Abstract
Objective: The aim of this study was to prospectively evaluate the evolution and postoperative complication patterns relating to the use of suction drains, in comparison with not using these devices in total knee arthroplasty (TKA) procedures. Methods: Forty-two patients at a knee surgery referral clinic were included. Fifteen patients did not receive suction drainage postoperatively and 27 received suction drainage. The parameters evaluated were the range of motion, hematological indices, knee circumference and complication rate. The observation period was for six months after the surgical procedure. Results: There were no statistically significant differences between the groups regarding knee circumference, hemoglobin, hematocrit, transfusion rate or infection index. Regarding range of motion, there was no statistically significant difference between the groups with and without drains preoperatively (p = 0.126), during the first postoperative day (p = 0.583), on the fifth to seventh postoperative day (p = 0.076) or at the six-month follow-up (p = 0.848). There was a statistically significant difference between the groups in the evaluation performed between the 14th and 28th postoperative days (p = 0.025). Conclusion: From this study, it was concluded that there was no benefit from using closed suction drains in TKA cases beyond six months after the operation. However, the range of movement at the end of the first month was greater in the patients that received suction drainage.
Keywords: Arthroplasty, Knee, Drainage Channel, Hemorrhage, Range of Motion, joint
INTRODUCTION
Total knee arthroplasty (TKA) is among the most commonly performed types of orthopedic surgery worldwide. Bleeding is a frequent event, and this mainly originates in the medulla of the bone and occurs after the tourniquet has been released(1).
Since 1961, following the work of Waugh and Stinchfield(2), suction drains have been used in orthopedic surgery3, 4 with the purpose of diminishing the formation of hematomas and the risk of infection.
Once formed, hematomas impair the healing capacity because of increased pressure at the surgical site and consequent reduction of tissue perfusion. The capacity to opsonize bacteria is thus diminished, and this is considered to be a predisposing factor for the appearance of infections(5). Moreover, it is considered that early mobilization is more difficult and postoperative pain is greater when hematomas are formed6, 7, 8, with increased risk of wound dehiscence and formation of fibrosis, thereby leading to joint stiffness9, 10.
On the other hand, drains can act as a source of contamination5, 9, 11 and impede the natural plugging effect that occurs when surgical wounds are simply closed by suturing. For this reason, the blood loss may be greater when drains are used(7).
The aim of the present study was to prospectively evaluate the evolution and postoperative complication patterns relating to the use of suction drains, in comparison with not using these devices in TKA cases.
MATERIALS AND METHODS
Forty-two patients with primary or secondary gonarthrosis were studied. They underwent operations between October 2007 and April 2009. Fifteen patients were included in the group that did not receive drains and 27 patients received drains.
The patients were randomized shortly before closing the operative wound, after achieving hemostasis by means of electrocautery. The groups were defined by means of a draw, by tossing a coin, such that “heads” would indicate the group with a drain and “tails” would indicate the group without a drain.
All the patients signed a consent statement after receiving explanations from the attending physician. Patients with mental deficiencies, those with coagulation disorders and those who did not agree to participate in the study were excluded.
The preoperative preparation consisted of drawing blood for a blood derivative reserve, production of a hemogram and coagulogram, and an assessment of surgical risk by the anesthesiology team. The range of motion (ROM) of the knee to be operated was measured using a goniometer, and the joint circumference was measured, taking the middle third of the patella as the reference. These principles were also used in the postoperative evaluation. Data gathering was undertaken by physicians from the orthopedics service who had received prior training for this (TVOC, LCB and MEA).
All the patients received prophylaxis against thromboembolic events consisting of unfractionated heparin (5,000 UI subcutaneously every eight hours), starting on the day of the surgery, and prophylaxis against surgical site infection consisting of cefazolin (intravenously every eight hours), at a dose adjusted for the patient's weight, for a 24-hour period. All the surgical procedures were carried out by orthopedic surgeons who were members of the knee surgery service. A pneumatic tourniquet, with pressure adjusted according to the patient's systolic arterial pressure, was used during the procedure for a maximum of 120 minutes. The patients received a cemented knee prosthesis (Nex Gen; Zimmer, Inc. Warsaw, IN, USA). Gait training using a walking frame was started on the first or second day after the operation, according to how well the patient tolerated this.
The patients who were drawn for the group with a drain received a Portovac drain (Simon, number 3.2), which was kept in place for a 24-hour period.
