the time of the operation until the last evaluation. The proximal bone remodeling (Figures 4a, 4b and 4c), which was evaluated on radiographs at the last outpatient consultation and compared with the first radiographs produced after the operation, was classified as type A, one case, type b, 14 cases, and type C, 15 cases, in accordance with Callaghan et al(31).
Figure 4.
A) Patient CM, presenting aseptic loosening and femoral stem with skewed positioning. B) Postoperative control radiograph showing extensive proximal bone loss, and only with fixation of the greater trochanter using a steel wire. C) Control radiograph at the last evaluation (two years after the operation), showing proximal bone remodeling with using a graft
Surgical complications occurred in seven cases (Box 2). The patient with deep vein thrombosis did not present any symptomatic respiratory complications, and this condition was treated with anticoagulants and elastic stockings for six, without development of sequelae.
Box 2.
Postoperative complications
| Complications | Patients |
|---|---|
| Deep vein thrombosis (DVT) | 1 |
| Failure of acetabular component fixation | 2 |
| Luxation | 1 |
| Superficial infection | 1 |
| Deep infection | 1 |
| Cerebral fat embolism | 1 |
The patients with early loosening of the acetabular component were reoperated. In the first case, the loosened reconstruction ring was removed and replaced with an acetabular reconstruction consisting of a homologous structural bone graft from a tissue bank and a polyethylene cemented acetabulum. In the second case, there was fracturing of the acetabular roof that had not been recognized during the surgery. Thus, the acetabular dome had remained unstable, thereby making osseointegration impossible. This case was also treated by means of replacement with homologous structural bone graft and a polyethylene cemented dome.
In the patient who suffered luxation, this occurred in the eighth week after the operation. This was reduced without open surgery and the patient was strongly advised about early postoperative care precautions that should be taken, in order to avoid recurrence.
The patient with superficial infection was treated with readmission to hospital and intravenous antibiotics. Remission of the infectious process was achieved, with clinical and laboratory improvement. The case of the patient who developed deep infection was much more difficult to handle. This patient presented a positive culture from the sample of periprosthetic tissue that had been collected during the operation, developed bacteremia and septic shock, was admitted to the intensive care unit (ICU) and underwent three surgical interventions to clean the joint. The patient evolved satisfactorily, with clinical and laboratory improvements and, so far, is continuing to use the implant without signs of loosening, despite extensive proximal femoral bone loss. Another serious postoperative complication occurred with the patient who developed cerebral fat embolism, who was also admitted to the ICU for support measures and remained in hospital for a long period. Despite presenting an excellent orthopedic result and being able to walk without support, this patient is continuing to take neurological medications for balance control and mood disorders even today, after three years of follow-up.
DISCUSSION
The development of modular implants for promoting correction of lower-limb discrepancies, greater implant stability and adaptation to proximal bone losses has increased the success rate of femoral revision procedures using cementless prostheses with distal fixation3, 14, 15, 23, 24, 25, 26, 27, 28, 29.
We did not find any published papers in Brazilian orthopedic journals on revision of total hip arthroplasty using modular cementless prostheses with distal fixation, and this encouraged us to publish our results and stimulate interest in this surgical procedure in Brazil.
The studies published in the foreign literature have presented good clinical and radiographic results. McCarthy and Lee(27) described results from THA revision using a modular distal fixation prosthesis and mean follow-up of 14 years, in which the aseptic loosening rate was 9%. All the cases that evolved with mechanical failure presented Paprosky IIIB and IV bone losses, and none of the patients with types II and IIIA bone losses evolved with loss of fixation. Among our sample of 30 operated cases, we have not yet had any cases of aseptic loosening: the mean duration of our follow-up is still short (two years) and, moreover, five of the cases were classified as Paprosky IIIB and three as type IV (Figures 5a and 5b), which led us to be more rigorous with these patients' follow-up. The other studies that we found are cited in Box 3.
Figure 5.
