Abstract
Gorham-Stout syndrome is a disease that presents idiopathic osteolysis of a bone or closely contiguous area. The etiology is unknown. It is a rare condition that is difficult to diagnose, and its treatment is controversial. It affects individuals irrespective of age or sex. In this study, we conducted a bibliographic review of the disease, specifically focusing on the differential diagnosis, and we demonstrated the follow-up on a patient with this syndrome from the time of its diagnosis, through treatment, to its current state of evolution.
Keywords: Essential Osteolysis/etiology, Osteolysis/diagnosis, Osteolysis/radiography, Clavicle
INTRODUCTION
The term osteolysis indicates a reduction in the quantity of bone tissue seen on radiographs. This condition can be caused by a large number of known lesions, but there are few cases of idiopathic osteolysis.
In 1838, Jackson(1) described complete osteolysis of the humerus in a 12-year-old boy. In 1955, Gorham and Stout(2) reported the main pathological characteristics of what was named “disease of the disappearing bone with intraosseous vascular abnormalities”. Since then, this disease has been called Gorham syndrome, Gorham-Stout syndrome, massive osteolysis, idiopathic osteolysis, disappearing bone disease, phantom bone disease, spontaneous bone absorption, progressive bone atrophy or bone hemangiomatosis and lymphangiomatosis. Fewer than 200 cases have been described in the literature(3).
Gorham-Stout syndrome presents in the form of osteolysis of a bone or a contiguous bone area close to the focus, without respecting joint limits. Pit may affect any portion of the skeleton, but it is single-centered. The structures most involved are the bones of the cranium and the scapular and pelvic belts2, 4, 5, 6. It is a rare disease, of unknown etiology, in which osteolysis begins through proliferation of vascular structures originating in the bone tissue, thereby causing destruction of the bone matrix(7).
This condition may present at any age, but it is generally recognized in children and young adults. There is no predilection for sex or any pattern of genetic inheritance8, 9. So far, there have not been any cases with a family history(4). It is known that there is a history of associated trauma in 57% of the cases(7).
In relation to the clinical condition, it does not present major symptoms, although the appearance of the radiological condition is much worse than that of the clinical condition. During the acute phase, patients complain of pain, edema, progressive deformity and contractures. Nevertheless, the function of the limb affected remains remarkably good. Laboratory tests are generally normal and help physicians to rule out other diagnoses. Alkaline phosphatase may be elevated when patients present fractures(10).
The involvement tends to be contiguous, without occurrences of multiple foci or metastases. There is one documented case of malignant degeneration that occurred in a patient with a diagnosis of hypernephroma(11).
Deaths caused by the disease have occurred in patients in whom the process was localized in the costal arches, mandible or vertebrae, thereby leading to fatal respiratory complications, airway obstruction or compression of the spinal medulla4, 12, 13. It is common for the osteolysis to stop spontaneously after years of bone destruction(2). The final result is deformity and functional impotence.
Chylothorax is a rare complication, although it is serious and is associated with osteolysis of the scapular belt or the thoracic spine(9). It results from impairment of the thoracic duct, or communication between lymphatic dysplasia and the pleural cavity. It is frequently fatal and progresses with lymphopenia, malnutrition and superimposed opportunistic infections(14).
On radiographs of the long bones, the phenomenon starts with intramedullary and subcortical foci of radiolucency, resembling a condition of unequal osteoporosis. It has slow and irregular progression, with concentric reduction of the diaphysis of the bones, tapering to the extremities involved and causing the complete disappearance of the bone, unless if spontaneous remission occurs(4-6,10,12). Pathological fractures may occur, and they rarely consolidate. Thus, the osteolytic process continues through the fragments4, 15, 16. One typical and notable finding is the absence of sclerosis or osteoblastic reaction.
Axial computed tomography (ACT) is useful for delimiting the extent of the soft tissues, as well as enabling guided biopsy. ACT with three-dimensional (3D) reconstruction aids in surgical planning for reconstructions(17).
Lymphangiography can be used to evaluate the impairment of the thoracic duct in patients with chylothorax. The lymphatic vessels and lymph nodes have normal appearance, although the abnormal lymphatic flow may lead to obstruction and edema(18).