The bleeding was assessed from the mean values of the hemoglobin and hematocrit concentrations on the first postoperative day, in comparison with the previous values. The volume of blood that was drained over the first 12 and 24 hours from the patients who received a drain was also measured. These parameters were evaluated in conjunction with the transfusions received by the respective patients. The criterion for transfusion was the presence of clinical signs and symptoms that could be explained as anemia.
Range of motion was assessed on the first and seventh postoperative days, between the 14th and 28th days after the operation and six months after the operation. The joint circumference was measured on the first and seventh postoperative days and between the 14th and 28th days after the operation.
Intercurrences during the hospitalization and postoperative follow-up were recorded.
The data were analyzed by means of the SPSS for Windows software, version 10.0.1. Continuous numerical variables were tested for normality, and the statistical test to be used was proposed accordingly. Variables with normal distribution were compared using Student's t test and ANOVA. Variables with non-normal distribution were compared using the Kruskal-Wallis test.
RESULTS
The patients were evaluated over six months, with periodic consultations in accordance with the protocol described. One patient was not assessed beyond the third postoperative day because of death due to a condition suggestive of pulmonary thromboembolism.
The means for age, length of hospital stay, height, weight, duration of the surgical procedure, hemoglobin/hematocrit, knee circumference and pre and postoperative range of motion are shown in Table 1.
Table 1.
Data gathered before and after the operation on patients who underwent total knee arthroplasty with or without the use of a drain.
| Without drain | With drain | p value | |
|---|---|---|---|
| Number of patients | 15 | 27 | - |
| Age (years) | 69.93 ± 7.11 | 69.00 ± 9.31 | 0.738 |
| Length of hospital stay (days) | 2.31 ± 0.67 | 2.14 ± 0.35 | 1 |
| Height (m) | 1.68 ± 0.06 | 1.61 ± 0.08 | 0.131 |
| Weight (kg) | 74.2 ± 11.76 | 74.6 ± 14.04 | 0.711 |
| Duration (minutes) | 152.78 ± 37.43 | 137.62 ± 19.47 | 0.49 |
| Preoperative hemoglobin (g/dl) | 14.18 ± 2.04 | 14.12 ± 1.54 | 0.914 |
| Preoperative hematocrit (g/dl) | 41.07 ± 4.88 | 42.06 ± 3.83 | 0.421 |
| Postoperative hemoglobin | 10.47 ± 1.74 | 10.12 ± 1.14 | 0.429 |
| Postoperative hematocrit | 30.30 ± 4.26 | 30.60 ± 3.33 | 0.757 |
| Preoperative circumference (cm) | 40.27 ± 3.55 | 40.35 ± 4.66 | 0.962 |
| Postoperative circumference (cm) | 43.05 ± 3.99 | 43.27 ± 4.67 | 0.9 |
| Postoperative circumference on fifthseventh postoperative day (cm) | 43.5 ± 4.94 | 42.09 ± 4.58 | 0.931 |
| Preoperative ROM | 109.26 ± 19.99 | 98.33 ± 24.54 | 0.126 |
| ROM on first postoperative day | 65.67± 18.21 | 69.81 ± 25.36 | 0.583 |
| ROM on seventh postoperative day | 73.85 ± 20.63 | 85.96 ± 18.97 | 0.076 |
| ROM between 14th and 28th days after the operation | 78.64 ± 25.99 | 95.20 ± 14.61 | 0.025* |
| ROM six months after the operation | 109.00 ± 15.17 | 107.08 ± 15.73 | 0.848 |
Continuous variables are expressed as the mean ± standard deviation. ROM: range of motion measured by means of goniometry
p < 0.05
Comparison between the groups regarding the mean knee circumference before the operation (p = 0.962), in the immediate postoperative period (p = 0.900) and on the fifth to seventh postoperative day (p = 0.931) did not reveal any significant difference between the groups.
With regard to the range of motion, there was no statistical difference between the groups with and without drainage before the operation (p = 0.126), on the first postoperative day (p = 0.583), on the fifth to seventh postoperative day (p = 0.076) or six months after the operation (p = 0.848). There was a statistically significant difference between the groups in the evaluation performed between the 14th and 28th days after the operation (p = 0.025). In this case, the patients who received a postoperative suction drain presented a larger range of motion than did the group without a drain. It should be emphasized that this difference started to be shown on the seventh postoperative day, when there was already a tendency towards significance (p = 0.076), with a mean range of motion that was greater in the group of patients that received a drain (Figure 1).
