Abstract
Acute lateral ankle sprain (ALAS) is a common injury, but its treatment has yet to be firmly established. The purpose of this study was to investigate how Brazilian Orthopedists (including residents) manage the diagnosis, classification, treatment and complications of ALAS. Methods: A multiple-choice questionnaire was developed with the aim of addressing the main aspects of the treatment of ALAS. The questionnaire was made available on the official website of the Brazilian Society of Orthopedics and Traumatology between June 15 and August 1, 2004. Results: 444 questionnaires were included in the analysis. The results showed agreement among most of the interviewees in the following regards: 90.8% used a classification method to guide treatment of the sprain; 59% classified the ankle sprain with certainty; 63.7% used rigid immobilization in cases of totally torn ligaments; 60.6% used anti-inflammatory medication in cases of partial ligament tears; and 75.9% reported that residual pain was the most frequent complication. There was no consensus regarding the immobilization method for partial ALAS, given that immobilization and functional treatment were chosen with the same frequency (47%). There was no significant difference between the responses from residents and from orthopedists (p = 0.81). Conclusions: Orthopedists and orthopedic residents in Brazil have difficulty classifying ALAS and there is no consensus about the best therapeutic option for partial ALAS.
Keywords: Lateral Ligament, Ankle; Sprains and Strains; Health Evaluation
INTRODUCTION
The term “sprain” is defined as a traumatic ligament injury suffered by a joint because of sudden movement, which does not go as far as causing dislocation(1). It has been estimated that one case of acute lateral ankle sprain (ALAS) occurs among every 10,000 individuals per day. This is one of the commonest injuries to the musculoskeletal system, and also one of the commonest in sports(2).
Despite this high frequency, the diagnosis and management of ALAS remains a challenge(3), given that it is difficult to establish the severity of the injury definitively at the time of the initial trauma3, 4. Within this scenario, the management for ALAS continues to be a reason for divergences, as shown by several recent papers4, 5, 6, 7, 8, 9, 10, 11. In addition, over the long term, several studies have highlighted a worrying number of complications, including recurrent sprains, ankle instability and residual pain after the first sprain2, 3, 6, 12, 13, 14. This increases the socioeconomic importance of ALAS, since it may interfere acutely and chronically in individuals' professional and social lives3, 6, 9, 10.
Over the last five years, a considerable number of randomized controlled studies, along with systematic reviews, have been conducted or are under development8, 12, 15, 16, 17, 18, 19, 20, focusing on therapeutic improvements for soft-tissue ankle injuries, including ALAS6, 7, 9, 10. However, several authors have stated that there are still methodological limitations on clinical studies on the management of ALAS, because of methodological problems (sample size, heterogeneity of treatment methods or lack of standardization of the final outcomes from treatments)2, 9. In a systematic review on functional immobilization versus rigid immobilization and in 2006, in a review on surgical treatment versus conservative treatment for ALAS, Kerkhoffs et al(18) pointed out that the number of studies presenting methodological quality that was adequate for defining treatment evidence was very limited. The results from a recently published study comparing four treatment methods for severe ankle sprains(19) have also been criticized20, 21.
Thus, considering the frequency and socioeconomic importance of ALAS cases, and the divergences in the literature, evaluation of the knowledge and approaches taken by medical professionals in managing this injury is relevant both for gauging the need for discussion of this topic at scientific meetings and for guiding future clinical trials.
In this light, we conducted this psychometric study with the primary aim of answering the following question: How do Brazilian orthopedists treat ALAS? The secondary objective was to assess whether the management of ALAS treatment varied among the professional categories studied.
MATERIAL AND METHODS
This was a descriptive study. A questionnaire was drawn up (Annex 1), containing six objective multiple-choice questions that covered the main aspects of the diagnosis, classification, treatment and complications of ALAS. The questionnaire was evaluated and validated by the Continuing Education Commission of the Brazilian Society of Orthopedics and Traumatology (SBOT) and was made available between June 15 and August 1, 2004, on the SBOT's official website (www.sbot.org.br). The target public included residents undertaking a residency program on orthopedics and traumatology and orthopedists practicing in Brazil. The register was programmed such that only completely filled out forms would be accepted and such that each participant would only be able to send in the questionnaire once. In this manner, we did not have any sample losses. To resolve any doubts or problems among the participants, the electronic addresses of two of the investigators were made available. The terminology used in the questionnaire was defined before the interviewee would answer the questions.
Annex 1.
