Abstract
Objective: To evaluate the functional and anatomical results from surgical treatment via arthroscopy in cases of complete rupture of the rotator cuff, using ultrasound images and the Constant and Murley functional index to investigate the correlation between them. Methods: 100 patients (110 shoulders) were evaluated. The mean follow-up was 48.8 ± 33.28 months (12 to 141 months). The mean age was 60.25 ± 10.09 (36 to 81 years). Rupture of the supraspinal tendon alone occurred in 85 cases (77%), and in association with the infraspinatus in 20 cases (18%) and subscapularis in four shoulders (4%). An association of supraspinatus, infraspinatus and subscapularis lesions was found in one shoulder (1%). The lesions were classified according to DeOrio and Cofield scores as small/medium in 85 shoulders (77%) and large/extensive in 25 (23%). The clinical results were assessed in accordance with the Constant and Murley criteria. The ultrasound results relate to reports issued by different radiologists. Statistical analysis was carried out using the chi-square test, Fisher's exact test, Student's t test, Pearson's correlation, Kruskal-Wallis correlation and logistic regression (significance: p < 0.05). Results: The mean Constant evaluation was 85.3 ± 10.06 in the normal shoulders and 83.96 ± 8.67 in the operated shoulders (p = 0.224). Excellent and good results were found in 74 shoulders (67%), satisfactory and moderate results in 32 (29%) and poor results in four (4%). The ultrasound evaluation showed 38 shoulders with re-rupture (35%) and absence of rupture in 71 (65%). Among the 74 shoulders (67%) with excellent/good results, 22 (30%) presented re-rupture in the ultrasound report (p = 0.294). Among the four shoulders (4%) with poor results, two (50%) presented reports of intact tendons (p = 0.294). Conclusion: There was no statistically valid correlation between the ultrasound diagnosis and the clinical evaluation of results among the patients who underwent arthroscopic repair to treat full tear lesions of the rotator cuff. The clinical results from the complete rotator cuff repairs via arthroscopy presented a high level of functional recovery (Constant 83.96), compared with the contralateral shoulder. The postoperative ultrasound reports presented a high percentage of re-rupture (35%). Postoperative strength was greater among the patients aged under 60 years (p = 0.002) and in cases of lesions less than or equal to 3 cm (p = 0.003).
Keywords: Rotator cuff, Arthroscopy, Ultrasonography
INTRODUCTION
Rotator cuff tears occur frequently in the population over 50 years of age. This is a condition of multifactorial etiology, with the characteristics of degenerative lesions in most cases, and it affects 10 to 90% of the population1, 2. The diagnosis is based on clinical evaluation and imaging methods. Factors such physiological age and functional demand will determine whether the treatment should be conservative or surgical (open or arthroscopic repair). The functional and structural evaluation has been a subject of discussion3, 4, since most studies have had short follow-ups and small samples. Many difficulties are found in postoperative evaluations on the rotator cuff by means of ultrasonography, and understanding the anatomical variations is among these.
Although this imaging examination has high preoperative sensitivity and specificity rates, this is not the case in postoperative evaluations. Despite such imprecision5, 6, 7, it is often used as an imaging examination for diagnosing re-rupture of the rotator cuff because it is a low-cost and noninvasive examination that is easily accessible for the population and, in addition, it enables evaluation of the contralateral shoulder(8). This method may identify the tendons involved and the extent of the lesion(6), but the quality of the image is fundamental for the diagnosis(9).
Arthroscopic repair of lesions of the rotator cuff presents high rates of good and excellent clinical results1, 4, 5, 10, 11, even though adequate healing of the tendon does not occur in many cases(3). Re-rupture is one of the complications encountered. Studies using functional scores and imaging examinations have demonstrated incoherent correlations between function and reports of re-rupture. For this reason, there is no well-defined standard that would correlate functional capacity and anatomical integrity of the tendons(3). Images of re-rupture remain a challenge for radiologists. There is a need to standardize what an image of re-rupture consists of, because the definitions of this lesion and its extent vary significantly in the literature(3). Nevertheless, the high cost of nuclear magnetic resonance (NMR), the degree of difficulty in understanding the postsurgical anatomy of the rotator cuff through this examination and the impossibility of performing arthroscopy (gold standard) on all patients undergoing postoperative follow-up make ultrasonography a viable option. Because ultrasonography is an examiner-dependent examination, it ought to be performed by a single radiologist. Unfortunately, this is not the real situation in Brazil and, often for reasons outside of physicians' requirements, the examinations are performed randomly.