Figure 1.
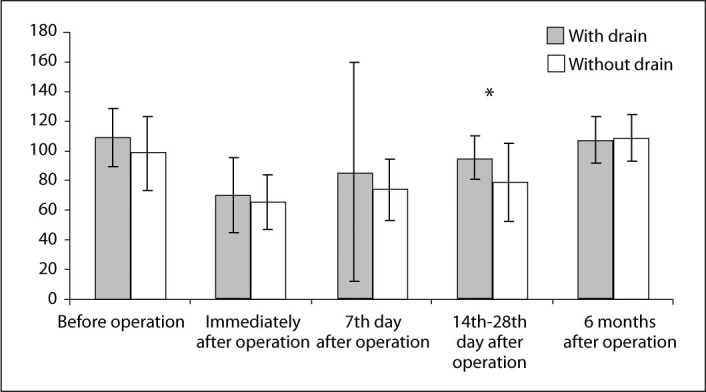
Mean and standard deviation of range of motion in degrees, among patients who underwent total knee arthroplasty with or without the use of a drain, from before the operation to six months after the operation.
In the indirect assessment of blood losses, no statistical difference was seen in the mean pre and postoperative hemoglobin and hematocrit values between the groups. However, comparison between the preoperative hemoglobin and the postoperative hemoglobin (both the general mean and the mean for each group) showed a significant difference (p < 0.000 for all comparisons). Two patients in each group received transfusions, which represented 7.4% of the patients in the group with drains and 13.3% of the patients without drains.
The volume that was drained from the patients who received continuous suction drains was concentrated in the first 12 hours (Figure 2).
Figure 2.
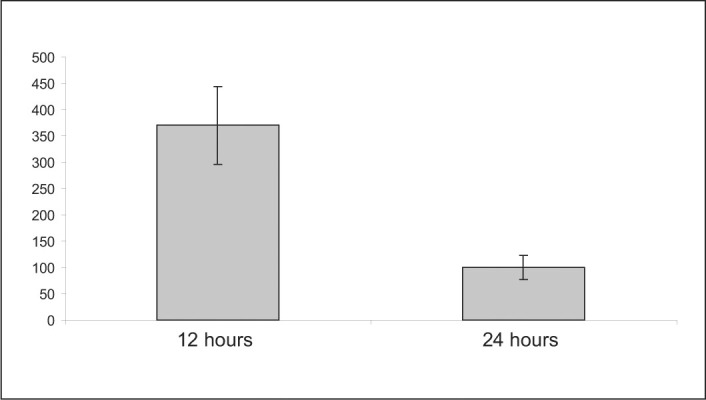
Mean and standard deviation of drainage pattern (ml) among the patients who received suction drains during the postoperative period.
With regard to postoperative complications, there were three cases in the group of patients who received drains that were considered to be serious (dehiscence of the wound during the first week after the operation, deep infection with the need to remove the prosthesis and limitations on flexion). In the group of patients who did not receive drains, there was one death due to suspected pulmonary embolism and one case of a deep infectious process that progressed to the need to remove the prosthesis.
DISCUSSION
The use of drains in knee arthroplasty procedures is a controversial topic3, 4, 7, 8, 10, 12, 13, 14, 15, 16, 17, 18, 19. Many studies have investigated the role of suction drains in preventing postoperative complications in orthopedic surgery, but so far, few conclusions have been reached2, 3, 4, 6, 10, 12, 13, 14, 16, 17, 18, 20, 21. It has been established that in cemented TKA procedures, the risk of hemorrhage is lower than in uncemented procedures and, for this reason, the need to implant drains in such cases has been questioned(13).
The present study showed that using a drain did not modify patients' evolution in relation to the hematological indices. These findings are in agreement with those of Kim et al(15), Esler et al(7) Adalberth et al(10), Ritter et al(3), Beer et al(14), Jenny et al(17) and Niskanen et al(16), who did not perceive any differences in the parameters analyzed between the groups treated with and without a drain, in their prospective studies. A contrary stance was taken by Leb et al, Waugh and Stinchfield(2) and Simpson et al apud Adalberth et al(10), who affirmed that suction drains were useful in orthopedic surgery.
