Abstract
Objective: To evaluate the preliminary results from the METIS-Newdeal® metatarsophalangeal prosthesis for treating hallux rigidus grade III/IV. Methods: This was a prospective study on eight metatarsophalangeal prostheses that were placed in six patients between November 2007 and July 2009. The patients' mean age was 55 years and the mean follow-up after the surgery was 50 weeks. The results were evaluated using the AOFAS-MTP score and x-ray images as controls. Results: The AOFAS-MTP score increased significantly from 42p before the surgery to 82p after the surgery (↑ 1.95x), mainly due to improvement in the functional level. No intercurrences were identified radiologically. Among the five patients who underwent operations, only one expressed dissatisfaction with the surgery: this was expressed after early infection appeared at the surgical site, and it was the only postoperative complication found. Conclusion: Total metatarsophalangeal arthroplasty using METIS-Newdeal® presented promising short-term results. However, evaluations on a larger number of cases with a longer follow-up are needed in order to draw more consistent conclusions.
Keywords: Hallux Rigidus, Metatarsophalangeal Joint, Arthroplasty
INTRODUCTION
Degenerative pathology of the first metatarsophalangeal (MTP) joint, known as hallux rigidus, was first described in 1887 by Davies-Colley-Cotterill apud Faraj(1) and involves progressive loss of joint range of motion, pain on mobilization (especially in dorsiflexion) and deformity. It affects about 2% of the population aged over 50 years(2), is prevalent among females, and is associated with the first long metatarsal, flat MTP joint, and a history of hyperextension injury.
Several therapeutic options are available depending on the degenerative stage of the MTP joint, which may include conservative supporting measures through to surgical procedures, such as cheilectomy, phalangeal or first metatarsal osteotomy, Keller procedure or MTP arthrodesis. MTP arthroplasty was first proposed in the late 19th century by Heuter, using an acrylic prosthesis(3). Since then various evolutions of the procedure have been presented. In 1979, Swanson proposed the use of the interposition silicone prosthesis (Silastic®)(4). However, these prostheses presented several complications, including fracture of the prosthesis and synovitis and bone lysis related to worn particles of silicone5, 6, 7. In 1994, the use of zirconium ceramic components (Moje®) was tested, but these materials also presented several complications, particularly due to fracture of the material2, 8, 9.
Other materials and solutions were proposed in an attempt to find a prosthesis model that would replicate the anatomy and biomechanics of the normal joint, and at the same time, enable long-lasting use.
This work presents the preliminary results of eight MTP arthroplasties performed at the Centro Hospitalar do Porto – Hospital de Santo António (CHP-HSA), using the METIS-Newdeal® prosthesis, with anaverage follow-up period of 50 weeks.
MATERIAL AND METHODS
The prosthesis
The METIS® prosthesis consists of three components: metatarsal (cobalt-chromium alloy), phalangel (titanium), and a third-generation interposition component composed of polyethylene. Metatarsal and phalangeal components are coated with hydroxyapatite. The design seeks to preserve the normal anatomy of the MTP joint, preserving the sesamoid bones and their tendinous insertions, with an expected range of motion of about 85° (-20:0:60) (Figure 1).
Figure 1.

The METIS-Newdeal® prosthesis.
The trial
A prospective trial was conducted between November 2007 and July 2009 to evaluate the clinical and functional results of eight total MTP arthroplasties using the METIS® prosthesis in six patients at the CHP-HSA. Two patients were submitted (in different surgical times) to bilateral arthroplasty. For all the patients, the surgery was indicated due to painful hallux rigidus with major functional limitation (Coughlin grades 3 and 4). The patient group consisted of four male and two female patients, with an average age of 55 years (42-63) at the time of surgery. The main comorbidity was diabetes mellitus affecting two patients who were being treated for that pathology.
All the patients were evaluated before the surgery using the AOFAS-MTP (American Orthopaedic Foot & Ankle Society) score for the metatarsophalangeal joint, which ranges between 0 and 100 points and evaluates parameters such as pain (40p), function (45p) and alignment (15p).
All the surgeries were performed by the same surgeon, using the same surgical technique. In the immediate postoperative period, the patients were encouraged to perform passive and active movements (as tolerated), followed by two weeks of walking with partial weight-bearing, using Baruk shoes with crutch support. The first observation in an outpatient clinic was made on day 15 when the stitches were removed. Six weeks after the surgery, a follow-up radiography was taken to evaluate the integration and alignment of the prosthesis, and the collection of information began, to complete the AOFAS-MTP score. The patients were also asked to report their satisfaction in relation to the surgery by stating whether they would undergo the surgery again. The average follow-up time was 50 weeks (13-64).
