Abstract
Care for elderly patients undergoing orthopedic surgery, particularly for those requiring emergency surgery, needs to take into account an analysis of physical capacity and risks specific to elderly individuals, in an attempt to reduce the risks. Nevertheless, these remain high in this group. Despite the risks, procedures developed promptly have a positive effect on these patients’ evolution. Coordinated care, composed of teams of specialists within clinical medicine, geriatrics, orthopedics, anesthesiology and critical care, along with other healthcare professionals, may be highly beneficial for this group of patients.
Keywords: Aged, Orthopedic, Emergency Medicine
INTRODUCTION
Orthopedic surgery is becoming more frequent and more complex. The technical development of prostheses, anesthetic equipment and technology and perioperative controls, added to the age group changes among the population have been transforming something that was exceptional until a few years ago into routine practice: large-scale orthopedic surgery on elderly patients.
The particular preoperative clinical condition may vary according to the type of condition presented by the patient. Patients assessed in a consultation office or outpatient clinic in preparation for elective surgery, even involving large-scale procedures such as total hip or knee prostheses, cannot be compared with those who are attended in walk-in services, under conditions requiring emergency surgery following fracture or trauma.
Notwithstanding these differences, the major clinical factors of perioperative complications are approximately the same, and identifying and treating them is one of clinicians’ most important tasks1, 2. Care in identifying and controlling preexisting individual organic limitations and care regarding the possibilities of deep vein thrombosis, pulmonary embolism, cardiological complications, respiratory complications, indications for and risks of blood transfusion, infections, delirium and dementia should always accompany the clinical attention that is provided for elderly patients perioperativel3, 5.
Preexisting functional limitations
Progressive functional loss occurs in various organic systems and goes on accumulating over the years6, 5. Some of these changes are age-related and lead to specific perioperative risks, as can be seen in Table 1.
Table 1.
Physiological changes due to aging and their significance for perioperative complications.
| System | change | Significance |
|---|---|---|
| General |
|
|
| Skin |
|
|
| Cardiac | Fibrosis of sinus and conducting tissues Alteration of diastolic function
|
|
| Pulmonary | changes to ventilation mechanisms
|
|
| Renal |
|
|
| immune | Involution of thymus
|
↑ Risk of infection |
| Hepatic | ↓ Blood flow and microsomal oxidation | ↑ Drug half-life |
| Endocrine |
|
Overload hyperglycemia and glucose intolerance |
| Others | Hyperplasia of the prostate |
|
(Adapted from Francis J. Perioperative management of the older patient in principles of geriatric medicine and gerontology. In: Hazzard W, Bierman EL, Blass JP, Ettinger W Jr, Halter JB. editors. Geriatric Medicine & Gerontology. New York: McGraw-Hill; 1994).
Perioperative assessment
The preoperative assessment seeks to identify and quantify possible risk factors and to take measures that, if possible, will correct or prevent complications relating to the postoperative period. Perioperative care intensifies with increasing age, because of the severity of the surgical condition, presence of comorbidities and changes to elderly individuals’ functional state 2, 7.
Surgical risk: overall risk predictor
It is evident that surgery presents risks that become accentuated not only through the complexity of the surgical procedure, but also and especially through the patient’s clinical condition. This is more important among elderly patients, given the functional limitations that accompany the reduction of the organic reserve7, 8.
There is greater mortality during the first postoperative week. Deaths on the first day are more related to problems from the surgical procedure in itself, whereas those during the first week are more related to clinical complications from the intervention (embolism, infarction, pneumonia, etc). It can be inferred that most lethal complications, especially postoperatively among elderly patients, occur because of problems of a clinical nature. This makes it clear that adequate clinical support is essential in order to increase safety.
Overall assessment scales: the ASA scale
The surgical risk scale of the American Society of Anesthesiology (known by its abbreviation, ASA) was described in the 1960s and has changed little over the years. It continues to be one of the most used scales because of its practicality and sensitivity for predicting the overall risk of mortality, according to patients’ ages and functional status, independent of the type of procedure that will be performed2, 7, 8. The ASA classification and one of the risk tables relating to its scoring are presented in Table 2.
Table 2.
Risk scale of the American Society of Anesthesiology (ASA).
| ASA | ||||
|---|---|---|---|---|
| I Healthy individual, under 70 years of age | ||||
| II Mild systemic disease – without functional limitation or > 70 years | ||||
| III Severe systemic disease – defined functional limitation | ||||
| IV Incapacitating systemic disease that is a constant threat to life | ||||
| V Moribund – not expected to survive for 24 h with or without surgery | ||||
| VI Organ donor | ||||
| Age/Class | Class i | Class ii | Class iii | Class IV |
| 1 year | 4% | 4% | 27% | 43% |
| 1-30 years | 6% | 8% | 22% | 28% |
| 31-50 years | 2% | 11% | 25% | 37% |
| 51-70 years | 1% | 8% | 29% | 39% |
| » 70 years | - | 5% | 25% | 45% |
Cardiac risk scales
Most complications, particularly mortal complications during the postoperative period, are of cardiac origin. It is important to stratify this risk in isolation, in order to achieve support that is more differentiated and safer, and thus seek to minimize this risk. The commonest cardiac complications are myocardial infarction, decompensation relating to heart failure, arterial pressure abnormalities and arrhythmia9, 10.