Leb et al(22) used hematocrit as a parameter for estimating blood loss, in a way that was similar to the method used in this study, which used hemoglobin and hematocrit levels for evaluating blood losses.
Porteus and Bartlett(18) took the parameter of bleeding greater than 1,000 ml in cases of uncemented and hybrid knee prostheses and maintained the indication for using drains in these situations. The present study did not show any cases with drainage greater than or equal to such a notable volume, although it should also be borne in mind that all the prostheses were cemented.
A meta-analysis(19) showed that the infection rate in total hip/knee arthroplasty procedures with and without drains were respectively 0.5% and 0.2%. It also showed that there were no differences regarding the reoperation rate, hematomas, dehiscence, increase limb volume, deep vein thrombosis, range of motion, function, length of hospital stay or strength. The only proven advantage from using a drain was the reduction in blood leakage through the operative wound. These data could not be confirmed in the present study because of the size of the sample and the low number of complications.
Kumar et al(23) monitored the drainage performed by continuous suction devices and concluded that most of the drainage occurred during the first 12 hours (on average, 562 ml over the first 12 hours and 627 ml over 24 hours) and that, for this reason, there was no advantage in leaving the devices in place for a longer time. The same drainage pattern was confirmed in the studies by Ritter et al(3), Carvalho Júnior et al(24), Willemen et al(12) and Niskanen et al(16), and in the present study, which arouses interest in a future study to compare the use of drains for 12 and 24 hours.
Comparison of the evolution of range of motion in the two groups showed a statistically significant difference in the evaluation over the period from the 14th to the 28th day after the operation. However, at the six-month evaluation, there was no statistically significant difference. This finding is in agreement with studies by some other authors who contested the need for a drain for achieving better range-of-motion results over the long term3, 4, 7, 8, 10, 12, 13, 14, 15, 16, 17, 18, 19. Greater early range of motion among patients with a drain may be explained by the lower degree of hematoma formation that occurs in these patients. Similar range of motion on the first postoperative days may be due to similar pain levels in the two groups.
CONCLUSION
From this study, it is concluded that there was no benefit in using closed suction drains in TKA cases beyond six months after the operation. However, the range of motion at the end of the first month was greater in the group that used the suction drain.
Footnotes
Work performed at Hospital das Clínicas, Federal University of Minas Gerais.
REFERENCES
- 1.Burke DW, O'Flynn H. Primary total knee arthroplasty. In: Chapman MW, editor. Chapman's orthopaedic surgery. 3rd edition. Lippincott Williams & Wilkins; Philadelphia: 2001. pp. 2870–2895. [Google Scholar]
- 2.Waugh TR, Stinchfield FE. Suction drainage of orthopaedic wounds. J Bone Joint Surg Am. 1961;43(7):939–946. [PubMed] [Google Scholar]
- 3.Ritter MA, Keating M, Faris M. Closed wound drainage in total hip or total knee replacement. J Bone Joint Surg Am. 1994;76(1):35–38. doi: 10.2106/00004623-199401000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Ovadia D, Luger E, Bickels J, Menachem A, Dekel S. Efficacy of closed wound drainage after total joint arthroplasty. J Arthroplasty. 1997;12(3):317–321. doi: 10.1016/s0883-5403(97)90029-2. [DOI] [PubMed] [Google Scholar]
- 5.Alexander JW, Korelitz J, Alexander NS. Prevention of wounds infections. Am J Surg. 1976;132(1):59–63. doi: 10.1016/0002-9610(76)90291-9. [DOI] [PubMed] [Google Scholar]
- 6.Bryan RS, Dickson JH, Taylor W. Recovery of the knee following meniscectomy. J Bone Joint Surg Am. 1969;51(5):973–978. [PubMed] [Google Scholar]