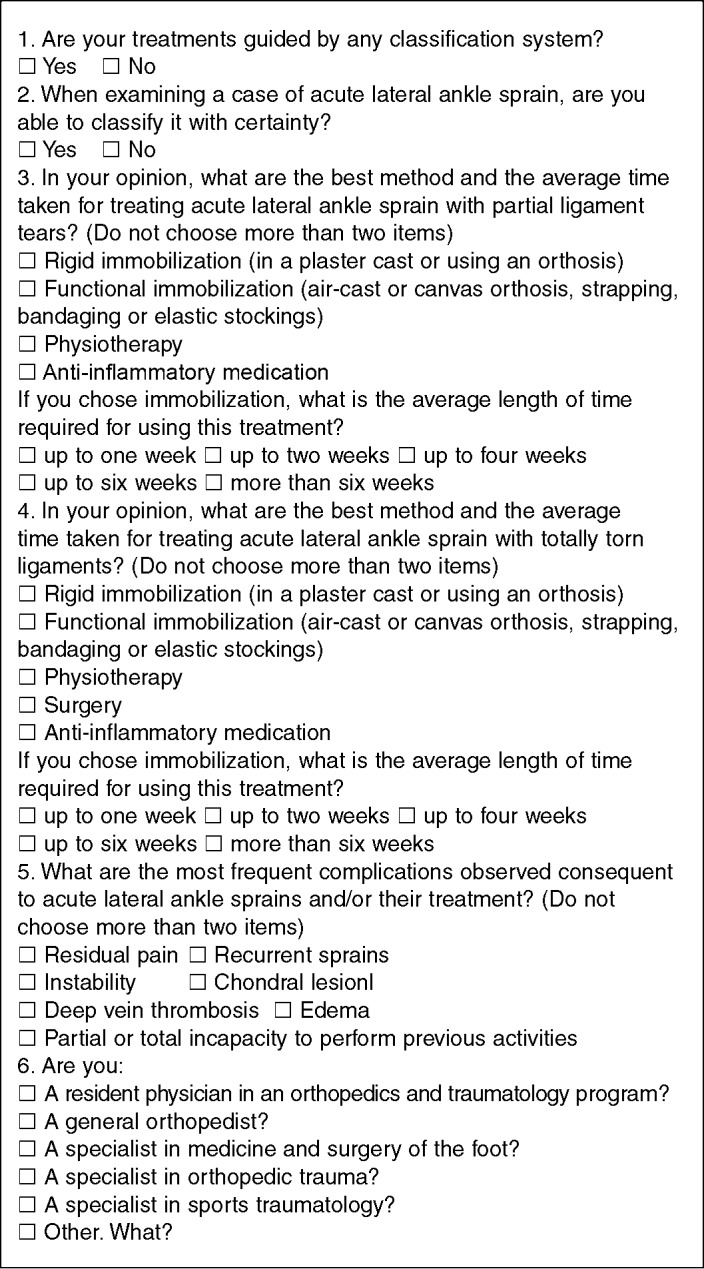
Evaluation questionnaire on acute lateral ankle sprains.
STATISTICAL ANALYSIS
The statistical analysis was performed using the Cochran Q test, Kruskal-Wallis test, Mann-Whitney test and chi-square test for category distribution, taking the critical value to be p < 0.05. To assess the sample adequacy, the possibility of agreement in the responses was taken to be 60%, with a maximum estimated error of 5% and an overall total of 10,000 orthopedists. Thus, the minimum sample size would be 369 participants.
RESULTS
A total of 444 professionals completely filled in the questionnaire and composed the sample for analysis. Among these, 173 (39%) were general orthopedists (O), 108 (24.3%) were residents in orthopedics and traumatology (R), 109 (24.5%) were specialists in foot medicine or surgery or in orthopedic trauma or sports traumatology (OE) and 54 (12.2%) were included as orthopedists in other specialties (OOE).
The results relating to knowledge of a classification method and its use for guiding the treatment are shown in Table 1. We found that 90.8% used a classification method to guide their treatment, but that only 59% were sure about classifying ALAS.
Table 1.
Results from questions 1 and 2 on the use of classifications for diagnosing acute lateral ankle sprains and confidence in the classification.
| Confidence in the classification |
Treatment based on a classification |
||
|---|---|---|---|
| Question 2 | Question 1 | ||
| Yes | No | Total | |
| n (%) | n (%) | n (%) | |
| Yes | 254 (57.2) | 8 (1.8) | 262 (59) |
| No | 149 (33.6) | 33 (7.4) | 182 (41) |
| Total n (%) | 403 (90.8) | 41 (9.2) | 444 (100) |
There were no significant differences in the responses to questions 1 and 2, or in the professionals' qualifications (Kruskal-Wallis; p = 0.28 and p = 0.47, respectively for questions 1 and 2).
