Abstract
Objective: To assess the correlation between post-traumatic kyphosis in patients with thoracolumbar burst fractures undergoing surgical treatment and the functional result from treatment. Methods: A retrospective study was conducted on 27 patients with thoracolumbar burst fractures according to Denis and A3 to Margerl's classification who met the inclusion criteria for this sample and underwent surgical treatment with a minimum follow-up of six months. The patients’ mean age was 46.96, with a range from 16 to 73 years. The treatment outcome was evaluated based on applying the short-form 36 (SF-36) quality of life questionnaire, Denis pain and work scale and visual pain scale. The kyphosis was measured according to the Cobb method at the end of the follow-up. Results: The residual kyphosis was found not to correlate with the SF-36, Denis pain and work scale or visual pain score (p > 0.05). Conclusion: There is no correlation between the final clinical result and residual kyphosis in patients with thoracolumbar burst fractures who undergo surgical treatment.
Keywords: Spinal Fractures/therapy, Spinal Fractures/complications, Kyphosis
INTRODUCTION
Thoracolumbar burst fractures result from axial compression with rupture of the anterior and medial structures of the vertebral body, with retropulsion of a bone fragment into the spinal canal and an increase in the interpedicular distance. This region is a common site for injuries, with frequencies ranging from 10 to 45%1, 2, 3.
This type of injury occurs frequently in young individuals of productive age and results from high-energy trauma. It may be associated with other injuries, such as fractures at other levels of the spine, or in limbs or the pelvis, and chest and abdominal injuries(4).
Around 90% of all spinal fractures occur between T11 and L4, and around 14 to 17% are classified as burst fractures. This region is sensitive to injury for three reasons: loss of the stabilization provided by the ribs and thoracic musculature; the transition from kyphotic thoracic curvature to lordotic lumbar curvature; and the change in orientation of the joint facets from coronal in the thoracic spine to sagittal in the lumbar spine(4).
Thoracolumbar burst fractures can be classified using the AO method, as originally described by Magerl et al(5). Type A comprises axial compression fractures affecting the vertebral body. Subtype A1 includes fractures with impaction of spongy bone without fragmentation, subtype A2 includes fractures with sagittal or coronal shearing and subtype A3 consists of cases of partial or total comminution with or without retropulsion of fragments to the spinal canal. Subtype A3 can also be stratified as A3.1, comprising incomplete burst fractures; A3.2, burst with shearing; and A3.3, complete burst (Figure 1). Type β consists of fractures due to flexion-distraction, and type C consists of any fracture mentioned above with a superimposed rotational component1, 5.
Figure 1.
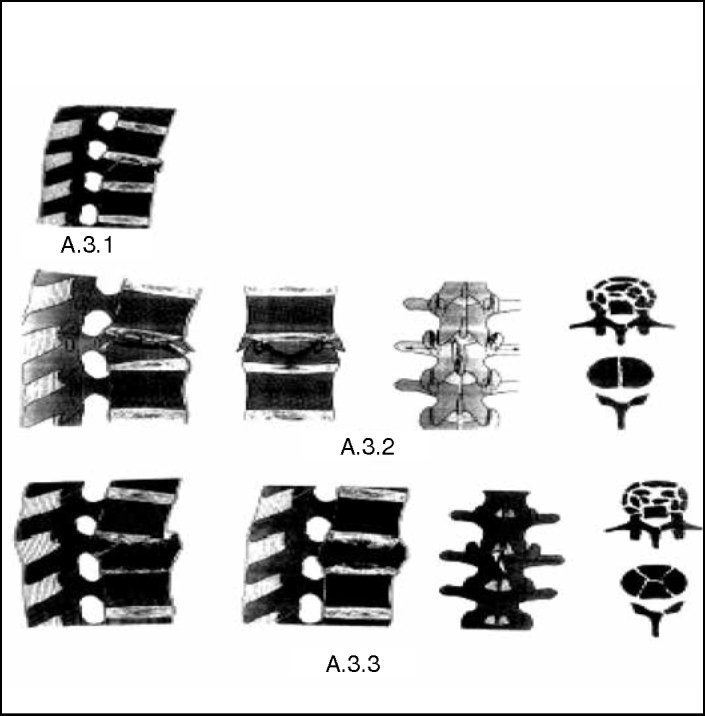
Magerl classification(6).
