Abstract
Objective: To report on the management of five cases of pyomyositis in athletes after the use of anabolic steroids. Method: Over the past 10 years, five cases of athletes who developed pyomyositis after using anabolic steroids were attended at the Sports Trauma Center (CETE), EPM-UNIFESP. Results: All the patients were diagnosed clinically and through laboratory and imaging tests. Surgical treatment was carried out (with collection of material for culturing) and antibiotic therapy was administered. In four cases, the injection sites were in the upper limbs and in one case, in the gluteus muscles bilaterally as well as in the upper limbs. In all five cases, occurrences of leukocytosis and neutrophilia were observed in the hemogram. After debridement, the germs of normal skin (S. aureus and S. viridans) were found in cultures on the secretions. Demarcation of the abscess and examination of the muscle plane in which the abscess was located were performed using ultrasound and magnetic resonance imaging. All the patients responded to broad-spectrum antibiotic therapy. Two cases required more than one surgical procedure because of the appearance of more than one abscess site with different evolution times. Conclusion: The use of anabolic steroids by some athletes may have grave consequences. Rapid, energetic and multidisciplinary intervention is necessary in such cases in order to avoid undesirable results. The right treatment healed the athletes completely, and they returned to their sports at the same level.
Keywords: Pyomyositis, Steroids/adverse Effects, Athletes, Anabolic Agents
INTRODUCTION
Pyomyositis is a disease that is characteristic of countries with a tropical climate and, for this reason, it is also known as tropical myositis. It is a condition without great prevalence and therefore delays in diagnosing it may occur. If it is not diagnosed in time, it may lead to pyoarthritis, osteomyelitis, compartmental syndrome, muscle necrosis, sepsis or even death. Its occurrence may be associated with the use of immunosuppressant drugs, diabetes, patients with transplants, AIDS, multiple myeloma and the use of injection drugs1, 2, 3
Within some sports settings, there is a belief among some athletes that improvement in performance and muscle mass gain can be achieved through using anabolic steroids. It is common for users to inject steroids at the site at which it is desired to increase the muscle mass, while ignoring the many risks and great harm that this may cause. The systemic effects from anabolic steroids include early epiphyseal closure, testicle atrophy, acne, sterility, gynecomastia, liver diseases, sterility, baldness, testicular cancer, insulin resistance, salt and water retention, increased cholesterol and early infarction, among others. The local side effects include tendon lesions, stress fractures, neurological lesions, cellulitis, tissue necrosis, abscesses and even, in extreme cases, necrotizing fasciitis.
The aim of this study was to report on the occurrence of cases that demonstrate the adverse effects from these substances and the importance of rapid and energetic intervention in such cases, in order to avoid unsatisfactory results
CASE REPORTS
Case 1 - The patient was a 29-year-old male bodybuilder from São Paulo, SP, who was attended as an outpatient with a complaint of pain and edema in his right arm. He reported that he had used anabolic steroids at home, 10 days earlier. On physical examination, he presented pain, heat and redness, and fluctuation on local palpation. The range of motion was painful but could be maintained. He was admitted to the emergency service, and laboratory tests (hemogram, VHS and PCR) and imaging examinations (ultrasound and magnetic resonance) were performed. A diagnosis of pyomyositis of the brachial biceps was confirmed. Emergency surgical cleaning was performed, and material was collected for culturing. A Penrose drain was placed and was removed on the second postoperative day. The result from culturing was positive for Staphylococcus aureus, and the patient was administered antibiotic therapy. He returned to his sport 30 days later, without performance loss (Figure 1)
Figure 1.

Material collected for culturing.
Case 2 - The patient was a 31-year-old male bodybuilder from São Paulo, SP, who was attended as an outpatient with a complaint of pain and edema in his left arm. He had made use of anabolic steroids several times, and the last application was three days earlier, at the training place. On physical examination, he presented phlogistic signs at the location. The range of motion was painful and limited. He was admitted to the emergency service and underwent laboratory tests (hemogram, VHS and PCR) and imaging examinations (ultrasound and magnetic resonance), which confirmed a diagnosis of pyomyositis of the brachial biceps. Emergency surgical cleaning was performed, and material was collected for culturing. A Penrose drain was placed and was removed on the second postoperative day. The result from culturing was positive for Staphylococcus aureus, and the patient was administered antibiotic therapy. He returned to his sport 42 days later, without performance loss.