The Detsky cardiac index, as modified by Eagle et al(8) and Mangano et al(11) with low-risk variables, is easy to apply and is fundamentally based on clinical history and electrocardiograms. It has been validated by the American College of Physicians (ACP)1, 7, 8 (Figure 1).
Figure 1.
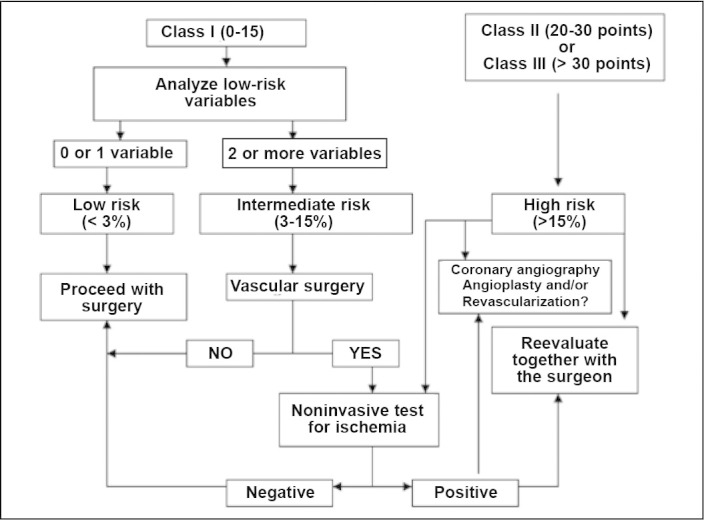
Assessment algorithm and procedure for evaluating surgical risk and guiding noninvasive testing (American College of Physicians).
An initial classification into classes I, II and III is made according to the sum of the points attributed to the items in Table 3. For patients in class I, the number of low-risk variables needs to be evaluated.
Table 3.
Modified Detsky Index.
| Condition | Score |
|---|---|
| Acute myocardial infarction within last six months | 10 points |
| Previous acute myocardial infarction, more than six months ago | 5 points |
| Angina class III | 10 points |
| Angina class IV | 20 points |
| Unstable angina within last three months | 10 points |
| Pulmonary edema within last seven days | 10 points |
| Previous pulmonary edema, more than seven days ago | 5 points |
| Severe aortic stenosis | 20 points |
| Non-sinusoidal rhythm or atrial extrasystole on preoperative electrocardiogram | 5 points |
| Five ventricular extrasystoles/min on any electrocardiogram before the operation | 5 points |
| Poor general condition (PO2 < 60 or PCO2 > 50, K < 3.0, bic < 20, U > 50, C > 3.0, chronic liver disease) | 5 points |
| Emergency surgery | 10 points |
| Age over 70 years | 5 points |
| Low-risk variables | |
| Age > 70 years | |
| History of chest angina | |
| Diabetes | |
| History of acute myocardial infarct | |
| History of congestive heart failure | |
| Ventricular ectopia | |
| Ischemic abnormalities of the ST segment on resting electrocardiogram | |
| Systemic Arterial hypertension with severe ventricular hypertrophy | |
| Note: Evaluate the number of variables present and apply to the algorithm below | |
| Class I | = 15 points |
| Class II | = 15-30 points |
| Class III | = 30 points or more |
Patients classified as class II or III are considered to be at high risk, and indications for surgery should be considered within this context, because the chance of complications is greater than 15%. If surgery is fundamental, patients should be stratified using cardiological examinations, which include myocardial scintigraphy (MIBI), stress echocardiogram with dobutamine and coronary angiography when indicated9, 10.
Patients in class I with 0-1 variables are considered to present low risk and are released for surgery without cardiological stratification. Patients with two or more variables are considered to present intermediate risk. They should be stratified in cases of vascular surgery, or released without additional examinations in cases of nonvascular surgery.
There is strong evidence for indication of beta-blocker use in high or intermediate-risk patients, or in those with coronary disease already established, in order to prevent the appearance of ischemic events during the postoperative period10, 12, 13, 14, 15.
Beta-blockers reduce morbidity and mortality when they are administered to high-risk patients(15). A target heart rate of 70 beats per minute is recommended(3).
Cardioselective beta-blockers should be chosen. The following drugs are recommended: atenolol, 50 to 100mg/day orally; bisoprolol, 5 to 10mg/day orally; atenolol, 5 to 10mg intravenously; and metoprolol, 5 to 10 mg intravenously. Oral administration is recommended before the operation, and parenteral use is recommended at the time of inducing anesthesia, intraoperatively and postoperatively for as long as the fasting period continues.
