Abstract
We present a case of Guyon's canal syndrome caused by a synovial cyst within the left wrist of a 48-year-old female patient. The patient presented pain and paresthesia in the region of the ulnar nerve, with loss of muscle strength and left-hand deformity. Electroneuromyography showed a compression of the ulnar nerve at the wrist level. Surgical decompression of the nerve at Guyon's canal with resection of the cyst was performed. After the surgery, the patient presented an improvement in the pain and paresthesia, as well as an increase in muscle trophism and correction of the deformity.
Keywords: Ulnar Nerve Compression Syndromes, Synovial Cyst, Nerve Compression, Ulnar Nerve
INTRODUCTION
The ulnar nerve can be compressed in some parts of its path, including the cubital canal, arcade of Struthers and Guyon's canal(1). Compression at Guyon's canal is considered rare in the literature. There are various causes of compression at Guyon's canal, such as trauma, tumors, thrombosis of the ulnar artery or cysts. The increased pressure inside the canal causes a decrease in the conduction velocity of nerve stimuli, thereby generating pain, paresthesia and muscle weakness.
Synovial cysts may occur in any joint, but they are most frequent in the wrist, on its dorsal face, and they can function as a compressive factor in osteofibrous tunnels.
In this study, we present the description of a case of Guyon's canal syndrome caused by a synovial cyst in the left wrist of a 48-year-old female patient.
CASE REPORT
The patient was a 48-year-old right-handed nonwhite woman who worked in her home, with a report of pain in the hypothenar region of the left hand that had started insidiously and had evolved for four months. She also presented paresthesia on the path of the ulnar nerve and a strength deficit in her left hand. The pain was constant, of medium intensity, with worsening upon mobilization of the left thumb. She said that she had not suffered any local trauma of any type, or previous lesions to the wrist.
Upon physical examination (Figure 1), she presented hypotrophy of the intrinsic musculature of the hand and hypothenar eminence, and cubital ulnar claw on the fourth and fifth fingers. She showed difficulty in moving her hand, especially the fourth and fifth fingers, with incapacity to extend these fingers. There were no other evident abnormalities. Upon palpation, she presented diminished sensitivity along the little finger and the ulnar face of the ring finger. The sensitivity of the dorsum of the hand was preserved. The radial and ulnar pulses were palpable, with good tissue perfusion in the hand, and the Allen test was negative. In the neurological examination, she presented pain on finger percussion (Tinel) along the path of the ulnar nerve, which started at the wrist and went towards the fourth and fifth fingers.
Figure 1.

Appearance of the patient's left hand before the operation. Note the hypotrophy of the hypothenar region and interosseous musculature, along with the claw deformity of the fourth and fifth fingers. To the left: the markings for the surgical incision in the volar region.
The radiographic examination did not show any anatomical abnormalities, and electroneuromyography showed motor, axonal and distal (wrist region, in Guyon's canal) neuropathy of the left ulnar nerve.
The patient underwent surgical exploration of Guyon's canal by means of a 6 cm zigzag incision in the volar-ulnar region of the left wrist and hand, under an anesthetic block of the brachial plexus, with the use of a pneumatic tourniquet. The exploration was deepened carefully in layers, and it was observed that the compression was caused by a synovial cyst of around 5 mm x 12 mm, between the hook of the hamate and the pisiform (Figures 2 and 3). The cyst was resected, along with the neurolysis in the canal, and the skin was sutured using nylon thread after reviewing the hemostasis. The patient was thus diagnosed as presenting type I compression (motor and sensory deficit).
Figure 2.