The aim of the present study was to evaluate the anatomical and functional integrity of arthroscopic repairs on cases of complete tearing of the rotator cuff, using ultrasound images and Constant and Murley functional scores(12), and to investigate the degree of concordance between them.
SAMPLE AND METHODS
A prospective study with functional and ultrasound evaluations was conducted in relation to 1,531 operations that were carried out between September 1996 and May 2007, at the Orthopedic Hospital and Belo Horizonte Hospital, in the city of Belo Horizonte, Minas Gerais.
The exclusion criteria consisted of less than one years of follow-up, glenohumeral arthrosis with advanced joint degeneration, calcaneal tendinitis, rheumatoid arthritis, adhesive capsulitis, sequelae from fractures, failure to locate patients or insufficient documentation (Figure 1).
Figure 1.

A) Ultrasound image demonstrating an anatomical abnormality consequent to an area of scarring on the supraspinal tendon. B) Ultrasound image showing anatomical integrity
A sample of 147 patients (159 shoulders) was selected, from whom 47 patients (49 shoulders) were excluded because of a lack of postoperative ultrasound examination, incomplete functional assessment, or both. Thus, 100 patients (110 shoulders) remained in the sample, consisting of 36 men (33%) and 74 women (67%). The mean follow-up was 48.8 ± 33.28 months (ranging from 12 to 141 months). The mean age of the study group was 60.25 ± 10.09 years (ranging from 36 to 81 years) (Figure 2). The right shoulder was affected in 86 cases (78%) and the left shoulder in 24 cases (22%). Ten patients (10%) had bilateral lesions. The affected shoulder was on the dominant side in 88 cases (80%) and the non-dominant side in 22 cases (20%). Thirty-four percent of the patients were sports practitioners and 66 (66%) were not.
Figure 2.
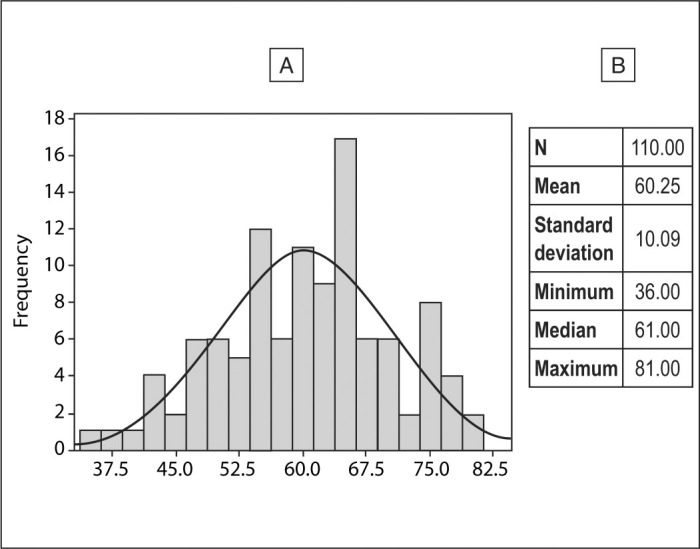
A) Population distribution according to age. B) Population characterization according to age
Before the operation, it was observed that in the topography of the tendons involves, the supraspinatus was present in 110 shoulders (100% of the cases). Rupture of the supraspinatus tendon alone was present in 85 shoulders (77%), while it was present in association with the infraspinatus (posterosuperior lesion) in 20 shoulders (18%) and in association with the subscapularis (anterosuperior lesion) in four shoulders (4%). Anassociation involving lesions of the supraspinatus, infraspinatus and subscapularis was found in one shoulder (1%) (Figure 3).
Figure 3.