Some patients with burst fractures develop progressive mechanical instability, characterized by increased kyphosis, back pain and neurological sequelae7, 8.
Unstable fractures with kyphosis > 30°, height loss > 50%, compression of the spinal canal > 50% and associated neurological deficits generally present an indication for surgical treatment, according to most authors(9). However, for thoracolumbar burst fractures without signs of instability and with normal neurological examinations, there are divergences regarding the treatment method. Authors who advocate a surgical procedure affirm that this provides better correction of kyphosis, thereby diminishing pain and future degenerative alterations; prevents neurological deterioration and recurrence of the deformity; and reduces the duration of immobilization, resting and hospital stay10, 11, 12, 13.
Recurrence of kyphosis following surgical treatment of this type of fracture has already been reported in the literature. Its frequency is correlated with the type of surgery performed, the initial kyphosis and the reduction in the height of the vertebral body. Moreover, it occurs more frequently in patients who have undergone removal of the synthesis material(14) (Figure 2).
Figure 2.

Long-term postoperative result from thoracolumbar fracture, showing evolution with residual kyphosis.
OBJECTIVE
The aim of this study was to evaluate the correlation between recurrence of kyphosis and function, in patients who underwent surgical treatment of thoracolumbar burst fractures.
MATERIALS AND METHODS
A retrospective cross-sectional study was conducted at the Department of Orthopedics and Traumatology, Santa Casa de Misericórdia de São Paulo. All the medical files from patients with thoracolumbar burst fractures hospitalized between 1991 and 2010 were retrieved from the Medical Archive and Statistics Service (SAME).
Patients with burst fractures as defined using the Denis criteria and Magerl classification of subtype A3(5) who had been followed up for at least six months and who responded to a recall for clinical reassessment were included in this study, by means of questionnaires and radiographs.
Cases without complete documentation (medical files and radiographs), patients who did not respond to the recall, patients with pathological fractures and victims of firearm wounds were excluded. Patients admitted more than 10 days after the date of the fracture (late fractures) were also excluded.
The patients were evaluated based on the Short
Rev Bras Ortop. 2012;47(4):474–8 Form 36 (SF-36) quality-of-life questionnaire(15), in its version validated for the Portuguese language. The Denis work and pain scales were also applied(1) (Tables 1 and 2).
Table 1.
Functional pain scale according to Denis(1).
| Score | Criteria of the pain scale |
|---|---|
| 1 | No pain |
| 2 | Minimal pain, without using medication |
| 3 | Moderate pain, with occasional use of medication |
| 4 | Moderate to severe pain, with constant use of medication |
| 5 | Severe pain, with chronic use of medication |
Table 2.
Functional work scale according to Denis(1).
| Score | Criteria of the functional work scale |
|---|---|
| 1 | Returned to heavy work |
| 2 | Returned to sedentary work, without weight restriction |
| 3 | Returned to work, but changed activity |
| 4 | Returned to work, but only part-time |
| 5 | Incapable of working |
Measurements of kyphosis were made in accordance with the Cobb method(16), after producing lateral-view radiographs of the segment affected, at the time of the recall for applying the questionnaire.
For the statistical analyses of this study, the significance level was taken to be 5%. The SPSS software (Statistical Package for the Social Sciences), version 13.0, was used to analyze and produce the results.
Spearman's correlation analysis was used, with the aim of ascertaining the degree of relationship between the variables of interest, examined pair-by-pair.
Twenty-seven patients fulfilled the inclusion criteria for this study. Their mean age was 46.96 years (ranging from 16 to 73 years), and there were 14 males and 13 females. The trauma mechanism consisted of falling from a height in 23 cases, being run over in two cases, a motorcycle accident in one case and a heavy object falling onto the patient in one case. Regarding the vertebra that was fractured, 11 patients had a fracture in L1, nine in L2 and seven in T12. All of the patients remained free from neurological lesions during the hospital stay (Table 3).
