Abstract
Objective: To analyze whether the Bernageau radiographic view is adequate for studying the anterior glenoid rim and to determine the distance between the posterior and anterior glenoid rims. Methods: Fifty patients (31 males) with a mean age of 34 years were evaluated by positioning their arm at 160° forward flexion and body at 70° to the x-ray chassis, while positioning the x-ray tube at 30° craniocaudally, centered on the scapula spine. Three of the authors measured the distance between the posterior and anterior glenoid rim three times. The variability and reproducibility of this distance were studied. Three shoulder surgeons performed a subjective evaluation by answering whether it was possible to evaluate the anterior glenoid rim in the view studied. Results: The mean distance was 24.48 mm ± 0.332 mm (left) and 24.82 mm ± 0.316 mm (right). The Anderson-Darling test showed that the measurements had normal distribution, and Pearson's correlation showed significant reproducibility (P < 0.01). The first observer found that 67% of the x-ray images were suitable for evaluating the anterior glenoid rim. The second found that 81% were suitable and the third, 78%. The kappa coefficient showed that the second and third observers had substantial agreement of opinion. Conclusion: The Bernageau view provided a suitable x-ray image for studying the anterior glenoid rim and for assessing erosion after comparison with the unaffected side.
Keywords: Shoulder Dislocation, Radiography, Orthopedics, Planning
INTRODUCTION
Bone erosion on the anterior glenoid rim has been correlated with a series of shoulder dislocation events and, depending on its magnitude, there may be an indication for using a bone graft to avoid its recurrence1, 2, 3, 4.
Several radiographic views for assessing the anterior. glenoid rim, and consequently the presence of erosion, have been described2, 5, 6, 7. Even though radiography is a low-cost examination, few studies have demonstrated that it might be a suitable examination for measuring anteroinferior glenoid erosion. Moreover, these radiographic views depend on special equipment for adjusting the patient's positioning and are difficult to reproduce2, 5, 6.
Other methods for evaluating the anterior glenoid rim include tomography(6), tomography with three-dimensional reconstruction8, 9 and shoulder arthroscopy with the aid of a probe marked out in millimeters(10). However, these methods are expensive and, unfortunately are not available in all institutions.
The aim of this study was to conduct a prospective analysis on the anteroinferior border of the glenoid, and consequently on the presence of erosion, with adequately positioned subjects and using an ordinary x-ray machine to reproduce the radiographic view described by Bernageau et al(5). In addition, the aim was to analyze the distance between the anterior and posterior rims of the glenoid, in order to evaluate the variability and reproducibility of the view.
MATERIALS AND METHODS
During the months of January and February 2008, 50 healthy adults without any previous history of pathological conditions in the shoulders underwent a radiographic assessment on their shoulders (100 examinations). The mean age of the individuals was 34 years (ranging from 20 to 68 years); 31 were male and 19 were female.
This study was approved by the research ethics committee of our institution, under the number 082/2009. All the subjects read and signed an informed consent statement before undergoing the radiographic examination.
Individual positioning
The radiographic examination was performed after standardization of the positioning of the subjects and of the x-ray tube.
Each individual was put in a standing position, with the arm to be assessed in anterior flexion at 160° and the chest in contact with the radiographic cassette at an angle of 70°. To ensure the reproducibility of this positioning in all the examinations, a specially prepared cushion was placed on the anterior surface of the subject's chest, thereby ensuring that the chest maintained this angle in relation to the radiographic cassette (Figures 1 and 2).
Figure 1.

Positioning of the patient, showing the x-ray tube at a craniocaudal angle of 30° and centered on the spine of the scapula, with the use of a special cushion to correct the chest inclination.
Figure 2.

Positioning of the patient with the chest at an angle of 70° with the radiographic chassis (upper view).
The radiographic apparatus used in this study was the Shimadzu 1/2P38D (Shimadzu Corporation, Kyoto, Japan). The x-ray tube was positioned at a distance of 100 cm from the shoulder under examination, at an angle of 30° of caudal inclination and centered on the spine of the scapula (Figure 1). The same technique was used in all the examinations [65 kV (± 5 kV) and 20 mA], and the same type and size of radiographic film was used (FotoMed™; 24 x 30 cm).
A Steinmann number 3 pin of 10 cm in length was placed on the subject's shoulder for correction of the magnification.
Objective evaluation
The objective evaluation was performed by measuring the distance between the anterior and posterior glenoid rims (anteroposterior axis), along the anterior and posterior cortical bone of the scapula.
This measurement was made by three independent examiners, and each examiner did each examination three times randomly, without knowing which case was under evaluation.