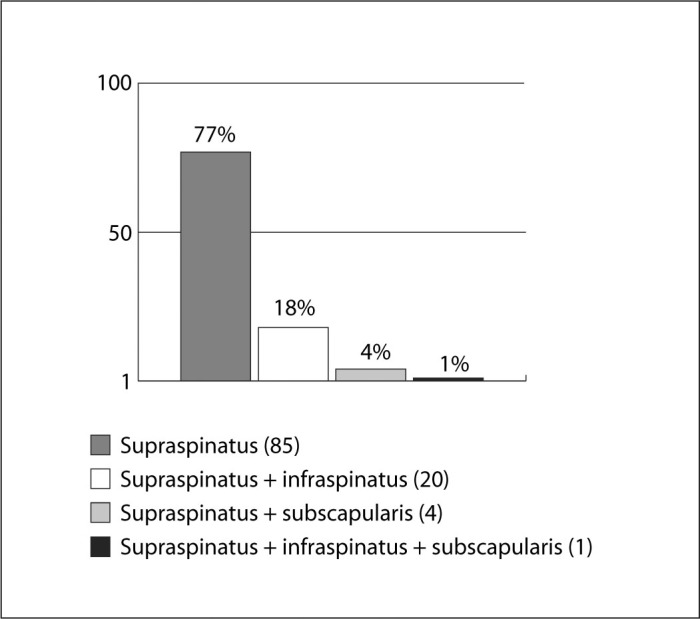
Tendons affected
The length of the lesions in the anteroposterior orientation, as measured during the arthroscopic procedure, after debridement, ranged from 0.5 cm to 5.4 cm. In accordance with DeOrio and Cofield(13), the lesions were classified as small (≤ 1 cm), present in 14 shoulders (13%); medium (1-3 cm) in 71 shoulders (65%); large (3-5 cm) in 23 shoulders (21%); and extensive (> 5 cm) in two shoulders (2%) (Figure 4).
Figure 4.
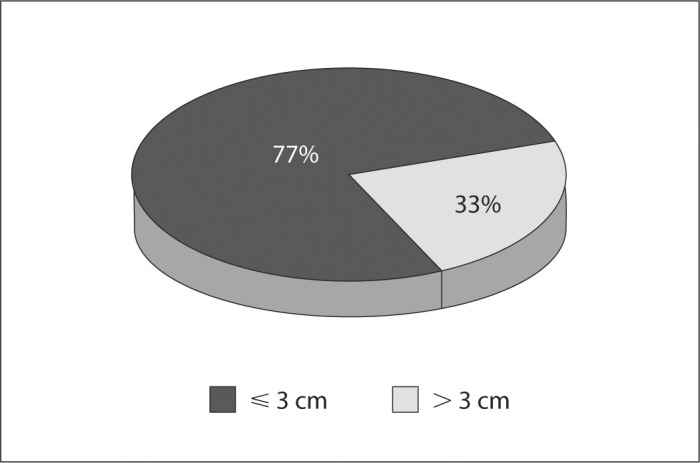
Extent of the lesion in the anteroposterior orientation following tendon debridement
Evaluation of the tendon of the long head of the biceps during the operation showed that there were 63 normal tendons (57%) and five ruptured tendons (5%). The remainder presented some degree of degeneration: tenolysis was performed on two (2%), tenotomy on 31 (28%) and tenodesis on nine (8%).
Subacromial decompression (anteroinferior acromioplasty) was performed on 108 shoulders (98%).
The clinical evaluation on the results was performed in accordance with the criteria of Constant and Murley(12), who used two subjective parameters (pain and activities of daily living) and two objective parameters (range of motion and strength). The maximum score of 100 points would correspond to an asymptomatic shoulder with complete function and strength of approximately 11 kg). Pain could be absent (15 points), mild (10 points), moderate (5 points) or intense (0). The activities of daily living could total 20 points: full-time work without limitations (4 points), recreational activity without limitations (4 points), lack of sleep disturbance due to pain (2 points) and positioning of the hand in space (10 points when the hand reached the level of above the head). Function was evaluated according to range of motion (ROM), with 10 points for each integral evaluation (medial rotation, lateral rotation, abduction and flexion), thus totaling 40 points. Strength was measured in pounds (kg multiplied by a constant of 2.2). Thus, the normal pattern referred to an asymptomatic 25-year-old individual with a strength of 25 pounds (approximately 11 kg). For this, a fixed-point domestic balance was used (Figures 5A and 5B), with marking limited to 12 kg, for recording the values measured through the Jobe test12, 14. According to Boehm(15), the results encountered through Constant's method may be excellent (91-100), good (81-90), satisfactory (71-80), moderate (61-70) or poor (< 60).
