Abstract
Background
Brief interventions delivered in primary health care are effective in reducing excessive drinking; online behavior-changing technique interventions may be helpful. Physicians may actively encourage the use of such interventions by helping patients access selected websites (a process known as “facilitated access”). Although the therapeutic working alliance plays a significant role in the achievement of positive outcomes in face-to-face psychotherapy and its development has been shown to be feasible online, little research has been done on its impact on brief interventions. Strengthening patients’ perception of their physician’s endorsement of a website could facilitate the development of an effective alliance between the patient and the app.
Objective
We describe the implementation of a digitally mediated personal physician presence to enhance patient engagement with an alcohol-reduction website as part of the experimental online intervention in a noninferiority randomized controlled trial. We also report the feedback of the users on the module.
Methods
The Download Your Doctor module was created to simulate the personal physician presence for an alcohol-reduction website that was developed for the EFAR-FVG trial conducted in the Italian region of Friuli-Venezia-Giulia. The module was designed to enhance therapeutic alliance and thus improve outcomes in the intervention group (facilitated access to the website). Participating general and family practitioners could customize messages and visual elements and upload a personal photo, signature, and video recordings. To assess the perceptions and attitudes of the physicians, a semistructured interview was carried out 3 months after the start of the trial. Participating patients were invited to respond to a short online questionnaire 12 months following recruitment to investigate their evaluation of their online experiences.
Results
Nearly three-quarters (23/32, 72%) of the physicians interviewed chose to customize the contents of the interaction with their patients using the provided features and acknowledged the ease of use of the online tools. The majority of physicians (21/32, 57%) customized at least the introductory photo and video. Barriers to usage among those who did not customize the contents were time restrictions, privacy concerns, difficulties in using the tools, and considering the approach not useful. Over half (341/620, 55.0%) of participating patients completed the optional questionnaire. Many of them (240/341, 70.4%) recalled having noticed the personalized elements of their physicians, and the majority of those (208/240, 86.7%) reacted positively, considering the personalization to be of either high or the highest importance.
Conclusions
The use of a digitally mediated personal physician presence online was both feasible and welcomed by both patients and physicians. Training of the physicians seems to be a key factor in addressing perceived barriers to usage. Further research is recommended to study the mechanisms behind this approach and its impact.
Trial Registration
Clinicaltrials.gov NCT 01638338; https://clinicaltrials.gov/ct2/show/NCT01638338 (Archived by WebCite at http://www.webcitation.org/6f0JLZMtq)
Keywords: alcohol drinking, physician-patient relations, behavior and behavior mechanisms, research design, Internet, multimedia, primary health care, family physicians
Introduction
Alcohol is the third leading cause of diseases and premature death globally [1], and it has been estimated that it accounts for 3.8% of deaths and 4.6% of disability-adjusted life years [2]. Brief interventions delivered in primary health care settings have been shown to be both efficacious and effective in reducing excessive drinking in Italy and worldwide [3-7]. However, some individual large-scale pragmatic trials have failed to report significant findings [8-10], and no reductions in drinking or very small effects were observed in results from studies in probation offices, emergency departments, and among college students in Sweden and New Zealand [11-14]. Remarkably, the optimal contents and delivery strategies and the impact of the brief interventions on alcohol problems and specific population groups are not clear [7]. Comparing different brief intervention programs may be challenging because of differences in their contexts, the implementation strategies, and the indicators employed [6]. Moreover, there are important barriers to implementation, such as insufficient training, lack of resources, and time constraints, which prevent brief interventions from being employed widely [4,15-17].
Internet interventions based on behavior change techniques may be helpful to tackle these barriers [4,18]. Health care professionals may actively encourage the use of such digital applications by helping patients access selected websites (this process is known as “facilitated access”) [19]. Initially adopted primarily for the management of patients with mental health problems including depression and anxiety [20], facilitated access has been extended to addictive behaviors including smoking cessation and alcohol screening, as well health promotion and the management of long-term conditions [4,21-25]. Ensuring effective patient interaction with the website following facilitated access may be an issue [26], and additional mechanisms are therefore likely to be necessary to achieve more consistent engagement. In this paper, we describe the development and use of digitally mediated personal physician presence to enhance patient engagement with an alcohol-reduction website as part of the experimental online intervention in a noninferiority randomized controlled trial [27]. The intervention was designed to reinforce patients’ perception of their physician’s endorsement of the website and thus promote the development of an effective therapeutic working alliance between the patient and the application.
Described in a seminal paper by Bordin [28], the therapeutic working alliance refers to the personal relationship between the therapist and patient that stems from a collaborative endeavor to attain the goals of the treatment. Such an agreement on goals and tasks and the establishment of a personal bond of reciprocal positive feelings constitute the cornerstones of the alliance. There is a large body of evidence suggesting that it plays an important role in the achievement of positive outcomes in face-to-face psychotherapy [29-31], where patients who experience a strong alliance show more motivation and invest more effort to complete their treatment [30]. The importance of the alliance is also highlighted by researchers who suggest that nonspecific factors are largely responsible for the outcomes of different psychotherapies; these factors are common in the majority of the therapeutic interventions and include the healing setting, the expectations of improvement, and the therapeutic bond [32]. Little research has been done on the role of the therapeutic working alliance in treatment of alcohol problems or in brief interventions, but evidence is beginning to emerge that it may have an important influence on patient outcomes [33].
Researchers argue that the quality of the therapeutic working alliance is largely determined by the therapist variation, which may also explain the therapist’s effects on the outcomes [32]. Patient expectations of Internet-delivered behavioral change techniques may play a significant role as well [31], and according to Jasper et al, the development of the therapeutic alliance online may require more time than when therapy is delivered face-to-face [34]. In the context of facilitated access, agreement on goals and tasks can generally be achieved relatively easily online through the offer of a menu of options [34,35], but the maintenance and enhancement of the therapeutic alliance is considerably more problematic.