Angiography depicts the absence of neovascularization in the area involved, and scintigraphy shows normal uptake throughout the skeleton, or increased uptake in the areas involved18, 19.
Magnetic resonance imaging (MRI) demonstrates the morphological disappearance of the bone, and areas with increased or decreased signal that represent hemorrhages at different stages(18).
The differential diagnosis of Gorham syndrome includes bone hemangioma, angiosarcoma, essential osteolysis and hereditary osteolysis. The radiographic pattern is very similar, but in these other diseases, there are no occurrences of major effusion and other pulmonary alterations(3).
Skeletal hemangiomas may cause osteolysis and present histological characteristics that are very similar to Gorham syndrome. However, hemangiomas present limited growth, with a tendency to preserve cortical bone stocks, and do not present dissemination to the adjacent soft tissues(3).
Angiosarcomas, even when well differentiated, present focal cell atypia and endothelial cells with a tendency to proliferate. On the other hand, in Gorham syndrome, the vessels present a single layer of endothelial cells1, 7.
Essential osteolysis causes carpal and/or tarsal bone reabsorption and evolves with progressive renal failure but without vascular changes. On the other hand, hereditary osteolysis occurs during infancy and is presented mainly on the hands and feet, also without evolving to vascular changes(3). Thus, through the multicenter nature of these diseases, the differential diagnosis with the disease of the present study can be made. Other possible causes of osteolysis come from systemic diseases such as rheumatoid arthritis, syphilis, hyperparathyroidism, multiple myeloma and lymphoma. However, the histological evaluation differs from the abnormalities seen in patients with Gorham syndrome(7).
Treatment for Gorham syndrome should be instituted when the process is progressive and the osteolysis is extensive. It is based on local resection, with or without the use of prosthetics, radiotherapy or amputation. Incomplete resection of the lesion is rarely curative, and the process of bone lysis is perpetuated20, 21. Immobilization does not change the prognosis, nor does administration of estrogen, androgen, magnesium, calcium, adrenergic extracts, vitamin D, aluminum solution, ultraviolet radiation, somatotrophin, placental extracts, vitamin B12, amino acids or blood transfusion for growing children22, 23, 24.
Because of the rarity of this disease, we describe below the report on a case of a patient with Gorham-Stout syndrome.
CASE REPORT
The patient was a boy born on August 20, 1996, who was attended for the first time by the senior author (OL) at the age of 12 years, with a history of medical followup since the age of six years. There were no abnormalities during early childhood, or any previous diseases. In 2002, at the age of six years, he suffered a condition of falling from his own height in which he fractured his left clavicle. The treatment was administered by an orthopedist in a conservative manner, by means of immobilization with a bandage in a “posterior figure-of-eight” and reports of bone consolidation with formation of bone callus.
One year later, he had another fall from his own height, with a new fracture of the clavicle, close to the site of consolidation of the anterior fracture. Conservative treatment was again implemented, with immobilization in a sling and consolidation of the fracture.
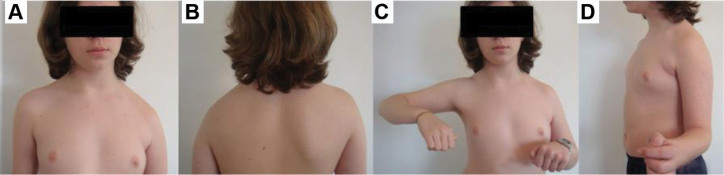
In 2004, then at the age of eight years, he suffered direct trauma on the left shoulder, which resulted in a new fracture of the clavicle and treatment similar to the previous occasions. During a consultation three weeks after the third fracture of the clavicle, the radiographs showed “disappearance” of part of the left clavicle (Figure 1). The medical team monitoring the case produced radiographs of the cranium, pelvis and spine, which were seen to be normal. Because of the suspicion of malignant disease, the team completed the staging of the lesion by requesting ACT, MRI and biopsy. MRI demonstrated that there was no impairment of the soft tissues and the biopsy material showed histopathological abnormalities suggestive of “bone angioma”.
Figure 1.
