Abstract
Objective: To assess the clinical results obtained of patients who underwent arthroscopic surgical treatment following a first episode of traumatic anterior shoulder dislocation. Methods: Between August 2000 and October 2008, 14 shoulders of 14 patients were treated by the Shoulder and Elbow Group of Santa Casa Hospital, São Paulo. Thirteen patients (93%) were male and one (7%) was female; their ages ranged from 17 to 41 years, with a mean of 28 years. All of the patients evaluated were regularly practicing a sports activity (which required physical vigor of the upper limbs). The time that had elapsed between the trauma and the surgical treatment ranged from seven to 60 days, with a mean of 20 days. The surgical procedure was performed with arthroscopic viewing, with the patient positioned in lateral decubitus. Fixation of the labral-ligamentous complex was achieved using bioabsorbable anchors. The postoperative clinical assessment was made using Rowe and UCLA criteria. Joint mobility was measured according to the guidance from ASES (American Shoulder and Elbow Surgeons). The length of postoperative follow-up ranged from 24 to 120 months, with a mean of 45 months. Results: All the patients achieved satisfactory results, (85% excellent and 15% good), as shown by UCLA, while 100% of the results were excellent according Rowe. The “grip test” was negative for all the patients. Conclusion: Surgical treatment after a first episode of traumatic anterior shoulder dislocation seems to be a good therapeutic option for young active patients who practice sports activities.
Keywords: Shoulder Joint, Shoulder Dislocation, Arthroscopy, Joint Instability
INTRODUCTION
After a first episode of traumatic anterior dislocation (TAD) of the shoulder, up to 93.5% of such cases may present lesions of the glenoid capsule or labrum(1). Early treatment may avoid further damage to the joint, such as bone erosion at the anterior rim of the glenoid or in the posterosuperior region of the humeral head (Hill-Sachs lesion), and it may also avoid excessive capsule distension. These factors generally make the necessary treatment more difficult, non-anatomical and technically more complex, and such cases may evolve with limitation of joint mobility, especially regarding lateral rotation, and may even evolve with osteoarthrosis1, 2, 3.
Conservative treatment for TAD consists of closed reduction and immobilization for four weeks, followed by a rehabilitation program(4). The clinical evolution of these patients may follow one of three possible patterns: the shoulder may never dislocate again and the patient will evolve favorably; the shoulder may dislocate again, but the patient will learn to live with the dislocations; or lastly, the shoulder will dislocate again and patient will choose to undergo surgical treatment after a recurrent condition has become established(5).
In a systematic review, Brophy and Marx(6) demonstrated recurrence rates that ranged from 38 to 80% among patients who had undergone conservative treatment, and rates of between 3 and 20% among patients who had been treated surgically. Jakobsen et al(1) found a recurrence rate of 54% after two years of follow-up on patients who had been treated conservatively. Larrain et al(7) showed that athletes who had undergone conservative treatment had a recurrence rate of 94%, while the rate for patients who had been treated surgically was 4%. Bottoni et al(4) found a recurrence rate of 75% among patients who had been treated conservatively and that if arthroscopic suture of the Bankart lesion was performed after the first episode of TAD of the shoulder, the rate found was 11.1%. After this study, treatment for TAD of the shoulder under arthroscopic viewing started to be used1, 4, 8, 9.
The present study had the aim of evaluating the clinical results obtained among a group of patients who underwent suturing of a Bankart lesion under arthroscopic viewing, after a first episode of TAD of the shoulder.
MATERIALS AND METHODS
Between August 2000 and October 2008, 14 shoulders of 14 patients with a diagnosis of TAD of the shoulder were surgically treated (Table 1). The patients underwent surgical treatment after their first episode of dislocation. The surgery was performed under arthroscopic viewing by the Shoulder and Elbow Group of the Department of Orthopedics and Traumatology, School of Medical Sciences, Santa Casa de São Paulo.
Table 1.