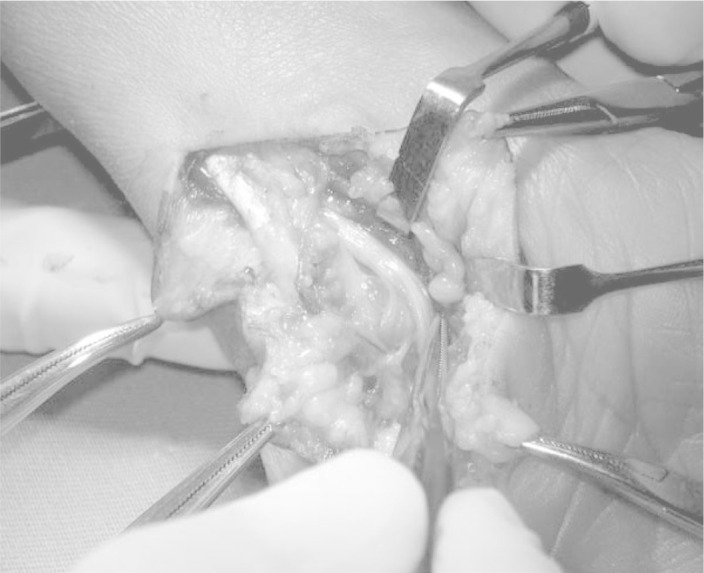
View of the ulnar nerve on its path, with the synovial cyst protruding in its floor.
Figure 3.
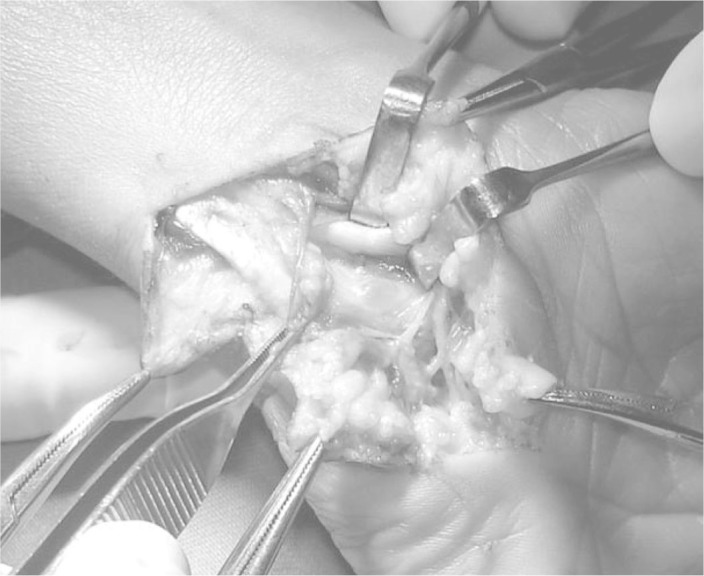
View of the synovial cyst in Guyon's canal, after separation of the ulnar nerve radially.
The patient evolved with pain relief and improved sensitivity, as well as progressive improvement of the hypotrophy of the musculature and increased muscle strength. She is currently using an orthosis to correct the cubital claw (Figure 4) and is undergoing physiotherapeutic rehabilitation.
Figure 4.

The orthosis for correcting the cubital claw, positioned on the patient's hand. Note the flexion of the metacarpophalangeal joints of the fourth and fifth fingers and the adduction of the fifth finger.
After 14 months of postoperative follow-up, the patient only presents difficulty in abducting the fifth finger of the left hand. She has completely recovered this movement in the other fingers (Figure 5).
Figure 5.

Left hand of the patient 14 months after the surgery. Note the diminution of the hypotrophy of the intrinsic musculature and the recovery of the movement of the fingers, with the exception of the fifth finger.
The orthosis for correction of the cubital claw, which is currently accepted as the best type of conservative treatment for this deformity, is being used full-time, with removal only for physiotherapy and for personal hygiene.
DISCUSSION
The ulnar tunnel described by the French urologist Guyon in 1861Del Pozo and Patel, 2009, Kurtz et al., 2008, Mortazavi et al., 2010 is an oblique semi-rigid canalDel Pozo and Patel, 2009, Mortazavi et al., 2010, Frommelt, 2006 with a bone floor and fibrous roof. Its limits are the pisiform proximally, the hook of the hamate distally and medially, and the volar carpal ligament laterally, together with the tendon insertion of the ulnar flexor of the carpus anteriorly and the pisohamate ligament and tendon of the short palmar muscle posteriorlyDel Pozo and Patel, 2009, Frommelt, 2006, Mangram et al., 1999, Cabrita et al., 2007.