- 7.Esler CNAC, Blakeway C, Fiddian NJ. The use of a closed-suction drain in total knee arthroplasty. A prospective randomized study. J Bone Joint Surg Br. 2003;85(2):215–217. doi: 10.1302/0301-620x.85b2.13357. [DOI] [PubMed] [Google Scholar]
- 8.Parker MJ, Roberts CP, Hay D. Closed suction drainage for hip and knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2004;86(6):1146–1152. doi: 10.2106/00004623-200406000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Raves JJ, Slifkin M, Diamond DL. A bacteriologic study comparing closed suction and simple conduit drainage. Am J Surg. 1984;148(5):618–620. doi: 10.1016/0002-9610(84)90336-2. [DOI] [PubMed] [Google Scholar]
- 10.Adalberth G, Byström S, Kolstad K, Mallmin H, Milbrink J. Postoperative drainage of knee arthroplasty is not necessary: a randomized study of 90 patients. Acta Orthop Scand. 1998;69(5):475–478. doi: 10.3109/17453679808997781. [DOI] [PubMed] [Google Scholar]
- 11.Magee C, Rodeheaver G, Golden GT, Edgerton MT, Edilich RF. Potentiation of wound infection by surgical drains. Am J Surg. 1976;131(5):547–549. doi: 10.1016/0002-9610(76)90007-6. [DOI] [PubMed] [Google Scholar]
- 12.Willemen D, Paul J, White SH, Crook DW. Closed suction drainage following knee arthroplasty. Effectiveness and risks. Clin Orthop Relat Res. 1991;(264):264–274. [PubMed] [Google Scholar]
- 13.Mylod AG, Jr, France MP, Muser DE, Parsons JR. Perioperative blood loss associated with total knee arthroplasty. A comparison of procedures performed with and without cementing. J Bone Joint Surg Am. 1990;72(7):1010–1012. [PubMed] [Google Scholar]
- 14.Beer KJ, Lombardi AV, Jr, Mallory TH, Vaughn BK. The efficacy of suction drains after routine total joint arthroplasty. J Bone Joint Surg Am. 1991;73(4):584–587. [PubMed] [Google Scholar]
- 15.Kim YH, Cho SH, Kim RS. Drainage versus nondrainage in simultaneous bilateral total hip arthroplasties. J Arthroplasty. 1998;13(2):156–161. doi: 10.1016/s0883-5403(98)90093-6. [DOI] [PubMed] [Google Scholar]
- 16.Niskanen RO, Korkala OL, Haapala J, Kuokkanen HO, Kaukonen JP, Salo SA. Drainage is of no use in primary uncomplicated cemented hip and knee arthroplasty for osteoarthritis: a prospective randomized study. J Arthroplasty. 2000;15(5):567–569. doi: 10.1054/arth.2000.6616. [DOI] [PubMed] [Google Scholar]
- 17.Jenny JY, Boeri C, Lafare S. No drainage does not increase complication risk after total knee prosthesis implantation: a prospective, comparative, randomized study. Knee Surg Sports Traumatol Arthrosc. 2001;9(5):299–301. doi: 10.1007/s001670100220. [DOI] [PubMed] [Google Scholar]
- 18.Porteus AJ, Bartlett RJ. Post-operative drainage after cemented, hybrid and uncemented total knee replacement. Knee. 2003;10(4):371–374. doi: 10.1016/s0968-0160(03)00002-4. [DOI] [PubMed] [Google Scholar]
- 19.Parker MJ, Livingstone V, Clifton R, Mackee A. Closed suction surgical wound drainage after orthopaedic surgery. Cochrane Database Syst Rev. 2007;(3):CD001825. doi: 10.1002/14651858.CD001825.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Browett JP, Gibbs AN, Copeland SA, Deliss LJ. The use of suction drainage in the operation of meniscectomy. J Bone Joint Surg Br. 1978;60(4):516–519. doi: 10.1302/0301-620X.60B4.711799. [DOI] [PubMed] [Google Scholar]
- 21.Nixon J. Wound drainage the long term results after primary hip and knee arthroplasty. J Bone Joint Surg. 2000;82(Suppl 2):125. [Google Scholar]
- 22.Leb RB, Parker RD, Cohn BT, Fabian V. The efficacy of closed suction drainage in total knee arthroplasty. Orthop Trans. 1995;19:332–333. [Google Scholar]
- 23.Kumar S, Penematsa S, Parekh S. Are drains required following a routine primary total joint arthroplasty? Int Orthop. 2007;31(5):593–596. doi: 10.1007/s00264-006-0245-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carvalho Júnior LH, Paiva EB, Campos LVM, Andrade MAP, Lemos WG, Pinheiro Júnior LFB. Drenagem pós-operatória após artroplastia total do joelho. Rev Bras Ortop. 1998;33(8):659–661. [Google Scholar]