Cases treated surgically after a first episode of traumatic anterior dislocation of the shoulder.
| Patient | Sex | Age | Dom. | Sport | ΔT | Associated lesions | PO-ROM | UCLA | Rowe | Follow-up (months) | Complications |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 35 | − | Swimming | 14 | HS | 160-50-T12 | 35 | 100 | 94 | − |
| 2 | M | 38 | (+) | Tennis | 14 | HS | 160-45-T5 | 35 | 100 | 81 | − |
| 3 | F | 19 | − | Tennis | 28 | HS | 140-45-T5 | 35 | 100 | 120 | − |
| 4 | M | 28 | (+) | Tennis | 7 | Posterior lesion (SLAP VI) | 160-40-T7 | 35 | 100 | 59 | − |
| 5 | M | 31 | − | Muscle-building | 7 | SLAP II + glenoid FT | 160-70-T5 | 35 | 100 | 35 | − |
| 6 | M | 37 | (+) | Gymnastics | 28 | SLAP III + HS+ glenoid FT + neuropraxia of axillary nerve | 160-70-T5 | 35 | 100 | 32 | − |
| 7 | M | 39 | − | Running | 21 | SLAP V | 150-60-T8 | 29 | 90 | 28 | Adhesive capsulitis |
| 8 | M | 17 | − | Handball | 21 | HS | 160-70-T5 | 35 | 100 | 25 | − |
| 9 | M | 18 | (+) | Swimming | 60 | HS | 160-70-T5 | 35 | 100 | 24 | − |
| 10 | M | 28 | − | Golf | 14 | HS+ IRCL | 150-45-T8 | 35 | 100 | 24 | − |
| 11 | M | 20 | (+) | Muscle-building | 14 | SLAP II + 360° lesion | 160-70-T5 | 35 | 100 | 24 | − |
| 12 | M | 41 | (+) | Water polo | 9 | SLAP III+ 360° lesion | 160-70-T5 | 35 | 100 | 24 | − |
| 13 | M | 17 | (+) | Muscle-building | 28 | SLAP V | 160-35-T5 | 28 | 90 | 35 | − |
| 14 | M | 30 | (+) | Tennis | 18 | SLAP V | 160-70-T5 | 35 | 100 | 30 | − |
Legend: N – case number; DOM – dominance; ΔT – length of evolution of the trauma before the surgery; PO-ROM – postoperative joint range of motion; HS – Hill-Sachs lesion; FT – fracture; IRCL – incomplete rotator cuff lesion.
Source: Medical archiving and statistics service, Central Hospital, Santa Casa de São Paulo.
The patients evaluated here fulfilled the following inclusion criteria: traumatic anterior dislocation of the shoulder; antecedents of only one episode of shoulder dislocation; absence of clinical evidence of multidirectional instability; postoperative follow-up lasting for 24 months or more; and presence of detachment of the anteroinferior glenoid labrum, diagnosed by means of imaging examinations. All the patients underwent simple radiography, along with magnetic resonance or magnetic arthro-resonance imaging, in order to view and diagnose the Bankart lesion and other possible associated lesions.
Among the 14 patients evaluated, 13 (93%) were male and one (7%) was female. Their ages ranged from 17 to 41 years, with a mean of 28 years. The dominant side was affected in eight patients (57%). All the patients evaluated were regularly practicing some form of sports activity (of types that demand physical vigor of the upper limbs), and two were professional athletes. The time that elapsed between the trauma and the surgical treatment ranged from seven to 60 days, with a mean of 20 days.
The repair on the shoulder lesions under arthroscopic viewing was done after implementing regional anesthetic blockade and general anesthesia. The patient was positioned in lateral decubitus and the limb that was to be operated was placed under traction. After inspection of the joint cavity, the labral lesion and possible associated lesions were identified. Deinsertion of the labrum at the rim of the glenoid cavity was completed with the aim of facilitating its mobilization and repositioning. The anterior surface of the glenoid cavity was then surgically prepared for better integration of the labral tissue and insertion area. Fixation of the labrum-ligament complex of the shoulder joint was then performed using two to six bioabsorbable anchors (mean of four anchors). In eleven patients, we used Bio-Suturetak-Arthrex® anchors; in two, Bio-FASTak-Arthrex® anchors; and in one, a Panalok-Mitek® anchor.