The ulnar nerve originates in the nerve roots of C8 and T1 and it is the thickest branch of the medial fascicle of the brachial plexus. Around 6 to 8 cm proximally to the wrist, it sends out a dorsal cutaneous branch to the hand(3). On its path, it crosses the retinaculum of the flexors and Guyon's canal, and this is a site of possible compressionKurtz et al., 2008, Frommelt, 2006. The nerve is accompanied by the ulnar artery when it penetrates Guyon's canalMortazavi et al., 2010, Frommelt, 2006, Mangram et al., 1999, Cabrita et al., 2007, Estes et al., 2010 and, in this region, it divides into superficial and deep branches. The superficial branch is sensory and innervates the little finger and the ulnar edge of the ring finger, while the deep branch is purely motor and innervates the abductor, opponens and short flexor muscles of the little fingerDel Pozo and Patel, 2009, Frommelt, 2006. In the proximal segment of the palmar region, this branch innervates the third and fourth lumbrical muscles and also all of the interosseous muscles. The terminal part innervates the adductor of the thumb and the deep head of the short flexor of the thumbDel Pozo and Patel, 2009, Kurtz et al., 2008, Frommelt, 2006.
Several factors can be correlated as the causes of compression in Guyon's canal(2-4,7,8). These promote increased pressure inside the structures of the canal, thus causing delays in conducting stimuliMortazavi et al., 2010, Rudelli et al., 2008, Kurd et al., 2010. They are divided into three types: compression with sensory and motor deficit (type I); compression of the deep branch alone, with motor functional changes alone (type II); and compression of the surface branch alone, with sensory deficit without motor impairment (type III)Del Pozo and Patel, 2009, Kurtz et al., 2008, Frommelt, 2006, Whang and Wang, 2003.
Synovial cysts are tumor bodies of unknown etiology that are most commonly located on the dorsal face of the wristMortazavi et al., 2010, Frommelt, 2006, Vaccaro et al., 2002. Compression of the ulnar nerve caused by a cyst is a rare event in the medical literature(4).
The clinical condition varies according to the time elapsed since the start of the symptoms, the magnitude and level of the compression. The manifestations can go from pain and paresthesia(2-5,8) to hypotrophy and significant loss of muscle strength(4), with significant deformities of the hand that are often irreversibleAlbrektsson and Johanson, 2001, Bauer and Muschler, 2000. One of these, claw hand, can occur as a consequence of nerve compressions(14). The wrist is fixed in palmar flexion, the metacarpophalangeal joints in hyperextension and the interphalangeal joints in flexionAlbrektsson and Johanson, 2001, Bauer and Muschler, 2000.
The diagnosis is based on taking a detailed history, making a detailed clinical examination and using appropriate complementary examinations(8). Electroneuromyography is the neurological examination of choice for locating the compressionKurtz et al., 2008, Frommelt, 2006. Ultrasound and magnetic resonance imaging also assist in locating the cystMangram et al., 1999, Albrektsson and Johanson, 2001, Bauer and Muschler, 2000, Tomford, 1995. It is emphasized that an early diagnosis for the compressive syndrome is important for enabling a better postoperative prognosisFrommelt, 2006, Tomford, 1995.
The treatment is usually surgical, with decompression of the nerve inside the canal by means of a volar access and careful explorationKurtz et al., 2008, Mortazavi et al., 2010, Frommelt, 2006.
The differential diagnosis should be done in relation to bone, tendon, ligament and vascular lesionsMortazavi et al., 2010, Estes et al., 2010.
