Abstract
Objective: Radiographic assessment of lower limb alignment, in the frontal and sagittal planes, after high tibial osteotomy. To stabilize the osteotomy, a tricortical iliac graft was used, along with a positioning screw. Methods: Prospective study on 46 patients with ages ranging from 17 to 61 years. Among them, 42 patients presented genu varum secondary to knee osteoarthritis and four from other causes. Teleradiography was performed for surgical planning, using the Frank Noyes method, as modified by Fugizawa. A conventional surgical access of 3 cm was made to harvest a tricortical iliac graft. Osteotomy was performed under radioscopic control, by means of an anteromedial incision of 3 cm with release of the superficial portion of the medial collateral ligament. The graft was placed in the posterior portion of the osteotomy, to maintain an unaltered tibial slope. The screw crossed the osteotomy orthogonally to protect the lateral cortex. Pre and postoperative radiographic criteria were established to assess the results. Results: There was consolidation in 100% of the cases and maintenance of the mechanical axis, obtained intraoperatively, in 94% of the cases. The posterior slope of the tibial plateau in the sagittal plane ranged from 7° to 12°. Joint mobility was restored in all the patients. Eleven patients presented temporary pain at the site of graft harvesting, but none had paresthesia. The incidence of complications was 8% (infection, loss of correction and joint fracture). Conclusion: The technique was shown to be reproducible, simple, biological, accurate and low-cost, and it may be an alternative to the existing techniques.
Keywords: Osteotomy, Knee, Osteoarthritis, Tibia/surgery
INTRODUCTION
Angular deformities of the knee have a variety of causes and osteoarthrosis is one of them. This is an inflammatory and degenerative pathological condition with consequent progressive nature. Its final outcome is always destruction of the chondral tissue and its inherent consequences1, 2.
Proximal osteotomy of the tibia has been a treatment method for angular deformities of the knee for decades. It was first described by Jackson(3) and subsequently was better studied and disseminated by Coventry et al(4) and Insall et al(5). Orthopedic treatment by means of osteotomy, thereby correcting the angular deformity, may diminish the speed of progression of this pathological phenomenon.
Improvements in the prognostic perspectives for degenerative chondropathy through the emergence of chondroprotective therapy and viscosupplementation have been corroborated through scientific studies(6). This has been one of the reasons responsible for the resurgence of osteotomy as a further useful possibility in the therapeutic arsenal for osteoarthrosis. It has come about in the light of improvements in the quality and survival of single-compartmental or total prostheses. When indicated within the criteria that have been well established in the literature(1,2), restoration of the mechanical axis of the lower limb and consequent balancing of the load distribution in the joint have led to relief of the painful symptoms and incontestable functional gains, with improvement of patients' quality of life7, 8.
Proximal tibial varus osteotomy is the recommended procedure for treating angular varus deformities of the knee, secondary to osteoarthrosis of the medial compartment or other etiologies. The classically described procedure, which is still much used, is lateral subtraction wedge osteotomy(9), but medial addition wedge osteotomy has been shown in the literature to present advantages, which has encouraged its use10, 11, 12.
The medium and long-term results depend fundamentally on maintaining the correction that was obtained during the operation, after consolidation of the osteotomy. For this, the fixation method is of fundamental importance13, 14. Tricortical iliac grafts have been shown to be sufficiently resistant to maintain this correction, even without adjuvant synthesis material(15). As well as maintaining the alignment, this allows early mobilization given that the fold mechanism formed by the lateral cortex and the muscle-tendon and lateral ligament structures, along with the extensor apparatus, ensure sufficient stability for this.
In subtraction wedge osteotomy, certain complications are relatively common. Among these, the following can be cited: delayed consolidation, pseudarthrosis, recurrence of the deformity through lack of stability, impossibility of repositioning the mechanical axis after making the bone cuts, and neurovascular lesions worsened through osteotomy of the fibula(16). In addition wedge osteotomy, these complications practically do not exist. Other factors of relevance include the preservation of the bone stock of the tibial plateau and its non-lateralization in relation to the diaphysis of the tibia. These points are fundamental for a possible future total knee arthroplasty procedure11, 12, 15.
The aim of the present study was to evaluate the radiographic results from the proposed surgical technique and its viability. We analyzed the time taken to achieve consolidation, the maintenance of the mechanical axis obtained through the surgical correction and the posterior slope angle of the tibial plateau on radiographs in true lateral view.
METHODS
Following analysis of the bibliography, this study was approved by the research ethics committee.
Between August 2004 and October 2008, 46 patients underwent operations (total of 50 osteotomy procedures). The patients' ages ranged from 17 to 61 years. Of these, three presented primary genu varum, without arthrosis, and one other patient had a varus deformity due to skewed consolidation of a proximal metaphyseal fracture of the tibia. The other 42 patients presented genu varum secondary to osteoarthrosis.