Among the associated lesions, we found two fractures of the anterior rim of the glenoid, nine bone lesions of the humeral head (Hill-Sachs lesions), one partial lesion of the rotator cuff and eight lesions of the superior labrum (SLAP). Among the SLAP lesions, two were type II, two were type III, three were type V and one was type VI, in which the posterior labrum was also affected(10). One of the patients (case 6) presented neuropraxia of the axillary nerve (Table 1).
In addition to the essential fixation of the Bankart lesion, thermal capsuloplasty was performed in the anterior region of the joint in case 3; a posterior labrum-ligament lesion was repaired using a Bio-Suturetak-Arthrex® anchor in case 4; a partial lesion of the joint surface of the rotator cuff was repaired using a Bio-Suturetak-Arthrex® anchor in case 10, without completing the lesion; and the slap lesions were repaired in cases 4, 5, 6, 7, 11, 12, 13 and 14.
After the operation, the operated limb was immobilized in a sling for six weeks. In the rehabilitation program, pendular movements and lateral rotation to zero degrees were allowed starting immediately after the operation; passive and active movements (to gain range of motion) were started six weeks after the operation and muscle strengthening was started 12 weeks after the operation. Patients were released to do their habitual physical activities six months after the operation. The length of follow-up ranged from 24 to 120 months, with a mean of 45 months.
The postoperative clinical evaluation was done using the Rowe scale(11) and the scale of the University of California at Los Angeles (UCLA)(12). Joint mobility was measured in accordance with the guidance of the American Shoulder and Elbow Surgeons (ASES) apud Hawkins and Bokor(13).
RESULTS
From the UCLA functional assessment score(12), we found that 85% of the patients achieved excellent results and 15% good results. There were no fair or poor results. From the evaluation criteria proposed by Rowe et al(11), we found that 100% of the results were excellent.
The average shoulder joint mobility measurements at the time of the last assessment were: elevation of 158° (using the parameters of the lateral rim of the scapula and the longitudinal axis of the humerus), lateral rotation of 58° and medial rotation as far as T7. The grip test was negative for all the patients.
Two cases were only considered to be good, according to the UCLA assessment score: case 7 (UCLA 29 and Rowe 90), because the patient evolved with a condition of adhesive capsulitis; and case 13 (UCLA 28 and Rowe 90), because after three years of follow-up, the patient reported pain when making great effort, despite presenting good function, strength and range of motion.
All the patients, except for cases 7 and 13, returned to their work and sports activities without any complaints or functional limitations.
The sample size (n = 14) was too small for statistical analysis to be used.
DISCUSSION
The objective in treating TAD of the shoulder is to return patients to their work and sports activities as quickly as possible, with the highest potential performance in these activities and with the lowest risk of recurrence.
The results from conservative or surgical treatment have been discussed in several studies. Recurrence rates ranging from 38% to 80% can be seen in the literature, for patients who were treated conservatively, and from 3% to 20% among patients who were treated surgically(6). In a randomized prospective study, Bottoni et al(4) divided a group of 29 young active patients who were practicing a sports activity into two subgroups: group I underwent conservative treatment (four weeks of immobilization in a sling, followed by rehabilitation) and group II underwent surgical treatment under arthroscopic viewing after their first episode of TAD of the shoulder. These authors found that the recurrent rate for dislocation for 75% among the patients treated conservatively and 11.1% among the patients treated surgically. These were the first authors to demonstrate good results from an early surgical approach.
Certain factors may indicate what the likely evolution will be after the first episode of TAD of the shoulder. Kralinger et al(14) demonstrated an important relationship between the patient's age and the risk of recurrence. In their study, the patients included in the age group from 21 to 30 years who underwent conservative treatment presented a recurrence rate of 61%. This rate diminished to 13% among the patients from 61 to 70 years. Another significant factor demonstrated in their study was that there was a directly proportional relationship between the intensity of the physical activity exerted by the patients (manual workers and practitioners of impact sports) and the risk of recurrence.