Subjective evaluation
The subjective evaluation was performed by three shoulder and elbow surgeons who were invited in. These surgeons had not participated directly in designing the study. They answered a questionnaire that asked for their opinions regarding whether the proposed positioning was suitable for achieving the Bernageau view and, consequently, whether it would be possible to assess the anteroinferior glenoid rim.
Statistical analysis
The SPSS software (Statistical Package for Social Sciences, version 13.0, SPSS Inc., Chicago, USA) was used for the statistical analysis. Pearson's correlation coefficient was applied to assess the intra and inter-observer reproducibility. The Anderson-Darling normality test was used to evaluate whether the objective measurements presented normal distribution and the kappa coefficient was applied to evaluate the concordance between the opinions of the three shoulder and elbow surgeons. We took p < 0.05 to be significant.
RESULTS
Objective analysis
The distance between the anterior and posterior glenoid rims ranged from 16.92 mm to 31.81 mm in the right shoulder (mean of 24.82 mm ± 3.16 mm) and from 18.64 mm to 32.22 mm in the left shoulder (mean of 24.48 mm ± 3.32 mm).
The reproducibility between the three measurements made by each of the three examiners was assessed. For this, Pearson's correlation test was used. We found significant correlations both between the three measurements of each examiner and between the three examiners, with P < 0.05 (Tables 1 and 2).
Table 1.
Distribution of the measurements made by the examiners.
| Examiner 1 |
Examiner 2 |
Examiner 3 |
|||||
|---|---|---|---|---|---|---|---|
| Pair of Variables | N | Correlation coefficient | Significance(p) | Correlation coefficient | Significance(p) | Correlation coefficient | Significance(p) |
| GLE-1-R x GLE-2-R | 50 | 0.976 | <0.001 | 0.949 | <0.001 | 0.962 | <0.001 |
| GLE-1-R x GLE-3-R | 50 | 0.95 | < 0.001 | 0.989 | < 0.001 | 0.967 | < 0.001 |
| GLE-2-R x GLE-3-R | 50 | 0.942 | < 0.001 | 0.952 | < 0.001 | 0.962 | < 0.001 |
| GLE-1-L x GLE-2-L | 50 | 0.976 | < 0.001 | 0.955 | < 0.001 | 0.97 | < 0.001 |
| GLE-1-L x GLE-3-L | 50 | 0.978 | < 0.001 | 0.586 | < 0.001 | 0.974 | < 0.001 |
| GLE-2-L x GLE-3-L | 50 | 0.97 | < 0.001 | 0.952 | < 0.001 | 0.977 | < 0.001 |
Legend: GLE1- first measurement by examiner, GLE2- second measurement by examiner, GLE3- third measurement by examiner, R: right side, L left side.
Source: Radiology Service.
Table 2.
Comparative distribution of the measurements made by the three examiners on the right and let sides.
| Right side |
Left side |
||||
|---|---|---|---|---|---|
| Pair of Variables | N | Correlation coefficient | Significance(p) | Correlation coefficient | Significance(p) |
| Examiner 1 GLE-1 x Examiner 2 GLE-1 | 50 | 0.805 | < 0.001 | 0.709 | < 0.001 |
| Examiner 1 GLE-1 x Examiner 3 GLE-1 | 50 | 0.782 | < 0.001 | 0.77 | < 0.001 |
| Examiner 2 GLE-1 x Examiner 3 GLE-1 | 50 | 0.936 | < 0.001 | 0.899 | < 0.001 |
| Examiner 1 GLE-2 x Examiner 2 GLE-2 | 50 | 0.759 | < 0.001 | 0.634 | < 0.001 |
| Examiner 1 GLE-2 x Examiner 3 GLE-2 | 50 | 0.735 | < 0.001 | 0.689 | < 0.001 |
| Examiner 2 GLE-2 x Examiner 3 GLE-2 | 50 | 0.877 | < 0.001 | 0.814 | < 0.001 |
| Examiner 1 GLE-3 x Examiner 2 GLE-3 | 50 | 0.777 | < 0.001 | 0.682 | < 0.001 |
| Examiner 1 GLE-3 x Examiner 3 GLE-3 | 50 | 0.719 | < 0.001 | 0.723 | < 0.001 |
| Examiner 2 GLE-3 x Examiner 3 GLE-3 | 50 | 0.9 | < 0.001 | 0.882 | < 0.001 |
Legend: GLE1- first measurement by examiner, GLE2- second measurement by examiner, GLE3- third measurement by examiner.
Source: Radiology Service.
The distance between the anterior and posterior glenoid rims had normal distribution in 16 of the 18 measurements made in this study, using the Anderson-Darling normality test (95% of the samples within the confidence interval) (Figure 3).