Figure 5.

A) Positioning for strength measurements in accordance with Constant and Fisher. B) Device with fixed-point conventional dynamometer, limited to 12 kg
The results from ultrasonography related to reports issued by different radiologists, using equipment with transducers of varying power (7.5 to 15 MHz). The examinations were performed postoperatively, after an interval of one to two years in the cases of 52 shoulders (47%); two to five years in the cases of 31 shoulders (28%); and more than five years in the cases of 27 shoulders (25%).
The statistical analysis was performed in accordance with the methods of the chi-square test, Fisher's exact test, Student's t test, Pearson's correlation, Kruskal-Wallis test and logistic regression, with the significance level set at p < 0.05.
RESULTS
The mean from the Constant evaluation was found to be 85.3 ± 10.06 (range 46 to 99) for the normal shoulders and 83.96 ± 8.67 (range 59 to 99) for the operated shoulders (p = 0.224). There were excellent and good results from 74 shoulders (67%), satisfactory and moderate results from 32 (29%) and poor results from four (4%).
Excluding the bilateral cases, the mean ipsilateral postoperative strength was 5.53 kg ± 2.34 (range 2 to 11) and the contralateral strength was 5.88 kg ± 2.45 (range 0.6 to 11) (p = 0.091). The mean postoperative strength was 6.38 kg ± 2.53 among the patients in the age group between 41 and 60 years, and 4.78 kg ± 2.23 among the patients over the age of 60 years (p = 0.002). Among the lesions that were less than or equal to 3 cm, 85 shoulders (77%) presented a mean postoperative strength of 5.64 kg ± 2.41. Among the lesions that were greater than 3 cm, 25 shoulders (23%) demonstrated strength of 4.00 kg ± 2.03 (p = 0.003).
There was no statistically significant difference in the mean postoperative strength between the patients who presented ultrasound reports showing re-rupture and those showing anatomical integrity (p = 0.256) (Figure 6).
Figure 6.

Descriptive statistics showing the non-significant difference in postoperative strength measurements between tendons with and without re-rupture, as shown by ultrasonography. (p = 0.256). No: absence of re-rupture; Yes: presence of re-rupture
The mean score on Constant's scale among the patients who had undergone tenodesis of the long head of the biceps was 86.73 ± 9.42, versus 78.10 ± 10.60 in the cases with tenotomy (p = 0.035).
Eighty-one of the patients evaluated (74%) did not have any complaint of pain, while 29 (26%) presented some degree of residual pain. Of the latter, 20 (17%) complained of mild pain, five (5%) of moderate pain and four (4%) of severe pain. Among the patients with excellent and good results, eight (11%) presented complaints of pain.
The ultrasound evaluation showed that 38 shoulders (35%) presented re-rupture, while there was absence of rupture in 71 shoulders (65%). One diagnosis was inconclusive and was therefore excluded.
Simultaneous occurrences of results according to Constant's classification and the ultrasound reports are represented in Box 1 (P = 0.294) (Box 1).
Box 1.
Correlation between Constant's functional assessment (categorized by Boehm)(15) and the ultrasound results.
| Constant | Ultrasound |
Total | |
|---|---|---|---|
| Re-rupture | Integral | ||
| Excellent and good | 22 | 51 | 73 |
| Satisfactory and moderate | 14 | 18 | 32 |
| Poor | 2 | 2 | 4 |
| Total | 38 | 71 | 109 |
The correlation between the ultrasound findings and the length of follow-up is represented in Box 2 (P = 0.133).
Box 2.
Correlation between length of follow-up and the ultrasound results.
| Follow-up | Ultrasound |
Total | |
|---|---|---|---|
| Re-rupture | Integral | ||
| 1 to 2 years | 14 (27%) | 38 (73%) | 52 (100%) |
| 2 to 5 years | 11 (35%) | 20 (65%) | 31 (100%) |
| ' 5 years | 13 (50%) | 13 (50%) | 26 (100%) |
Occurrences of re-rupture (ultrasound) according to the extent of the lesions is represented in Box 3 (P = 0.531).
Box 3.