The responses relating to therapeutic indications and time taken to treat ALAS with a partial injury showed that there was no consensus, given that equal numbers of participants suggested that functional immobilization (47.0%) and rigid immobilization (47.1%) were the interventions most used (chi-square test; p = 0.84). Since the question accepted two therapeutic options, physiotherapy was the second type of therapy suggested, with 30.4% of the responses.
With regard to the best method of treatment for ALAS with a totally torn ligament, rigid immobilization was the method most used (63.7%), followed by surgery (40.5%), physiotherapy (24.3%) and functional immobilization (16.2%).
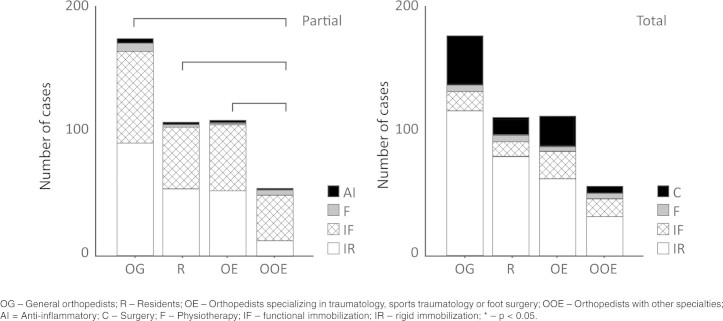
There was a statistically significant difference in the professional's qualifications regarding the type of therapeutic indication for treating partial ALAS (Kruskal-Wallis; p = 0.001). The difference occurred in the group of orthopedists from other specialties (OOE) in relation to all the other categories (Mann-Whitney U test; OOE vs. O, p = 0.000; OOE vs. R, p = 0.001; and OOE vs. E, p = 0.000). This difference consisted of greater frequency of indications for functional immobilization in this group of professionals, in relation to the other three groups (Figure 1). With regard to treating total ALAS, there was no significant difference between the professionals (Kruskal-Wallis; p = 0.11).
Figure 1.
Number of responses regarding the type of treatment for partial acute ankle sprain (left) and total acute ankle sprain (right), according to the type of professional.
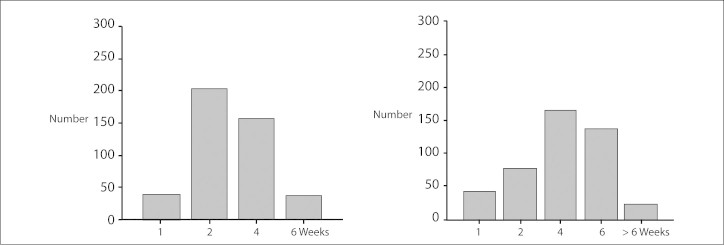
In the figures below, the responses relating to the time taken to treat partial or total ALAS are presented (Figure 2).
Figure 2.
Histogram of the number of responses in relation to the length of treatment, in weeks, for partial acute ankle sprains (left) and total acute ankle sprains (right).
It can be seen that the time of up to two weeks taken to treat partial injuries included 55.5% of the responses, and up to four weeks, 91% of the responses, with a mean of 2.96 ± 1.39 weeks. For total injuries, the time of up to four weeks taken for the treatment included 64% of the responses, and up to six weeks, 95% of the responses, with a mean of 4.1 ± 1.79 weeks. The time taken to treat total ALAS was significantly longer than for partial ALAS (Mann Whitney U test; p = 0.00), and there was no difference in this respect in relation to the professional's qualifications (Kruskal-Wallis; p = 0.23).
Anti-inflammatory medication was significantly more used for partial ligament tears (60.6%) that for total tears (39%) (Mann-Whitney U test; p = 0.00). There was no difference in these indications regarding the interviewees' professional qualifications (Kruskal-Wallis; p = 0.71; p = 0.46).
Residual pain was the most frequent complication OG – General orthopedists; R – Residents; OE – Orthopedists specializing in traumatology, sports traumatology or foot surgery; OOE – Orthopedists with other specialties; AI = Anti-inflammatory; C – Surgery; F – Physiotherapy; IF – functional immobilization; IR – rigid immobilization; * – p < 0.05. from ALAS (75%), followed by recurrent sprains (43.5%) and instability (34.5%). Edema (25%), partial or total incapacity to perform previous activities (11.5%), chondral lesions (5.6%) and deep vein thrombosis (0.2%) were less reported. There was no significant difference in these data in relation to the professionals' qualifications (Kruskal-Wallis, p = 0.71).
