Abstract
Objectives: To evaluate the efficacy of osteosynthesis on femoral neck fractures using two instead of three screws. Methods: Thirty-nine fractures were retrospectively evaluated, divided into groups in which two screws were used in parallel (n = 28) or three screws (n =11) in an inverted triangle configuration (in accordance with the AO technique). The patients were then followed up until reaching the outcome of either consolidation or failure. Results: In the group in which two screws were used, consolidation was observed in 23 of the 28 fractures (82%). In the group in which three screws were used, consolidation was observed in 6 of the 11 fractures (55%). There was no statistically significant difference between these percentages. Conclusion: There was no difference in the prognosis for these fractures when treated using two screws in parallel or three screws in an inverted triangle in accordance with the AO technique. Further studies are needed in order to establish a definitive conclusion.
Keywords: Femoral Neck Fractures; Fracture Fixation, Internal; Bone Screws; Longitudinal Studies
INTRODUCTION
Femoral neck fractures are a challenge even for experienced surgeons(1), because of the high rates of postoperative complications. Problems relating to fracture reduction and correct placement of screws often make such operations difficult(2). The poor results reported in the literature3, 4 have contributed towards low enthusiasm for non-arthroplastic treatment of this fracture.
Few papers have clarified what the ideal number of screws for treating neck fractures should be(5). Here, we retrospectively compare the osteosynthesis technique using three screws, in accordance with the AO-ASIF technique(6), with a simpler technique of placing only two parallel screws: one higher and the other lower in the femoral neck.
MATERIALS AND METHODS
This study was submitted for consideration by the research ethics committee of UNIFESP, under number 1701/10 and was duly approved.
Radiographs of patients with femoral neck fractures who underwent osteosynthesis with two or three cannulated 6.5 mm steel screws were evaluated.
The patients were operated by two senior surgeons between January 2000 and December 2010.
Inclusion criteria:
All the patients needed to be over 18 years of age, presenting an intracapsular fracture with or without displacement that was treated by means of osteosynthesis using two or three screws in parallel, inserted only using a percutaneous technique.
Exclusion criteria:
Patients with an immature skeleton, extracapsular fracture or osteosynthesis using screws placed in non-parallel positions were excluded.
Thirty-nine fractures in 39 patients were evaluated. Table 1 presents the distribution of the 22 female and 17 male patients, subdivided into age groups of older or younger than 65 years (thus defining elderly and young patients). The patients' ages ranged from 18 to 88 years, with a mean of 54 years.
Table 1.
Distribution of fractures according to their classification.
| Two screws | Three screws | |
|---|---|---|
| Garden I | 9 | 2 |
| Garden II | 3 | 1 |
| Pauwels I | 1 | 0 |
| Pauwels II | 3 | 2 |
| Pauwels III | 12 | 6 |
| Total | 28 | 11 |
In the subgroup that underwent osteosynthesis with two screws, 28 fractures were evaluated, and these were classified according to the Garden system (when over the age of 65 years), according to the Pauwels system (when under the age of 65 years) and anatomically (both age groups). In the subgroup that underwent osteosynthesis with three screws, 11 fractures were evaluated, classified in the same manner.
Radiographs:
The preoperative radiographs were analyzed and the fractures were classified according to their anatomy (subcapital, transcervical and basicervical), orientation of the fracture line (Pauwels classification)(7) and, for patients over 65 years of age, we added the Garden classification(8).
Postoperative radiographs were assessed until the end point was reached, defined as fracture consolidation, collapse of the femoral neck, loss of reduction that necessitated reintervention, necrosis of the head or pseudarthrosis of the neck, with a minimum period of six months elapsed from the time of the fracture(9) (Figure 1).
Figure 1.

Osteosynthesis with three screws using the AO-ASIF technique.
RESULTS
In the subgroup that underwent osteosynthesis with two screws, there were nine fractures classified as Garden I and three as Garden II. One fracture was classified as Pauwels I, three as Pauwels II and 13 as Pauwels III. Regarding the anatomical region, 10 were transcervical, four were basicervical and three were subcapital (Figure 2).
Figure 2.