Correlation between the extent of the lesion of the rotator cuff and the ultrasound results.
| Extent of lesion | Ultrasound |
Total | |
|---|---|---|---|
| Re-rupture | Integral | ||
| ≤ 3 cm | 30 (35%) | 55 (65%) | 85 (100%) |
| > 3 cm | 8 (33%) | 16 (67%) | 24 (100%) |
DISCUSSION
Ultrasonography is widely used for diagnosing rotator cuff injuries9, 16. However, the results from analysis on operated shoulders are compromised16, 17. Some authors have stated that this diagnostic method may present high rates of sensitivity, specificity and precision, even under such conditions, when they are performed by experienced professionals5, 6, 7, 18, 19. Through the present study, we did not find any coherent correlation between the structural analysis on the tendons (ultrasound) and the functional result (Constant). We observed re-rupture rates of up to 20% among patients with excellent and good functional results, and this has also been cited in the literature1, 3, 4, 17. Postoperative functional and structural evaluations have been a subject of discussion3, 4, 17. It can be seen that the studies on repairs performed arthroscopically present results from short follow-ups on small samples3, 6, 7, 20. Inadequate understanding and lack of standardization of postoperative ultrasound findings(21) may at least partially explain our incoherent findings. Crass et al(21) described anatomical distortion consequent to adherence between the deltoid muscle and the rotator cuff, presence of granulation tissue and changes in the direction of fibers as veritable obstacles hindering precise diagnosis (i.e. diagnosis of what re-rupture really represents). This suggests that there is a need for a more effective method for image evaluation. Similar characteristics have been cited in other studies16, 20. In the light of such limitations, Furtschegger and Resch(16) designed a study that attempted to define postoperative ultrasound criteria for rotator cuff injuries. They highlighted inability to view the tendon and its echogenic discontinuity as determining factors for diagnosing such injuries.
Standardization of the equipment and of the ultrasonography technique has been recommended by several authors3, 5, 6. Nevertheless, this academic practice does not reflect the realities of clinical practice. Patients and physicians cannot always entrust their examinations to the few highly experienced professionals, or to centers of excellence with latest-generation equipment. Thus, studies conducted under special conditions overvalue the method, in a generic manner that is distant from the realities. Diagnostic ultrasonography has undergone significant advances that should be reconsidered.
We used the functional protocol of Constant and Murley(12) and grouped our results as suggested by Boehm(15), contrary to some authors who used protocols that emphasized criteria that were more subjective3, 8, 17, 22. In the total scores possible according to this protocol, 25 points were attributed to strength, which corresponds to a direct correlation with the anatomical integrity of the tendon4, 23. In the present series, we found that the absolute mean score using the protocol of Constant e Murley(12) on the operated shoulders was 83.96 ± 8.67. Gartsman et al(23) found a similar value (83.6) from their evaluation on 73 patients with a two-year follow-up. They also compared the mean preoperative strength with the mean postoperative strength and found that the mean increase was 2.9 kg, which was statistically significant.
In the present study, we compared the mean ipsilateral postoperative strength (5.53 kg ± 2.34) with the contralateral strength (5.88 kg ± 2.45) and did not find any statistical significant difference (p = 0.091), thus demonstrating that the strengths were equivalent to each other. We also did not find any significant difference in mean postoperative strength between the patients who presented ultrasound reports showing re-rupture (4.77 kg ± 2.45) and those showing integral tendons (5.50 kg ± 2.39) (p = 0.126).
We evaluated the correlation between the extent of the lesions and the postoperative strength and found better results in relation to the lesions that were less than or equal to 3 cm. The mean strength observed among these patients was 5.64 kg ± 2.03, versus 4.0 kg ± 2.41 for those with lesions larger than 3 cm (p = 0.003).
For 39 patients (41 shoulders), we documented the preoperative strength with the aim of carrying out a prospective study. Among this group, the change in mean strength from before to after the operation was from 3.82 kg to 5.05 kg (p < 0.0001), respectively.
Mack et al(20) found that pain was a residual symptom among 26% of their patients with excellent and good results who had undergone open surgery. We observed the presence of pain of different intensities in 26% of the cases that we studied. Among the 74 shoulders (67%) with excellent and good functional results, eight shoulders (11%) presented pain, although its intensity was mild.