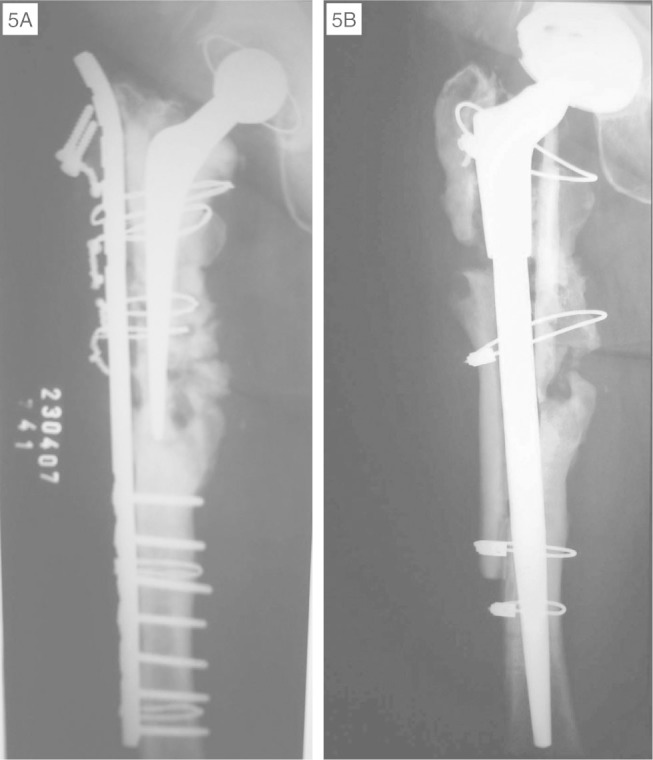
A) Patient DFC, who had undergone four previous surgical interventions, presenting extensive proximal femoral bone loss. B) Follow-up 16 months after the operation, showing signs of integration of the homologous graft, with formation of a medial bone callus
Box 3.
Results from revisions on THA cases using modular cementless femoral components with distal fixation
| Authors | Sample | Follow-up (years) | Survival |
|---|---|---|---|
| Kwong | 143 | 3.25 | 97.20% |
| Murphy | 35 | 2 | 97.10% |
| Schuh | 179 | 4 | 98.90% |
| Wirtz | 142 | 2.3 | 95.80% |
| Kang | 42 | 2 to 5 | 97.60% |
| Cameron | 320 | 2 to 12 | 98.60% |
| Christie | 163 | 4 to 7 | 97.10% |
Migration of the femoral stem was defined by Sporer and Paprosky(21) as distal displacement greater than 5 mm, comparing the radiographs produced just after the revision surgery with those from the last follow-up. This classification is extremely useful, because there is a direct relationship between migration and early mechanical failure of the implant(3). In none of our cases was there any distal displacement greater than 5 mm, by the time of the last evaluations.
Proximal bone restoration was achieved, to a greater or lesser extent, in 29 of our 30 cases. These were divided, according to the classification of Callaghan et al(31), into 14 type B cases and 15 type C cases. The bone formation observed was concordant with what has been found in many studies in which titanium femoral stems with distal fixation were used, thus diminishing the need to use homologous bone grafts from tissue banks32, 33.
The increase in the mean Harris Hip Score among our patients, from 39.2 to 93.8, indicated that the results were excellent, and these were in line with similar results in the literature3, 18, 28.
With regard to our complications, we found similar data in the studies investigated3, 14, 16, 17, 18, 24, 27, 28, and none of them interfered significantly with the osseointegration of the prostheses. Only in two cases (IPM and DKC) was there significant functional loss due to neurological sequelae and extensive proximal femoral bone loss, respectively. On the other hand, contrary to these other studies, we did not have any cases of femoral fracture. We believe that in addition to the careful preoperative procedures, the wire loop placed on the distal femur prior to stem impaction contributed towards increasing the mechanical resistance.
The greatest concern regarding modular prostheses with distal fixation is the risk of fracturing at the junctions between the components. Pierson et al(34) reported that the incidence of breakage of material with modular designs was 0.29%, in which there were direct associations with: (1) femoral components with an extended offset (greater lever arm); and (2) extensive proximal femoral bone loss (less support for the prosthesis). None of the patients in our sample have suffered fracturing of the implant so far. Reports of stem fracturing have not come exclusively from modular prostheses: fractures also occur in single-piece implants35, 36. To avoid greater mechanical stress on implants, structural bone grafts from tissue banks (Figure 5b) are strongly recommendable in cases of extensive bone loss, in order to increase the proximal support for the femoral components.
CONCLUSION
Our results from revision of total hip arthroplasty using ZMR® modular cementless distal fixation prostheses were extremely encouraging. All the components became osseointegrated and remained fixed at the time of the final evaluation. This forms a valuable treatment option for femoral revision of THA cases.
Footnotes
Work performed at Hospital de Caridade and Hospital Governador Celso Ramos (HGCR), Florianópolis (SC) Brazil, and at Hospital de Clínicas, UFPR, Curitiba (PR).