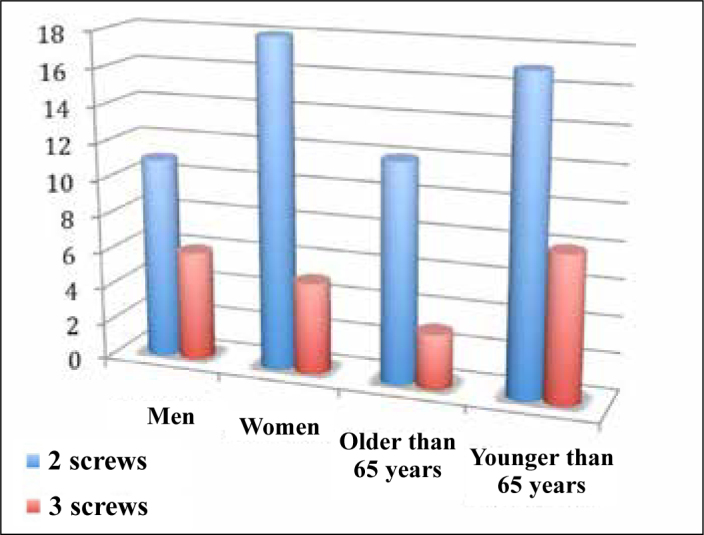
Patient distribution in the study groups.
In the subgroup that underwent osteosynthesis with three screws, there were two fractures classified as Garden I, one as Garden II, two as Pauwels II and six as Pauwels III. Regarding the location of the fracture line, six were transcervical, two were subcapital and three were basicervical (Figure 2).
Among the young patients (< 65 years), there were four failures out of 11 fractures (36%) in the group that underwent osteosynthesis with three screws, and two failures out of 16 fractures (12.5%) in the group operated with two screws.
Among the elderly patients (> 65 years), there were four failures (25%) out of 12 fractures in the group that underwent osteosynthesis with two screws, and one failure (33.3%) out of three fractures in the group operated with three screws.
In the subgroup with two screws, consolidation was achieved in 23 (82%), while in the group with three screws, six fractures consolidated (55%) (Figure 3).
Figure 3.
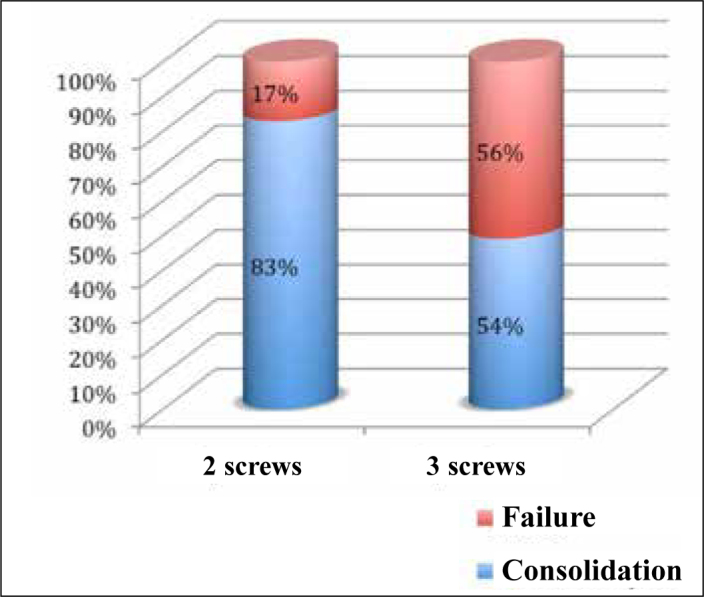
Patient distribution according to outcome from osteosynthesis.
In the subgroup with two screws, evolution to osteonecrosis of the femoral head occurred in four fractures. Loss of reduction only occurred in one of these, and this was followed by segmental collapse and evolution to pseudarthrosis.
In the subgroup operated with three screws, there were four fractures with loss of reduction followed by collapse and pseudarthrosis, and a single case of osteonecrosis of the femoral head.
Pauwels III fractures are considered to be unstable, and we observed in the subgroup with two screws that two of these fractures had unfavorable evolution (one with collapse and loss of reduction and one with osteonecrosis). However, 11 of them did not have any complications. In the subgroup with three screws, there were six Pauwels III fractures, and four of them had poor evolution (three collapses followed by loss of reduction, and one case of osteonecrosis).
