Abstract
Background:
Use of electronic medical record systems has increased in the recent years. Epic is one such system gaining popularity in the USA. Epic is a private company, which invented the electronic documentation system adopted in our hospital. In spite of many presumed advantages, its use is not critically analyzed. Some of the perceived advantages are increased efficiency and protection against litigation as a result of accurate documentation.
Materials and Methods:
In this study, retrospective data of 305 patients who underwent endoscopic retrograde cholangiopancreatography (wherein electronic charting was used - “Epic group”) were compared with 288 patients who underwent the same procedure with documentation saved on a paper chart (“paper group”). Time of various events involved in the procedure such as anesthesia start, endoscope insertion, endoscope removal, and transfer to the postanesthesia care unit were routinely documented. From this data, the various time durations were calculated.
Results:
Both “anesthesia start to scope insertion” times and “scope removal to transfer” times were significantly less in the Epic group compared to the paper group. Use of Epic system led to a saving of 4 min of procedure time per patient. However, the mean oxygen saturation was significantly less in the Epic group.
Conclusion:
In spite of perceived advantages of Epic documentation system, significant hurdles remain with its use. Although the system allows seamless flow of patients, failure to remove all artifacts can lead to errors and become a source of potential litigation hazard.
Keywords: Anesthesia documentation, electronic medical documentation, endoscopic retrograde cholangiopancreatography, Epic
Introduction
Epic (not an acronym) is a private company that has created a popular and relatively new electronic medical record (EMR) system. Amongst its many uses, the system allows documentation and online access of perioperative medical records from almost anywhere in the world. It also allows integration of data entered by different health care providers, facilitating seamless cross-specialty information access. The system replaced paper-based system at the Hospital of the University of Pennsylvania, Philadelphia, USA, in June 2013.
Materials and Methods
After obtaining Institutional Review Board approval, the perioperative EMRs of all patients who underwent endoscopic retrograde cholangiopancreatography (ERCP) between July 1, 2013 and June 30, 2014 were reviewed. To eliminate bias associated with learning in the initial phase of implementation, we excluded the first month data. ERCP is a complicated and sometimes prolonged endoscopic procedure similar in length and complexity to minor surgical procedures, normally performed general anesthesia or deep sedation. In our hospital, typically the patients are consented in the preoperative holding area. As soon as the endoscopist is available and the nurse anesthetist or the resident (who provide anesthesia services for these procedures under the supervision of an anesthesiologist) is ready, the patient is transported to the procedure room. The patient's EMR is opened on a computer in the procedure room. The identification details, history, examination, and investigation findings are reviewed. During the course of the anesthetic, the time of the following events are routinely documented; anesthesia start time (the time patient presenting into the procedure room), endoscope insertion time, endoscope removal time, and the time of patient transfer from the endoscopy room to the recovery area. Retrospectively, the following data were extracted from the patient's records.
Total anesthesia time (from the time patient presenting into the procedure room and care transferred to the postoperative care unit nurse).
Anesthesia start to scope in time (from the time patient presenting into the procedure room to the introduction of an endoscope).
Total scope time (from the introduction of the endoscope to its withdrawal).
Scope out to patient care transfer time (from the withdrawal of the endoscope to transfer of care to postoperative care unit nurse).
Minimum recorded oxygen saturation (minimum oxygen saturation recorded at any time during the endoscopy, irrespective of the duration).
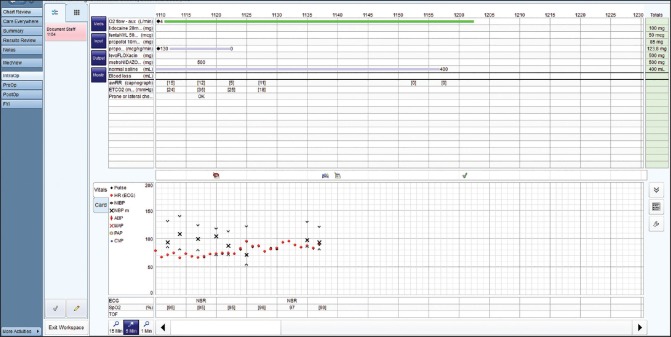
A comparison with the paper documentation system was made. There was no difference in the anesthesia methodology or the involved anesthesia providers between the two groups. An illustrative screen shot of the Epic documentation system is displayed in Figure 1.
Figure 1.
Screenshot of Epic anesthesia documentation page
Results
Results are presented in the Table 1 and Figure 2.
Table 1.