Adverse effects are rare and include the appearance of bradycardia and hypotension. They are worse in patients with perioperative heart rates of less than 60 beats/min. A recent study showed that high doses of beta-blockers and preventive use in high-risk patients increase mortality and the risks of stroke, septic shock and the complications from septicemia(16).
Perioperative circulatory problems angina pectoris
In assessing an anginous patient preoperatively, the characteristics of the angina, the patient’s degree of functional limitation and the efficacy of the anti-angina medication should be ascertained. The medication should be reassessed and, if it is not being efficient, it should be intensified before the surgery or reviewed at the time of proceeding with the surgery5, 13.
It should be taken into consideration that many patients (particularly diabetics, hypertensive individuals and those with peripheral vasculopathy) possibly have a condition of silent ischemia, an entity that increases in prevalence with advancing age. To assess the degree of coronary abnormality, it may be necessary, when possible, for the patients to undergo an ergo-metric test, myocardial scintigraphy at rest and with pharmacological stress (MIBI-dipyridamole), stress echocardiogram with dipyridamole or dobutamine and, possibly, coronary angiography.
Deep vein thrombosis (DVT) and pulmonary embolism (PTE)
To guide prophylaxis better, the physiological condition that predisposes patients to develop deep vein thrombosis (DVT) and pulmonary embolism (PTE) needs to be understood. Venous stasis, lesions of the intimal layer of vessels and states of hypercoagulability make up the physiopathological trio involved greater risk of DVT and PTE. The supine position of the surgical table, the anatomical positioning of the extremities, the effect of the anesthesia and the duration of the surgical procedure under anesthesia contribute towards venous stasis during the operation(17).
The scale for assessing the risk of DVT and PTE does not differ from what is normally used for younger patients. The points are summed according to the risk factors listed in Table 4. The scores are classified as low risk (≤ 1 point), moderate risk (2-4 points) and high risk (> 4 points). It can be seen that elderly people at the perioperative stage of orthopedic surgery or presenting fractures are always considered to be at high risk2, 17.
Table 4.
Risk of deep vein thrombosis (DVT) or pulmonary thromboembolism (PTE).
| One point/item | Two points/item | Four points/item |
|---|---|---|
| ✓≥ 40 years | ✓≥ 60 years | ✓Hip surgery |
| ✓ Smoker | ✓Neoplasia | ✓Hip surgery |
| ✓ Obesity | ✓Immobilization | ✓Knee surgery |
| ✓Estrogen or contraceptives | ✓Thrombophilia | ✓Prosthesis |
| ✓Pregnancy and puerperium | ✓Polycythemia | ✓Long-bone or multiple fractures |
| ✓Nephritic syndrome | ✓ Antecedents of DVT/PTE | ✓Multiple trauma |
| ✓Autoimmune disease | ✓AF of DVT/PTE | |
| ✓Leukemia | ✓ Complicated acute myocardial infarction | |
| ✓Uncomplicated acute myocardial infarction | ✓Ischemic stroke | |
| ✓Diabetes | ✓ Edema, varicose veins, ulcers and stasis of lower limbs | |
| ✓Infections | ✓ Congestive heart failure | |
| ✓Large-sized SO (< 6 m) | ✓Extensive burns | |
| ✓ Surgery ≤ 60 min | ✓ Antiphospholipid antibodies | |
| ✓ Surgery > 60 min |
In moderate-risk cases, the percentages are 2 to 8% for DVT and 1 to 8% for PTE. In high-risk cases, they are 10 to 20% for DVT and 5 to 10% for symptomatic PTE. The recommendations for the treatment are listed in Table 5. Drug prophylaxis should start 12 hours before the surgery. It is recommended that patients presenting bleeding or conditions with a high risk of bleeding should only start to receive drug prophylaxis after the operation, when the risk of hemorrhage ceases. Non-pharmacological prophylaxis measures such as elastic stockings and intermittent pneumatic compression should be started on admission to hospital and should be maintained intraoperatively and postoperatively.
Table 5.
Recommendations for DVT/PTE prophylaxis.
| Prophylaxis according to DVT/PTE risk calculation | ||
|---|---|---|
| low Risk | Moderate Risk | High Risk |
| Non-Pharmacological Measures: | Pharmacological Measures: | Pharmacological Measures: |
| Active movement of lower limbs | Enoxaparin 20 mg SC 1x/d | Enoxaparin 40 mg SC 1x/d |
| Early walking | Nadroparin 0.3 ml SC 1x/d | Nadroparin 0.6 ml SC 1x/d |
| Medium-compression elastic stockings up to the thighs, or | Dalteparin 2,500 UI SC 1x/d | Dalteparin 5,000 UI SC 1x/d |
| Intermittent pneumatic compression | Heparin 5,000 UI SC 2x/d | Heparin 5,000 UI SC 3x/d |
| Always in association with the non-pharmacological measures | Always in association with the non-pharmacological measures | |
The risk of bleeding is greater in patients with antecedents of coagulopathy (generally due to deficiencies of coagulation factors), low platelet counts or use of drugs that interfere with platelet aggregation. For this reason, use of medications that interfere with this function, such as aspirin, dipyridamole, ticlopidine and clopidogrel should be suspended for at least seven day before carrying out elective surgery(8).