In health-promoting websites selected for facilitated access, customization of the information delivered to patients combined with multimedia emulation of their physician’s presence online may increase patient engagement, potentially by strengthening the online therapeutic alliance. Based on this hypothesis, we developed the digitally mediated primary care physician presence (Download Your Doctor) as a mechanism for achieving this end. We describe below how this was implemented in the context of a trial designed to determine whether facilitated access by primary care physicians to an alcohol-reduction website was superior to traditional face-to-face brief intervention [27] and to report the feedback of the users on the module.
Methods
The Download Your Doctor module was developed as an additional feature to an alcohol-reduction website [36] with the objective of generating a simulated personal physician presence in the online environment. The website was developed as part of a randomized controlled trial conducted in primary health care settings in the Italian Region of Friuli-Venezia-Giulia (EFAR-FVG), aiming to test the effectiveness of facilitated access to an alcohol-reduction website compared with standard face-to-face brief intervention [27,36]. Its contents and design were based on the UK counterpart, DownYourDrink, which has been described elsewhere [37,38]. The rationale for the trial is that general practitioners (GPs)/family physicians (FPs) are generally reluctant to screen for alcohol misuse and delivery rates of brief interventions are low [27,39]. The use of facilitated access to a selected website to provide patients with an opportunity to undertake screening and brief intervention online rather than in the consultation offers significant promise, but a trial was needed to establish noninferiority of this approach. The study protocol was approved by the Isontina Independent Local Health Unit Ethics Committee on June 14, 2012.
For the duration of the trial, the participating GPs/FPs provided facilitated access consisting of a short discussion followed by presentation to the patient of a pamphlet describing the website and containing the patient’s personal login code. The first 3 digits of the login code were specific to the general practitioner and the last 4 to the patient. The online alcohol screening module was based on the 3-item Alcohol Use Disorders Identification Test (AUDIT-C). Those scoring above the designated cut point were requested to provide consent to the trial and then undergo an online baseline assessment, followed by the randomized assignment to receive either online facilitated access to the alcohol-reduction website or the face-to-face intervention by their GP/FP. Follow-up assessment took place online at 3 and 12 months using the full version of the AUDIT questionnaire [40] and the EQ-5D [41].
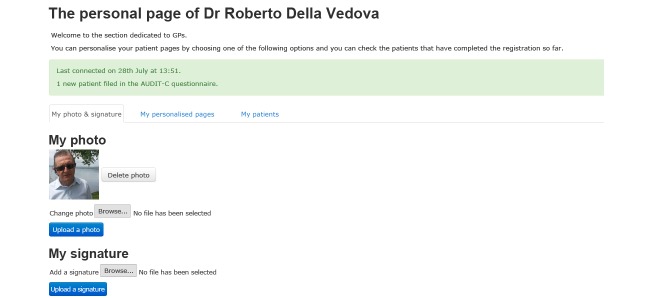
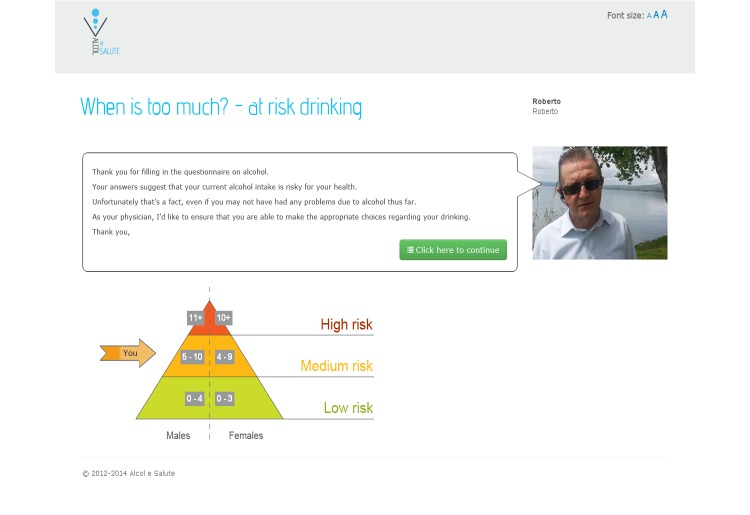
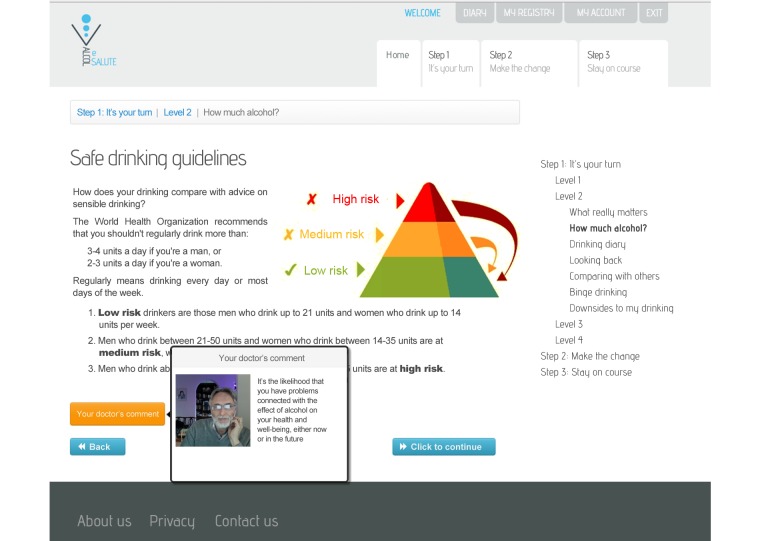
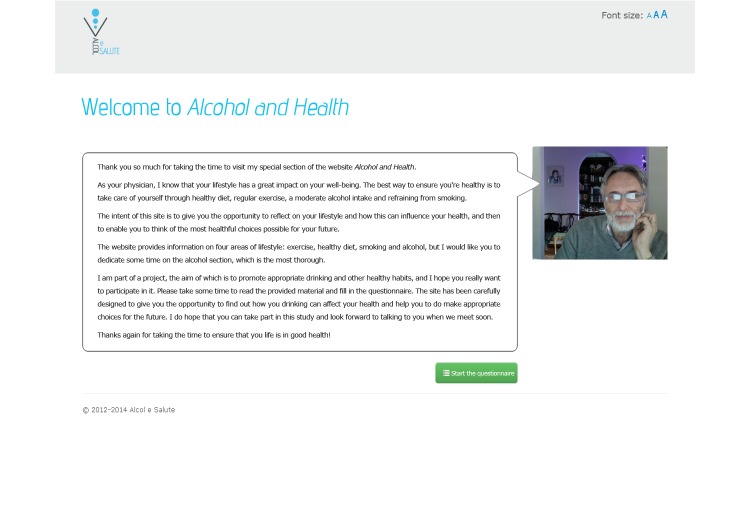
The Download Your Doctor facility enabled the GPs/FPs participating in the study to personally customize selected messages and visual elements of the user interface to be presented to their patients after logging on to the website and following screening (see Figure 1). Each practitioner was additionally able to upload their personal photograph and signature for integration with their messages on the website. The appearance of each message could thus be customized by inserting links and images shown in a “speech bubble” next to text and along with the photo of the GP/FP (see Figures 2-4). Finally, they were also given the option to upload video recordings in order to simulate online communication with their patients even more directly.
