INTRODUCTION
Rotator cuff injuries are common in all athletic. Of all rotator cuff injuries, the supraspinatus tendon involves mostly. Severe supraspinatus tendon injury may affect the patient's quality of life. However, supraspinatus tendon injury can be relatively asymptomatic in some cases and may require sonographic examination for diagnosis.[1,2] With continued improvement in shoulder arthroscopy, surgical treatment for supraspinatus tendon injury has become more effective and less invasive.[3] Therefore, there has been increasing demand for the accurate morphologic and dynamic characterization of both the severity and location of supraspinatus tendon injury to guide management.[4]
METHODS
Research participants
The Institutional Review Board approved this study, and all subjects provided written informed consent. From May 2010 to December 2014, we prospectively enrolled 192 consecutive patients (75 men and 117 women, age range 22–79 years, mean age 53 ± 2 years) who were under the care of an orthopedic surgeon in the Department of Sports Medicine due to a history of shoulder pain and limited shoulder range of motion for 3–12 months. All patients underwent conventional shoulder ultrasonography 1–5 days before the arthroscopy.
Equipment
All ultrasound (US) examinations were performed with a Hitachi Preirus (Hitachi Medical Systems, Chiyoda-ku, Tokyo, Japan) scanner and multi-frequency linear-array transducer (5.0–13.0 MHz).
Patient position and scanning method
We scan the shoulder facing the front of the patient who is seated on a stool without armrests. We keep the probe vertical in orientation with respect to the surface of the humeral head and include the acromion and greater tuberosity in the field of view. We ask the patients to reach with affected arm behind their lower back as if reaching to a rear pant pocket on the opposite side of their body (keeping the upper arm close to the body, overextended, and the shoulder turned midway inward). This position (Crass position) places the supraspinatus in maximum inward rotation for long axis scan.
Statistical analysis
All statistical analyses were conducted using the software package SPSS (Version 19, SPSS Inc, Chicago, Illinois, USA). Relevant data were tested using Chi-square analysis with paired data, If n < 40 and t < 1, using the Fisher exact probability method. The test level is μ = 0.05 (P < 0.05 statistically significance).
RESULTS
Patient information analysis
Arthroscopic surgery confirmed 173 patients (56 men and 117 women) of supraspinatus tendon tear. The average age of the patients was 53 ± 2 years old (range of 22–79 years old). The majority of the patients were between 51 and 60 years old. The proportion of men and women was 1.0:2.1; the right shoulder injure happened more, the proportion of left and right was 1:2. For most of the patients, their shoulder pain has been ongoing for 3 months to 1 year.
Supraspinatus tendon injury sonographic features
Based on the degrees of the supraspinatus injury, US diagnosis is divided into three main types such as full-thickness tear (FTT), partial-thickness tear (PTT) [Figure 1], and chronic tear (CT). All patients with CT type of supraspinatus abnormality experience various levels of shoulder pain. The sonographic appearances include: (a) the supraspinatus tendon appears thickened and heterogeneous. Tendon thickness exceeds 8 mm without optimal tears. The effusion appears in at least one of the following areas: The bicep tendon sheath, the coracoid bursa, the subacromial bursa, and the postlabrum; and (b) the entire supraspinatus tendons are thinner (the maximal thickness is <4 mm) and no visible tears are present.
Figure 1.
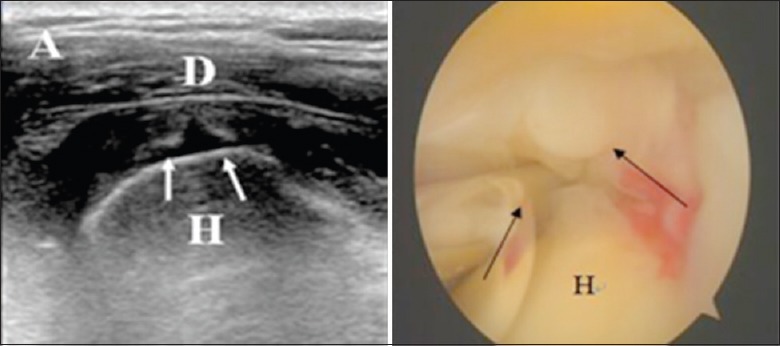
Articular-side partial-thickness tear sonographic image shows that anechoic fluid fills in the region of articular-sided tendon (white arrows, left image) while bursal-sided tendon is still relatively intact. This kind of injury is considered partial-thickness tear at the supraspinatus tendon articular-side. The result is confirmed with arthroscopic (black arrows, right image). H: Humeral head; D: Deltoid.