Comparison of various times related to the ERCP between Epic documentation and paper documentation
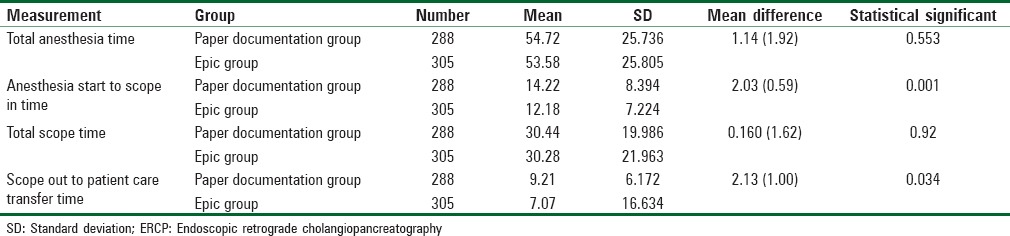
Figure 2.
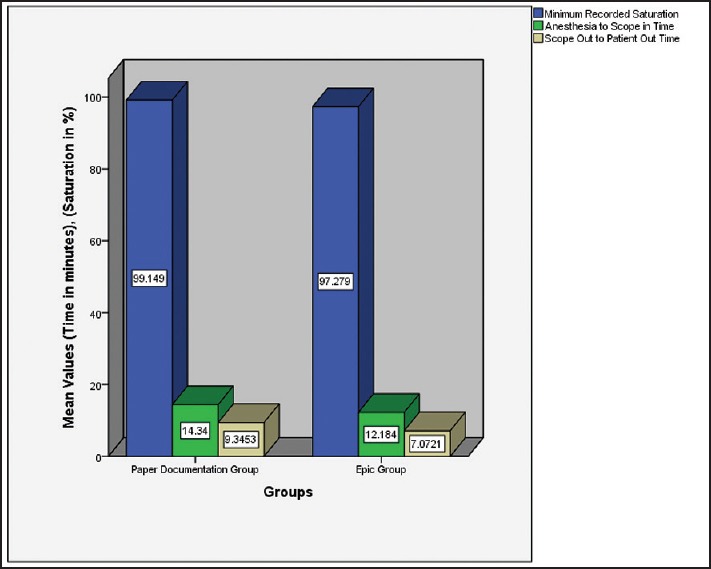
Comparison of the important times and desaturation between the Epic and paper groups
All the procedures were performed in the outpatient unit of the hospital of the University of Pennsylvania. The various times were typed in manually in an Excel spreadsheet for analysis. Data of all 305 patients who underwent ERCP between July 1, 2013 and June 30, 2014 (with documentation entered in Epic system) were compared with consecutive 288 patients who underwent ERCP during a 12 month period from July 3, 2009 to July 1, 2010. The mean times are presented in the table. As elaborated in Table 1, the mean anesthesia start to endoscope insertion time is significantly shorter in the group where Epic recording was used. On an average, 4 minutes were saved per ERCP procedure. Similarly, scope out to patient care transfer time is shorter in patients wherein Epic documentation system was used. The mean oxygen saturation was lower in patients wherein the Epic was used for documentation. The 4 minutes saved time per ERCP was significantly less than the patients where the paper record was used (Student's t-test).
Discussion
As a result of a federal mandate on the use of electronic medical charting systems, regardless of their pros and cons, paperless medical charting systems are here to stay. As a result, the authors are not making a case for reinstatement of paper medical records. However, before electronic medical systems are widely accepted, a critical analysis of their utility in certain areas of care, with an aim to address their with an aim to address their shortcomings is essential.
With health care spending accounting to more than 17.4% of gross domestic product in 2014 in USA, it is essential that every effort is made to increase the efficiency in the delivery of medical care.[1] A large component of billing in any medical/surgical procedure is due to the time spent in the procedure/operating room. The cost of staying in the procedure/operating room is estimated to be $62/min.[2,3] With an ever increasing need for accurate documentation (at least to defend ones practice), the Epic provides an efficient and cost-effective platform. As we have clearly demonstrated, use of Epic charting led to significant time saving, both before endoscope insertion and after its withdrawal. On an average, 4 min were saved per endoscopic procedure, saving about $250 in terms of procedure room cost. With an estimated 15 million colonoscopies performed each year in USA, this could amount to a saving of $3.75 billion/year from during procedures alone.[4] The Epic system, like most EMR documentation systems is designed to meet the demands of most surgical procedures and increase the efficiency. The touch screen options (in our hospital) might have increased the efficiency. The cost savings are likely to be restricted to areas of rapid turnover like endoscopy. In major surgeries where the surgical time is a large percentage of the total time, these advantages might be of less relevance.
With the federal government initiative to link the pay of the physicians with there, increasing efficiency without compromising patient safety has taken a center stage. The value of anesthesia information management systems in this regard was recognized and discussed by other investigators.[5] With the affordable health care law firmly in place, the concept of fee-for-value reimbursement has gained more attention.[6,7,8] It is demonstrated that a model whereby the same group of anesthesiologists are utilized to provide services involving repetitive tasks like endoscopy anesthesia services saves costs.[9] However, all physicians are not equally efficient in providing skill based services. Providing endoscopy anesthesia services can be one such area. It is shown that paying physicians to reach a common predetermined target will do little to increase the performance. It will only incentivize the physicians with a higher baseline performance measure.[10] As a result, research into initiatives that enhance the global performance like the Epic EMR systems might be very relevant.