Blood transfusion
Evaluation of the red series is very important among elderly people(18). Relatively small improvements in hematocrit and hemoglobin rates may bring dramatic improvements in elderly patients’ symptoms, thus emphasizing the importance of investigating and correcting their levels in the blood before the operation(5).
In preoperative assessments before elective surgery, hemoglobin levels lower than 11 g% in elderly patients deserve investigation and, if necessary, replacement. In any event, there seems to be a consensus that patients over 50 years of age or those with cardiopathy should never be sent for surgery with hemoglobin levels lower than 10 g%. With regard to the replacement method, supplying packed red blood cells during the procedure or just afterwards seems to be the most effective means.
Hemotherapy is frequently used in orthopedic surgery, either to prepare for the surgical procedure, or during or after it. This is because of the large quantities of blood that are lost due to bone trauma and the difficulties of achieving hemostasis in this tissue.
It is known that patients with anemia have a notably higher risk of surgical complications and death, which may reach 30% of the cases in which the hemoglobin level is lower than 6 g%. However, it is increasingly accepted that infusions of red blood cells leads to diminished immunity after the operation. It has been found that infection rates are higher among patients undergoing femoral neck surgery who received transfusions.
Greater tolerance regarding hemoglobin levels in non-coronary disease patients is recommended, but attentiveness must be maintained since elderly people may present silent ischemia. In coronary disease patients, hemoglobin levels greater than or equal to 11 g% at the time of starting the surgical procedure are desirable5, 8.
Renal and urological abnormalities
Elderly individuals present greater renal risk because of the progressive decrease in clearance. Comorbidities, especially diabetes, hypertension and heart failure, worsen the risk of kidney failure after the operation. Requesting routine tests such as urea, creatinine, urine I with culturing and creatinine clearance, when indicated, is recommended.
One extremely important calculation in this situation may be the estimated creatinine clearance, as proposed by Cockcroft and Gault (Figure 2). Knowledge of simple variables such as the patient’s age, sex and serum creatinine level enables good assessment of creatinine clearance and thus enables prevention of the iatrogenic complications that are frequently connected with surgical interventions, especially among frail patients(3).
Figure 2.
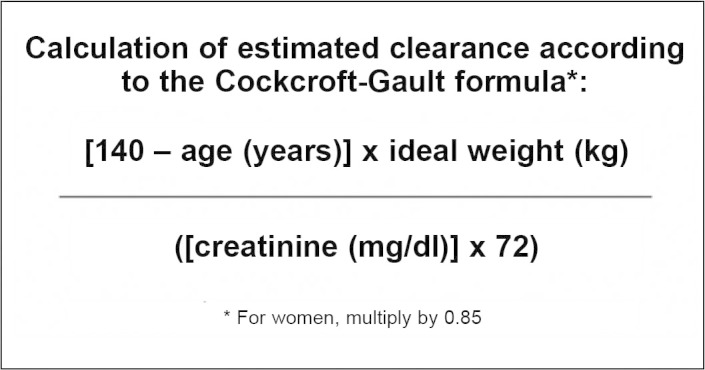
Cockcroft-Gault formula.
Unsurprisingly, iatrogenic complications are among the biggest causes of death among elderly patients(8). Potentially nephrotoxic medications such as aminoglycosides or non-hormonal anti-inflammatory agents should be avoided, as should iodide and gadolinium contrast media. Hydration is fundamental after the operation, until oral ingestion has been well established. Support measures such as prior use of acetylcysteine at a dose of 1.2 grams/day preceding contrast examinations may be beneficial2, 8. Another prudent measure among frail patients with serum creatinine levels greater than 2 mg% is to keep in contact with the hospital’s nephrology, in a state of “armed alert” for possible dialytic intervention if necessary.
Among elderly individuals, cases of prostatic hypertrophy and/or the need to force the bladder are common, with difficulty in urinating after the operation. It is not uncommon for an enlarged bladder to appear, which gives rise to the need to pass a probe into the bladder to relieve and/or delay the condition. This situation may be particularly common in patients who have received regional anesthesia (peridural or spinal anesthesia) using morphine, which may lead to transitory urine retention.
Elderly women may present urinary incontinence and attention needs to be given to changing nappies/diapers and/or passing a probe into the bladder, with the aim avoiding the appearance of blisters and ulcers of sacral decubitus. Use of a delay probe is also recommended for patients whose hydric balance needs to be brought under control. Collection of urine type I and urine culturing is also recommended for patients who will undergo arthroplasty because of the risk of infection in the prosthesis.
