Abstract
Objective: To compare the magnetic resonance imaging findings from the pubis of professional soccer players without any history or clinical findings of groin pain, and from sedentary individuals, also without symptoms, and to determine the prevalence of changes compatible with pubic overload. Methods: Nineteen professional soccer players without complaints of groin pain and seventeen sedentary individuals, also asymptomatic, underwent magnetic resonance imaging of the pubis. The results from the examinations were analyzed regarding the presence of degenerative changes, boned medullary edema and tendinopathy, and the two study groups were compared. Results: High prevalence of bone edema, tendinopathy and degenerative findings in the pubic symphysis was seen in the athletes, with statistically significant higher odds ratios and relative risk in the population studied. Conclusion: Professional soccer players are at a higher risk of developing changes in the pubic region, shown in magnetic resonance images, compared with sedentary individuals. These findings are not necessarily caused by groin pain, and are probably related to intense exertion.
Keywords: Pubalgia, Athletes, Osteitis pubis, Magnetic Resonance, Pubis, Soccer Players
INTRODUCTION
Groin pain is a relatively common pathological condition and it affects 2% to 7% of professional athletes in different sports1, 2, 3. Among soccer players, the prevalence may reach 58%(4). The chronic pain in the inguinal region is incapacitating and may stop the athlete from performing at competitive level in his sport, thus generating a large socioeconomic impact1, 3, 5, 6. Together with other pathological conditions in the hip, such as femoroacetabular impact, labral lesions and hip joint conditions, hip pain is an important reason why athletes may be kept away from their competitive activities.
The etiology of groin pain is diverse and includes osteitis pubis, tendinopathy of the adductors (especially the long adductor), lesions of the rectus abdominis muscle and sports hernia1, 2, 4, 7, 8. Other pathological conditions such as bruising, lesions or tendinitis of the gracilis, iliopsoas or rectus femoris muscles, labral lesions, degenerative changes to the hip or pubic symphysis, ossifying myositis, stress fractures, epiphysitis, avulsion fractures, lumbar radiculopathy, neoplasia and spondyloarthropathy, along with urological or gynecological disorders, complete the differential diagnosis6, 9, 10.
The diagnosis is essentially clinical and is based on the compatible history and on physical examination. Ultrasound, scintigraphy and magnetic resonance imaging (MRI) are used as complementary methods, and MRI is the gold standard, with the highest sensitivity, specificity and accuracy1, 2, 5, 9, 10, 11, 12.
Groin pain is characterized by the presence of insidious pain in the pubic and deep inguinal regions that worsens with exertion and while walking. It may spread out to the perineal, mid-thigh and rectus abdominis areas. It is more commonly unilateral, although several reports of bilaterality exist(1-5,9). Histories of intense sports activities that require abrupt acceleration, kicking, rapid alternation of single-leg load bearing, abrupt changes in direction and circular movement of the trunk are generally present5, 7, 8, 13, and groin pain is a common reason why top-level athletes may be kept away from their sport.
Periods of improvement and exacerbation may be reported, relating to the intensity of training and competitions. In physical examinations, pain may be observed upon resisted adduction of the hip, along with hypersensitivity of the pubic symphysis and the insertion region of the rectus abdominis and adductor longus muscles3, 4, 8.
MRI on the pubis is the complementary examination of choice for diagnosing these lesions(10). Although computed tomography may show early degenerative bone lesions, MRI presents greater sensitivity, given that it allows tendon and muscle lesions to be identified early on. Findings of bone edema in the public symphysis, degenerative changes, intra-articular fluid or lesions of the tendons of the adductor and rectus abdominis muscles are commonly correlated with this pathological condition10, 11, 12. In assessments on asymptomatic athletes, some authors have found the same changes in a significant number of cases, thereby reducing the accuracy of the examination. In their view, up to two thirds of asymptomatic athletes may have changes suggestive of pubic pathological conditions. Although MRI is considered to have sensitivity of 98% and specificity of 100% in diagnosing groin pain, it was shown to be insensitive in those reports, with a high false positive rate10, 14, 15, 16. This finding suggests that although the athletes presented lesions that would be considered suggestive of groin pain, there was no clinical repercussion at the time of the study, thereby showing that the changes found in the images translated the excessive exertion and did not diagnose the pathological condition. Our hypothesis here is that changes seen on MRI are more frequent in athletes but are not necessarily caused by groin pain.