Figure 1.
The GP/FP customization page (adapted in English).
Figure 2.
The screening page with the personalized speech bubble (adapted in English).
Figure 4.
The GP/FP can provide customized comments on the different patient inputs (adapted in English).
Before the onset of the trial, the participating GPs/FPs were invited to attend a training session, during which a stepwise presentation of the website was carried out and the Download Your Doctor module was explained with interactive examples. Particular attention was given to the ways the physicians could enhance patient participation and adherence to the study. Subsequent use of the module by each participating physician was recorded by the study team.
To assess the perceptions and the attitudes of the physicians with regard to their participation in the study, an interview was conducted 3 months after the start of the trial. The interview was conducted by 2 psychologists using a semistructured questionnaire format. It sought information on such aspects of the trial as the nature of physicians’ interactions with the patients (recruitment and instructions) and their satisfaction with the participation in the trial. During the interview, the use and evaluation of the website (personalization, usability, and usefulness of the content) were also explored.
Moreover, a short online questionnaire was developed post hoc by the research team to evaluate the perceptions and attitudes of the trial participants about their experience in the study, their use of Internet and health-related websites, and the quality of their online experiences. A number of questions specifically sought information about the patient perceptions of the importance of the features related to the Download Your Doctor module. Five categories were available to rate the features (“highest,” “high,” “average,” “low,” “lowest”). Completion of the questionnaire was optional, and it was included in the final assessment that each patient was requested to undertake online 12 months following recruitment to the trial.
Figure 3.
The personalized welcome page (adapted in English).
Results
Of the 44 participating GP/FPs approached by the research team, 32 (73%) agreed to be interviewed, and 23 (72%) of those used the Download Your Doctor module and personalized some of its parts by uploading photos and/or adding their own text messages (see Table 1).
Table 1.
Personalization of the website (and lack of) among interviewed doctors (N=32).
| Personalization details | n (%) | |
| Interviewed doctors who personalized one or more elements of the website | 23 (72) | |
|
|
The introductory photo and video | 21 (57) |
|
|
The introductory text | 11 (34) |
| Interviewed doctors’ reasons for not personalizing the website | 9 (28) | |
|
|
Limited time | 3 (33) |
|
|
Seemed to be complicated | 2 (22) |
|
|
Seemed not useful | 2 (22) |
|
|
Unwilling to publish personal photos on the Internet | 3 (33) |
Physicians’ Evaluation of the Website
According to the feedback from the physicians, the website scored highly in the aspects of user-friendliness and intuitive navigation, while overall the contents were considered to be useful for their patients (see Table 2). No significant differences emerged between physicians who personalized the website and those who did not do so with regard to the aforementioned aspects of user-friendliness and content usefulness, as well as the level of interest and overall satisfaction with the participation in the trial (P>.10).
Table 2.
Physician feedback on the website based on Likert scales, ranging from 1-10 (lowest-highest).
| Survey question | Median | Interquartile range |
| To what degree do you find the website easy to browse and interact with? | 10 | 8-10 |
| To what extent do you rate the website’s contents and activities to be useful for the patients? | 8 | 8-10 |
Patients’ Evaluation of the Website
Of the 620 patients who completed the 12-month follow-up questionnaires, 341 (55.0%) also completed the optional questionnaire. The demographic characteristics and information technology (IT) skills of the sample are shown in Table 3.
Table 3.
Demographic characteristics and IT skills of the sample (N=341; only valid answers are shown).
| Characteristics | Values | |
| Gender, n (%) | ||
|
|
Males | 215 (64.2) |
|
|
Females | 120 (35.8) |
|
|
Age, mean (SD) interquartile range | 47.27 (14.60) 36.00-58.00 |
| IT skills, n (%) | ||
|
|
Poor | 47 (14.0) |
|
|
Basic | 90 (26.9) |
|
|
Intermediate | 82 (24.5) |
|
|
Advanced | 116 (34.6) |
Nearly three-quarters (240/341, 70.4%) of the patients recalled having noticed the personalized elements of their GPs/ FPs (see Table 4). There were no significant differences in the gender, age, and IT skills between the participants who noticed the personalization and those who did not (P≥.05). Similarly, the two groups did not differ in the frequency with which the participants used the Internet and various health-related websites (P≥.05).