RESULTS
Preoperative results
The AOFAS-MTP score had an average of 42 points (12-52), with partial scores of: pain (19p), function (15p) and alignment (8p). Before surgery, all the patients reported expectations of decreased pain and improved walking ability as decisive factors in their decision to undergo surgery.
Postoperative results
On reassessment in the outpatient clinic, there was a significant increase in the average AOFAS-MTP score, to 82 points (50-95) (Figure 2). Analyzing this score, an increase was observed in all the partial scores: pain (33p), function (36p) and alignment (14p). The results were most evident at the function level, for which the point increase was 2.4 times higher, compared with the preoperative scores (Table 1).
Figure 2.
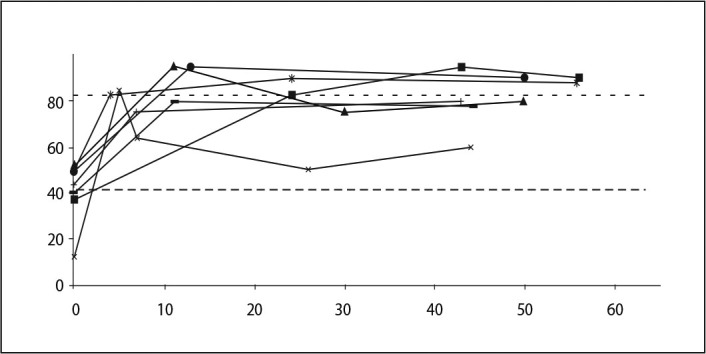
Analysis of the AOFAS-MTP score.
Table 1.
Partial and total values of the AOFAS-MTP scale
| Preop. | Postop | Range | |
|---|---|---|---|
| Pain | 19 | 33 | ↑1.73x |
| Function | 15 | 36 | ↑2.4x |
| Alignment | 8 | 14 | ↑1.75x |
| AOFAS-MTP | 42 | 82 | ↑1.95x |
In the radiological analysis, none of the implants showed signs of early suture, fracture or problems of misalignment of the components (Figure 3).
Figure 3.

Radiographic image after surgery.
Regarding the patients' level of satisfaction after surgery, only one patient reported being disappointed with the results, owing to an infectious complication that affected the results.
Complications
One patient had an intraoperative complication in which the proximal phalange of the hallux was fractured. However, this fracture did not prevent the completion of the surgery, and no modification to the postoperative protocol used was needed. In the follow-up, the results were similar to those of patients without any complications.
One patient had infection at the surgery site seven weeks after surgery. The patient was treated immediately with oral antibiotics (amoxicillin + clavulanate) and was apparently cured. In relation to the results, in the first seven weeks the patient showed an improvement in the AOFAS-MTP score in relation to their preoperative score; after the infection, the score decreased dramatically, and this patient had the worst results of the study group. This was also the only patient who reported being disappointed with the surgery, stating that they would never undergo the procedure again.
DISCUSSION
Depending on the degree of the hallux rigidus, cheilectomy, Keller procedure and MTP arthrodesis are considered the gold standard treatment for this pathology. Despite showing good results in many cases, these procedures are not without failures and complications. Cheilectomy has been used with good results for pain relief only in the initial stages, when the joint space and the range of mobility are preserved, or it is limited to pain on dorsiflexion only(10). However, it is not recommended for more advanced conditions. In patients who already have significant MTP joint destruction, resection of the proximal portion of the first phalange (Keller procedure) or MTP arthrodesis are the traditional options. Although the Keller procedure preserves an acceptable range of MTP motion, it does so at the expense of losing driving force when walking, and is not indicated for younger or active middle-aged patients. In the long term, the development of central transfer metatarsalgia in about 30% of patients(11) or swan neck deformity, can cause problems with the use of standard footwear. Arthrodesis of the first MTP is considered by many as the treatment to be adopted for young or active patients because it has positive results in the long term, in relieving pain and preserving the transfer of driving forces to the hallux, even enabling the practice of certain sports activities(12). However, studies have shown that this is a surgery that has a high failure rate in first metatarsophalangeal joint fusion (> 20%)(1) and although a successful arthrodesis does not usually require surgical revision, this joint fusion alters the biomechanics of the forefoot. Many patients develop calluses under other metatarsal heads, due to weight transfer, and pain is often experienced in the hallux interphalangeal joint(1). Many patients also report that although they are able to perform daily activities with less pain, they can no longer wear regular footwear. This is predominantly reported by young female patients (26%) – they are no longer able to wear high heels – and individuals who are frequently required to adopt a squatting position.