Figure 3.
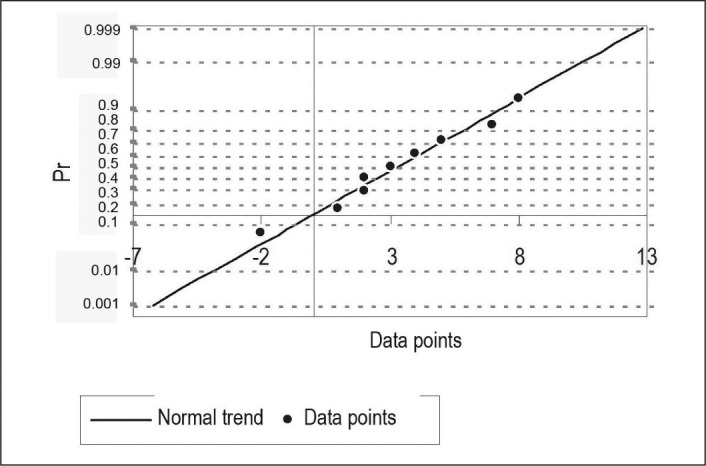
Distribution of the first measurement made by examiner 1 on the right shoulder (example of normal distribution)
Subjective analysis
The three shoulder and elbow surgery specialists were named observers 1, 2 and 3. Out of the 100 assessments made by observer 1, he believed that in 67% of the cases, this radiographic view was similar to the Bernageau view and consequently was suitable for evaluating the anteroinferior glenoid rim. Observer 2 believed that the radiographs were adequate in 81% in the case and observer 3 concluded that 78% of the examinations were adequate for evaluating the anteroinferior glenoid rim.
From the kappa coefficient test, we observed that there was significant agreement between the information obtained by observers 2 and 3 (P = 0.037). Between observers 1 and 2 and between observers 1 and 3, there was no statistically significant correlation between the measurements (p > 0.05).
DISCUSSION
The presence of erosion of the anteroinferior glenoid rim may lead to high rates of recurrence of shoulder dislocation when conventional treatment is performed on traumatic dislocation, especially when it is greater than 25%1, 9, 11, 12. Burkhart and De Beer et al(1) found a recurrence rate of 67% in cases with significant bone loss that were treated arthroscopically, while the recurrence was only 4% in the cases without erosion. Thus, preoperative planning is of prime importance, in order to avoid this complication.
Although several authors have demonstrated that it is possible to determine, during arthroscopic treatment, whether significant erosion of the glenoid is present (inverted pear format) and to measure it using a probe marked out in millimeters(10), others have observed that the intraoperative evaluation may not always be correct(13). Miyasaki et al demonstrated the difficulty in determining the presence of erosion of the anteroinferior glenoid rim and in quantifying it(14). However, the importance of arthroscopic assessment prior to open surgery is well documented(4).
The radiographic assessment is part of the preoperative planning, when attempting to quantify the presence of bone erosion. The Garth, axillary and West Point views were cited by Doneux et al(15) as views that could be requested in order to adequately assess the glenoid in cases of traumatic anterior instability of the shoulder. However, noting was said about quantification of the possible bone loss. Itoi et al(6) demonstrated that with the West Point view, it was possible to quantify the erosion of the anteroinferior rim with good precision. However, to reproduce this view, a radiographic tube that can angle at 25° in different planes has to be used, and some machines do not have this freedom of movement. In addition, in the same study, Itoi et al(6) cited that this view is difficult to reproduce in patients, even with x-ray apparatus that has this range of motion.
Bernageau et al(5) described a radiographic view that would make it possible to evaluate erosions or fractures of the anteroinferior glenoid rim. However, the description of how to reproduce it is incomplete. Edwards et al(2) used this view to assess lesions of the anteroinferior glenoid rim, with patient positioning achieved with the aid of a fluoroscope in order to ensure reproducibility.
In our study, it was possible to reproduce the same radiographic view by using a simple x-ray machine, without using a fluoroscope to support this. Three shoulder surgery specialists who had not participated directly in designing this study assessed 100 radiographs and observed that in most cases, it was possible to adequately assess the anteroinferior glenoid rim.
The distance measurement proposed in this study proved to be reproducible and presented normal distribution, and the values found were similar to the findings in other papers10, 13.
It is important to emphasize that we are not proposing a new radiographic view. Rather, we are describing a simple means of reproducing a view that was previously described by Bernageau et al for assessing the anteroinferior glenoid rim (Figure 4). Since it was possible to measure the distance between the anterior and posterior glenoid rims, we were able to assess the percentage bone loss by comparing the distance in the affected shoulder with the distance in the healthy shoulder (Figure 5). To the best of our knowledge, this evaluation by means of radiographs had not been put forward until now.