MATERIALS AND METHODS
Twenty-six athletes (the whole squad) of a professional soccer team in the first division of the State of Rio de Janeiro, which was working at competitive pace, were eligible for examination. At that time, the team was competing in the state championship, playing one competitive game per week and undertaking give training sessions per week, of which three reproduced the sports movements. The images were produced mid-season, at the time of the round of 16 in the championship. Three athletes were excluded because of a prior suggestive clinical condition, with a previous diagnosis of osteitis pubis that had been treated conservatively; along with three who did not agree to undergo the examination, even though they were asymptomatic; and one who had been off training activities for two months because of a painful condition in the hip suggestive of a pubic pathological condition. The remaining 19 athletes all underwent the MTI examination on the pubis. None of them presented any previous pathological condition in the hip, and none of them mentioned any complaints of pubic or femoroacetabular pain. The mean length of time for which they had been professionally active was 54 months, with a range from 18 to 96 months.
As controls, 17 asymptomatic male individuals aged 23 to 38 years, who did not have any history of inguinal pain and were not practicing any sports activity (i.e. sedentary habits), also underwent the same examination. Regular practice of any sports activity at any previous time, or any occasional activity over the last six months, was considered to be an exclusion criterion. This group of individuals, which was age and sex-matched, was chosen because there was less likelihood that such individuals had been subjected to pubic stress over recent months. A group composed of amateur athletes could have led to unreliable results, given that the athletes' degree of activity would not be a controlled factor.
The ages of the athletes studied ranged from 18 to 31 years, with a mean of 22.05 years and a median of 22 years. The sedentary controls were between 23 and 38 years of age, with a mean of 28.56 years and median of 28 years. The groups were shown to be equivalent, with a p-value of 0.71.
Both group (athletes and sedentary individuals) underwent the same MRI protocol. Panoramic images of the pelvis were obtained in T1 and STIR in the coronal plane, with slices of 5 mm in thickness and FOV (field of view) of 42 cm, and specific localized images of the pubis in proton density with FSE (fast spin echo) fat suppression, with slices of 3 mm in the sagittal and oblique coronal planes (TR 2450 and TE 37). All the examinations were generated on the same apparatus (General Electric® 1.5 T).
The images were examined to search for any degenerative changes, which would be characterized by osteophytes, irregularity of the cortical bone and posterosuperior protrusion of the joint disc. In addition, signals suggestive of osteitis pubis (bone edema) or myotendinous lesions in the rectus abdominis, adductor longus and adductor brevis muscles, characterized by lesions of the aponeurosis, complete tearing and tendinosis were also investigated3, 5.
Two experienced radiologists independently analyzed all the images and issued reports on changes compatible with the causes of groin pain. The first radiologist analyzed the images obtained from all the athletes and from the control group, and the images and reports were reviewed by the senior radiologist. Neither of the radiologists was aware of the nature of the patient examined (i.e. athlete or sedentary individual).
The results were analyzed statistically, and p < 0.05 was considered significant. The data were analyzed in the Epi-Info 6.0 and Meta-DiSc v.1.4 software, using the Kolmogorov-Smirnov test, and the analyses were reviewed by a professional mathematician-statistician.
RESULTS
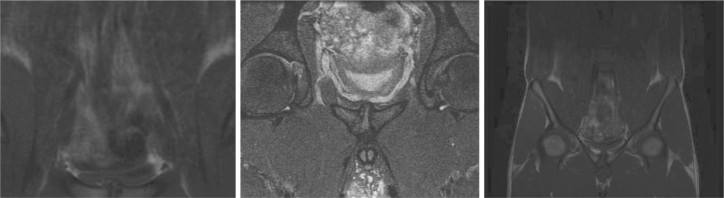
Eighteen athletes (94.73%) presented signs suggestive of degenerative changes such as osteophytes, irregularity of the cortical bone and posterosuperior protrusion of the joint disc (Figure 1), while only one non-athlete (6.25%) had an image compatible with such findings, with a p-value of 0.018. The calculated relative risk (RR) was 15.16 and the odds ratio (OR) was 28.8 (Tables 1 and 2).
Figure 1.
Magnetic resonance imaging of the pubis in a professional soccer player, showing degenerative changes in the pubic symphysis, such as osteophytes, irregularity of the joint surface and disc protrusion.
Table 1.
Number of cases and prevalence of degenerative changes, including the presence of osteophytes, cortical irregularity, disc protrusion, bone edema (representing osteitis) and myotendinous lesions. Findings shown on magnetic resonance imaging of the pubic, among asymptomatic athletes and sedentary individuals.
| Degenerative changes |
Edema (Osteitis) |
Myotendinous lesions |
||||
|---|---|---|---|---|---|---|
| Cases | Prevalence | Cases | Prevalence | Cases | Prevalence | |
| Athletes | 18 | 94.73% | 5 | 26.31% | 6 | 31.57% |
| Sedentary individuals | 1 | 6.25% | 1 | 6.25% | 0 | 0% |
Table 2.