Size of partial-thickness supraspinatus tendon tear
Measurements of the tear should include size (anteroposterior dimension in short axis and transverse dimension in long axis) and depth (the distance between the PTT and the insertion point of the supraspinatus tendon on the greater tuberosity) of the tear. For measuring size of the tears, we first average two measurements in each axis (long and transverse). Mean tear thickness is then determined by averaging the measurements in two axes. For measuring the depth of tears, US probe must be switched to long axis view once the tubercle sulcus has been found on short-axis view.[4] In our study, 81.3% of the cases with the distance between the location of the tear and the frontal area of the supraspinatus and greater tuberosity insertion point were between 2.4 mm and 13.7 mm, with an average distance of 6.1 ± 2.1 mm.
Analysis of the sensitivity and specificity of ultrasonic inspection is shown in Table 1. The sensitivity is 93.6%, and the specificity is 89.5%. The difference in diagnosing PTT between US and magnetic resonance imaging (MRI) was statistically significant (P = 0.04). However, the difference between the two in the diagnosis of FTT and CT were not statistically significant (P > 0.05). One case of pigmented villonodular synovitis with FTT was interpreted as Prompt FTT. Two cases of greater tuberosity avulsion fracture were misdiagnosed as PTTs with calcified supraspinatus tendinitis. Another pitfall was incomplete evaluation of supraspinatus tendon and/or co-existing injuries in both tendons and muscles.
Table 1.
Correlation between ultrasonography and arthroscopy
| Arthroscopic result | No tear | CT (n) | PTT (n) | FTT (n) | Total (N) |
|---|---|---|---|---|---|
| No tear | 17 | 0 | 2 | 0 | 19 |
| CT | 0 | 45 | 3 | 0 | 48 |
| PTT | 6 | 1 | 70 | 1 | 78 |
| FTT | 0 | 0 | 0 | 47 | 47 |
| Total | 23 | 46 | 75 | 48 | 192 |
CT: Chronic tear; PTT: Partial-thickness tear; FTT: Full-thickness tear.
DISCUSSION
The data showed that ultrasonic diagnosis of supraspinatus tendon injury with high sensitivity and specificity, especially the ultrasonography, has certain advantages in the diagnosis of partial tear. This improvement in accuracy is due to the fact that US is much more flexible than MRI in terms of operating methods. US scan, unlike MRI, is a dynamic examination that enables the examiner to repeat and rescan the area of interest. US also offers the opportunity to perform dynamic studies in internal and external rotation with enhanced visualization of the tendons during motion. Tendon thinning usually results in impingement syndrome since normal thickness of the supraspinatus tendon ranges 4.5–7.9 mm.[5,6] In our patient group, all patients who were diagnosed with tendon thickening on ultrasonography suffered from impingement syndrome. Synovial hypertrophy may occur at the site of tendon injury. As a result, such growth may obscure the tears and provide an illusion of tendon thickening, which may lead to a false-positive interpretation. The use of dynamic graded compression can help distinguish intact tendon tissue from abnormal synovial or granulation tissue within the tendon defect.[7]
Special attention should be paid to sonographic pitfalls during the scanning and interpretation of supraspinatus tendon injuries. The most common pitfall relates to anisotropy when the tendon is not perpendicular to the sound beam as US beam is reflected away from the transducer. As a result, normal hyperechoic tendon may appear hypoechoic. This artifact is especially problematic when evaluating the supraspinatus tendon, as it is curved to its insertion following the contours of the adjacent humeral head. At the posterior aspect of the rotator cuff, it is common to see alternating hypoechoic bands at the junction of the supraspinatus and infraspinatus tendons from anisotropy. When performing shoulder sonography, the probe must be adjusted to ensure vertical positioning of its long axis to minimize anisotropic artifact. The visualization