Figure 4.

Evaluation of the anterior glenoid rim.
Source: Radiology Service
Figure 5.

Example of erosion calculation, measuring the anteroposterior distance of the glenoid rim in both shoulders and comparing them.
In summary, radiographic examinations are less expensive and release less radiation that computed tomography does. For this reason, we propose that this evaluation method should be used whenever there is a clinical suspicion of erosion of the anteroinferior glenoid rim, as described by Bigliani et al(16), and that computed tomography should only be performed on patients in whom erosion has already been confirmed through a radiographic assessment.
CONCLUSION
We conclude that this radiographic view is an adequate and reproducible way of measuring the presence of glenoid erosion.
The mean distance was 24.48 mm ± 0.332 mm in the left shoulder and 24.82 mm ± 0.316 mm in the right shoulder.
Footnotes
Work performed in the Shoulder and Elbow Surgery Group, ABC Medical School and Hospital do Ipiranga.
REFERENCES
- 1.Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16(7):677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 2.Edwards TB, Boulahia A, Walch G. Radiographic analysis of bone defects in chronic anterior shoulder instability. Arthroscopy. 2003;19(7):732–739. doi: 10.1016/s0749-8063(03)00684-4. [DOI] [PubMed] [Google Scholar]
- 3.Boileau P, Villalba M, Hery JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88(8):1755–1763. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 4.Speer KP, Deng X, Borrero S, Torzilli PA, Altchek DA, Warren RF. Biomechanical evaluation of a simulated Bankart lesion. J Bone Joint Surg Am. 1994;76(12):1819–1826. doi: 10.2106/00004623-199412000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Bernageau J, Patte D, Debeyre J, Ferrane J. Value of the glenoid profil in recurrent luxations of the shoulder. Rev Chir Orthop Reparatrice Appar Mot. 1976;62(2 Suppl):142–147. [PubMed] [Google Scholar]
- 6.Itoi E, Lee SB, Amrami KK, Wenger DE, An KN. Quantitative assessment of classic anteroinferior bony Bankart lesions by radiography and computed tomography. Am J Sports Med. 2003;31(1):112–118. doi: 10.1177/03635465030310010301. [DOI] [PubMed] [Google Scholar]
- 7.Rockwood CA. X-ray evaluation of shoulder problems. The shoulder. W.B. Saunders; Philadelphia: 1990. pp. 196–200. [Google Scholar]
- 8.Chuang TY, Adams CR, Burkhart SS. Use of preoperative three-dimensional computed tomography to quantify glenoid bone loss in shoulder instability. Arthroscopy. 2008;24(4):376–382. doi: 10.1016/j.arthro.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 9.Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am. 2003;85(5):878–884. doi: 10.2106/00004623-200305000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Burkhart SS, Debeer JF, Tehrany AM, Parten PM. Quantifying glenoid bone loss arthroscopically in shoulder instability. Arthroscopy. 2002;18(5):488–491. doi: 10.1053/jars.2002.32212. [DOI] [PubMed] [Google Scholar]
- 11.Carr AJ. Biomechanics of shoulder stability. Curr Orthop. 1996;10:146–150. [Google Scholar]
- 12.Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am. 1978;60(1):1–16. [PubMed] [Google Scholar]
- 13.Kralinger F, Aigner F, Longato S, Rieger M, Wambacher M. Is the bare spot a consistent landmark for shoulder arthroscopy? A study of 20 embalmed glenoids with 3-dimensional computed tomographic reconstruction. Arthroscopy. 2006;22(4):428–432. doi: 10.1016/j.arthro.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 14.Miyazaki AN, Doneux PS, Fregoneze M, Silva LA, Checcia SL. Avaliação da capacidade de mensuração visual da erosão em um modelo de gesso simulando a cavidade glenoidal na luxação recidivante anterior do ombro¨. Rev Bras Ortop. 2002;37(9):403–407. [Google Scholar]
- 15.Doneux PS, Checchia SL, Miyazaki NA. Padronização do estudo radiográfico da cintura escapular. Rev Bras Ortop. 1998;33(11):883–888. [Google Scholar]
- 16.Bigliani LU, Newton PM, Steinmann SP, Connor PM, Mcllveen SJ. Glenoid rim lesions associated with recurrent anterior dislocation of the shoulder. Am J Sports Med. 1998;26(1):41–45. doi: 10.1177/03635465980260012301. [DOI] [PubMed] [Google Scholar]