The data obtained were subjected to statistical analysis using Fisher's exact test, and a p-value of 0.109 was found. The results encountered suggest that there was no association between the technique used and the outcome from osteosynthesis.
DISCUSSION
A wide diversity of methods and different techniques are used for osteosynthesis of femoral neck fractures10, 11, 12. Prominent among these is fixation using cannulated screws, which are used to facilitate the surgical procedure.
There is a great variety of studies citing the advantages and disadvantages of different methods and implants. However, few authors have examined whether osteosynthesis is better with two or three screws.
In the classic study by Selvan et al(13), the traditional configuration of three screws in the shape of an inverted triangle is advocated as the mechanically most stable option. The AO-ASIF group has also supported placement of three screws in the shape of an inverted triangle.
The fact that a layout with three screws is more stable than using two screws in vitro is not surprising. However, the result that we obtained here opens up the perspective that using only two screws, despite the less stable format, is sufficiently stable for correct treatment of femoral neck fractures.
Krastman et al(14) obtained good results from using only two screws for synthesis in cases of stable fractures. In the biomechanical study conducted by Walker et al(15), using only two screws was deemed sufficient. Alhol et al16, 17 and Austdal et al(18) also did not find any difference between using two and three screws, and observed a failure rate of around 14% both for two and for three screws, while in our study, the failure rate from using two screws was 13.3%. The failure rate that we found in cases of osteosynthesis of fractures in young patients was similar to what has been found by other authors, such as Henari et al(19), whose sample of 12 patients presented failure in 25% of the cases.
Placing the implants in an exactly parallel position, even when only using two screws, is not easy. The percutaneous technique requires skill to correctly position the Kirschner wires.
The difficulty in achieving absolute parallelism is much more evident when the third screw is placed. Furthermore, considering that some of our population presented a narrow femoral neck, placement of three screws became even more difficult.
A vertical fracture line with a tendency towards shearing was not an impediment to placement of only two screws. In fractures with significant instability, use of other devices (dhs) or even three screws was not proven to be superior to other types of osteosynthesis. We also did not observe any difference in our study, in which a more vertical fracture line (Pauwels III) was treated with only two screws in most cases.
No osteosynthesis was performed in any patients over the age of 65 years presenting Garden III or IV. In these cases, coxofemoral arthroplasty was performed. Like Alho et al16, 17 and Austdal et al(18), we did not indicate osteosynthesis for elderly patients with displaced fractures. The very high reoperation rate and relatively long immobilization time make osteosynthesis a poor option.
The difference in the size of the samples between the groups using two screws (n = 28) and three screws (n = 11) constitutes a source of bias in this study, along with the non-randomization. Nonetheless, we observed surprising results that suggest that there is no difference in treating these fractures, even when dealing with fractures with a significant tendency towards vertical shearing, as in Pauwels III fractures.
CONCLUSION
In our study, osteosynthesis of femoral neck fractures with two screws presented results similar to using three screws. Prospective randomized studies with greater numbers of patients need to be conducted in order to better assess whether the technique using two screws for femoral neck fractures is superior to the three-screw technique.
Footnotes
Work performed in the Paulista School of Medicine, Federal University of São Paulo, São Paulo, SP, Brazil.