of the long head of the biceps tendon in the rotator interval is critical to ensure that the most anterior aspect of the supraspinatus tendon is evaluated. The long axis view of the supraspinatus is an important view in that the anatomic surfaces of the supraspinatus tendon (intra-articular, bursal, and greater tuberosity) are identified, allowing accurate characterization of a tear. We use cine loop to record sweeping the greater tuberosity 2–3 cm (anterior to posterior) with transducer to ensure complete evaluation. We also carefully scan anterior aspect of supraspinatus tears near the rotator interval. When imaging the supraspinatus tendon, it is ideal to begin just anterior to the supraspinatus over the rotator interval and the long head of the biceps brachii tendon. This ensures that the most anterior aspect of the supraspinatus has been included. In addition, once the long axis of the biceps tendon is in plane, this establishes the long axis plane of the supraspinatus so that the transducer is then simply moved posterior over the tuberosity in the same imaging plane to complete evaluation of the supraspinatus tendon. The transducer is turned to transverse view to begin with the transducer over the articular surface of the humeral head; the smooth, round echogenic surface of the humeral head and thin layer of hypoechoic hyaline cartilage with a uniform thickness of the overlying rotator cuff are seen, which indicate that the transducer is orientated correctly in the short axis of the supraspinatus.[8]
In conclusion, ultrasonography has high sensitivity and specificity in the assessment of location and severity of the supraspinatus tendon injury. Such information plays an important role in designing precise and individualized treatment plan.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Li-Min Chen
REFERENCES
- 1.Keener JD, Steger-May K, Stobbs G, Yamaguchi K. Asymptomatic rotator cuff tears: Patient demographics and baseline shoulder function. J Shoulder Elbow Surg. 2010;19:1191–8. doi: 10.1016/j.jse.2010.07.017. doi: 10.1016/j.jse.2010.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schibany N, Zehetgruber H, Kainberger F, Wurnig C, Ba-Ssalamah A, Herneth AM, et al. Rotator cuff tears in asymptomatic individuals: A clinical and ultrasonographic screening study. Eur J Radiol. 2004;51:263–8. doi: 10.1016/S0720-048X(03)00159-1. doi: 10.1016/S0720-048X(03)00159-1. [DOI] [PubMed] [Google Scholar]
- 3.Burkhart SS, Cole BJ. Bridging self-reinforcing double-row rotator cuff repair: We really are doing better. Arthroscopy. 2010;26:677–80. doi: 10.1016/j.arthro.2010.02.007. doi: 10.1016/j.arthro.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Yablon CM, Bedi A, Morag Y, Jacobson JA. Ultrasonography of the shoulder with arthroscopic correlation. Clin Sports Med. 2013;32:391–408. doi: 10.1016/j.csm.2013.03.001. doi: 10.1016/j.csm.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 5.Akturk M, Karaahmetoglu S, Kacar M, Muftuoglu O. Thickness of the supraspinatus and biceps tendons in diabetic patients. Diabetes Care. 2002;25:408. doi: 10.2337/diacare.25.2.408. doi: 10.2337/diacare.25.2.408. [DOI] [PubMed] [Google Scholar]
- 6.Leong HT, Tsui S, Ying M, Leung VY, Fu SN. Ultrasound measurements on acromio-humeral distance and supraspinatus tendon thickness: Test-retest reliability and correlations with shoulder rotational strengths. J Sci Med Sport. 2012;15:284–91. doi: 10.1016/j.jsams.2011.11.259. doi: 10.1016/j.jsams.2011.11.259. [DOI] [PubMed] [Google Scholar]
- 7.Moosmayer S, Heir S, Smith HJ. Sonography of the rotator cuff in painful shoulders performed without knowledge of clinical information: Results from 58 sonographic examinations with surgical correlation. J Clin Ultrasound. 2007;35:20–6. doi: 10.1002/jcu.20286. doi: 10.1002/jcu.20286. [DOI] [PubMed] [Google Scholar]
- 8.Jacobson JA. Shoulder US: Anatomy, technique, and scanning pitfalls. Radiology. 2011;260:6–16. doi: 10.1148/radiol.11101082. doi: 10.1148/radiol.11101082. [DOI] [PubMed] [Google Scholar]