Table 3.
Distribution of the patients hospitalized between 1991 and 2010.
| Patient | Sex | Age | Mechanism | Level | Kyphosis | VAS | Denis pain | Denis work | SF 36 |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 50 | Run over | L1 | 19 | 4 | 3 | 2 | 104 |
| 2 | M | 42 | Fall | L1 | 27 | 6 | 3 | 3 | 74.35 |
| 3 | M | 58 | Fall | T12 | 30 | 1 | 2 | 1 | 137.4 |
| 4 | F | 45 | Run over | L1 | 28 | 7 | 3 | 4 | 95.75 |
| 5 | F | 60 | Direct trauma | L2 | 19 | 0 | 1 | 2 | 139.4 |
| 6 | M | 36 | Fall | L2 | 40 | 3 | 1 | 1 | 128.35 |
| 7 | M | 45 | Fall | T12 | 1 | 2 | 2 | 3 | 119.25 |
| 8 | M | 26 | Fall | L1 | 19 | 8 | 3 | 3 | 75.75 |
| 9 | F | 67 | Fall | T12 | 14 | 5 | 2 | 2 | 112 |
| 10 | F | 61 | Fall | L1 | 16 | 2 | 2 | 1 | 106.25 |
| 11 | M | 59 | Fall | L2 | 10 | 10 | 5 | 5 | 61 |
| 12 | F | 60 | Fall | L1 | 28 | 7 | 3 | 3 | 92.25 |
| 13 | M | 57 | Fall | T12 | 18 | 10 | 3 | 4 | 86.6 |
| 14 | F | 25 | Fall | L2 | 24 | 5 | 2 | 3 | 82.5 |
| 15 | F | 16 | Fall | L2 | 0 | 5 | 3 | 3 | 106.1 |
| 16 | F | 36 | Fall | T12 | 14 | 2 | 1 | 2 | 109.5 |
| 17 | M | 46 | Fall | T12 | 30 | 8 | 3 | 3 | 76.25 |
| 18 | F | 50 | Fall | T12 | 8 | 8 | 3 | 2 | 89.75 |
| 19 | F | 42 | Fall | L2 | 13 | 8 | 3 | 5 | 102.35 |
| 20 | F | 41 | Fall | L1 | 23 | 0 | 2 | 1 | 104 |
| 21 | M | 47 | Motorcycle accident | L1 | 36 | 0 | 1 | 3 | 119.25 |
| 22 | F | 33 | Fall | L2 | 14 | 8 | 2 | 2 | 83 |
| 23 | M | 48 | Fall | L1 | 10 | 1 | 2 | 1 | 117.8 |
| 24 | M | 41 | Fall | L2 | 22 | 5 | 2 | 3 | 115.1 |
| 25 | M | 73 | Fall | L2 | 10 | 2 | 1 | 1 | 137 |
| 26 | M | 52 | Fall | L1 | 48 | 2 | 2 | 1 | 133.8 |
| 27 | M | 52 | Fall | L1 | 19 | 5 | 2 | 1 | 129.25 |
Legend: age in years and kyphosis in degrees. F = female; M = male; VAS = visual analogue pain scale.
RESULTS
In the radiographic evaluation, the mean kyphosis encountered was 20°, with a range from 0 to 48°. Regarding pain, five patients were free from pain; 11 presented minimal pain without using medication; 10, moderate pain with occasional use of medication; and one, severe pain with chronic use of medication. Regarding work, eight patients had returned to doing heavy work; six had returned to sedentary work without weight restrictions; nine had returned to work but had changed their activity; two had returned to work part-time; and two remained incapable of working.
No correlations were observed between the residual kyphosis and any of the following: total SF-36 score (p = 0.647), SF-36 domain scores, visual analogue pain score (p = 0.366), Denis pain scale (p = 0.263) or Denis work scale (p = 0.335) (Tables 4 and 5).