Pulmonary abnormalities
Aging is associated with a series of changes that may place elderly individuals in situations of greater risk of perioperative pulmonary complications. Changes to deglutition increase the risk of oropharyngeal dysphagia; diminution of the cough reflex implies less protection for the airways; changes to connective tissue cause alveolar deformities similar to those found in emphysema; kyphoscoliosis and calcification of the costal cartilage cause lower compliance of the chest cavity; and sarcopenia results in lower performance of the intercostal muscles and diaphragm6, 19, 20.
The main pulmonary complications found after the operation are atelectasis, bronchospasm, tracheobronchial infection, pneumonia, exacerbation of chronic obstructive pulmonary disease (COPD), respiratory failure and prolonged mechanical ventilation. Occurrences of these complications are closely linked to the existence of risk factors relating to the patient and to the procedure. The main factors encountered were ASA > 2, chest X-ray showing abnormalities, age > 70 years, congestive heart failure, albumin < 3.5 mg/dl, aortic surgery, chest surgery, upper abdominal surgery and prolonged surgery19, 20, 21.
Patients with COPD should be treated aggressively in order to obtain the best control possible. All patients with symptomatic COPD should receive ipratropium or tiotropium every day during the perioperative period. Inhaled beta agonists should be used as needed to control the symptoms. Patients with persistent wheezing or functional limitation despite optimized bronchodilation therapy should receive systemic corticosteroid6, 19, 20.
All patients should undergo respiratory and motor physiotherapy starting from when they are admitted to hospital, with the aim of preventing respiratory complications, which increase mortality and prolong hospitalization8, 20, 21 (Table 6).
Table 6.
Torrington and Henderson scale for pulmonary risk classification.
| Parameter | Score | ||
|---|---|---|---|
| FCV < 50% of prediction | 1 | ||
| FEV1/FCV: 65-75% | 1 | ||
| FEV1/FCV: 50-64% | 2 | ||
| FEV1/FCV: < 50% | 3 | ||
| Age > 65 years | 1 | ||
| Weight > 150% of the ideal | 1 | ||
| Upper abdominal or thoracic surgery | 2 | ||
| Smoking | 1 | ||
| Symptoms (coughing, dyspnea or secretion) | 1 | ||
| History of pulmonary disease | 1 | ||
| Risk classification | Points | Pulmonary complication | Mortality |
| Low | 0 -3 | 6 % | 2% |
| Moderate | 4 -6 | 23% | 6% |
| High | ≥ 7 | 35% | 12% |
Delirium during the perioperative period
Delirium is a frequent complication during the postoperative period18, 22. Approximately 30% of hospitalized elderly patients develop conditions of delirium. The main clinical manifestations are:
-
•
Disorganized and incoherent thinking. Difficulty in understanding facts and recognizing situations
-
•
Altered perception in 40% (illusions and visual and auditory hallucinations)
-
•
Persecution delirium in 50%
-
•
Impaired fixation and evocation memory
-
•
Diminished attention
-
•
Psychomotor activity (hyper or hypo)
According to the DSM-IV, delirium is characterized by altered consciousness, difficulty in focusing attention, cognitive impairment and disorganized thinking, and it may be associated with perception disorders. It develops over a short space of time (from hours to days), with a tendency to fluctuate over the course of the day. The main predisposing factors are advanced age, sensory deficit and diseases of the central nervous system such as dementia, stroke and Parkinson disease18, 22, 23.
-
•
There are multiple triggering factors and they are listed in the following:
-
•
Hydroelectrolytic disorders (dehydration, hypo/hypernatremia or hypercalcemia);
-
•
Infections (urinary, respiratory, skin or soft-tissue);
-
•
Toxicity due to medications;
-
•
Metabolic changes (hypoglycemia, hypothyroidism, uremia or liver failure);
-
•
Low cardiac output (shock, heart failure or myocardial infarction);
-
•
Hypoxemia.
Environmental factors are important triggering factors. The main ones are:
-
•
Loss of time and space references (lack of natural lighting, calendar or clock);
-
•
Immobility (including use of physical containment);
-
•
Use of bladder probe;
-
•
Sleep deprivation;
-
•
Frequent changing of bedroom;
-
•
Being in an intensive care unit or chronic treatment unit.
Toxicity due to medications occurs in approximately 30% of the cases of delirium, and the main drug classes involved are antidepressants, antihistamines, antiparkinsonians, analgesics, anesthetics, sedatives, hypnotics and quinolone antibiotics. On the other hand, abrupt withdrawal of certain agents such as benzodiazepines induces abstinence and consequently delirium10, 23.
Furlanetto and Garcez Leme studied 103 elderly patients hospitalized with hip fractures who presented delirium diagnosed using the “confusion assessment method” (CAM), and they observed that delirium is a frequent complication among elderly people hospitalized with femoral fractures. It is associated with cognitive and functional deficits and increases the duration of hospital stay and the mortality rate(18).