In a prospective study that included 253 patients, Robinson et al(15) found a recurrence rate of 67% over the first five years after the first episode of dislocation. In the group of patients within the age range from 15 to 25 years, this rate reached 80%. The authors also added that the patients developed a progressive functional deficit relating to the recurrent condition(3). In another study conducted at the same clinic as above, the following risk factors for recurrence of dislocations were determined: high-energy trauma, regional neurological deficit after the trauma, lesions associated with the rotator cuff and fractures of the glenoid(15).
DeBerardino et al(16) obtained excellent results from indication of early surgical treatment under arthroscopic viewing for young athletes. After two to five years of follow-up, 88% of the cases did not present recurrence and, in functional assessments, the mean score achieved on the Rowe scale was 92 points. The recurrences suffered by the other 12% were attributed to factors such as: presence of multidirectional instability, severe labral and capsular lesions and a long time interval before the surgical procedure. Owens et al(8) reassessed this same group of patients after 11 years of follow-up and observed that the good results were maintained with regard to satisfaction, function and return to sports activities. Other authors have found recurrence rates ranging from 3 to 11% and excellent results in 75 to 94% of their patients1, 4, 7.
In our group of patients, 100% of the results were satisfactory, with excellent results for 85% and good for 15%. None of the results were fair or poor, as measured using the UCLA score, and 100% of the results were excellent on the Rowe scale. We did not have any cases of recurrence. Only one patient was excluded from this study because the minimum follow-up of 24 months was not fulfilled: this patient suffered an episode of recurrence after a new trauma. However, this patient was uncooperative after the operation and only came back once for the stitches in his skin to be removed. He was contacted by telephone, which was how we learned about the occurrence.
Two cases that were followed up presented complications. Case 7 scored 29 points on the UCLA scale and 90 points on the Rowe scale because of a condition of adhesive capsulitis. This case underwent conservative treatment and 17 serial blockades of the suprascapular nerve were applied(17), which produced an improvement in the state of pain, but slight functional limitation was maintained. Case 13 scored 28 points on the UCLA scale and 90 points on the Rowe scale, and despite presenting good function, mobility and strength, reported feeling pain on making great effort, which partially limited him in his activities with heavy physical loads.
Recently, at the International Congress of Shoulder and Elbow Surgery (ICSES), in Edinburgh, 2010, Habermeyer et al(18) presented the Severity Shoulder Instability Score (SSIS), which determines risk factors for recurrence and might facilitate the decision on whether to intervene conservatively or surgically in cases of TAD of the shoulder. Among the criteria indicated by Habermeyer et al(18) were the patient's age, characteristics of the type of sports practiced, type of lesion observed in the glenoid (Bankart lesion with or without fracturing of the glenoid and/or SLAP lesion), history of trauma, presence of associated lesions (rotator cuff or Hill-Sachs lesion), presence of generalized ligament laxity, how the dislocation was reduced (by the patient or in a hospital environment) and how reliable the patient was regarding compliance with a rehabilitation protocol. By applying this score to a group of 80 patients, Habermeyer et al(18) found recurrence rates of 2.9% for patients who had been treated surgically and 10.9% for those treated conservatively.
Our criteria for indicating surgery after the first episode of dislocation partially corroborate those of Habermeyer: traumatic etiology; young patients or active young adult patients; practitioners of impact sports or types of sport that demand intense upper-arm activity; and presence of associated lesions that add to the instability.
Lack of healing of labral lesions in an anomalous site on the glenoid, absence of capsular, ligament and labral degeneration caused by disuse, persistent inflammatory reaction and residual anatomical deformity (Figure 1), and especially the presence of a severe lesion that is still open at the time of the repair (Figure 2), are relevant biological factors relating to the tissue healing process and functional rehabilitation. We believe that these factors favored the good results that we obtained among our patients.
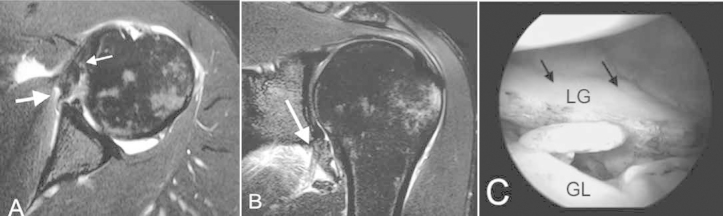
Figure 1.