DISCUSSION
From reviewing the literature, two studies that had the aim of evaluating which were the treatment methods most used in cases of severe ankle sprain were found: one conducted in the United Kingdom(22) and the other in the Netherlands, focusing on the adequacy of physiotherapeutic management, in 2006(23). No studies with such aims were found in the Brazilian literature.
From a socioeconomic point of view, ALAS needs to be understood as a frequent, debilitating and burdensome disease. By using the approximate figure of one ALAS case for every 10,000 individuals per day(2), an extrapolation can be made showing that in the city of São Paulo (estimated population of around 10 million individuals; IBGE, 2007), 1,000 cases of lateral ankle sprains occur every day. Since around half of the population is in the economically active age group (between 20 and 65 years), 500 new cases appear among workers every day (IBGE CITIE). According to the data from the present study, at least half of the patients would be treated with rigid immobilization, which would stop them from carrying out their work activities during the immobilization period. If it is supposed that they are only off work for 14 days (1,750 absences per day), this would amount to around 1,277,500 days not worked over a one-year period. Taking the mean value of São Paulo workers' monthly salaries as R $818.00 (Federal Government “Zero Hunger” Program), this period off work would result in an annual cost of approximately 34 million reais. These figures show the need for standardized management, preferably based on the efficacy, cost and safety of the treatment.
It is difficult to precisely define the severity of ALAS at the first evaluation2, 4, 21, 24. This implies that the decision on the initial therapy is usually based on nonuniform criteria in the literature. In 2009, Lamb et al(19) used the criterion “inability to walk for three days” to classify ALAS as severe, whereas according to other authors, the gold standard criterion would be findings of abnormalities in the physical examination carried out five days after the sprain21, 24. Thus, the observation of Bernett and Schirmann(25) remains valid: these authors emphasized that the parameters used in the classifications that are available are anatomical and have little clinical applicability. These points may explain the paradoxical result from our study that more than 90% of the orthopedists used a classification method in making diagnoses, but only 57% of them used this to guide the treatment.
Although the results relating to the treatment options for total ALAS were better defined (60% with rigid immobilization and 40% with surgical treatment), the options for partial ALAS treatment were clearly undefined (47% both for functional immobilization and for rigid immobilization). This variability of management for ALAS cases was also observed in a similar study conducted in the United Kingdom(22). These results can be interpreted as adequate in the absence of any consensus seen in the literature on this topic. In a systematic review on functional immobilization versus rigid immobilization in cases of acute ankle sprain, Kerkhoffs et al(18) observed that although several factors favored functional immobilization, the conclusions should be interpreted cautiously, since they were not maintained when studies of poor methodological quality were excluded.
In relation to comparing surgical and non-surgical treatment, no conclusions have been reached regarding the best treatment method for ALAS, even through conducting randomized controlled studies8, 12, 15, 16, 17, 18, 19, 20 or systematic reviews6, 7, 9, 10. The two most recent reviews, by Kerkhoffs et al(2) and Jones(9), comparing surgical versus conservative treatment, produced contradictory results. In the first, the authors suggested that there was a statistical difference favoring surgical treatment, while in the second, it was concluded that functional immobilization was better. However, in both of these studies, it was emphasized that confidence in the results was low because of the methodological limitations of the studies included. In the study by Lamb et al(19), it was suggested that rigid immobilization (plaster cast for 10 days starting on the third day after the injury) was better with regard to quality of life and duration of pain, although their results have been criticized both because of a lack of control regarding other forms of treatment(21) and because of the case selection criteria, which did not take into consideration late examination of the ankle as an ideal method for case selection(24).
In treating cases of partial ALAS, the treatment type that was chosen the second most frequently was the use of non-hormonal anti-inflammatory drugs. In a recent review, there were indications that these drugs may improve joint function and accelerate injury cure, but they do not present any diminution of the pain and edema(11).
The results regarding the length of treatment were homogenous, such that most treatments took four to six weeks. The time taken was significantly longer in cases of totally torn ligaments. These data corroborate the common daily practice of emergency services, but despite this “tacit consensus”, no consistent data on this subject were found in the literature(26).