The treatment for delirium is based on two simultaneous objectives: management of behavioral alterations; and actively seeking and treating triggering factors. Haloperidol at low doses (0.5 to 1.0 mg orally, intravenously or intramuscularly) may be used to control agitation or psychotic symptoms, but on rare occasions, it may induce sedation and hypotension. Its action starts 30 to 60 minutes after parenteral administration(23).
Strategies for preventing delirium, through characterizing and minimizing the risk factors are effective(18). It is recommended that oxygen therapy (2 l/min) should be used routinely over the first 48 hours after the operation, even when the individual does not present signs of dyspnea or respiratory decompensation(24). Atypical neuroleptics such as risperidone and olanzapine present fewer adverse effects and have shown efficacy similar to that of haloperidol in retrospective studies, but have not been studies over the perioperative period(23).
Nutritional abnormalities
It is known that malnutrition is a serious problem among elderly patients who need to undergo arthroplasty, particularly when secondary to hip fracture. The poor nutritional condition shown by this patient profile may stem from very many factors, including: changes to gastrointestinal physiology, medications, chronic clinical conditions, diminished appetite, diminished physical activity, diminished lean mass in the organism, chronic liver and kidney disease, cancer and surgery25, 26.
The nutritional status of elderly patients influences postoperative recovery, and those in a good nutritional condition have better and faster clinical rehabilitation(10). Protein deficiency causes increased numbers of infections, bed sores, muscle weakness, poor respiratory function, myocardial hypertrophy and death(26). Low albumin levels are associated with high morbidity and mortality, long hospital stays and readmissions.
It is recommended that the following biochemical indicators of malnutrition should be used: anemia; vitamin deficiency; low levels of pre-albumin, albumin, transferrin and cholesterol; and low lymphocyte counts. Three of these variables present proven clinical relevance as prognostic factors: albumin > 3.5 mg/dl, lymphocytes > 1800 mm3 and involuntary weight loss < 10%. Preoperative serum albumin is a strong predictor of complications within the first 30 postoperative days(7).
Preoperative nutritional support is beneficial in these patients, and it significantly reduces mortality and surgical complications. Use of orally administered enteral supplements is recommended, and this may contribute towards improving the protein-energy supply8, 27.
Infections
Infections are among the main causes of death among the elderly population. Early diagnosis of infections is essential, given that morbidity and mortality have significant roles in such conditions. The atypical presentation of some manifestations of infections constitutes a further challenge. It is known that only 60% of elderly individuals with severe infectious conditions develop leukocytosis; also in this regard, the response to fever may be weak, and temperatures greater than 38.3°C many indicate severe infection. On the other hand, cognitive manifestations may be present in 50% of elderly individuals with infections, particularly cases of delirium. Pneumonia, urinary infections and skin infections occur frequently.
In cases of infection associated with orthopedic interventions, the complications are given additional potency because of the difficulty of achieving antibiotic access to bone tissue and the chronic nature of such complications. These may require new and repeated interventions, with the removal of prosthesis or synthesis materials.
It is essential in orthopedic surgery to have an accurate assessment of possible foci before the operation, including foci in the skin, teeth, respiratory tract and urinary tract, given the greater incidence of infection of the surgical site in patients who already present other foci.
Blood glucose control in diabetic patients is also important. The risk ratio for transoperative infection is greater than 3 in patients who present fasting blood glucose levels higher than 300 mg%4, 5.
It is essential to be attentive regarding the appropriate antibiotic prophylaxis as recommended by the hospital infection control committee, along with prophylaxis for bacterial endocarditis and treatment for preexisting infections, before proceeding with the surgery.
Antibiotic prophylaxis is applied universally to patients undergoing implantation of prostheses or synthesis material. It currently consists of administration of second-generation cephalosporins over the 24-hour period encompassing the operation. Special measures need to be structured for cases of trauma, particularly those that incorporate exposure of soft tissues, as is the case of exposed fractures.
Waiting time for the intervention
The multiple coexisting conditions and frailness observed among elderly patients may often lead the surgical and anesthetic team to postpone the surgical intervention(4).
Controlling the risk factors and scheduling the intervention under the best technical conditions possible are highly desirable for reducing the risk among these patients. However, in cases of acute conditions such as hip fractures in frail patients, this type of approach is often not possible or even desirable.
Suspension or postponement of an emergency surgical intervention does not eliminate from the patient the risk of the intervention but, rather, it incorporates into this risk the risk inherent to non-intervention or to the postponement itself. Delaying the surgical intervention by more than 48 hours in cases of patients with hip fractures increases the risk of complications and corresponds to a significant decrease in one-year survival. The importance of rapidly assessing and preparing these patients is emphasized, in order to avoid the risks inherent to delays in the intervention. Such risks include, among other consequences of prolonged immobility, muscle atrophy, bed sores, osteopenia, pneumonia, urinary sepsis, pulmonary thromboembolism, embolization of fat and institutionalization.