Risk of developing degenerative changes in the pubic symphysis, osteitis or myotendinous lesions, among male soccer players under an intense regime at competitive level, compared with sedentary individuals of the same sex, matched according to age.
| Relative risk | Odds ratio | p-value | |
|---|---|---|---|
| Degenerative changes | 15.16 | 28.8 | 0.048 |
| Edema (osteitis) | 5.26 | 7.38 | 0.001 |
| Myotendinous lesions | 4.21 | 5.71 | 0.04 |
Bone edema representing osteitis pubis (Figure 2) was observed in six athletes (31.57%), but this change was seen in only one sedentary individual (6.25%), with a p-value of 0.001. The RR was 5.26 and the OR was 7.38 (Tables 1 and 2).
Figure 2.
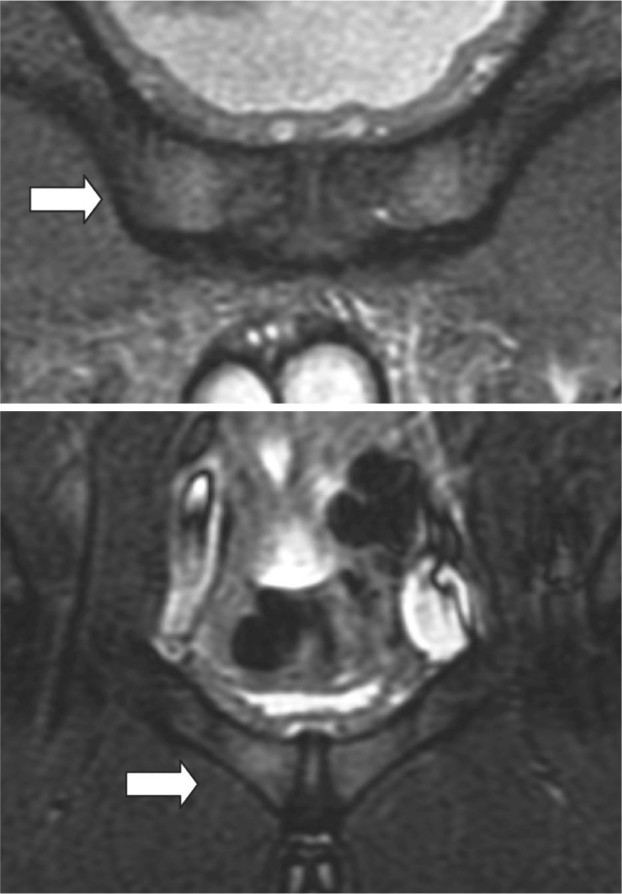
Magnetic resonance imaging of the pubis in a professional soccer player at competitive level showing medullary edema (arrows), suggestive of osteitis pubis.
Changes in the muscles or tendons suggestive of degeneration or tearing of adductors or the rectus abdominis, were found in five athletes (26.31%) and in one sedentary individual (6.25%), with a p-value of 0.04. The RR was 4.21 and the OR was 5.71.
DISCUSSION
Groin pain is very common among athletes and, in our setting, particularly among soccer players. Because of the acceleration and deceleration, abrupt changes in direction and repeated kicking, practitioners of this sport have a greater likelihood of presenting pain in the inguinal region. The etiology is diverse and includes osteitis pubis, tendinopathy of the rectus abdominis and adductor longus, hernias, and other causes1, 2, 3, 4, 5, 6, 7, 8, 14, 16.
MRI is considered to be the gold standard for diagnosing changes of this nature that are present in the pubis. Bone edema, joint effusion into the pubic symphysis and muscle-tendon lesions are frequent findings, along with degenerative changes.
In recent studies, the same changes as described in patients with painful complaints have been found in asymptomatic athletes14, 15, 16. Although the prevalence of osteotendinous changes seen on MRI in athletes without previous complaints is lower, it has been speculated that signs that were previously described as etiological diagnoses of groin pain are, in reality, degenerative changes relating to repetitive exertion.
The pubic symphysis is composed of an intra-articular disc interposed between the two innominate bones anteriorly, and is responsible for the anterior stability of the pelvic ring. There is no joint capsule. The presence of four peripheral ligaments ensures that the joint compartment is maintained. The oval surface is responsible for load transmission and joint stability. A small range of motion is present in this joint, decomposed in rotation of around 3° and craniocaudal translation of around 2 mm8, 9, 12.