Case 6: arthroscopic view of the right shoulder with the viewing device introduced through the anterosuperior portal, showing the detachment of the anterior labrum (larger arrow) with medial displacement (smaller arrow). GL – glenoid; LG – labrum of glenoid.
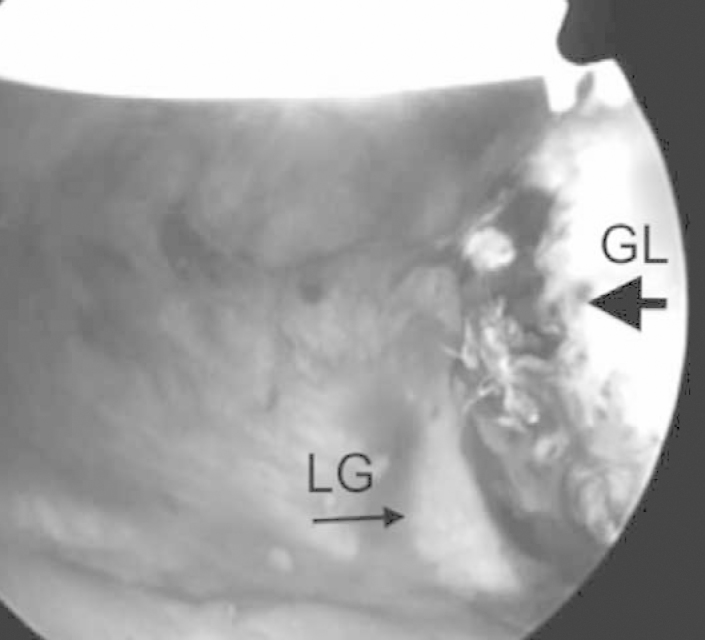
Figure 2.
Case 8: A) Magnetic arthro-resonance image of the left shoulder, in axial slice (T2), showing labral lesion (larger arrow) and capsular lesion (smaller arrow), which represent high-intensity trauma. B) Magnetic arthro-resonance image of the left shoulder, in coronal slice (T2), showing labral and capsular lesions (arrow). C) Arthroscopic image of the left shoulder with the optical device introduced through the posterior portal, showing severe anterior capsular-ligament lesion. LG – labrum of glenoid; GL – glenoid.
CONCLUSION
We did not have any recurrences of dislocations among our young patients or active young adult patients who were practitioners of impact sports or types of sport demanding intense activity of the upper limbs, after their first episode of traumatic dislocation, when they underwent Bankart lesion repair by means of arthroscopic viewing. This encourages us to indicate surgical treatment for patients with this profile.
However, it needs to be emphasized that other studies with a higher level of evidence and involving a greater number of patients are necessary for a conclusion to be reached regarding the best form of treatment after a first episode of TAD of the shoulder.
Footnotes
Work performed in the Department of Orthopedics and Traumatology, School of Medical Sciences, Santa Casa de São Paulo (DOT-FCMSCSP), “Fernandinho Simonsen” Wing (Director: Prof. Dr. Osmar Avanzi), São Paulo, SP.