Case 3 - The patient was a 32-year-old male bodybuilder and jiu-jitsu player from Campinas, SP, who was attended with a complaint of pain in his right arm. He reported that he had used anabolic steroids at home, 16 days earlier. On physical examination, he presented pain and local hyperemia. The range of motion was painful but could be maintained. He was admitted to the emergency service and underwent laboratory tests (hemogram, VHS and PCR) and imaging examinations (ultrasound and magnetic resonance), which confirmed a diagnosis of pyomyositis of the brachial biceps and ipsilateral triceps. Emergency surgical cleaning was performed, and material was collected for culturing. A Penrose drain was placed and was removed on the second postoperative day. The result from culturing was positive for Streptococcus viridians, and the patient was administered antibiotic therapy. He returned to his sport 38 days later, without performance loss (Figures 2 and 3)
Figure 2.

Hyperemia in right arm.
Figure 3.
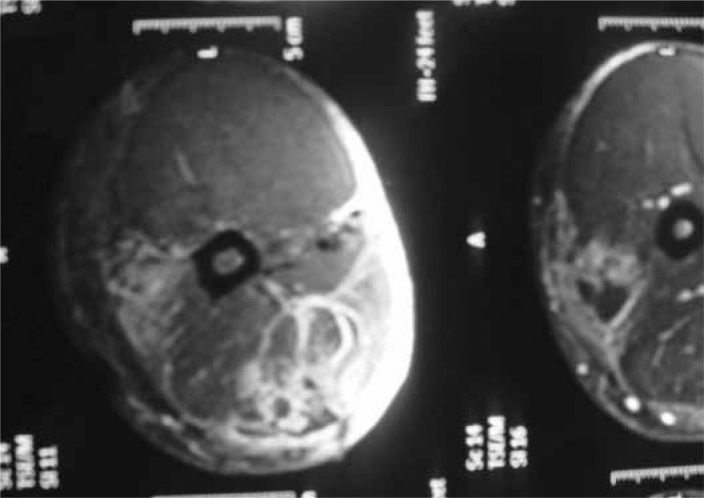
Magnetic resonance imaging.
Case 4 - The patient was a 34-year-old male bodybuilder and swimmer from São Paulo, SP, who was attended with a complaint of pain and edema in his left arm. He reported that he had used anabolic steroids at the training place, seven days earlier. On physical examination, he presented pain, heat and redness, fluctuation on palpation of the arm. The range of motion could be maintained, without joint blockage. He was sent to the emergency service and laboratory tests (hemogram, VHS and PCR) and imaging examinations (ultrasound and magnetic resonance) were performed, which confirmed a diagnosis of pyomyositis of the brachial biceps. Emergency surgical cleaning was performed, and material was collected for culturing. A Penrose drain was placed and was removed on the second postoperative day. Also on the second postoperative day, he presented a similar condition in the contralateral arm. New tests were performed, which confirmed the same diagnosis. He underwent surgical cleaning again, and material was collected. The result from both cultures was positive for Staphylococcus aureus, and the patient was administered antibiotic therapy. He returned to his sports activities 37 days later.
Case 5 - The patient was a 42-year-old male bodybuilder and physician from Jundiaí, SP, who was attended with a complaint of pain and edema in his arm. Initially, he did not report any use of anabolic steroids. On physical examination, he presented phlogistic signs in his left biceps. The range of motion was maintained. He was sent to the emergency service and laboratory tests (hemogram, VHS and PCR) and imaging examinations (ultrasound and magnetic resonance) were performed, which confirmed a diagnosis of pyomyositis of the left brachial biceps. Emergency surgical cleaning was performed and signs of muscle necrosis were observed. Material was collected for culturing. A Penrose drain was placed and was removed on the second postoperative day. On the third postoperative day, he presented phlogistic signs in the right gluteus. Ultrasound examination was performed, which showed fluid accumulations in the gluteus maximus and minimus. The limits of the accumulation area were defined using magnetic resonance. The patient's use of anabolic steroids was confirmed. He underwent a further surgical cleaning procedure. The result from the cultures was positive for Staphylococcus aureus in both locations, and antibiotic therapy was administered. The patient returned to his sports activities 45 days later
DISCUSSION
Anabolic steroids are used by some athletes as a way of gaining muscle mass and definition and achieving better performance. Since they are mostly applied without adequate asepsis, the administration site becomes a potential focus of infection. This local infection generally evolves into abscesses that tend to be very exuberant. Early treatment with energetic action becomes necessary in order to control these infectious processes, which may evolve rapidly to conditions of greater severity such as muscle necrosis or sepsis.