Coordinated interprofessional attention
Given the complexities of clinical follow-up for elderly patients undergoing orthopedic treatment, many clinics over the last 50 years have envisaged specific relationship structures coordinated between orthopedists and clinicians, especially geriatricians, with the aim of providing greater safety and speed for these high-risk patients4, 5.
As early as 1957, in the United Kingdom, the Hastings Clinic developed an Orthogeriatric Service run by Professors Michael Devas (orthopedist) and Bob Irvine (geriatrician). The benefit from this association became well known and, among its guidelines, there are principles that continue to be fundamental in caring for elderly individuals with orthopedic conditions, such as: the importance of early intervention, especially for the frailest patients; the importance of early rehabilitation; and the importance of interprofessional attention, among other principles. There is evidence indicating that the only intervention presenting statistical significance in terms of mortality, for elderly individuals with hip fractures, is differentiated geriatric attention that includes multiprofessional participation.
Satomi E, Sitta MC, Machado NA and Garcez-Leme LE observed that the majority of elderly individuals hospitalized due to fractures did not receive adequate prescriptions for treating osteoporosis and preventing new fractures after discharge from hospital. This serves as an alert regarding the need for clinicians to review prescriptions at the time of orthopedic discharge, in order to ensure that catastrophic events are prevented(28).
FINAL REMARKS
The care provided for elderly patients undergoing orthopedic surgery, particularly for those requiring emergency surgery, needs to take into account the assessment of elderly individuals’ physical capacity and specific risks, in an attempt to reduce the risks, which remain high in this group.
Despite the risks, procedures implemented promptly have a positive effect on these patients’ evolution. Coordinated care provision between the clinical/geriatric team, the orthopedic team, anesthetists, intensive care specialists and other professionals may be highly beneficial in this group of patients.
Footnotes
Work performed in the Medical Investigation Laboratory for the Musculoskeletal System (LIM41), Department of Orthopedics and Traumatology, University of São Paulo Medical School.
The authors declare that there was no conflict of interest in conducting this work
REFERENCES
- 1.Machado FS, Martins MA, Caramelli B. Perioperatório: procedimentos clínicos. Sarvier; São Paulo: 2004. [Google Scholar]
- 2.Pires PWA, Branco PD, Sitta MC, cirúrgico idoso O doente, Gama-Rodrigues JJ, Machado MC, Rasslan S. organizadores Clínica cirúrgica: Manole. 2008:2060–2074. [Google Scholar]
- 3.Pires PW, Branco PD, Sitta MC, cirúrgico idoso O doente, Utiyama EM, Otoch JP, Rasslan S, Birolini D. organizadores Propedêutica cirúrgica. 2a. ed. Manole; Barueri: 2007. pp. 249–263. [Google Scholar]
- 4.Polanczyk CA, Marcantonio E, Goldman L, Rohde LE, Orav J, Mangione CM. Impact of age on perioperative complications and length of stay in patients undergoing noncardiac surgery Ann Intern Med. 2001;134(8):637–643. doi: 10.7326/0003-4819-134-8-200104170-00008. [DOI] [PubMed] [Google Scholar]
- 5.Williams SL, Jones PB, Pofahl WE. Preoperative Management of the Older Patient. Clin Geriatr. 2006;4(6):24–28. [Google Scholar]
- 6.Smetana GW, Lawrence VA, Cornell JE. American College of Physicians Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med. 2006;144(8):581–595. doi: 10.7326/0003-4819-144-8-200604180-00009. [DOI] [PubMed] [Google Scholar]
- 7.Machado AN, Sitta Mdo C, Jacob Filho W, Garcez-Leme LE. Prognostic factors for mortality among patients above the 6th decade undergoing non-cardiac surgery: cares–clinical assessment and research in elderly surgical patients. Clinics (Sao Paulo) 2008;63(2):151–156. doi: 10.1590/s1807-59322008000200001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sitta MC, Machado AN, Apolinário D, Garcez-Leme LE. Avaliação perioperatória do idoso. Geriatr Gerontol. 2008;2(2):86–94. [Google Scholar]
- 9.Eagle KA, Brundage BH, Chaitman BR, Ewy GA, Fleisher LA, Hertzer NR. Guidelines for perioperative cardiovascular evaluation for noncardiac surgery. Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Perioperative Cardiovascular Evaluation for Noncardiac Surgery) J Am Coll Cardiol. 1996;27(4):910–948. doi: 10.1016/0735-1097(95)99999-x. [DOI] [PubMed] [Google Scholar]