Evolution of osteolysis of the left clavicle caused by Gorham-Stout disease. Radiographs of the clavicle produced in February 2004 (A), September 2004 (B) and January 2005 (C), showing the rapid evolution of the osteolysis.
From the patient's history and the results from the examination, a diagnosis of Gorham-Stout disease was reached. From then onwards, yearly follow-up by means of physical and radiographic examinations was proposed. Regarding treatment, the patient was encouraged to reinforce the musculature of the left upper limb by means of swimming classes.
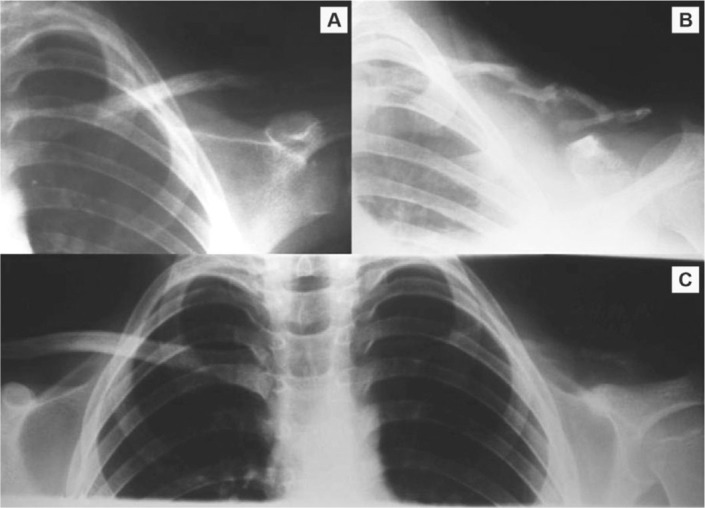
The follow-up was continued for three years until, in 2008, at the age of 12 years, the radiological evaluation showed that the pattern of osteolysis of the clavicle had stabilized, although the radiographs showed lesions in the upper part of the left scapula. ACT and MRI confirmed the presence of osteolytic lesions in the scapula as far as the glenoid mass, coracoid and acromion (Figure 2). Electroneuromyography produced normal results. Clinically, the patient went on presenting functional impotence with limitation of the range of motion of the left shoulder, without any clinical abnormality of reduced pulmonary ventilation.
Figure 2.

Current radiographic image showing the impairment of the scapula with foci of osteolysis (A). Axial computed tomography scan with 3D digital reconstruction, showing intense osteolysis in the left clavicle and foci of associated impairment of the scapula (B).
Currently, the evolution of the osteolysis seems to have become stationary. The treatment instituted at present consists of physiotherapy and hydrotherapy, focused on muscle strengthening for the stabilizers of the scapula, rotator cuff and deltoid, mainly aimed towards maintaining the range of motion. The patient is continuing to receive anti-reabsorption therapy by means of intake of bisphosphonate and calcitonin. Follow-up consultations are expected to be held every three months, in order to observe and reassess the patient's condition. His clinical condition can be seen in the clinical images (Figure 3).
Figure 3.
Current clinical images of the patient, showing significant collapse of the left scapular belt. (A) anterior view at rest, (B) posterior view, (C) incapacity to perform abduction, (D) left-side lateral view in external rotation.
DISCUSSION
Gorham-Stout syndrome should be diagnosed on the basis of the clinical history, radiographic images and, especially, knowledge of the disease. Among the various possible causes of secondary osteolysis, it needs to be differentiated from diffuse atrophy, algodystrophy, primary and metastatic tumors, hyperparathyroidism, gout, congenital pseudarthrosis, granulomatous diseases, rheumatoid arthritis, diabetes mellitus, psoriatic arthritis, osteomyelitis, systemic mastocystosis, aseptic necrosis, neurogenic arthropathy, prolonged therapy with corticoids, aneurysmatic bone cysts and bone hemangiomatosis(25). Idiopathic osteolysis forms a heterogenous group of rare diseases. Hardegger et al(26) proposed a classification for these conditions composed of five types (Table 1).
Table 1.