Table 4.
Patient feedback on website (N=341).
| Questions | n (%) | |
| All respondents (n=341): “When you first logged into the website, do you remember having seen a photo or a text message from your GP?” | ||
|
|
Yes | 240 (70.4) |
|
|
No | 101 (29.6) |
| Respondents who recalled GP personalization of the website (n=240): “To what extent do you think that seeing a photo or a message from your GP improved your confidence towards the information provided by the website?” | ||
|
|
Lowest | 1 (0.4) |
|
|
Low | 5 (2.1) |
|
|
Average | 25 (10.5) |
|
|
High | 74 (31.0) |
|
|
Highest | 134 (56.1) |
| Respondents who did not recall GP personalization of the website (n=101, valid answers=100): “To what extent do you think that seeing a photo or a message from your GP could have improved your confidence towards the information provided by the website?” | ||
|
|
Lowest | 15 (14.9) |
|
|
Low | 14 (13.9) |
|
|
Average | 17 (16.8) |
|
|
High | 37 (36.6) |
|
|
Highest | 18 (17.8) |
Of those patients who noticed the personalization, the majority (208/240, 86.7%) considered such an approach to be of either high or the highest importance for their level of confidence towards the information provided by the website (see Table 4). There were no significant correlations between the level of their confidence and the age, IT skills, and frequency with which the Internet and the health-related websites were employed (P≥.05), while the level of their confidence did not differ between the two sexes (P≥.05).
Furthermore, approximately half of those who did not notice any personalized element (55/101, 54.4%) considered such a feature to be potentially of either high or the highest importance (see Table 4).
With regard to the participants’ evaluation of the website, only a few replies differed significantly between those who noticed the personalization and those who did not recall such elements (see Table 5). There were no significant differences between the two groups in the subjective evaluation of the individual alcohol consumption and the role that the website played (P≥.05): “Do you think that you have reduced your alcohol intake compared with a year ago?,” “Do you consider that your way of drinking today poses a risk to your health?,” “Do you think that the website was helpful in changing your way of drinking alcohol?”. Finally, the majority of the patients considered the website very easy to use, and no differences were found between the two groups (median 4.52 for those who recalled the personalization vs median 4.35 for those who did not recall such elements).
Table 5.
Significant differences in the replies between the participants that recalled the personalization and those who did not do so. Answers were based on a 5-point Likert scale, ranging from 1-5 (lowest-highest).
| Questions | N | Mean | Standard deviation | t (df) | P | |
| “Do you assess your participation in the study positively?” | ||||||
|
|
Respondents who recalled the personalization | 238 | 4.09 | 0.86 | 3.18 (317) | .002 |
|
|
Respondents who did not recall the personalization | 101 | 3.74 | 1.04 |
|
|
| “Did you find the contents of the site interesting?” | ||||||
|
|
Respondents who recalled the personalization | 108 | 4.31 | 0.76 | 2.85 (154) | .005 |
|
|
Respondents who did not recall the personalization | 48 | 3.90 | 0.97 |
|
|
| “Would you recommend the website to others?” | ||||||
|
|
Respondents who recalled the personalization | 108 | 4.23 | 0.82 | 2.34 (154) | .020 |
|
|
Respondents who did not recall the personalization | 48 | 3.88 | 1.00 |
|
|
Discussion
Principal Findings
The Download Your Doctor module was developed to enhance the therapeutic alliance between patients and physicians, in order to improve the outcomes of a trial on facilitated access to an alcohol-reduction website. Our hypothesis was that while patients may appreciate the opportunities presented through facilitated access, there might be a risk that they perceive it as less valuable than face-to-face intervention. It was therefore important to provide for continuity of the therapeutic alliance while the patient was online. The GPs/FPs were provided with features enabling them to customize the contents of the interaction with their patients and the majority of them chose to do so, acknowledging the ease of use of the online tools. Most patients reported noticing the novelty of this approach and reacted positively to such customizations.
Providing general health communication materials may have limited effect when the information is not relevant to the individual’s context [42]. Tailored communication has been used in behavioral interventions delivered in print and by telephone. Yet the advances of technology have yielded new possibilities for this increasingly common practice [43], and interventions using computer tailoring to assess individuals and deliver adapted content and feedback according to the user’s characteristics have been proven to result in more behavioral changes compared to standard programs [42,44,45]. Such interventions may be more effective as they contain fewer unnecessary messages and increase the relevance of the information to the individuals, who are more likely to assimilate it [43-48]. Although interventions using social networks seem to be effective in behavioral change and higher recruitment and retention may be achieved by taking advantage of the participants’ existing social networks [49], their implementation in alcohol-reduction applications seems to be scarce [18]. Furthermore, personalized feedback based on the patient’s answers may have a positive influence on the therapeutic working alliance in Internet-delivered programs [18,30] and there is some evidence that the use of multimedia emulating a human therapist may further enhance its strength [50,51]. Self-help texts may also help foster an alliance based on the assumption that the patient attributes the preparation of the text to an empathetic clinician thus considering him/her present during the program [35,52].
As with many digital health applications, barriers to usage may include time limitations, insufficient skills, and privacy concerns [53-55]. The level of digital literacy of the practitioners may have played a role in whether they customized the contents of the module or not. Even though digital literacy was not assessed, the feedback from physicians relating to navigation and interaction with the website was generally positive and suggested that it was feasible for the majority to carry out the tasks of personalization after the training session. In fact, training seems to be a key factor in addressing the perceived barriers to usage, and according to literature it can also tackle the time constraint concerns, as more physicians are able to recognize the potential usefulness of the proposed tool [55].