MTP arthroplasty has the advantage that it offers relief of symptoms, keeping the anatomy and transfer of force as close to normal as possible.
Historically, several models of MTP prosthesis have been proposed. However, all of these models had complications that prevented their use as an ongoing treatment of hallux rigidus.
The silicone prostheses were first introduced in 1979 by Swanson et al(4). In studies to evaluate the results of these prostheses (Silastic®), we found wide variability in the conclusions, ranging from long-term success13, 14 to early failure. Shankar(5), in 1995, presented a trial involving 40 patients with an average follow-up period of 110 months, in which the complication rate was 36%, mainly due to fragmentation of the silicone. A high incidence of granulomatous reactions to silicone particles is also reported in about 72% of patients, and causes significant osteolysis6, 7.
In 1994, Townley and Taranow(15) developed a phalangeal hemiarthroplasty prosthesis made from titanium. However, the results were similar to those of older silicone prostheses, and they did not live up to the expectations(16). Raikin et al(17) presented a study comparing the results of 21 hemiarthroplasties and 27 MTP arthrodeses in an average follow-up period of 79 months. No advantages were found for performing hemiarthroplasty.
In 2002, the Medical Devices Agency of the UK issued a warning that led to the recall of the Moje® screw-fit prostheses, due to its high failure rate(2). In 2003, Redfern et al(8) published a review of 119 patients whose results at the first year were alarming, with 14% of surgical revisions and 5% of prostheses with significant but asymptomatic osteolysis. This prosthesis suffered changes, and the press-fit system came to be used as the means of bone fixation/integration. Malviya et al(18) showed positive results with this new Moje system, in a 35-month follow-up study. However, other studies report cases of failure of the Moje® press-fit prosthesis, due to problems with the materials used (zirconium ceramic)(9). In 2007, Nixon and Taylor(2) published the results of a study involving 21 prostheses, in which they found an unacceptable failure rate of around 29% requiring surgical revision and a complication rate of 71% within three years.
After the problems with the first prostheses, a new model of non-restrictive and anatomic prosthesis was introduced on the market. In 2001, Notni et al(19) evaluated the results of the ReFlexion® prosthesis (similar to METIS®), and found a significant reduction in pain and a high level of patient satisfaction after the surgery. These good results were supported by Fuhrmann(20) in 2005, who found an increase in the average AOFAS score from 51p (before surgery) to 74p (after surgery), in a follow-up period of 39 months using the same prosthesis. Nevertheless, both authors verified the existence of periprosthetic image in half of the prostheses without clinical reference.
Analyzing the METIS® prosthesis, its advantages are the fact that the prosthesis maintains the metatarsophalangeal joint function and range of motion within the normal anatomical standards; the excellent clinical and functional results obtained in this study, with an increase in the average AOFAS-MTP score from 42 to 82 (+40p); and the high level of patient satisfaction with the final result. Its disadvantages are the cost of the prosthesis (> ε 1000) compared with other simpler and cheaper procedures (Keller procedure, arthrodesis), and the fact that the implant requires a more demanding and time-consuming surgical technique and a longer learning period.
We may suggest some modifications to the trial, given that it is still in its initial phase, with little follow-up time, and few cases under evaluation. The patients will be assessed in an outpatient basis at irregular times, and the results may be influenced by the learning curve of the surgeon and the surgical team.
CONCLUSION
The total metatarsophalangeal joint arthroplasty using the METIS-Newdeal® prosthesis appears to be a valid alternative for the treatment of the pathologies affecting this joint. However, more data and a longer follow-up period are needed to obtain conclusive and statistically significant results. A long-term comparison of our results with those obtained from traditional approaches will also be necessary.
Footnotes
Work carried out at the Orthopedics and Traumatology Service of the Centro Hospitalar do Porto - Hospital de Santo António, EPE, Porto - Portugal.