Classification of idiopathic osteolysis according to Hardegger et al(26).
| Types | |
|---|---|
| 1. Hereditary multicenter osteolysis with dominant transmission | Between two and six years of age, spontaneous pain and edema begin in the hands and feet, with carpotarsal osteolysis. Progression ceases during adolescence. |
| 2. Hereditary multicenter osteolysis with recessive transmission | Similar to type 1, but may be associated with severe generalized osteoporosis. |
| 3. Non-hereditary multicenter osteolysis with nephropathy | Appears during infancy. Gradually disappears from the carpal and tarsal bones, but to a lesser degree and associated with proteinuria. Death occurs due to kidney failure or malignant hypertension. |
| 4. Gorham-Stout syndrome | Single-center occurrence in any part of the skeleton. Can start at any age. Hemangiomatous tissue is usually found at the foci of osteolysis. It is not hereditary and is not associated with nephropathy. The osteolysis usually ceases after some years. |
| 5. Winchester syndrome | Rare recessive autosomal syndrome. Carpotarsal osteolysis associated with contractures, reduced height, skin lesions, abnormalities in the cornea and osteoporosis without nephropathy. |
Source: Hardegger F, Simpson LA, Segmueller G. The syndrome of idiopathic osteolysis: classification, review and case report. J Bone Joint Surg Br. 1985;67:89-93
There are several published papers in which patients who did not fit into any of the five types of this classification method have been described. White described four patients with multifocal osteolysis associated with severe skin lesions(27). Beals and Bird(28) observed a case of carpotarsal osteolysis without nephropathy or any hereditary pattern.
The patient described in the present case report had a condition of single-center osteolysis that began during childhood, without any family history of osteolytic lesions or nephropathy. Using the Hardegger classification, we came to the conclusion that this was a type 4 case, i.e. Gorham-Stout syndrome.
The exact pathogenic mechanism for this disease is still unknown. There is controversy regarding whether osteoclasts might be present at the focus of the lesion. Spieth et al believed that the reabsorption was specifically caused by osteoclasts(29).
There is a large variety of explanations for the pathogenesis. Among these, we can cite the presence of a silent hamartoma that becomes active and starts the reabsorption after small-scale trauma. Some authors have believed that angiomatosis is responsible for the entire condition2, 11. Others have described neurovascular abnormalities, like those seen in the atrophy of Sudeck(30). Thompson and Shurman(31) suggested that the disease is a primary aberration of the bone vascular tissue, associated with granulation tissue. Young et al(32) believed that the osteolysis can be attributed to endothelial dysplasia of lymphatic and blood vessels.
Since osteoclasts are the only cells capable of reabsorbing bone, it can be taken that Gorham-Stout syndrome may pathologically represent a disarrangement of osteoclastic activity. These osteoclasts are stimulated through paracrine or autocrine action, thereby reabsorbing the bone tissue, which subsequently is exchanged for vascularized fibrous tissue. Therefore the apparent contradiction regarding the presence or absence of these cells in the disease can be explained by the different phases of the syndrome(25).
It seems to be sensate to provide treatment for patients with this disease using anti-reabsorptive therapy such as bisphosphonates and calcitonin, which should be started at an early stage, in an attempt to reduce the progression of the osteolytic process(25). However, there is still a lack of studies to prove these data, given the rarity of the syndrome.
Another therapeutic possibility consists of the use of radiotherapy. Carneiro and Steglich reported a case of a female patient with progressive osteolysis in the metacarpals, in which stabilization of the evolution for four months after a cycle of 21 days of radiotherapy using 2,400 rads reinforced the idea of performing bone grafts at the foci of the osteolysis(33). However, the disease continued its progression and reabsorbed all of the graft material used. The case described by those authors had a pause in its progression. In severe cases, with pulmonary or neurological complications, surgical treatment for resection of the diseased tissue is indicated, in an attempt to stop the progression of the disease.
Footnotes
Work performed at the Institute of Orthopedics and Traumatology, Passo Fundo, RS.