Arthroscopy for rotator cuff injuries presents high rates of good and excellent results1, 4, 5, 10, 11. Re-rupture is one of the complications reported, at a frequency ranging from 20 to 65% of the cases1, 4, 17. Through an evaluation using ultrasonography two years after open surgery to repair large and extensive injuries of the rotator cuff, Galatz et al(17) found new lesions in 94% of the cases. DeFranco et al(3) found a re-rupture rate of 40% from a three-year follow-up on arthroscopic repairs to lesions smaller than 3 cm, using ultrasound. Harryman et al(8) stated that ultrasound was capable of diagnosing 65% of the tendons that were unbroken, five years after the operation. Sugaya et al(22) found a re-rupture rate of 13% among medial lesion and 44% among large and extensive lesions, using NMR for postoperative structural analysis.
We found that re-rupture was shown in 35% of the ultrasound reports among our sample.
There are studies in the literature that show that there is no relationship between function and integrity of repair following surgery on the rotator cuff3, 24. Harryman et al(8) reported increases in strength, function and activity with the arm above head height, among the patients who presented structural integrity of the repaired tendons. They also reported that for 87% of the patients who presented re-rupture on ultrasound images, it was not possible to observe any abnormality in the clinical examination, thus affirming that ultrasound is imprecise in relation to evaluating re-rupture alone. DeFranco et al(3) stated that the functional improvement was more significant when the anatomical integrity was fully restored, but that partial lesions or re-ruptures did not necessarily imply unsatisfactory functional results. We did not find any statistical significance in relation to simultaneous occurrence of excellent/good functional results and ultrasound reports showing structural integrity (p = 0.294). Nor was there any statistical significance regarding the incoherent occurrences of excellent/good functional results with ultrasound reports showing re-rupture (p = 0.294).
DeFranco et al(3) reported that age was the main predictive factor for structural integrity following arthroscopic repair. In our study, age did not show any statistical significance in relation to postoperative integrity of the rotator cuff, as assessed using ultrasonography (p = 0.767). However, age was a negative predictive factor regarding excellent/good functional results (p = 0.008).
A significant difference was observed in the relationship between postoperative strength and age, such that it was observed that the patients under 60 years of age presented greater mean strength (5.90 kg ± 2.49) than those over the age of 60 years (4.70 kg ± 2.23) (p = 0.009).
It was observed that the patients whose mean postoperative follow-ups were longer (4.29 years ± 2.77) presented greater incidence of ultrasound reports of re-rupture than did the patients with shorter follow-ups (3.13 years ± 2.48) (p = 0.034).
CONCLUSIONS
-
1
–There was no statistically valid correlation between the functional result and the ultrasound image (p = 0.294).
-
2
–The clinical result from the repairs on the complete ruptures of the rotator cuff using arthroscopy presented a high percentage of functional recovery (Constant 83.96), in comparison with the contralateral side.
-
3
–The evaluation using ultrasound images presented high rates of re-rupture (35%).
-
4
– The postoperative strength was greater among patients younger than 60 years (p = 0.002) and among cases of lesions of less than or equal to 3 cm (p = 0.003).
Footnotes
Work performed by the Shoulder Group at the Orthopedic Hospital and Belo Horizonte Hospital, Belo Horizonte, MG.