We declare that thers is no confilct of interests in this article
REFERENCES
- 2.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87(7):1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 2.Sculco TP, Sporer SM. Primary total hip and knee arthroplasty projections for the US population to the year 2030. American Academy of Orthopaedic Surgeons; Rosemont, IL: 2002. [Google Scholar]
- 3.Kang MN, Huddleston JI, Hwang K, Imrie S, Goodman SB. Early outcome of a modular femoral component in revision total hip arthroplasty. J Arthroplasty. 2008;23(2):220–225. doi: 10.1016/j.arth.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 4.Mulroy WF, Harris WH. Revision total hip arthroplasty with use of so-called second-generation cementing techniques for aseptic loosening of the femoral component. A fifteen-year-average follow-up study. J Bone Joint Surg Am. 1996;78(3):325–330. doi: 10.2106/00004623-199603000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Kavanagh BF, Ilstrup DM, Fitzgerald RH., Jr Revision total hip arthroplasty. J Bone Joint Surg Am. 1985;67(4):517–526. [PubMed] [Google Scholar]
- 6.Katz RP, Callaghan JJ, Sullivan PM, Johnston RC. Long-term results of revision total hip arthroplasty with improved cementing technique. J Bone Joint Surg Br. 1997;79(2):322–326. doi: 10.1302/0301-620x.79b2.7245. [DOI] [PubMed] [Google Scholar]
- 7.Haydon CM, Mehin R, Burnett S, Rorabeck CH, Bourne RB, McCalden RW. Revision total hip arthroplasty with use of a cemented femoral component. Results at a mean of ten years. J Bone Joint Surg Am. 2004;86(6):1179–1185. doi: 10.2106/00004623-200406000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Berry DJ, Harmsen WS, Ilstrup D, Lewallen DG, Cabanela ME. Survivorship of uncemented proximally porous-coated femoral components. Clin Orthop Relat Res. 1995;(319):319–377. [PubMed] [Google Scholar]
- 9.Malkani AL, Lewallen DG, Cabanela ME, Wallrichs SL. Femoral component revision using an uncemented, proximally coated, long-stem prosthesis. J Arthroplasty. 1996;11(4):411–418. doi: 10.1016/s0883-5403(96)80031-3. [DOI] [PubMed] [Google Scholar]
- 10.Hedley AK, Gruen TA, Ruoff DP. Revision of failed total hip arthroplasties with uncemented porous-coated anatomic components. Clin Orthop Relat Res. 1988;(235):235–290. [PubMed] [Google Scholar]
- 11.Woolson ST, Delaney TJ. Failure of a proximally porous-coated femoral prosthesis in revision total hip arthroplasty. J Arthroplasty. 1995;(10 Suppl):S22–S28. doi: 10.1016/s0883-5403(05)80227-x. [DOI] [PubMed] [Google Scholar]
- 12.Halliday BR, English HW, Timperley AJ, Gie GA, Ling RS. Femoral impactiongrafting with cement in revision total hip replacement. Evolution of the technique and results. J Bone Joint Surg Br. 2003;85(6):809–817. [PubMed] [Google Scholar]
- 13.Sierra RJ, Charity J, Tsiridis E, Timperley JA, Gie GA. The use of long cemented stems for femoral impaction grafting in revision total hip arthroplasty. J Bone Joint Surg Am. 2008;90(6):1330–1336. doi: 10.2106/JBJS.G.00055. [DOI] [PubMed] [Google Scholar]
- 14.Sporer SM, Paprosky WG. Femoral fixation in the face of considerable bone loss: the use of modular stems. Clin Orthop Relat Res. 2004;(429):429–431. doi: 10.1097/01.blo.0000150120.80409.0d. [DOI] [PubMed] [Google Scholar]
- 15.Engh CA, Jr, Hopper RH, Jr, Engh CA., Sr Distal ingrowth components. Clin Orthop Relat Res. 2004;(420):420–441. doi: 10.1097/00003086-200403000-00019. [DOI] [PubMed] [Google Scholar]
- 16.Ko PS, Lam JJ, Tio MK, Lee OB, Ip FK. Distal fixation with Wagner revision stem in treating Vancouver type B2 periprosthetic femur fractures in geriatric patients. J Arthroplasty. 2003;18(4):446–452. doi: 10.1016/s0883-5403(03)00148-7. [DOI] [PubMed] [Google Scholar]
- 17.Paprosky WG, Greidanus NV, Antoniou J. Minimum 10-year-results of extensively porous-coated stems in revision hip arthroplasty. Clin Orthop Relat Res. 1999;(369):369–370. doi: 10.1097/00003086-199912000-00024. [DOI] [PubMed] [Google Scholar]