Table 4.
Correlation between the SF-36 domains and kyphosis.
| SF-36 domains / kyphosis | Correlation coefficient | P |
|---|---|---|
| Functional capacity | 0.261 | 0.189 |
| Physical aspects | 0.195 | 0.330 |
| Pain | −0.008 | 0.970 |
| General state of health | −0.111 | 0.580 |
| Vitality | 0.095 | 0.636 |
| Social aspects | 0.156 | 0.436 |
| Emotional aspects | 0.357 | 0.067 |
| Mental health | 0.041 | 0.840 |
Table 5.
Correlation between the variables and kyphosis.
| Variable/kyphosis | Correlation coefficient | P |
|---|---|---|
| Pain | −0.008 | 0.970 |
| VAS | −0.181 | 0.366 |
| Denis pain scale | −0.223 | 0.263 |
| Denis work scale | −0.193 | 0.335 |
| SF-36 | 0.92 | 0.647 |
Legend: VAS = visual analogue pain scale.
DISCUSSION
The treatment for thoracolumbar burst fractures is a matter that is still under discussion. Observational studies on neurologically intact patients have not shown any differences in the long-term functional results among patients with this type of lesion, independent of whether they underwent surgical treatment or not2, 3, 10. However, the surgical method is generally proposed for patients whose fractures have led to loss of 50% of the height of the vertebral body and kyphosis greater than 30°, because of inadequate functional results. The authors who have advocated this type of treatment have used shorter hospital stay and early mobility as arguments in its favor11, 13, 17, 18.
In the literature, there are still few studies showing any specific relationship between functional results and surgical treatment for thoracolumbar burst fractures. Andress et al(19) conducted a study on a retrospective series of 50 patients with burst factures who underwent surgical treatment, and were unable to prove any correlation between the radiographic findings and the patients’ long-term functional results, in relation to pain. In another retrospective study conducted by Lakshmanan et al(14), in which they sought to correlate recurrence of kyphosis in 26 patients who had undergone surgical treatment, with the functional implications, no statistical correlation could be found. The results from those studies were similar to ours.
To evaluate the quality of life among the patients in our study, the SF-36 and visual analogue scale were used. These instruments have been validated for use in our setting and are of great value for analyzing the results from patient-centered treatment that is not just based on radiographic criteria. In the same way as in our findings, the other case series surveyed also showed a lack of evident correlation between kyphosis and spinal symptoms or function following surgical treatment.
The limitations observed in this study were its retrospective nature, with the inherent difficulty in locating the patients for inclusion in the study (lack of correct addresses and telephone numbers in the databases), the relatively small number of patients and the lack of comparison with patients undergoing conservative treatment. Other studies with different methodologies and statistical designs could be conducted to increase the statistical significance of the results obtained. Nonetheless, the scarcity of information on this subject provided justification for the present study.
CONCLUSION
No evident correlations were found between residual kyphosis, pain and functional results, as shown on the SF-36 and Denis scales after surgical treatment on patients with thoracolumbar burst fractures of subtype Denis-A3 without neurological lesions.
ACKNOWLEDGEMENTS
We thank the Publications Support Unit of the School of Medical Sciences, Santa Casa de São Paulo (NAP-SC) for technical and scientific support towards publication of this manuscript.
Footnotes
Work performed by the Spine Group of the “Fernandinho Simonsen” Wing of the Department of Orthopedics and Traumatology, School of Medical Sciences, Santa Casa de Misericórdia de São Paulo (SCMSP).