REFERENCES
- 1.Williams GR, Jr, Rockwood CA, Jr, Bigliani LU, Lannotti JP, Stanwoo W. Rotator cuff tears: Why do we repair them? J Bone Joint Surg Am. 2004;86(12):2764–2776. [PubMed] [Google Scholar]
- 2.Veado MAC, Gomes TPO, Pinto RZA. Análise funcional e estrutural do reparo das lesies extensas do manguito rotador. Rev Bras Ortop. 2006;41(8):294–301. [Google Scholar]
- 3.DeFranco MJ, Bershadsky B, Ciccone J, Yum J, Lannotti JP. Functional outcome of arthroscopic rotator cuff repairs: A correlation of anatomic and clinical results. J Shoulder Elbow Surg. 2007;16(6):759–765. doi: 10.1016/j.jse.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 4.Gazielly DF, Gleyze P, Montagnon C. Functional and anatomical results after rotator cuff repair. Clin Orthop Relat Res. 1994;(304):304–353. [PubMed] [Google Scholar]
- 5.Lannotti JP, Ciccone J, Buss DD, Visotsky JL, Mascha E, Cotman K. Accuracy of office-based ultrasonography of the shoulder for the diagnosis of rotator cuff tears. J Bone Joint Surg Am. 2005;87(6):1305–1311. doi: 10.2106/JBJS.D.02100. [DOI] [PubMed] [Google Scholar]
- 6.Teefey SA, Hasan A, Middleton WD, Patel M, Wright RW, Yamaguchi K. Ultrasonography of the rotator cuff: A comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am. 2000;82(4):498–504. [PubMed] [Google Scholar]
- 7.Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears: comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. 2004;86(4):708–716. [PubMed] [Google Scholar]
- 8.Harryman DT, 2nd, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA., 3rd Repairs of the rotator cuff: correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73(7):982–989. [PubMed] [Google Scholar]
- 9.Brandt TD, Cardone BW, Grant TH, Post M, Weiss CA. Rotator cuff sonography: a reassessment. Radiology. 1989;173(2):323–327. doi: 10.1148/radiology.173.2.2678248. [DOI] [PubMed] [Google Scholar]
- 10.Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87(6):1229–1240. doi: 10.2106/JBJS.D.02035. [DOI] [PubMed] [Google Scholar]
- 11.Godinho GG. Reparação artroscópica do manguito rotador do ombro: avaliação funcional dos resultados de 87 pacientes [tese] Universidade Federal de São Paulo. Escola Paulista de Medicina; São Paulo: 2002. [Google Scholar]
- 12.Constant CR, Murley AHG. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214):214–215. [PubMed] [Google Scholar]
- 13.DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am. 1984;66(4):563–567. [PubMed] [Google Scholar]
- 14.Fischer BW, Gross MR, McCarthy JA, Arroyo JS. Incidence of acromioclavicular joint complications after athroscopic subacromial descompression. Arthroscopy. 1999;15(3):241–248. doi: 10.1016/s0749-8063(99)70028-9. [DOI] [PubMed] [Google Scholar]
- 15.Boehm D. Valuation of the Constant score. In: Habermeyer P, Magosch P, Lichtenberg S, editors. Classifications and scores of the shoulder. Springer; Heidelberg: 2006. p. 204. [Google Scholar]
- 16.Furtschegger A, Resch H. Value of ultrasonography in preoperative diagnosis of rotator cuff tears and postoperative follow-up. Europ J Radiology. 1988;8(2):69–75. [PubMed] [Google Scholar]
- 17.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86(2):219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Prickett WD, Teefey SA, Galatz LM, Calfee RP, Middleton WD, Yamaguchi K. Accuracy of ultrasound imaging of the rotator cuff in shoulders that are painful postoperatively. J Bone Joint Surg Am. 2003;85(6):1084–1089. doi: 10.2106/00004623-200306000-00016. [DOI] [PubMed] [Google Scholar]
- 19.Crass JR, Craig EV, Feinberg SB. Ultrasonography of rotator cuff tears: a review of 500 diagnostic studies. J Clin Ultrasound. 1988;16(5):313–327. doi: 10.1002/jcu.1870160506. [DOI] [PubMed] [Google Scholar]
- 20.Mack LA, Nyberg DA, Matsen FR, 3rd, Kilcoyne RF, Harvey D. Sonography of the postoperative shoulder. Am J Roentgenol. 1988;150(5):1089–1093. doi: 10.2214/ajr.150.5.1089. [DOI] [PubMed] [Google Scholar]
- 21.Crass JR, Craig EV, Feinberg SB. Sonography of the postoperative rotator cuff. Am J Roentgenol. 1986;146(3):561–564. doi: 10.2214/ajr.146.3.561. [DOI] [PubMed] [Google Scholar]
- 22.Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural otcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005;21(11):1307–1316. doi: 10.1016/j.arthro.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 23.Gartsman GM, Khan M, Hammerman SM. Arthroscopic repair of full-thickness tears of the rotator cuff. J Bone Joint Surg Am. 1998;80(6):832–840. doi: 10.2106/00004623-199806000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Anderson K, Boothby M, Aschenbrener D, Holsbeeck MV. Outcome and structural integrity after arthroscopic rotator cuff repair using 2 rows of fixation: minimum 2-year follow-up. Am J Sports Med. 2006;34(12):1899–1905. doi: 10.1177/0363546506290187. [DOI] [PubMed] [Google Scholar]