REFERENCES
- 1.Jackson JB. A boneless arm. Boston Med Surg J. 1838;18:368–369. [Google Scholar]
- 2.Gorham LW, Stout AP. Massive osteolysis (acute spontaneous absorption of bone, phantom bone, disappearing bone): its relation to hemangiomatosis. J Bone Joint Surg Am. 1955;37(5):985–1004. [PubMed] [Google Scholar]
- 3.Collins J. Case 92: Gorham syndrome. Radiology. 2006;238(3):1066–1069. doi: 10.1148/radiol.2383032126. [DOI] [PubMed] [Google Scholar]
- 4.Gowin W, Rahmanzadeh R. Radiologic diagnosis of massive idiopathic osteolysis (Gorham-Stout Syndrome) Rontgenpraxis. 1985;38(4):128–134. [PubMed] [Google Scholar]
- 5.Horst M, Zsernaviczky J, Delling G. A rare case of so-called idiopathic osteolysis associated with a lymphangioma of the fibula. Z Orthop Ihre Grenzgeb. 1979;117(1):88–95. [PubMed] [Google Scholar]
- 6.Flörchinger A, Böttger E, Claass-Böttger F, Georgi M, Harms J. Gorham Stout syndrome of the spine. Case report and review of the literature. Rofo. 1998;168(1):68–76. doi: 10.1055/s-2007-1015184. [DOI] [PubMed] [Google Scholar]
- 7.Choma ND, Biscotti CV, Bauer TW, Mehta AC, Licata AA. Gorham's syndrome: a case report and review of the literature. Am J Med. 1987;83(6):1151–1156. doi: 10.1016/0002-9343(87)90959-4. [DOI] [PubMed] [Google Scholar]
- 8.Touraine R, Bernard JP, Trouillier JP, Balandreau AM. Chylothorax and Gorham's disease (or regional massive osteolysis) J Fr Med Chir Thorac. 1971;25(3):315–326. [PubMed] [Google Scholar]
- 9.Chavanis N, Chaffanjon P, Frey G, Vottero G, Brichon PY. Chylothorax complicating Gorham's disease. Ann Thorac Surg. 2001;72(3):937–939. doi: 10.1016/s0003-4975(00)02417-6. [DOI] [PubMed] [Google Scholar]
- 10.Johnson PM, McClure JG. Observations of massive osteolysis: a review of the literature and report of a case. Radiology. 1958;71(1):28–42. doi: 10.1148/71.1.28. [DOI] [PubMed] [Google Scholar]
- 11.Fretz CJ, Jungi WF, Neuweiler J, Haertel M. The malignant degeneration of Gorham-Stout disease? Rofo. 1991;155(6):579–581. doi: 10.1055/s-2008-1033321. [DOI] [PubMed] [Google Scholar]
- 12.Tilling G, Skobowytsh B. Disappearing bone disease, morbus Gorham. Report of a case. Acta Orthop Scand. 1968;39(3):398–406. doi: 10.3109/17453676808989475. [DOI] [PubMed] [Google Scholar]
- 13.Ellis DJ, Adams TO. Massive osteolysis: report of case. J Oral Surg. 1971;29(9):659–663. [PubMed] [Google Scholar]
- 14.Riantawan P, Tansupasawasdikul S, Subhannachart P. Bilateral chylothorax complicating massive osteolysis (Gorham's syndrome) Thorax. 1996;51(12):1277–1278. doi: 10.1136/thx.51.12.1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gorham LW, Wright AW, Schultz HH, Maxon FC. Disappearing bones: a rare form of massive osteolysis: report of 2 cases, 1 with autopsy findings. Am J Med. 1954;17(5):674–682. doi: 10.1016/0002-9343(54)90027-3. [DOI] [PubMed] [Google Scholar]
- 16.Kery L, Wouters HW. Massive osteolysis: report of two cases. J Bone Joint Surg Br. 1970;52(3):452–459. [PubMed] [Google Scholar]
- 17.Vinée P, Tanyü MO, Hauenstein KH, Sigmund G, Stöver B, Adler CP. CT and MRI of Gorham syndrome. J Comput Assist Tomogr. 1994;18(3):985–989. doi: 10.1097/00004728-199411000-00028. [DOI] [PubMed] [Google Scholar]