REFERENCES
- 1.Rocha MA, Carvalho WS, Zanqueta C, Lemos SC. Estudo epidemiológico retrospectivo das fraturas do fêmur proximal tratados no Hospital Escola da Faculdade de Medicina do Triângulo Mineiro. Rev Bras Ortop. 2001;36(8):311–316. [Google Scholar]
- 2.Gurusamy K, Parker MJ, Rowlands TK. The complications of displaced intracapsular fractures of the hip: the effect of screw positioning and angulation on fracture healing. J Bone Joint Surg Br. 2005;87(5):632–634. doi: 10.1302/0301-620X.87B5.15237. [DOI] [PubMed] [Google Scholar]
- 3.Lu-Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg Am. 1994;76(1):15–25. doi: 10.2106/00004623-199401000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Huang HK, Su YP, Chen CM, Chiu FY, Liu CL. Displaced femoral neck fractures in young adults treated with closed reduction and internal fixation. Orthopedics. 2010;33(12):873. doi: 10.3928/01477447-20101021-15. [DOI] [PubMed] [Google Scholar]
- 5.Önnerfält R. Treatment of the displaced femoral neck fracture, as reflected in Acta Orthopaedica Scandinavica - The rise and fall of internal fixation. Acta Orthop. 2010;81(1):15–20. doi: 10.3109/17453671003635801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lindequist S, Wredmark T, Eriksson SA, Samnegård E. Screw positions in femoral neck fractures: comparison of two different screw positions in cadavers. Acta Orthop Scand. 1993;64(1):67–70. doi: 10.3109/17453679308994532. [DOI] [PubMed] [Google Scholar]
- 7.Pauwels F. Der Schenkelhalsbruch: Ein mechanisches problem. Ferdinand Enke Verlag; Stuttgart: 1935. [Google Scholar]
- 8.Garden RS. Reduction and fixation of subcapital fractures of the femur. Orthop Clin North Am. 1974;5(4):683–712. [PubMed] [Google Scholar]
- 9.Leighton RK. Fractures of the neck of the femur. In: Bucholz RW, Heckman JD, Court-Brown C. Rockwood & green's fractures in adults. 6th ed. Lippincott Williams & Wilkins. p. 1780-81
- 10.Parker MJ, Blundell C. Choice of implant for internal fixation of femoral neck fractures. Meta-analysis of 25 randomised trials including 4,925 patients. Acta Orthop Scand. 1998;69(2):138–143. doi: 10.3109/17453679809117614. [DOI] [PubMed] [Google Scholar]
- 11.Osorio L, Couto P, Giesta C. Osteossíntese com dois parafusos no tratamento das fraturas do colo do fêmur. Rev Bras Ortop. 1993;28(6):353–356. [Google Scholar]
- 12.Lichtblau S, Gallina J, Nasser P, Munyoki M, Jepsen K. A biomechanical comparison of two patterns of screw insertion. Bull NYU Hosp Jt Dis. 2008;66(4):269–271. [PubMed] [Google Scholar]
- 13.Selvan VT, Oakley MJ, Rangan A, Al-Lami MK. Optimum configuration of cannulated hip screws for the fixation of intracapsular hip fractures: a biomechanical study. Injury. 2004;35(2):136–141. doi: 10.1016/s0020-1383(03)00059-7. [DOI] [PubMed] [Google Scholar]
- 14.Krastman P, van den Bent RP, Krijnen P, Schipper IB. Two cannulated hip screws for femoral neck fractures: treatment of choice or asking for trouble? Arch Orthop Trauma Surg. 2006;126(5):297–303. doi: 10.1007/s00402-006-0143-4. [DOI] [PubMed] [Google Scholar]
- 15.Walker E, Mukherjee DP, Ogden AL, Sadasivan KK, Albright JA. A biomechanical study of simulated femoral neck fracture fixation by cannulated screws: effects of placement angle and number of screws. Am J Orthop (Belle Mead NJ) 2007;36(12):680–684. [PubMed] [Google Scholar]
- 16.Alho A, Austdal S, Benterud JG, Blikra G, Lerud P, Raugstad TS. Biases in a randomized comparison of three types of screw fixation in displaced femoral neck fractures. Acta Orthop Scand. 1998;69(5):463–468. doi: 10.3109/17453679808997779. [DOI] [PubMed] [Google Scholar]
- 17.Alho A, Austdal S, Benterud JG, Blikra G, Lerud P, Raugstad TS. Problems in orthopedic multicenter studies - screw fixation of displaced femoral neck fracture [abstract] Acta Orthop Scand. 1998;(Suppl 282):11. doi: 10.3109/17453679808997779. [DOI] [PubMed] [Google Scholar]
- 18.Austdal S, Benterud JG, Blikra G, Kuokkanen H, Lindequist S, Lerud P. Osteosynthesis of displaced femoral neck fractures with multiple screws - a randomised multicenter study [abstract] J Bone Joint Surg Br. 1993;75(Suppl 2):199. [Google Scholar]
- 19.Henari S, Leonard M, Hamadto M, Cogley D. Review of a single contemporary femoral neck fracture fixation method in young patients. Orthopedics. 2011;34(3):171. doi: 10.3928/01477447-20110124-09. [DOI] [PubMed] [Google Scholar]