In a chapter by Crum-Cianflone, in a book reviewing clinical microbiology published by the American Society for Microbiology, the possible causes of myositis are cited as being bacterial, viral, parasitic and fungal. Bacterial forms are the commonest cause and, among these, S. aureus is the agent most commonly encountered, as seen in the cases reported here5, 6, 7, 8. Most infections are diagnosed clinically, and imaging examinations only complement the diagnosis. Blood cultures are positive only in 16% to 38% of the patients, and secretion cultures are positive only in 21% to 41%
In a survey of the literature, Bickels et al(9) found 676 cases reported over a 42-year period, and observed that primary pyomyositis was more prevalent in the quadriceps, whereas is our study, it was predominantly in the brachial biceps muscle. In an attempt to better standardize the lesions and consequently gain greater efficiency in treating this condition, these authors described three stages of pyomyositis: stage I – muscle pain, inflammatory signs and fever; stage II – formation of abscesses; stage III – signs of toxemia, with the possibility of progression to septic shock.
This type of infection usually responds to ordinary broad-spectrum antibiotics, thus leading to favorable evolution of the condition.
Multidisciplinary, energetic attendance with immediate action is fundamental for achieving a satisfactory result(10)
The strong points of this study are that the sample was a homogenous group and no patients were lost during the follow-up. Its weak points are that this was a retrospective and non-randomized study.
Footnotes
Work performed at the Sports Traumatology Center (CETE) of the Department of Orthopedics and Traumatology, Federal University of São Paulo, SP, Brazil (DOT-UNIFESP/EPM)
REFERENCES
- 1.Ejnisman B, Filho JS, Andreoli CV, Monteiro GC, Pochini AC, Cohen M. Piomiosite multifocal em atleta: relato de caso. Rev Bras Ortop. 2007;42(5):157–160. [Google Scholar]
- 2.Rotman-Pikielny P, Levy Y, Eyal A, Shoenfeld Y. Pyomyositis or “injectiositis” Staphylococcus aureus multiple abscesses following intramuscular injections. Isr Med Assoc J. 2003;5(4):295–296. [PubMed] [Google Scholar]
- 3.Rossi L, Conen D. Intramuscular injections – An outdated form of administration? Six cases of Staphylococcus aureus sepsis following intramuscular injections. Schweiz Med Wochenschr. 1995;125(31-32):1477–1482. [PubMed] [Google Scholar]
- 4.Al-Ismail K, Torreggiani WC, Munk PL, Nicolaou S. Gluteal mass in a bodybuilder: radiological depiction of a complication of anabolic steroid use. Eur Radiol. 2002;12(6):1366–1369. doi: 10.1007/s00330-001-1169-1. [DOI] [PubMed] [Google Scholar]
- 5.Crum-Cianflone NF. Bacterial, fungal, parasitic, and viral myositis. Clin Microbiol Rev. 2008;21(3):473–494. doi: 10.1128/CMR.00001-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Block AA, Marshall C, Ratcliffe A, Athan E. Staphylococcal pyomyositis in a temperate region: epidemiology and modern management. Med J Aust. 2008;189(6):323–325. doi: 10.5694/j.1326-5377.2008.tb02050.x. [DOI] [PubMed] [Google Scholar]
- 7.Nather A, Wong FY, Balasubramaniam P, Pang M. Streptococcal necrotizing myositis: a rare entity. A report of two cases. Clin Orthop Relat Res. 1987;(215):215–221. [PubMed] [Google Scholar]
- 8.Koutures CG, Savoia M, Pedowitz RA. Staphylococcus aureus thigh pyomyositis in a collegiate swimmer. Clin J Sport Med. 2000;10(4):297–299. doi: 10.1097/00042752-200010000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Bickels J, Ben-Sira L, Kessler A, Wientroub S. Primary pyomyositis. J Bone Joint Surg Am. 2002;84(12):2277–2286. doi: 10.2106/00004623-200212000-00024. [DOI] [PubMed] [Google Scholar]
- 10.Puşchiţă M, Ciobanu G, Amza O. Multidisciplinary approach in pyomyositis early diagnosis. Rev Med Chir Soc Med Nat Iasi. 2006;110(1):66–72. [PubMed] [Google Scholar]