The study was exploratory in nature and has a number of limitations. Notwithstanding the patients attributing a high significance to the customization, its impact on the outcomes of the trial could not be robustly evaluated due primarily to the variable degree of customization applied by the GPs/FPs. Not only did the content and multimedia elements vary among the participating physicians, but also some of them delayed customization until after the onset of the study. The main trial was designed to measure the effectiveness of the facilitated access to a dedicated alcohol-reduction website compared with the standard face-to-face brief intervention in primary care settings, while the evaluation of the Download Your Doctor module was added post hoc. As a result, the methodology and the available data were not adequate to enable us to draw firm conclusions. For example, we were unable to exclude “false positive” cases, namely patients who stated that they had noticed customization elements when their doctors had not actually made any modifications to the original presentation of the website. Nonetheless, while the study should be considered exploratory, as far as we are aware it is the first to address the impact of a digitally mediated primary care physician presence in an online application. As such, we have reported primarily on the feasibility of the implementation of this approach, which provides a foundation for future research into improving the quality of online therapeutic alliances by offering continuity of the already established relationship between patient and physician in the context of facilitated access to an intervention website.
Conclusion
We have described a novel approach using a digitally mediated primary care physician presence based on customized content by GPs/FPs in order to increase patient engagement and promote their online therapeutic working alliance. Our findings suggest that this approach was both feasible and welcomed by both patients and physicians. As behavior change interventions are based on multiple techniques that may work synergistically and have variable effects in different patient groups [18], further investigation should focus on determining the mechanisms of this approach and its impact on the outcomes facilitated access to Internet-delivered brief interventions programs.
Acknowledgments
The authors wish to extend our gratitude to all the physicians that participated in the EFAR-FVG project: Acampora Giosué, Bravo Maria Angela, Bregant Chiara, BunelloGianna, Butà Leonardo, Casatta Lucia, Castellarin Egidio, Chamouni Benyamin Moshé, Cisilin Maria Pia, Condello Clemente, Della Vedova Roberto, Drigani Nelly, Ermacora Tiziano, Falcidia Alessandro, Fasiolo Adriana, Florio Angelo, Gubiani Mauro, Iacuzzo Gianni, Ietri Edi, Latella Giuseppe, Lucca Guglielmo, Mamolo Ciro, Matera Carmelo, Mei Lucia, Melon Francesca, Mezzasalma Emilio, Milan Isabella, Miotti Carlo, Panizzo Gian Franco, Pighin Francesca, Principato Raffaela, Revignas Pierina, Rolff Antonella, Rupalti Ivana, Sellibara Rosanna, Sereni Michela, Silverii Gianfranco, Taglialatela Giuseppe, Toffoletti Chiara, Toffolo Massimo, Tonelli Laura Ivana, Trevisani Simone, Troisi Roberto, Tubaro Gianni, Vallini Roberto, Zappalà Elisabetta, and Zappi Antonio.
This project was possible thanks to the co-funding of the Italian Ministry of Health and the Region Friuli Venezia Giulia (Grant: RF-2012-2318620).
Finally, we wish to thank Richard McGregor for his work on the development of the website.
Abbreviations
- AUDIT
Alcohol Use Disorders Identification Test
- EFAR-FVG
effectiveness of primary care based Facilitated access to Alcohol Reduction website – a randomized controlled noninferiority trial in Region Friuli Venezia Giulia, IT
- GP
general practitioner
- FP
family physician
- IT
information technology
Footnotes
Conflicts of Interest: CL is the cofounder and Chief Executive Officer at Lumos Medica Srl, which provides software solutions for clinical trials.
PW has intellectual property rights for the Downyourdrink website, is Chief Medical Advisor to the UK charity Drinkaware, and has provided private consultancy on the topic of screening and brief interventions to several agencies.
References
- 1.Anderson P, Møller L, Galea G, World Health Organization . Alcohol in the European Union: consumption, harm and policy approaches. Copenhagen, Denmark: World Health Organization Regional Office for Europe; 2012. [Google Scholar]
- 2.Rehm J, Zatonksi W, Taylor B, Anderson P. Epidemiology and alcohol policy in Europe. Addiction. 2011 Mar;106 Suppl 1:11–19. doi: 10.1111/j.1360-0443.2010.03326.x. [DOI] [PubMed] [Google Scholar]
- 3.Kaner EFS, Beyer F, Dickinson HO, Pienaar E, Campbell F, Schlesinger C, Heather N, Saunders J, Burnand B. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev. 2007;(2):CD004148. doi: 10.1002/14651858.CD004148.pub3. [DOI] [PubMed] [Google Scholar]