REFERENCES
- 1.Jakobsen BW, Johannsen HV, Suder P, Søjbjerg JO. Primary repair versus conservative treatment of first-time traumatic anterior dislocation of the shoulder: a randomized study with 10-year follow-up. Arthroscopy. 2007;23(2):118–123. doi: 10.1016/j.arthro.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 2.Gamradt SC, Williams RJ, Warren RF. Arthoscopic treatment of shoulder instability. In: Rockwood CA Jr, Matsen FA 3rd, Wirth MA, Lippitt SB, editors. The shoulder. 4th ed. Saunders Elsevier; Philadelphia: 2009. pp. 940–996. [Google Scholar]
- 3.Robinson CM, Howes J, Murdoch H, Will E, Graham C. Functional outcome and riskof recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Joint Surg Am. 2006;88(11):2326–2336. doi: 10.2106/JBJS.E.01327. [DOI] [PubMed] [Google Scholar]
- 4.Bottoni CR, Wilckens JH, DeBerardino TM, D'Alleyrand JC, Rooney RC, Harpstrite JK. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30(4):576–580. doi: 10.1177/03635465020300041801. [DOI] [PubMed] [Google Scholar]
- 5.Sachs RA, Lin D, Stone ML, Paxton E, Kuney M. Can the need for future surgery for acute traumatic anterior shoulder dislocation be predicted? J Bone Joint Surg Am. 2007;89(8):1665–1674. doi: 10.2106/JBJS.F.00261. [DOI] [PubMed] [Google Scholar]
- 6.Brophy RH, Marx RG. The treatment of traumatic anterior instability of the shoulder: nonoperative and surgical treatment. Arthroscopy. 2009;25(3):298–304. doi: 10.1016/j.arthro.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 7.Larrain MV, Montenegro HJ, Mauas DM, Collazo CC, Pavón F. Arthroscopic management of traumatic anterior shoulder instability in collision athletes: analysis of 204 cases with a 4- to 9-year follow-up and results with the suture anchor technique. Arthroscopy. 2006;22(12):1283–1289. doi: 10.1016/j.arthro.2006.07.052. [DOI] [PubMed] [Google Scholar]
- 8.Owens BD, DeBerardino TM, Nelson BJ, Thurman J, Cameron KL, Taylor DC. Long-term follow-up of acute arthroscopic Bankart repair for initial anterior shoulder dislocations in young athletes. Am J Sports Med. 2009;37(4):669–673. doi: 10.1177/0363546508328416. [DOI] [PubMed] [Google Scholar]
- 9.Larrain MV, Botto GJ, Montenegro HJ, Mauas DM. Arthroscopic repair of acute traumatic anterior shoulder dislocation in young athletes. Arthroscopy. 2001;17(4):373–377. doi: 10.1053/jars.2001.23226. [DOI] [PubMed] [Google Scholar]
- 10.Maffet MW, Gartsman GM, Moseley B. Superior labrum-biceps tendon complex lesions of the shoulder. Am J Sports Med. 1995;23(1):93–98. doi: 10.1177/036354659502300116. [DOI] [PubMed] [Google Scholar]
- 11.Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am. 1978;60(1):1–16. [PubMed] [Google Scholar]
- 12.Ellman H, Kay SP. Arthroscopic subacromial decompression for chronic impingement. Two- to five-year results. J Bone Joint Surg Br. 1991;73(3):395–398. doi: 10.1302/0301-620X.73B3.1670435. [DOI] [PubMed] [Google Scholar]
- 13.Hawkins RJ, Bokor DJ. Clinical evaluation of shoulder problems. In: Rockwood CA Jr, Matsen FA, editors. The shoulder. 2nd ed. Saunders Elsevier; Philadelphia: 1998. pp. 175–180. [Google Scholar]
- 14.Kralinger FS, Golser K, Wischatta R, Wambacher M, Sperner G. Predicting recurrence after primary anterior shoulder dislocation. Am J Sports Med. 2002;30(1):116–120. doi: 10.1177/03635465020300010501. [DOI] [PubMed] [Google Scholar]
- 15.Robinson CM, Kelly M, Wakefield AE. Redislocation of the shoulder during the first six weeks after a primary anterior dislocation: risk factors and results of treatment. J Bone Joint Surg Am. 2002;84(9):1552–1559. doi: 10.2106/00004623-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 16.DeBerardino TM, Arciero RA, Taylor DC, Uhorchak JM. Prospective evaluation of arthroscopic stabilization of acute, initial anterior shoulder dislocations in young athletes. Two- to five-year follow-up. Am J Sports Med. 2001;29(5):586–592. doi: 10.1177/03635465010290051101. [DOI] [PubMed] [Google Scholar]
- 17.Checchia SL, Fregoneze M, Miyazaki AN, Doneux SP, Silva LA, Ossada A. Tratamento da capsulite adesiva com bloqueios seriados do nervo supra-escapular. Rev Bras Ortop. 2006;41(7):245–252. [Google Scholar]
- 18.Habermeyer P. The severity shoulder instability score (SSIS): a guide for therapy option for first traumatic shoulder dislocation [dissertação]. Edinburgh Escocia: 11° I.C.S.E.S. Congresso Mundial; 2010.