In the case presented here, the patient presented improvement of her pain and paresthesia, improvement of the muscle trophism and correction of the ulnar claw. The latter deformity should be treated early on with the use of orthoses(13), combined with passive movement of the limb, and the orthosis should be used until complete recovery has been achieved, or until the expectations for recovery are abandoned(14).
This is a rare event in the literatureMortazavi et al., 2010, Estes et al., 2010, and early surgical treatment leads to a better esthetic and functional result for the patientMangram et al., 1999, Bauer and Muschler, 2000.
Footnotes
Work performed at the Orthopedics and Traumatology Service, Hospital Mater Dei, Belo Horizonte, MG, Brazil.
REFERENCES
- Mattar Júnior R. Síndromes compressivas do membro superior. In: Hernandez AJ, editor. Ortopedia do adulto. Revinter; Rio de Janeiro: 2004. pp. 83–97. [Google Scholar]
- Leite NM, Albertoni WM, Leite VM. Compressão isolada do ramo profundo do nervo ulnal por variação da anatomia. Rev Bras Ortop. 1993;28(7):491–495. [Google Scholar]
- Shea JD, McClain EJ. Ulnar-nerve compression syndromes at end below the wrist. J Bone Joint Surg Am. 1969;51(6):1095–1103. [PubMed] [Google Scholar]
- Dupont C, Cloutier GE, Prévost Y, Dion MA. Ulnar-tunnel syndrome at the wrist: a report of four cases of ulnar-nerve compression at the wrist. J Bone Joint Surg Am. 1965;47:757–761. [PubMed] [Google Scholar]
- Severo A, Lech O, Silva LE, Ayzemberg H. Síndrome do canal de Guyon por cisto sinovial: relato de caso. Rev Bras Ortop. 2003;38(7):416–420. [Google Scholar]
- Inaparthy PK, Anwar F, Botchu R, Jähnich H, Katchburian MV. Compression of the deep branch of the ulnar nerve in Guyon's canal by a ganglion: two cases. Arch Orthop Trauma Surg. 2008;128(7):641–643. doi: 10.1007/s00402-008-0636-4. [DOI] [PubMed] [Google Scholar]
- Moraes EA, Pardini Júnior AG. Lipofibroma (hamartoma lipofibromatoso) dos nervos mediano e ulnal. Rev Bras Ortop. 1995;30(4):201–206. [Google Scholar]
- Shin AY, Deitch MA, Sachar K, Boyer MI. Ulnar-sided wrist pain: diagnosis and treatment. Instr Course Lect. 2005;54:115–128. [PubMed] [Google Scholar]
- Gelberman RH, Eaton R, Urbaniak JR. Peripheral nerve compression. Instr Course Lect. 1994;43:31–53. [PubMed] [Google Scholar]
- Hargens AR, Romine JS, Sipe JC, Evans KL, Mubarak SJ, Akeson WH. Peripheral nerve-conduction block by high muscle-compartment pressure. J Bone Joint Surg Am. 1979;61(2):192–200. [PubMed] [Google Scholar]
- Duggal A, Anastakis DJ, Salonen D, Becker E. Compression of the deep palmar branch of the ulnar nerve by a ganglion: a case report. Hand (N Y) 2006;1(2):98–101. doi: 10.1007/s11552-006-9008-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahra ME, Bucchieri JS. Ganglion cysts and other tumor related conditions of the hand and wrist. Hand Clin. 2004;20(3):249–260. doi: 10.1016/j.hcl.2004.03.015. [DOI] [PubMed] [Google Scholar]
- Neviaser JS. Splint for correction of claw-hand. J Bone Joint Surg Am. 1993;12:440–443. [Google Scholar]
- Pruce AM. Splint to correct deformity resulting from injury to ulnar nerve. J Bone Joint Surg Am. 1946;28:397. [PubMed] [Google Scholar]
- Boursinos LA, Dimitriou CG. Ulnar nerve compression in the cubital tunnel by an epineural ganglion: a case report. Hand (N Y) 2007;2(1):12–15. doi: 10.1007/s11552-006-9013-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