- 4.Keurhorst MN, Anderson P, Spak F, Bendtsen P, Segura L, Colom J, Reynolds J, Drummond C, Deluca P, van SB, Mierzecki A, Kłoda K, Wallace P, Newbury-Birch D, Kaner E, Gual T, Laurant MGH. Implementing training and support, financial reimbursement, and referral to an internet-based brief advice program to improve the early identification of hazardous and harmful alcohol consumption in primary care (ODHIN): study protocol for a cluster randomized factorial trial. Implement Sci. 2013;8:11. doi: 10.1186/1748-5908-8-11. http://www.implementationscience.com/content/8//11 .1748-5908-8-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Angus C, Scafato E, Ghirini S, Torbica A, Ferre F, Struzzo P, Purshouse R, Brennan A. Cost-effectiveness of a programme of screening and brief interventions for alcohol in primary care in Italy. BMC Fam Pract. 2014;15:26. doi: 10.1186/1471-2296-15-26. http://bmcfampract.biomedcentral.com/articles/10.1186/1471-2296-15-26 .1471-2296-15-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colom J, Scafato E, Segura L, Gandin C, Struzzo P. Brief interventions implementation on alcohol from the European health systems perspective. Front Psychiatry. 2014;5:161. doi: 10.3389/fpsyt.2014.00161. doi: 10.3389/fpsyt.2014.00161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O'Donnell A, Anderson P, Newbury-Birch D, Schulte B, Schmidt C, Reimer J, Kaner E. The impact of brief alcohol interventions in primary healthcare: a systematic review of reviews. Alcohol Alcohol. 2014;49(1):66–78. doi: 10.1093/alcalc/agt170. http://alcalc.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=24232177 .agt170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O'Donnell A, Wallace P, Kaner E. From efficacy to effectiveness and beyond: what next for brief interventions in primary care? Front Psychiatry. 2014;5:113. doi: 10.3389/fpsyt.2014.00113. doi: 10.3389/fpsyt.2014.00113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaner E, Bland M, Cassidy P, Coulton S, Dale V, Deluca P, Gilvarry E, Godfrey C, Heather N, Myles J, Newbury-Birch D, Oyefeso A, Parrott S, Perryman K, Phillips T, Shepherd J, Drummond C. Effectiveness of screening and brief alcohol intervention in primary care (SIPS trial): pragmatic cluster randomised controlled trial. BMJ. 2013;346:e8501. doi: 10.1136/bmj.e8501. http://www.bmj.com/cgi/pmidlookup?view=long&pmid=23303891 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Butler CC, Simpson SA, Hood K, Cohen D, Pickles T, Spanou C, McCambridge J, Moore L, Randell E, Alam MF, Kinnersley P, Edwards A, Smith C, Rollnick S. Training practitioners to deliver opportunistic multiple behaviour change counselling in primary care: a cluster randomised trial. BMJ. 2013;346:f1191. doi: 10.1136/bmj.f1191. http://www.bmj.com/cgi/pmidlookup?view=long&pmid=23512758 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drummond C, Deluca P, Coulton S, Bland M, Cassidy P, Crawford M, Dale V, Gilvarry E, Godfrey C, Heather N, McGovern R, Myles J, Newbury-Birch D, Oyefeso A, Parrott S, Patton R, Perryman K, Phillips T, Shepherd J, Touquet R, Kaner E. The effectiveness of alcohol screening and brief intervention in emergency departments: a multicentre pragmatic cluster randomized controlled trial. PLoS One. 2014;9(6):e99463. doi: 10.1371/journal.pone.0099463. http://dx.plos.org/10.1371/journal.pone.0099463 .PONE-D-14-01976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Newbury-Birch D, Coulton S, Bland M, Cassidy P, Dale V, Deluca P, Gilvarry E, Godfrey C, Heather N, Kaner E, McGovern R, Myles J, Oyefeso A, Parrott S, Patton R, Perryman K, Phillips T, Shepherd J, Drummond C. Alcohol screening and brief interventions for offenders in the probation setting (SIPS Trial): a pragmatic multicentre cluster randomized controlled trial. Alcohol Alcohol. 2014;49(5):540–548. doi: 10.1093/alcalc/agu046. http://alcalc.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=25063992 .agu046 [DOI] [PubMed] [Google Scholar]
- 13.McCambridge J, Bendtsen M, Karlsson N, White IR, Nilsen P, Bendtsen P. Alcohol assessment and feedback by email for university students: main findings from a randomised controlled trial. Br J Psychiatry. 2013 Nov;203(5):334–340. doi: 10.1192/bjp.bp.113.128660. http://bjp.rcpsych.org/cgi/pmidlookup?view=long&pmid=24072758 .bjp.bp.113.128660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kypri K, Vater T, Bowe SJ, Saunders JB, Cunningham JA, Horton NJ, McCambridge J. Web-based alcohol screening and brief intervention for university students: a randomized trial. JAMA. 2014 Mar 26;311(12):1218–1224. doi: 10.1001/jama.2014.2138. http://europepmc.org/abstract/MED/24668103 .1849990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Drummond C, Gual A, Goos C, Godfrey C, Deluca P, Von Der Goltz C, Gmel G, Scafato E, Wolstenholme A, Mann K, Coulton S, Kaner E. Identifying the gap between need and intervention for alcohol use disorders in Europe. Addiction. 2011 Mar;106 Suppl 1:31–36. doi: 10.1111/j.1360-0443.2010.03335.x. [DOI] [PubMed] [Google Scholar]
- 16.Anderson P, Wojnar M, Jakubczyk A, Gual A, Reynolds J, Segura L, Sovinova H, Csemy L, Kaner E, Newbury-Birch D, Fornasin A, Struzzo P, Ronda G, van SB, Keurhorst M, Laurant M, Ribeiro C, do RF, Alves I, Scafato E, Gandin C, Kolsek M. Managing alcohol problems in general practice in Europe: results from the European ODHIN survey of general practitioners. Alcohol Alcohol. 2014;49(5):531–539. doi: 10.1093/alcalc/agu043. http://alcalc.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=25031247 .agu043 [DOI] [PubMed] [Google Scholar]
- 17.Kolsek M, Struzzo P, Svab I. Qualitative study on community and primary health care involvement on alcohol and tobacco actions in seven European countries. Subst Use Misuse. 2008;43(3-4):303–316. doi: 10.1080/10826080701202759.791726194 [DOI] [PubMed] [Google Scholar]