The area of muscle insertion into the pubic ramus is broad. The rectus abdominis, internal and external oblique muscles and transverse muscles on both sides are inserted superiorly and act as dynamic stabilizers of the anterior pelvic ring. Inferiorly, the adductor longus, brevis and magnus, pectineus and gracilis muscles are inserted into the edge of the pubis. Medially, and peripherally to the pubic symphysis, the rectus abdominis muscle superiorly and adductor longus muscle inferiorly are the main stabilizers. They act as a single system, generating opposing vectors and restricting the movement of this joint, thereby preventing direct impact on and consequent wear of the joint cartilage component. These are antagonist muscles that present magnified action during walking1, 7, 8, 9, 11, 12, 17.
Either separately or in association with osteitis pubis and lesions of the rectus abdominis, the main cause of pain in the pubic-inguinal region is impairment of the tendon of the adductor longus muscle(18). Some authors have considered these pathological conditions to be just different spectra within the same disease(10), thus presenting a common cause characterized by overload and excessive exertion.
Professional athletes are subjected to intense training programs, as well as intense exertion during competitions. This overload on the pubic region may lead to degenerative changes to the symphysis. The insertions of the adductors and the rectus abdominis muscle may present lesions due to stress from training. Bone edema is related to biomechanical overload on the pubis(9). These changes are not necessarily related to groin pain. Athletes who go through the same training also present such changes(10). Up to two thirds of asymptomatic athletes present degenerative findings on MRI(10).
In our study, we compared asymptomatic athletes who were professional soccer players with sedentary individuals without any history of groin pain. We observed that there was a significantly higher prevalence of degenerative images in the examinations on the athletes than on the non-athletes. The prevalence of degenerative changes was 94.73% among the athletes and 6.25% among the non-athletes (p = 0.048).
The prevalence of bone edema was 31.57% among the athletes and 6.25% among the non-athletes, thus suggesting that this change was probably related to pubic overload (p = 0.001). Changes to soft tissues were also more prevalent among the athletes (26.31 %) than among the non-athletes (6.25%), with p = 0.04.
There was a single case of bone medullary edema in the sedentary group. This 23-year-old volunteer had previously done occasional physical activity (running and soccer), but had been away from these activities for eight months.
According to the results from the present study, professional soccer players present a risk of developing degenerative changes in the pubic region over the course of their careers that is 15 times greater than among non-athletes. The risk that these athletes will develop osteitis pubis is five times greater, and for myotendinous lesions, four times greater, than among sedentary individuals. The chance of occurrences of degenerative changes in the pubis in athletes is 28 times greater than among sedentary individuals. The chance of occurrences of bone medullary edema is seven times greater, and of myotendinous lesions is five times greater, in athletes than in non-athletes.
Our study has limitations relating to the small number of asymptomatic athletes and other individuals, the lack of comparative images from the same athletes at different phases of the training, and the age difference between the athlete and sedentary groups. Regarding this age difference, we consider that this was favorable, given that older sedentary individuals would theoretically be subjected to greater stress; however, we cannot prove this.
CONCLUSION
According to the present study, professional soccer players present greater risk of developing degenerative lesions, bone medullary edema and tendinous changes in the pubic region, compared with sedentary individuals. These findings are not necessarily caused by groin pain, and are probably related to intense exertion.
Footnotes
Work performed at the Orthopedics and Traumatology Service, Clementino Fraga Filho University Hospital (HUCFF), Federal University of Rio de Janeiro (UFRJ).