The authors declare that they did not have any conflict of interests in producing this article
REFERENCES
- 1.Faraj A. Management of hallux rigidus. Curr Orthop. 2008;22(6):422–427. [Google Scholar]
- 2.Nixon MF, Taylor GJS. Early failure of the Moje implant when used to treat hallux rigidus: the need for regular surveillance. Foot. 2008;18(1):1–6. [Google Scholar]
- 3.Fadel G, Sripada S, Abboud R, Jain AS. Ceramic implant arthroplasty of the hallux: early results. Foot Ankle Surg. 2005;11(3):149–153. [Google Scholar]
- 4.Swanson AB, Lumsden RM, Swanson GD. Silicone implant arthroplasty of the great toe. A review of single stem and flexible hinge implants. Clin Orthop Relat Res. 1979;(142):30–43. [PubMed] [Google Scholar]
- 5.Shankar NS. Silastic single-stem implants in the treatment of hallux rigidus. Foot Ankle Int. 1996;17(2):145–151. doi: 10.1177/107110079501600805. [DOI] [PubMed] [Google Scholar]
- 6.Moeckel BH, Sculco TP, Alexiades MM, Dossick PH, Inglis AE, Ranawat CS. The double-stemmed silicone-rubber implant for rheumatoid arthritis of the first metatarsophalangeal joint. Long-term results. J Bone Joint Surg Am. 1992;74(4):564–570. [PubMed] [Google Scholar]
- 7.Rahman H, Fagg PS. Silicone granulomatous reactions after first MTF hemiarthroplasty. J Bone Joint Surg Br. 1993;75(4):637–639. doi: 10.1302/0301-620X.75B4.8331122. [DOI] [PubMed] [Google Scholar]
- 8.Redfern DJ, Coleridge SD, Bendall SP. Early failure of the Moje screw-fit ceramic MTF joint replacement. Foot. 2003;13(4):204–208. [Google Scholar]
- 9.Pavier J. A catastrophic failure of a first MTF joint ceramic implant: Case report. Foot. 2005;15(1):47–49. [Google Scholar]
- 10.Harttrup SJ, Johnson KA. “Subjective results of hallux rigidus following treatment with cheilectomy. Clin Orthop Relat Res. 1988;(226):182–191. [PubMed] [Google Scholar]
- 11.Hamilton WG, O'Malley MJ, Thompson FM, Kovatis PE. “Capsular interposition Arthroplasty for severe hallux rigidus”. Foot Ankle Int. 1997;18(2):68–70. doi: 10.1177/107110079701800204. [DOI] [PubMed] [Google Scholar]
- 12.Maher AJ, Metcalfe SA. First MTP joint arthrodesis for the treatment of hallux rigidus: results of 29 consecutive cases using the foot health status questionnaire validated measurement tool. Foot (Edinb) 2008;18(3):123–130. doi: 10.1016/j.foot.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 13.Smetana M, Vencálková S. [Use of a silicone metatarsophalangeal joint endoprosthesis in hallux rigidus over a 15-year period] Acta Chin Orthop Traumatol Cech. 2003;70(3):177–181. [PubMed] [Google Scholar]
- 14.Jain SA, Banerjee BC. Silastic flexible hinge implant arthroplasty of the great toe for hallux rigidus. A retrospective analysis The Internet Journal of Orthopedic Surgery. 2008;9(2) [Google Scholar]
- 15.Townley CO, Taranow WS. A metallic hemiarthroplasty resurfacing prosthesis for the hallux metatarsophalangeal joint. Foot Ankle Int. 1994;15(11):575–580. doi: 10.1177/107110079401501101. [DOI] [PubMed] [Google Scholar]
- 16.Leavitt KM, Nirenberg MS, Wood B, Yong RM. Titanium hemi-great toe implant: a preliminary study of its efficacy. J Foot Surg. 1991;30(3):289–293. [PubMed] [Google Scholar]
- 17.Raikin SM, Ahmad J, Pour AE, Abidi N. Comparison of arthrodesis and metallic hemiarthroplasty of the hallux metatarsophalangeal joint. J Bone Joint Surg Am. 2007;89(9):1979–1985. doi: 10.2106/JBJS.F.01385. [DOI] [PubMed] [Google Scholar]
- 18.Malviya A, Udwadia A, Doyle J. Pressfit ceramic arthroplasty of the first metatarsophalangeal joint: a short-term review. Acta Orthop Belg. 2004;70(5):455–460. [PubMed] [Google Scholar]
- 19.Notni A, Fährmann M, Fuhrmann RA. [Early results of implantation of an unconstrained metatarsophalangeal joint prosthesis of the first toe] Z Orthop Ihre Grenzgeb. 2001;139(4):326–331. doi: 10.1055/s-2001-16919. [DOI] [PubMed] [Google Scholar]
- 20.Fuhrmann RA. MTP Prosthesis (ReFlexion™) for Hallux Rigidus. Techn Foot Ankle Surg. 2005;4(1):2–9. [Google Scholar]