- 18.Crane D, Garnett C, Brown J, West R, Michie S. Behavior change techniques in popular alcohol reduction apps: content analysis. J Med Internet Res. 2015;17(5):e118. doi: 10.2196/jmir.4060. http://www.jmir.org/2015/5/e118/ v17i5e118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.López-Pelayo H, Wallace P, Segura L, Miquel L, Díaz E, Teixidó L, Baena B, Struzzo P, Palacio-Vieira J, Casajuana C, Colom J, Gual A. A randomised controlled non-inferiority trial of primary care-based facilitated access to an alcohol reduction website (EFAR Spain): the study protocol. BMJ Open. 2014;4(12):e007130. doi: 10.1136/bmjopen-2014-007130. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=25552616 .bmjopen-2014-007130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cavanagh K, Shapiro DA, Van Den Berg S, Swain S, Barkham M, Proudfoot J. The effectiveness of computerized cognitive behavioural therapy in routine care. Br J Clin Psychol. 2006 Nov;45(Pt 4):499–514. doi: 10.1348/014466505X84782. [DOI] [PubMed] [Google Scholar]
- 21.Clark TC, Johnson EA, Kekus M, Newman J, Patel PS, Fleming T, Robinson E. Facilitating access to effective and appropriate care for youth with mild to moderate mental health concerns in new zealand. J Child Adolesc Psychiatr Nurs. 2014 Nov;27(4):190–200. doi: 10.1111/jcap.12095. [DOI] [PubMed] [Google Scholar]
- 22.Harris SK, Csémy L, Sherritt L, Starostova O, Van HS, Johnson J, Boulter S, Brooks T, Carey P, Kossack R, Kulig JW, Van VN, Knight JR. Computer-facilitated substance use screening and brief advice for teens in primary care: an international trial. Pediatrics. 2012 Jun;129(6):1072–1082. doi: 10.1542/peds.2011-1624. http://pediatrics.aappublications.org/cgi/pmidlookup?view=long&pmid=22566420 .peds.2011-1624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kypri K, Langley JD, Saunders JB, Cashell-Smith ML, Herbison P. Randomized controlled trial of web-based alcohol screening and brief intervention in primary care. Arch Intern Med. 2008 Mar 10;168(5):530–536. doi: 10.1001/archinternmed.2007.109.168/5/530 [DOI] [PubMed] [Google Scholar]
- 24.Kypri K, McAnally HM. Randomized controlled trial of a web-based primary care intervention for multiple health risk behaviors. Prev Med. 2005;41(3-4):761–766. doi: 10.1016/j.ypmed.2005.07.010.S0091-7435(05)00111-8 [DOI] [PubMed] [Google Scholar]
- 25.Parekh S, Vandelanotte C, King D, Boyle FM. Improving diet, physical activity and other lifestyle behaviours using computer-tailored advice in general practice: a randomised controlled trial. Int J Behav Nutr Phys Act. 2012;9:108. doi: 10.1186/1479-5868-9-108. http://www.ijbnpa.org/content/9//108 .1479-5868-9-108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.White A, Kavanagh D, Stallman H, Klein B, Kay-Lambkin F, Proudfoot J, Drennan J, Connor J, Baker A, Hines E, Young R. Online alcohol interventions: a systematic review. J Med Internet Res. 2010;12(5):e62. doi: 10.2196/jmir.1479. http://www.jmir.org/2010/5/e62/ v12i5e62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Struzzo P, Scafato E, McGregor R, Della VR, Verbano L, Lygidakis C, Tersar C, Crapesi L, Tubaro G, Freemantle N, Wallace P. A randomised controlled non-inferiority trial of primary care-based facilitated access to an alcohol reduction website (EFAR-FVG): the study protocol. BMJ Open. 2013;3(2) doi: 10.1136/bmjopen-2012-002304. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=23408073 .bmjopen-2012-002304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research & Practice. 1979;16(3):252–260. doi: 10.1037/h0085885. [DOI] [Google Scholar]
- 29.Preschl B, Maercker A, Wagner B. The working alliance in a randomized controlled trial comparing online with face-to-face cognitive-behavioral therapy for depression. BMC Psychiatry. 2011;11:189. doi: 10.1186/1471-244X-11-189. http://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-11-189 .1471-244X-11-189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Anderson RE, Spence SH, Donovan CL, March S, Prosser S, Kenardy J. Working alliance in online cognitive behavior therapy for anxiety disorders in youth: comparison with clinic delivery and its role in predicting outcome. J Med Internet Res. 2012;14(3):e88. doi: 10.2196/jmir.1848. http://www.jmir.org/2012/3/e88/ v14i3e88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bergman NL, Carlbring P, Linna E, Andersson G. Role of the working alliance on treatment outcome in tailored internet-based cognitive behavioural therapy for anxiety disorders: randomized controlled pilot trial. JMIR Res Protoc. 2013;2(1):e4. doi: 10.2196/resprot.2292. http://www.researchprotocols.org/2013/1/e4/ v2i1e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.DeRubeis R, Brotman M, Gibbons C. A Conceptual and Methodological Analysis of the Nonspecifics Argument. Clinical Psychology: Science and Practice. 2005;12(2):174–183. doi: 10.1093/clipsy.bpi022. [DOI] [Google Scholar]
- 33.Cook S, Heather N, McCambridge J, United Kingdom Alcohol Treatment Trial Research Team The role of the working alliance in treatment for alcohol problems. Psychol Addict Behav. 2015 Jun;29(2):371–381. doi: 10.1037/adb0000058. http://europepmc.org/abstract/MED/25961147 .2015-20858-001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jasper K, Weise C, Conrad I, Andersson G, Hiller W, Kleinstäuber M. The working alliance in a randomized controlled trial comparing Internet-based self-help and face-to-face cognitive behavior therapy for chronic tinnitus. Internet Interventions. 2014 Apr;1(2):49–57. doi: 10.1016/j.invent.2014.04.002. [DOI] [Google Scholar]
- 35.Andersson G, Paxling B, Wiwe M, Vernmark K, Felix CB, Lundborg L, Furmark T, Cuijpers P, Carlbring P. Therapeutic alliance in guided internet-delivered cognitive behavioural treatment of depression, generalized anxiety disorder and social anxiety disorder. Behav Res Ther. 2012 Sep;50(9):544–550. doi: 10.1016/j.brat.2012.05.003.S0005-7967(12)00085-X [DOI] [PubMed] [Google Scholar]