The following proposed protocol was used in this study: a) clinical assessment; b) preoperative radiographic assessment, consisting of AP and lateral radiographs with loading, axial radiograph of the patella and teleradiography of the lower limbs; c) surgical planning by means of teleradiography, using the Noyes method(17) (Figure 1); d) addition wedge osteotomy, using a tricortical iliac graft to maintain the angle of osteotomy opening, and fixation with a position screw (Figure 2); e) immobilization with an inguinal-malleolar orthosis for four weeks, but removing it during physiotherapy sessions from the second week onwards; f) weekly radiographic controls during the first month and then monthly until the end of the 16th postoperative week; g) walking with partial load-bearing in the 6th and full load-bearing in the 10th week; h) teleradiography on the lower limbs in the fifth month after the operation.
Figure 1.

Noyes method for planning osteotomy from teleradiography.
Figure 2.
Surgical technique: a) harvesting of tricortical iliac graft; b) maintenance of the angle of osteotomy opening by means of the graft; c) fixation with a positioning screw (postoperative radiograph).
With the radiographic control (teleradiography and lateral radiography on the tibia), the corrected mechanical axis of the lower limb and the posterior slope angle of the tibial plateau, respectively, were calculated.
The surgical technique consisted of harvesting the tricortical iliac graft, of approximate length 3.0 cm, based on the preoperative planning calculations from teleradiography. An anteromedial incision was made in the knee, of length 3.0 cm, followed by partial subperiosteal deinsertion of the goosefoot tendon and subtotal deinsertion of the superficial portion of the medial collateral ligament, under the insertion of the medial flexor tendon of the knee.
Oblique supra-tuberosity osteotomy was performed, while keeping the lateral cortex intact at the level of the apex of the head of the fibula. The osteotomy was opened and the graft was inserted until the cortical bone at the base of the graft coincided with the cortical bone of the tibia at the level of the osteotomy. In this way, the opening was maintained and the previously calculated alignment (mechanical axis) was attained.
A cannulated positioning screw (7.0) was inserted from proximal-medial to distal-lateral, thus crossing the osteotomy orthogonally to protect the lateral cortex (Figure 3).
Figure 3.
Postoperative view showing positioning screw crossing the osteotomy, with calculation of the posterior slope angle of the tibial plateau.
A suction drain was used for 24 hours in the graft harvesting area and in the osteotomy. Antibiotic prophylaxis was administered for 24 hours.
The technique proposed for this study was conceived based on studies that have already been published in the literature11, 12, 15.
RESULTS
Bone consolidation occurred within a maximum of 12 weeks in 100% of the cases. This made it possible to allow full loading within this period, in conformity with the protocol that had been established.
The radiographic evaluation in the coronal plane showed that the mechanical axis obtained during the operation was maintained in 94% (43 patients / 47 osteotomy procedures). The point at which the mechanical axis passed through the lateral tibial plateau, going from the center of the knee/point zero (Figure 4), presented the following distribution: 46% went through between 40% and 35%; 38% went through between 34% and 25%; 8% went through between 24 and 15%; 6% went through between 14% and 0%; and 2% went through the medial tibial plateau (Table 1).
Figure 4.
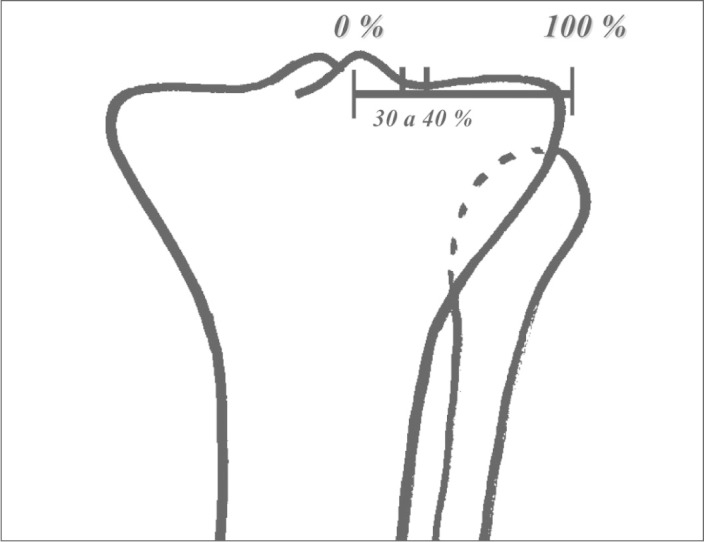
Ideal point of passage of the corrected mechanical axis, as recommended by Noyes et al.
Table 1.