REFERENCES
- 1.Cunningham PM, Brennan D, O'Connell M, MacMahon P, O'Neill P, Eustace S. Patterns of bone and soft-tissue injury at the symphysis pubis in soccer players: observations at MRI. AJR Am J Roentgenol. 2007;188(3):W291–W296. doi: 10.2214/AJR.06.0051. [DOI] [PubMed] [Google Scholar]
- 2.Biedert RM, Warnke K Meyer SS. Symphysis syndrome in athletes: surgical treatment for chronic lower abdominal, groin, and adductor pain in athletes. Clin J Sport Med. 2003;13(5):278–284. doi: 10.1097/00042752-200309000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Koulouris G. Imaging review of groin pain in elite athletes: an anatomic approach to imaging findings. AJR Am J Roentgenol. 2008;191(4):962–972. doi: 10.2214/AJR.07.3410. [DOI] [PubMed] [Google Scholar]
- 4.Omar IM, Zoga AC, Kavanagh EC, Koulouris G, Bergin D, Gopez AG. Athletic pubalgia and “sports hernia”: optimal MR imaging technique and findings. Radiographics. 2008;28(5):1415–1438. doi: 10.1148/rg.285075217. [DOI] [PubMed] [Google Scholar]
- 5.Lovell G, Galloway H, Hopkins W, Harvey A. Osteitis pubis and assessment of bone marrow edema at the pubic symphysis with MRI in an elite junior male soccer squad. Clin J Sport Med. 2006;16(2):117–122. doi: 10.1097/00042752-200603000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Brown RA, Mascia A, Kinnear DG, Lacroix V, Feldman L, Mulder DS. An 18-year review of sports groin injuries in the elite hockey player: clinical presentation, new diagnostic imaging, treatment, and results. Clin J Sport Med. 2008;18(3):221–226. doi: 10.1097/JSM.0b013e318172831a. [DOI] [PubMed] [Google Scholar]
- 7.Zajick DC, Zoga AC, Omar IM, Meyers WC. Spectrum of MRI findings in clinical athletic pubalgia. Semin Musculoskelet Radiol. 2008;12(1):3–12. doi: 10.1055/s-2008-1067933. [DOI] [PubMed] [Google Scholar]
- 8.Robinson P, Salehi F, Grainger A, Clemence M, Schilders E, O'Connor P. Cadaveric and MRI study of the musculotendinous contributions to the capsule of the symphysis pubis. AJR Am J Roentgenol. 2007;188(5):W440–W445. doi: 10.2214/AJR.06.1238. [DOI] [PubMed] [Google Scholar]
- 9.Johnson R. Osteitis púbis. Curr Sports Med Rep. 2003;2(2):98–102. doi: 10.1249/00149619-200304000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Paajanen H, Hermunen H, Karonen J. Pubic magnetic resonance imaging findings in surgically and conservatively treated athletes with osteitis pubis compared to asymptomatic athletes during heavy training. Am J Sport Med. 2008;36(1):117–121. doi: 10.1177/0363546507305454. [DOI] [PubMed] [Google Scholar]
- 11.Zoga AC, Kavanagh EC, Omar IM, Morrison WB, Koulouris G, Lopez H. Athletic pubalgia and the “sports hernia”: MR imaging findings. Radiology. 2008;247(3):797–807. doi: 10.1148/radiol.2473070049. [DOI] [PubMed] [Google Scholar]
- 12.Brennan D, O'Connell MJ, Ryan M, Cunningham P, Taylor D, Cronin C. Secondary cleft sign as a marker of injury in athletes with groin pain: MR image appearance and interpretation. Radiology. 2005;235(1):162–167. doi: 10.1148/radiol.2351040045. [DOI] [PubMed] [Google Scholar]
- 13.Verrall GM, Slavotinek JP, Fon GT. Incidence of pubic bone marrow oedema in Australan rules football players: relation to groin pain. Br J Sport Med. 2001;28(1):11–19. doi: 10.1136/bjsm.35.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brukner P, Cowan S, Crossley K, Schache A, Smith P. Is there a role for magnetic resonance imaging in chronic groin pain? Aust J Sci Med Sport. 2004;7(4 Suppl 1):76. [Google Scholar]
- 15.Albers SL, Spritzer CE, Garrett WE, Jr, Meyers WC. MR findings in athleteswith pubalgia. Skeletal Radiol. 2001;30(5):270–271. doi: 10.1007/s002560100335. [DOI] [PubMed] [Google Scholar]
- 16.Robinson P, Barron DA, Parsons W, Grainger AJ, Schilders EM, O'Connor PJ. Adductor related groin pain in athletes: correlation of MR imaging with clinical findings. Skeletal Radiol. 2004;33(8):451–457. doi: 10.1007/s00256-004-0753-2. [DOI] [PubMed] [Google Scholar]
- 17.Cunningham PM, Brennan D, O'Connell M, MacMahon P, O'Neill P, Eustace S. Patterns of bone and soft-tissue Injury at the symphysis pubis in soccer players: observations at MRI. AJR Am J Roentgenol. 2007;188(3):W291–W296. doi: 10.2214/AJR.06.0051. [DOI] [PubMed] [Google Scholar]
- 18.O'Connell MJ, Powell T, McCaffrey NM, O'Connell D, Eustace SJ. Symphyseal cleft injection in the diagnosis and treatment of osteitis pubis in athletes. AJR Am J Roentgenol. 2002;179(4):955–959. doi: 10.2214/ajr.179.4.1790955. [DOI] [PubMed] [Google Scholar]