- 36.Struzzo P, Wallace P, Della VR, Lygidakis C, Tersar C, Marcatto F, Ferrante D, Verbano L, Scafuri F, Scafato E. Ti vuoi bene. 2014. [2015-10-03]. https://www.itatvb.it/
- 37.Linke S, Brown A, Wallace P. Down your drink: a web-based intervention for people with excessive alcohol consumption. Alcohol Alcohol. 2004;39(1):29–32. doi: 10.1093/alcalc/agh004. http://alcalc.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=14691071 . [DOI] [PubMed] [Google Scholar]
- 38.Linke S, Harrison R, Wallace P. A Web-based intervention used in general practice for people with excessive alcohol consumption. J Telemed Telecare. 2005;11 Suppl 1:39–41. doi: 10.1258/1357633054461895. [DOI] [PubMed] [Google Scholar]
- 39.Anderson P, Chisholm D, Fuhr DC. Effectiveness and cost-effectiveness of policies and programmes to reduce the harm caused by alcohol. Lancet. 2009 Jun 27;373(9682):2234–2246. doi: 10.1016/S0140-6736(09)60744-3.S0140-6736(09)60744-3 [DOI] [PubMed] [Google Scholar]
- 40.Struzzo P, De Faccio S, Moscatelli E. Early detection of subjects at risk of alcohol abuse in a setting of primary health care in Italy: adaptation of a shorter version of the AUDIT Questionnaire and evaluation of its efficacy in the Italian context. Bollettino delle Farmacodipendenze e Alcolismo. 2006;XXIX:20–25. http://www.iss.it/binary/alco/cont/Boll%20farm%20alcol%2006%2029%201-6.1182506126.pdf . [Google Scholar]
- 41.Rabin R, de CF. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001 Jul;33(5):337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- 42.Kreuter M. Tailoring health messages: customizing communication with computer technology. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- 43.Krebs P, Prochaska JO, Rossi JS. A meta-analysis of computer-tailored interventions for health behavior change. Prev Med. 2010;51(3-4):214–221. doi: 10.1016/j.ypmed.2010.06.004. http://europepmc.org/abstract/MED/20558196 .S0091-7435(10)00231-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dijkstra A, De VH. The development of computer-generated tailored interventions. Patient Educ Couns. 1999 Feb;36(2):193–203. doi: 10.1016/s0738-3991(98)00135-9.S0738-3991(98)00135-9 [DOI] [PubMed] [Google Scholar]
- 45.Schulz DN, Candel MJ, Kremers SP, Reinwand DA, Jander A, de VH. Effects of a Web-based tailored intervention to reduce alcohol consumption in adults: randomized controlled trial. J Med Internet Res. 2013;15(9):e206. doi: 10.2196/jmir.2568. http://www.jmir.org/2013/9/e206/ v15i9e206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Campbell MK, DeVellis BM, Strecher VJ, Ammerman AS, DeVellis RF, Sandler RS. Improving dietary behavior: the effectiveness of tailored messages in primary care settings. Am J Public Health. 1994 May;84(5):783–787. doi: 10.2105/ajph.84.5.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Todkill D, Powell J. Participant experiences of an internet-based intervention and randomised control trial: interview study. BMC Public Health. 2013;13:1017. doi: 10.1186/1471-2458-13-1017. http://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-13-1017 .1471-2458-13-1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bottorff JL, Struik LL, Bissell LJL, Graham R, Stevens J, Richardson CG. A social media approach to inform youth about breast cancer and smoking: an exploratory descriptive study. Collegian. 2014;21(2):159–168. doi: 10.1016/j.colegn.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 49.Laranjo L, Arguel A, Neves AL, Gallagher AM, Kaplan R, Mortimer N, Mendes GA, Lau Annie Y S The influence of social networking sites on health behavior change: a systematic review and meta-analysis. J Am Med Inform Assoc. 2015 Jan;22(1):243–256. doi: 10.1136/amiajnl-2014-002841. http://jamia.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=25005606 .amiajnl-2014-002841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lieberman DZ. Effects of a personified guide on adherence to an online program for alcohol abusers. Cyberpsychol Behav. 2006 Oct;9(5):603–607. doi: 10.1089/cpb.2006.9.603. [DOI] [PubMed] [Google Scholar]
- 51.Barazzone N, Cavanagh K, Richards DA. Computerized cognitive behavioural therapy and the therapeutic alliance: a qualitative enquiry. Br J Clin Psychol. 2012 Nov;51(4):396–417. doi: 10.1111/j.2044-8260.2012.02035.x. [DOI] [PubMed] [Google Scholar]
- 52.Richardson R, Richards DA, Barkham M. Self-help books for people with depression: the role of the therapeutic relationship. Behav Cogn Psychother. 2010 Jan;38(1):67–81. doi: 10.1017/S1352465809990452.S1352465809990452 [DOI] [PubMed] [Google Scholar]
- 53.Barnett S, Jones SC, Bennett S, Iverson D, Bonney A. Usefulness of a virtual community of practice and web 2.0 tools for general practice training: experiences and expectations of general practitioner registrars and supervisors. Aust J Prim Health. 2013;19(4):292–296. doi: 10.1071/PY13024.PY13024 [DOI] [PubMed] [Google Scholar]
- 54.Higgins O, Barry M, Dmegan C. European Centre for Disease Control. Stockholm: ECDC; 2011. A literature review on health information seeking behaviour on the web: a health consumer and health professional perspective. [Google Scholar]
- 55.Barnett S, Jones SC, Bennett S, Iverson D, Bonney A. Perceptions of family physician trainees and trainers regarding the usefulness of a virtual community of practice. J Med Internet Res. 2013;15(5):e92. doi: 10.2196/jmir.2555. http://www.jmir.org/2013/5/e92/ v15i5e92 [DOI] [PMC free article] [PubMed] [Google Scholar]