Point of passage of the load line through the tibial plateau.
| Groups | Passage of the axis | Number of osteotomy procedures | % of osteotomy procedures |
|---|---|---|---|
| A | Between 35% and 30% | 23 | 46% |
| B | Between 29% and 25% | 19 | 38% |
| C | Between 24% and 15% | 4 | 8% |
| D | Between 14% and 0% | 3 | 6% |
| E | Varus | 1 | 2% |
The posterior slope angle of the tibia ranged from 7° to 12°. A comparison was made between the pre and postoperative posterior slope (sagittal plane) (Table 2). It was found that there was no inversion of the tibial slope, but that in some cases there was an increase, even placing the graft more posteriorly in the osteotomy opening.
Table 2.
Sagittal slope of the joint surface – tibial slope.
| Postoperative posterior slope in sagittal plane (*) | Number of osteotomy procedures | % of osteotomy procedures |
|---|---|---|
| 0 | 12 | 24% |
| 1 | 6 | 12% |
| 2 | 17 | 34% |
| 3 | 12 | 24% |
| 4 | 3 | 6% |
Comparison with preoperative tibial slope
There was no limitation on active or passive joint mobility in any of the patients who underwent the operation, including patients who were reoperated.
Eleven patients presented pain at the graft harvesting site for a period of between six and ten weeks after the operation.
The incidence of complications was 8% (four patients), and these consisted of infection with loss of alignment in two patients, one case of undercorrection and one case of joint fracture consequent to incomplete osteotomy (Figure 5).
Figure 5.
Case with complication described, showing joint fracture due to incomplete osteotomy, which was fixed during the operation.
DISCUSSION
When mechanical changes instituted through valgizing osteotomy on varus knees have been implemented under rigorous criteria of indication, they have translated into changes to the natural history of degenerative osteoarthritis(18). The favorable reports presented in the literature in relation to chondroprotective therapy6, 19 have become a further reason for carrying out procedures that are of more biological nature, such as osteotomy. On the other hand, there is no consensus in the literature regarding the possible benefits brought by combining this with arthroscopic procedures(16). In our study, arthroscopy was not performed on any of the patients.
Medial addition wedge osteotomy has been used increasingly because of the advantages it presents. Among these are the lack of need for osteotomy of the fibula, preservation of the bone stock of the proximal tibia, predictability of the number of degrees to be corrected and the smaller requirement for surgical dissection. This latter advantage, on its own, avoids a series of complications such as injuries to the fibular nerve(20). In our study, there were no cases of injury to the fibular nerve or to its branches.
When harvesting of the iliac graft is done in accordance with the techniques recommended in the literature, it is a low-morbidity procedure, and also has low incidence of ilioinguinal neuralgia(21). In our sample, pain at the graft harvesting site persisted in eight patients, for a maximum of 10 weeks. These data coincide with results presented in the literature(19).
Overcorrection, with passage of the mechanical axis through the lateral tibial plateau is fundamental for obtaining good results from valgizing osteotomy1, 2. With the technique described in this study, we achieved a correction that was considered ideal, going through between 40% and 30% of the lateral tibial plateau, in 84% of the cases. In a further 8%, the point of passage of the load line was between 29% and 25%. The slope of the tibial plateau in the sagittal plane is a critical point to be observed technically. Insertion of the graft posteriorly in the osteotomy is necessary for the tibial slope to be maintained within mechanically acceptable parameters(22). In our sample, a range between 7° and 12° could be seen, but there was no inversion of the tibial slope.
CONCLUSION
The surgical technique developed in the present study was shown to be reproducible and maintained a biological character because of the minimal quantity of implant used. In addition to presenting costs that were lower than those of most other techniques that exist for the same purposes, its consolidation rate was the same.
Footnotes
Work performed in Hospital de Clínicas, Federal University of Uberlândia, MG.