- 18.Dominguez R, Washowich TL. Gorham's disease or vanishing bone disease: plain film CT, and MRI findings of two cases. Pediatr Radiol. 1994;24(5):316–318. doi: 10.1007/BF02012113. [DOI] [PubMed] [Google Scholar]
- 19.Tie ML, Poland GA, Rosenow EC., 3rd Chylothorax in Gorham's syndrome: a common complication of a rare disease. Chest. 1994;105(1):208–213. doi: 10.1378/chest.105.1.208. [DOI] [PubMed] [Google Scholar]
- 20.Chambers TJ. The cellular basis of bone resorption. Clin Orthop Relat Res. 1980;(151):151–193. [PubMed] [Google Scholar]
- 21.Poirier H. Massive osteolysis of the humerus treated by massive resection and prosthetic replacement. J Bone Joint Surg Br. 1968;50(1):158–160. [PubMed] [Google Scholar]
- 22.Butler RW, McCance RA, Barrett AM. Unexplained destruction of the shaft of the femur in a child. J Bone Joint Surg Br. 1958;40(1):487–493. doi: 10.1302/0301-620X.40B3.487. [DOI] [PubMed] [Google Scholar]
- 23.Phillips RM, Bush OB, Jr, Hall HD. Massive osteolysis (phantom bone, disappearing bone). Report of a case with mandibular involvement. Oral Surg Oral Med Oral Pathol. 1972;34(6):886–896. doi: 10.1016/0030-4220(72)90227-7. [DOI] [PubMed] [Google Scholar]
- 24.Ross JL, Schinella R, Shenkman L. Massive osteolysis. An unusual cause of bone destruction. Am J Med. 1978;65(2):367–372. doi: 10.1016/0002-9343(78)90834-3. [DOI] [PubMed] [Google Scholar]
- 25.Möller G, Priemel M, Amling M, Werner M, Kuhlmey AS, Delling G. The Gorham-Stout syndrome (Gorham's massive osteolysis). A report of six cases with histopathological findings. J Bone Joint Surg Br. 1999;81(3):501–506. doi: 10.1302/0301-620x.81b3.9468. [DOI] [PubMed] [Google Scholar]
- 26.Hardegger F, Simpson LA, Segmueller G. The syndrome of idiopathic osteolysis: classification, review and case report. J Bone Joint Surg Br. 1985;67(1):89–93. doi: 10.1302/0301-620X.67B1.3968152. [DOI] [PubMed] [Google Scholar]
- 27.White AA. Disappearing bone disease with arthropathy and severe scarring of the skin. A report of four cases seen in South Vietnam. J Bone Joint Surg Br. 1971;53(2):303–309. [PubMed] [Google Scholar]
- 28.Beals RK, Bird CB. Carpal and tarsal osteolysis. A case report and review of the literature. J Bone Joint Surg Am. 1975;57(5):681–686. [PubMed] [Google Scholar]
- 29.Spieth ME, Greenspan A, Forrester DM, Ansari AN, Kimura RL, Gleason-Jordan I. Gorham's disease of the radius: radiographic, scintigraphic, and MRI findings with pathologic correlation. A case report and review of the literature. Skeletal Radiol. 1997;26(11):659–663. doi: 10.1007/s002560050306. [DOI] [PubMed] [Google Scholar]
- 30.Knoch HG. Die Gorhamsche Krankheit aus klinischer Sicht. Zentralbl Chir. 1963;18:674–683. [Google Scholar]
- 31.Thompson JS, Schurman DJ. Massive osteolysis: case report and review of the literature. Clin Orthop Relat Res. 1974;(103):103–111. [PubMed] [Google Scholar]
- 32.Young JW, Galbraith M, Cunningham J, Roof BS, Vujic I, Gobien RP. Progressive vertebral collapse in diffuse angiomatosis. Metab Bone Dis Relat Res. 1983;5(2):53–60. doi: 10.1016/0221-8747(83)90001-2. [DOI] [PubMed] [Google Scholar]
- 33.Carneiro RS, Steglich V. “Disappearing bone disease” in the hand. J Hand Surg Am. 1987;12(4):629–634. doi: 10.1016/s0363-5023(87)80225-3. [DOI] [PubMed] [Google Scholar]