- 18.Nadaud MC, Griffin WL, Fehring TK, Mason JB, Tabor OB, Jr, Odum S. Cementless revision total hip arthroplasty without allograft in severe proximal femoral defects. J Arthroplasty. 2005;20(6):738–744. doi: 10.1016/j.arth.2004.12.053. [DOI] [PubMed] [Google Scholar]
- 19.Valle CJ, Paprosky WG. Classification and an algorithmic approach to the reconstruction of femoral deficiency in revision total hip arthroplasty. J Bone Joint Surg Am. 2003;85(Suppl 4):1–6. doi: 10.2106/00004623-200300004-00001. [DOI] [PubMed] [Google Scholar]
- 20.McAuley JP, Engh CA., Jr Femoral fixation in the face of considerable bone loss: cylindrical and extensively coated femoral components. Clin Orthop Relat Res. 2004;(429):429–431. doi: 10.1097/01.blo.0000150274.21573.f4. [DOI] [PubMed] [Google Scholar]
- 21.Sporer SM, Paprosky WG. Revision total hip arthroplasty: the limits of fully coated stems. Clin Orthop Relat Res. 2003;(417):417–419. doi: 10.1097/01.blo.0000096803.78689.0c. [DOI] [PubMed] [Google Scholar]
- 22.Barrington JW, Freiberg AA, Rubash HE. Femoral component revision: modularity. In: Callaghan JJ, Rosenberg AG, Rubash HE, editors. The adult hip. 2nd. Lippincott Williams & Wilkins; Philadelphia: 2007. [Google Scholar]
- 23.Goldberg VM. Revision total hip arthroplasty using a cementless modular femoral hip design. Am J Orthop (Belle Mead NJ) 2002;31(4):202–204. [PubMed] [Google Scholar]
- 24.Park YS, Moon YW, Lim SJ. Revision total hip arthroplasty using a fluted and tapered modular distal fixation stem with and without extended trochanteric osteotomy. J Arthroplasty. 2007;22(7):993–999. doi: 10.1016/j.arth.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 25.Cherubino P, Surace MF, Zatti G. Stem revision: special implant versus primary device. Chir Organi Mov. 2003;88(3):281–284. [PubMed] [Google Scholar]
- 26.Hinrichs F, Boudriot U, Hünerkopf M, Griss P. [Design and first clinical results with the ZMR taper revision prosthesis] Z Orthop Ihre Grenzgeb. 2005;143(3):355–359. doi: 10.1055/s-2005-836456. [DOI] [PubMed] [Google Scholar]
- 27.McCarthy JC, Lee JA. Complex revision total hip arthroplasty with modular stems at a mean of 14 years. Clin Orthop Relat Res. 2007;465:166–169. doi: 10.1097/BLO.0b013e318159cb97. [DOI] [PubMed] [Google Scholar]
- 28.Kwong LM, Miller AJ, Lubinus P. A modular distal fixation option for proximal bone loss in revision total hip arthroplasty: a 2- to 6-year follow-up study. J Arthroplasty. 2003;18(3 Suppl 1):94–97. doi: 10.1054/arth.2003.50083. [DOI] [PubMed] [Google Scholar]
- 29.Jones RE. Modular revision stems in total hip arthroplasty. Clin Orthop Relat Res. 2004;(420):420–427. doi: 10.1097/00003086-200403000-00020. [DOI] [PubMed] [Google Scholar]
- 30.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 31.Callaghan JJ, Salvati EA, Pellicci PM, Wilson PD, Jr, Ranawat CS. Results of revision for mechanical failure after cemented total hip replacement, 1979 to 1982. A two to five-year follow-up. J Bone Joint Surg Am. 1985;67(7):1074–1085. [PubMed] [Google Scholar]
- 32.Boehm PM. Revision Wagner technique: stem. In: Callaghan JJ, Rosenberg AG, Rubash HE, editors. The adult hip. 2nd. Lippincott Williams & Wilkins; Philadelphia: 2007. [Google Scholar]
- 33.Pina Cabral FJS, Rabello BT, Pina Cabral FM, Silveira SLC, Penedo JLM, Freitas EHA. Revisão de artroplastia total de quadril utilizando haste femoral de Wagner. Rev Bras Ortop. 2006;41(10):393–398. [Google Scholar]
- 34.Pierson JL, Crowninshield RD, Earles DR. Fatigue fracture of a modular revision femoral component: a report of forty cases. American Academy of Orthopaedic Surgeons; Rosemont, IL: 2005. [Google Scholar]
- 35.Busch CA, Charles MN, Haydon CM, Bourne RB, Rorabeck CH, Macdonald SJ. Fractures of distally-fixed femoral stems after revision arthroplasty. J Bone Joint Surg Br. 2005;87(10):1333–1336. doi: 10.1302/0301-620X.87B10.16528. [DOI] [PubMed] [Google Scholar]
- 36.Crowninshield RD, Maloney WJ, Wentz DH, Levine DL. The role of proximal femoral support in stress development within hip prostheses. Clin Orthop Relat Res. 2004;(420):420–480. doi: 10.1097/00003086-200403000-00024. [DOI] [PubMed] [Google Scholar]