In evaluating the most frequent complications, most of the orthopedists indicated residual pain (75%) and, following this, recurrent sprains (43.5%) and instability (34.5%). Some recent studies have evaluated the short-term evolution of ALAS and its long-term evolution over a period of years and have shown that between one and three years after the trauma, there is a high prevalence of pain (33% to 43%), recurrent sprains (3% to 34%) and impossibility of walking for distances greater than one mile (1.6 km)(6,13,14). Thus, the results from the present study are congruent with regard to the types of complications encountered during the evolution of ALAS.
Certain points deserve to be raised regarding the analysis on our data. Since this was a study involving a questionnaire asking for memory recall, the events investigated may have been over or underestimated. Moreover, the data were obtained via the internet, which is a source of selection bias. On the other hand, this bias was diminished through the significant size of the sample. It is important to emphasize that these findings reflect the opinions of these orthopedists and do not necessarily represent a guide to treatment.
CONCLUSIONS
The data from this study showed that the Brazilian orthopedists had difficulty in classifying ALAS (only 57% did so securely). They had divergent opinions regarding the best therapeutic option for partial tears (47% used functional immobilization and 47.1% used rigid immobilization). However, they agreed in relation to total tears (63.7% indicated functional immobilization and 40.5%, surgery). They considered that pain was the main complication from ALAS (75%) and agreed regarding the duration of immobilization in cases of partial or total ALAS.
Implications for future research
There is a need for quality studies in order to develop a guide to uniform management of these injuries. Development of an objective, reproducible and clinically applicable classification system for ALAS should be the focus of future studies.
Footnotes
Work performed in the Department of Orthopedics and Traumatology, Federal University of São Paulo.
Declaramos inexistência de conflito de interesses neste artigo
REFERENCES
- 1.Kannus P, Renström P. Treatment for acute tears of the lateral ligaments of the ankle. Operation, cast, or early controlled mobilization. J Bone Joint Surg Am. 1991;73(2):305–312. [PubMed] [Google Scholar]
- 2.Kerkhoffs GM, Rowe BH, Assendelft WJ, Kelly K, Struijs PA, van Dijk CN. Immobilisation and functional treatment for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev. 2002;(3):CD003762. doi: 10.1002/14651858.CD003762. [DOI] [PubMed] [Google Scholar]
- 3.Abbassian A, Thomas R. Ankle ligament injuries. Br J Hosp Med (Lond) 2008;69(6):339–343. doi: 10.12968/hmed.2008.69.6.29624. [DOI] [PubMed] [Google Scholar]
- 4.Van Dijk CN, Lim LS, Bossuyt PM, Marti RK. Physical examination is sufficient for the diagnosis of sprained ankles. J Bone Joint Surg Br. 1996;78(6):958–962. doi: 10.1302/0301-620x78b6.1283. [DOI] [PubMed] [Google Scholar]
- 5.McKeon PO, Mattacola CG. Interventions for the prevention of first time and recurrent ankle sprains. Clin Sports Med. 2008;27(3):371–382. doi: 10.1016/j.csm.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 6.Margo KL. Review: many adults still have pain and subjective instability at 1 year after acute lateral ankle sprain. Evid Based Med. 2008;13(6):187. doi: 10.1136/ebm.13.6.187. [DOI] [PubMed] [Google Scholar]
- 7.Bleakley CM, McDonough SM, MacAuley DC. Some conservative strategies are effective when added to controlled mobilisation with external support after acute ankle sprain: a systematic review. Aust J Physiother. 2008;54(1):7–20. doi: 10.1016/s0004-9514(08)70061-8. [DOI] [PubMed] [Google Scholar]
- 8.Mohammadi F. Comparison of 3 preventive methods to reduce the recurrence of ankle inversion sprains in male soccer players. Am J Sports Med. 2007;35(6):922–926. doi: 10.1177/0363546507299259. [DOI] [PubMed] [Google Scholar]
- 9.Jones MH, Amendola AS. Acute treatment of inversion ankle sprains: immobilization versus functional treatment. Clin Orthop Relat Res. 2007;455:169–172. doi: 10.1097/BLO.0b013e31802f5468. [DOI] [PubMed] [Google Scholar]