REFERENCES
- 1.Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 1983;8(8):817–831. doi: 10.1097/00007632-198311000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Kraemer WJ, Schemitsch EH, Lever J, McBroom RJ, McKee MD, Waddell JP. Functional outcome of thoracolumbar burst fractures without neurological deficit. J Orthop Trauma. 1996;10(8):541–544. doi: 10.1097/00005131-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Thomas KC, Bailey CS, Dvorak MF, Kwon B, Fisher C. Comparison of operative and nonoperative treatment for thoracolumbar burst fractures in patients without neurological deficit: a systematic review. J Neurosurg Spine. 2006;4(5):351–358. doi: 10.3171/spi.2006.4.5.351. [DOI] [PubMed] [Google Scholar]
- 4.Knight RQ, Stornelli DP, Chan DP, Devanny JR, Jackson KV. Comparison of operative versus nonoperative treatment of lumbar burst fractures. Clin Orthop Relat Res. 1993;(293):112–121. [PubMed] [Google Scholar]
- 5.Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3(4):184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 6.Delfino HLA. Classificação das fraturas da coluna torácica e lombar. Coluna. 2002;1(1):41–48. [Google Scholar]
- 7.Jones RW. Manipulative Reduction of Crush Fractures of the Spine. Br Med J. 1931;1(3659):300–302. doi: 10.1136/bmj.1.3659.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am. 1970;52(8):1534–1551. [PubMed] [Google Scholar]
- 9.Domenicucci M, Preite R, Ramieri A, Ciappetta P, Delfini R, Romanini L. Thoracolumbar fractures without neurosurgical involvement: surgical or conservative treatment? J Neurosurg Sci. 1996;40(1):1–10. [PubMed] [Google Scholar]
- 10.Avanzi O, Chih LY, Meves R, Caffaro MFS, Bueno RS, Freitas MMF. Fratura toracolombar tipo explosão: resultados do tratamento conservador. Rev Bras Ortop. 2006;41(4):109–115. [Google Scholar]
- 11.Tezer M, Erturer RE, Ozturk C, Ozturk I, Kuzgun U. Conservative treatment of fractures of the thoracolumbar spine. Int Orthop. 2005;29(2):78–82. doi: 10.1007/s00264-004-0619-1. Epub 2005 Feb 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shen WJ, Liu TJ, Shen YS. Nonoperative treatment versus posterior fixation for thoracolumbar junction burst fractures without neurologic deficit. Spine (Phila Pa 1976) 2001;26(9):1038–1045. doi: 10.1097/00007632-200105010-00010. [DOI] [PubMed] [Google Scholar]
- 13.McEvoy RD, Bradford DS. The management of burst fractures of the thoracic and lumbar spine. Experience in 53 patients. Spine (Phila Pa 1976) 1985;10(7):631–637. doi: 10.1097/00007632-198509000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Lakshmanan P, Jones A, Mehta J, Ahuja S, Davies PR, Howes JP. Recurrence of kyphosis and its functional implications after surgical stabilization of dorso-lumbar unstable burst fractures. Spine J. 2009;9(12):1003–1009. doi: 10.1016/j.spinee.2009.08.457. Epub 2009 Oct 9. [DOI] [PubMed] [Google Scholar]
- 15.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 16.Harrison DE, Cailliet R, Harrison DD, Janik TJ, Holland B. Reliability of centroid, Cobb, and Harrison posterior tangent methods: which to choose for analysis of thoracic kyphosis. Spine (Phila Pa 1976) 2001;26(11):E227–E234. doi: 10.1097/00007632-200106010-00002. [DOI] [PubMed] [Google Scholar]
- 17.Gertzbein SD. Scoliosis Research Society. Multicenter spine fracture study. Spine (Phila Pa 1976) 1992;17(5):528–540. doi: 10.1097/00007632-199205000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Sanderson PL, Fraser RD, Hall DJ, Cain CM, Osti OL, Potter GR. Short segment fixation of thoracolumbar burst fractures without fusion. Eur Spine J. 1999;8(6):495–500. doi: 10.1007/s005860050212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andress HJ, Braun H, Helmberger T, Schürmann M, Hertlein H, Hartl WH. Long-term results after posterior fixation of thoraco-lumbar burst fractures. Injury. 2002;33(4):357–365. doi: 10.1016/s0020-1383(02)00030-x. [DOI] [PubMed] [Google Scholar]