REFERENCES
- 1.Camanho GL. Tratamento da osteoartrose do joelho. Rev Bras Ortop. 2001;36(5):135–140. [Google Scholar]
- 2.Camanho GL, Olivi R, Camanho LF. Técnica de fixação para osteotomia supratuberositária cupuliforme valgizante da tíbia. Rev Bras Ortop. 2001;36(7):263–267. [Google Scholar]
- 3.Jackson JP. Osteotomy for osteoarthrites of the knee. J Bone Joint Surg Br. 1958;40:826. [Google Scholar]
- 4.Coventry MB, Ilstrup DM, Wallrichs SL. Proximal tibial osteotomy: A critical long-term study of eighty seven cases. J Bone Joint Surg Am. 1993;75(2):196–201. doi: 10.2106/00004623-199302000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Insall JN, Joseph DM, Msika C. High tibial osteotomy for varus gonarthrosis: A long-term follow-up study. J Bone Joint Surg Am. 1984;66(7):1040–1048. [PubMed] [Google Scholar]
- 6.Brief AA, Maurer SG, Di Cesare Use of glicosamine and chondroitina sulfate in the management of osteoarthritis. J Am Acad Orthop Surg. 2001;9(2):71–78. doi: 10.5435/00124635-200103000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Molina DR, Sado JJ, Mendlovitz PSR, Rubin MLL, Camanho GL. Avaliação da deformidade rotacional do joelho em pacientes com genuvaro e osteoartrose. Rev Bras Ortop. 2002;37(10):430–435. [Google Scholar]
- 8.Keyes GW, Carr AJ, Miller RK, Goodfellow WJ. The arthrographic classification of medial gonarthrosis. Correlation with operation methods in 200 knees. Acta Orthop Scand. 1992;63(5):497–501. doi: 10.3109/17453679209154722. [DOI] [PubMed] [Google Scholar]
- 9.Magyar G, Ahl TL, Vibe P, Toksvig-Larsen S, Lindstrand A. Open-wedge osteotomy by hemicallotasis or the closed-wedge technique for osteoarthritis of the knee. A randomised study of 50 operations. J Bone Joint Surg Br. 1999;81(3):444–448. doi: 10.1302/0301-620x.81b3.8925. [DOI] [PubMed] [Google Scholar]
- 10.Nakamura E, Mizuta H, Kudo S, Takagi K, Sakamoto K. Open-wedge osteotomy of the proximal tíbia with hemicallotasis. J Bone Joint Surg Br. 2001;83(8):1111–1115. doi: 10.1302/0301-620x.83b8.11993. [DOI] [PubMed] [Google Scholar]
- 11.Staubli AE, Simoni C, Babst R, Lobenhoffer P. TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia – early results in 92 cases. Injury. 2003;34(Suppl 2):B55–B62. doi: 10.1016/j.injury.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 12.Hernigou P, Ma W. Open wedge tibial osteotomy with acrylic bone cement as bone substitute. Knee. 2001;8(2):103–110. doi: 10.1016/s0968-0160(00)00061-2. [DOI] [PubMed] [Google Scholar]
- 13.Billings A, Scott DF, Camargo MP, Hofmann AA. High tibial osteotomy with a calibrated osteotomy guide, rigid inter al fixation, and early motion: long-term follow-up. J Bone Joint Surg Am. 2000;82(1):70–79. doi: 10.2106/00004623-200001000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Hofmann AA, Wyatt RW, Beck SW. High tibial osteotomy. Use of an osteotomy jig, rigid fixation, and early motion versus conventional surgical technique and cast immobilization. Clin Orthop Relat Res. 1991;(271):271–277. [PubMed] [Google Scholar]
- 15.Patond KR, Lokhande AV. Medial open wedge high tibial osteotomy in medial compartment osteoarthrosis of the knee. Natl Med J India. 1993;6(3):104–108. [PubMed] [Google Scholar]
- 16.Wright JM, Crockett HC, Slawski DP, Madsen MW, Windsor RE. High tibial osteotomy. J Am Acad Orthop Surg. 2005;13(4):279–298. doi: 10.5435/00124635-200507000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Dugdale TW, Noyes FR, Styer D. Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length. Clin Ortop Relat Res. 1992;(274):274–284. [PubMed] [Google Scholar]
- 18.Kanamiya T, Naito M, Yoshimura I. The influence of biomechanical factorson cartilage regeneration after high tibial osteotomy for knees with medial compartiment osteoarthrites: Clinical and arthroscopic observations. Arthroscopy. 2002;18(7):725–729. doi: 10.1053/jars.2002.35258. [DOI] [PubMed] [Google Scholar]
- 19.Raman R, Dutta A, Day N, Sharma HK, Shaw CJ, Johnson GV. Efficacy of Hylan G-F 20 and Sodium Hyaluronate in the treatment of osteoarthritis of the knee – a prospective randomized clinical trial. Knee. 2008;15(4):318–324. doi: 10.1016/j.knee.2008.02.012. [DOI] [PubMed] [Google Scholar]
- 20.Kirgs A, Albrecht S. Palsy of the deep peroneal nerve after proximal tibial osteotomy. An anatomical study. J Bone Joint Surg Am. 1992;74(8):1180–1185. [PubMed] [Google Scholar]
- 21.Smith ES, DeLee JC, Ramamurthy S. Ilioinguinal neuralgia following iliac bone-grafting. Report of two cases and review of the literature. J Bone Joint Surg Am. 1984;66(8):1306–1308. [PubMed] [Google Scholar]
- 22.Noyes FR, Goebel SX, West J. Opening wedge tibial osteotomy: the 3-triangle method to correct axial alignment and tibial slope. Am J Sports Med. 2005;33(3):378–387. doi: 10.1177/0363546504269034. [DOI] [PubMed] [Google Scholar]