- 10.Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37(1):73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 11.Ivins D. Acute ankle sprain: an update. Am Fam Physician. 2006;74(10):1714–1720. [PubMed] [Google Scholar]
- 12.Hupperets MD, Verhagen EA, van Mechelen W. The 2BFit study: is an unsupervised proprioceptive balance board training programme, given in addition to usual care, effective in preventing ankle sprain recurrences? Design of a randomized controlled trial. BMC Musculoskelet Disord. 2008;9:71. doi: 10.1186/1471-2474-9-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haywood KL, Hargreaves J, Lamb SE. Multi-item outcome measures for lateral ligament injury of the ankle: a structured review. J Eval Clin Pract. 2004;10(2):339–352. doi: 10.1111/j.1365-2753.2003.00435.x. [DOI] [PubMed] [Google Scholar]
- 14.Braun BL. Effects of ankle sprain in a general clinic population 6 to 18 months after medical evaluation. Arch Fam Med. 1999;8(2):143–148. doi: 10.1001/archfami.8.2.143. [DOI] [PubMed] [Google Scholar]
- 15.Bleakley CM, O'Connor S, Tully MA, Rocke LG, Macauley DC, McDonough SM. The PRICE study (Protection Rest Ice Compression Elevation): design of a randomized controlled trial comparing standard versus cryokinetic ice applications in the management of acute ankle sprain [ISRCTN13903946] BMC Musculoskelet Disord. 2007;8:125. doi: 10.1186/1471-2474-8-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van Rijn RM, van Os AG, Kleinrensink GJ, Bernsen RM, Verhaar JA, Koes BW. Supervised exercises for adults with acute lateral ankle sprain: a randomised controlled trial. Br J Gen Pract. 2007;57(543):793–800. [PMC free article] [PubMed] [Google Scholar]
- 17.Petrella RJ, Petrella MJ, Cogliano A. Periarticular hyaluronic acid in acute ankle sprain. Clin J Sport Med. 2007;17(4):251–257. doi: 10.1097/JSM.0b013e3180f6169f. [DOI] [PubMed] [Google Scholar]
- 18.Kerkhoffs GM, Handoll HH, de Bie R, Rowe BH, Struijs PA. Surgical versus conservative treatment for acute injuries of the lateral ligament complex of the ankle in adults. Cochrane Database Syst Rev. 2002;(3):CD000380. doi: 10.1002/14651858.CD000380. [DOI] [PubMed] [Google Scholar]
- 19.Lamb SE, Marsh JL, Hutton JL, Nakash R, Cooke MW, Collaborative Ankle Support Trial (CAST Group) Mechanical supports for acute, severe ankle sprain: a pragmatic, multicentre, randomised controlled trial. Lancet. 2009;373(9663):575–581. doi: 10.1016/S0140-6736(09)60206-3. [DOI] [PubMed] [Google Scholar]
- 20.Cooke MW, Marsh JL, Clark M, Nakash R, Jarvis RM. Treatment of severe ankle sprain: a pragmatic randomised controlled trial comparing the clinical effectiveness and cost-effectiveness of three types of mechanical ankle support with tubular bandage. The CAST trial. Health Technol Assess. 2009;13(13):1–121. doi: 10.3310/hta13130. [DOI] [PubMed] [Google Scholar]
- 21.Kerkhoffs GM, van den Bekerom MP, Struijs PA, van Dijk CN. 10-day below-knee cast for management of severe ankle sprains. Lancet. 2009;373(9675):1601. doi: 10.1016/S0140-6736(09)60898-9. [DOI] [PubMed] [Google Scholar]
- 22.Cooke MW, Lamb SE, Marsh J, Dale J. A survey of current consultant practice of treatment of severe ankle sprains in emergency departments in the United Kingdom. Emerg Med J. 2003;20(6):505–507. doi: 10.1136/emj.20.6.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leemrijse CJ, Plas GM, Hofhuis H, van den Ende CH. Compliance with the guidelines for acute ankle sprain for physiotherapists is moderate in the Netherlands: an observational study. Aust J Physiother. 2006;52(4):293–299. doi: 10.1016/s0004-9514(06)70010-1. [DOI] [PubMed] [Google Scholar]
- 24.Van Rijn RM, van Middelkoop M. 10-day below-knee cast for management of severe ankle sprains. Lancet. 2009 May. 1999;373(9675):1601. doi: 10.1016/S0140-6736(09)60897-7. [DOI] [PubMed] [Google Scholar]
- 25.Bernett P, Schirmann A. [Acute sporting injuries of the ankle joint (author's transl)] Unfallheilkunde. 1979;82(4):155–160. [PubMed] [Google Scholar]
- 26.Yamamoto H, Ishibashi T, Muneta T, Furuya K. Nonsurgical treatment of lateral ligament injury of the ankle joint. Foot Ankle. 1993;14(9):500–504. doi: 10.1177/107110079301400903. [DOI] [PubMed] [Google Scholar]