- 10.Goldman L. Evidence-based perioperative risk reduction. Am J Med. 2003;114(9):763–764. doi: 10.1016/s0002-9343(03)00286-9. [DOI] [PubMed] [Google Scholar]
- 11.Mangano DT, Wong MG, London MJ, Tubau JF, Rapp JA. Perioperative myocardial ischemia in patients undergoing noncardiac surgery–II: Incidence and severity during the 1st week after surgery. The Study of Perioperative Ischemia (SPI) Research Group J Am Coll Cardiol. 1991;17(4):851–857. doi: 10.1016/0735-1097(91)90864-6. [DOI] [PubMed] [Google Scholar]
- 12.Auerbach AD, Goldman L. beta-Blockers and reduction of cardiac events in noncardiac surgery: scientific review. JAMA. 2002;287(11):1435–1444. doi: 10.1001/jama.287.11.1435. [DOI] [PubMed] [Google Scholar]
- 13.Devereaux PJ, Beattie WS, Choi PT, Badner NH, Guyatt GH, Villar JC. How strong is the evidence for the use of perioperative beta blockers in non-cardiac surgery? Systematic review and meta-analysis of randomised controlled trials. BMJ. 2005;331(7512):313–321. doi: 10.1136/bmj.38503.623646.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lindenauer PK, Pekow P, Wang K, Mamidi DK, Gutierrez B, Benjamin EM. Perioperative beta-blocker therapy and mortality after major noncardiac surgery. N Engl J Med. 2005;353(4):349–361. doi: 10.1056/NEJMoa041895. [DOI] [PubMed] [Google Scholar]
- 15.Redelmeier D, Scales D, Kopp A. Beta blockers for elective surgery in elderly patients: population based, retrospective cohort study. BMJ. 2005;331(7522):932. doi: 10.1136/bmj.38603.746944.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Devereaux PJ, Yang H, Yusuf S, Guyatt G, Leslie K, Villar JC. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008;371(9627):1839–1847. doi: 10.1016/S0140-6736(08)60601-7. [DOI] [PubMed] [Google Scholar]
- 17.Kearon C, Hirsh J. Management of anticoagulation before and after elective surgery. N Engl J Med. 1997;336(21):1506–1511. doi: 10.1056/NEJM199705223362107. [DOI] [PubMed] [Google Scholar]
- 18.Furlaneto ME, Garcez-Leme LE. Impact of delirium on mortality and cognitive and functional performance among elderly people with femoral fractures. Clinics (Sao Paulo) 2007;62(5):545–552. doi: 10.1590/s1807-59322007000500003. [DOI] [PubMed] [Google Scholar]
- 19.Chan ED, Welsh CH. Geriatric respiratory medicine. Chest. 1999;114(6):1704–1733. doi: 10.1378/chest.114.6.1704. [DOI] [PubMed] [Google Scholar]
- 20.Smetana GW. Preoperative pulmonary evaluation. N Engl J Med. 1999;340(12):937–944. doi: 10.1056/NEJM199903253401207. [DOI] [PubMed] [Google Scholar]
- 21.Arozullah AM, Daley J, Henderson WG, Khuri SF. Multifactorial risk index for predicting postoperative respiratory failure in men after major noncardiac surgery. The National Veterans Administration Surgical Quality Improvement Program. Ann Surg. 2000;232(2):242–253. doi: 10.1097/00000658-200008000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157. doi: 10.1056/NEJMra052321. [DOI] [PubMed] [Google Scholar]
- 23.Prado LK, Machado AN, Curiatti JAE, Sitta MC Delirium. RBM Rev Bras Med. 2008;65(1/2):28–33. [Google Scholar]
- 24.Aakerlund LP, Rosenberg J. Postoperative delirium: treatment with supplementary oxygen. Br J Anaesth. 1994;72(3):286–290. doi: 10.1093/bja/72.3.286. [DOI] [PubMed] [Google Scholar]
- 25.Howard L, Ashley C. Nutrition in the perioperative patient. Annu Rev Nutr. 2003;23:263–282. doi: 10.1146/annurev.nutr.23.011702.073353. [DOI] [PubMed] [Google Scholar]
- 26.Eneroth M, Olsson UB, Thorngren KG. Nutritional supplementation decreases hip fracture-related complications. Clin Orthop Relat Res. 2006;451:212–217. doi: 10.1097/01.blo.0000224054.86625.06. [DOI] [PubMed] [Google Scholar]
- 27.Duncan DG, Beck SJ, Hood K, Johansen A. Using dietetic assistants to improve the outcome of hip fracture: a randomised controlled trial of nutritional support in an acute trauma ward. Age Ageing. 2006;35(2):148–153. doi: 10.1093/ageing/afj011. [DOI] [PubMed] [Google Scholar]
- 28.Satomi E, Sitta MC, Machado NA, Garcez-Leme LE. Identification and treatment of osteoporosis among elderly patients with hip fractures. Clinics. 2009;64(12):1201–1204. doi: 10.1590/S1807-59322009001200010. [DOI] [PMC free article] [PubMed] [Google Scholar]