However, a drawback of the Epic system deals with the patient safety. In most major surgeries, the patient's airway is typically secured with either an endotracheal tube or a laryngeal mask airway. The documentation input (either retroactive or real-time) is done with the patient in a stable and safe condition. With continuous monitoring and a secure airway, the risks of desaturation are small. The situation during an upper endoscopy is entirely different. With the airway shared between the anesthesia provider and the gastroenterologist, continuous attention to the airway with necessary intervention is mandatory. The time available to document drugs administered, other interventions, and monitoring aspects is limited. The pressure to input these variables in real-time can be a distraction from the patient care. Anesthesia providers (rightly) will give priority to patient safety over any documentation. As a result, any outstanding documentation is carried out at the end of the procedure. While the patient waits for transfer to the postanesthesia care unit, the anesthesia provider is busy with “catching up” documentation. It is possible that many desaturations might be artifacts, and the providers did not have sufficient time to correct such errors leading to a false increase in the incidence of recorded hypoxemia. It is also conceivable that in a paper chart, the vital signs are likely to be entered based on the recollection of the trends than the actual numbers. In spite of this, the incidence and degree of desaturation in our practice is very low in comparison to much published work.[11,12,13,14] We have presented the results of a retrospective study analyzing the incidence of hypoxemia in patients undergoing ERCP elsewhere.[15]
Failure to rectify all the artifacts (low oxygen saturation, cardiac arrhythmias, hypo/hypertension) is a potential source for litigation. Drug documentation errors can lead to similar problems. Given the rapid turnover in the endoscopy suite, it is not always possible to rectify every error in the electronic documentation chart, A case in point relates to the recent unfortunate outcome of the comedian Ms. Joan Rivers.[16,17] The anesthesiologist has admitted to an error whereby she had documented the drug propofol twice by mistake, although administered once. In the circumstances, she did not rectify the error, which can be a potentially contentious issue.
Conclusion
Inspite of the need to document many variables, complicated case closure and transfer to post procedure care mechanisms associated with the use of Epic, the system is likely to increase the efficiency of the endoscopy suite with significant savings. The charting system is likely to decrease the cost of health care by increasing the efficiency. The inevitable distraction from patient care arising from the need for ongoing accurate documentation (while the ERCP is in progress) might explain the lower oxygen saturations. Failure to manually rectify all the artifacts involved with autocapturing of the vital signs, can become a contentious issue in the event of adverse outcome and (or) litigation. The implementation of Epic anesthesia charting in endoscopy needs to be studied further before the hospitals decide to embrace it.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Medicare C for, Baltimore MS 7500 SB, USA M. National Health Accounts Historical. 2014. [Last accessed on 2015 Apr 19]. Available from: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical.html .
- 2.Lau HK, Chen TH, Liou CM, Chou MC, Hung WT. Retrospective analysis of surgery postponed or cancelled in the operating room. J Clin Anesth. 2010;22:237–40. doi: 10.1016/j.jclinane.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Macario A. What does one minute of operating room time cost? J Clin Anesth. 2010;22:233–6. doi: 10.1016/j.jclinane.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 4.Seeff LC, Richards TB, Shapiro JA, Nadel MR, Manninen DL, Given LS, et al. How many endoscopies are performed for colorectal cancer screening?. Results from CDC's survey of endoscopic capacity. Gastroenterology. 2004;127:1670–7. doi: 10.1053/j.gastro.2004.09.051. [DOI] [PubMed] [Google Scholar]
- 5.Egger Halbeis CB, Epstein RH. The value proposition of anesthesia information management systems. Anesthesiol Clin. 2008;26:665–79, vi. doi: 10.1016/j.anclin.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 6.Lemak CH, Nahra TA, Cohen GR, Erb ND, Paustian ML, Share D, et al. Michigan's fee-for-value physician incentive program reduces spending and improves quality in primary care. Health Aff (Millwood) 2015;34:645–52. doi: 10.1377/hlthaff.2014.0426. [DOI] [PubMed] [Google Scholar]
- 7.Pursel KJ, Jacobson M, Stephenson K. Paying for quality not quantity: A wisconsin health maintenance organization proposes an incentive model for reimbursement of chiropractic services. J Manipulative Physiol Ther. 2012;35:472–6. doi: 10.1016/j.jmpt.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 8.Rie M. ICU discharge bias reveals ethically troubling pay-for-performance benchmark metrics. Crit Care Med. 2014;42:1285–6. doi: 10.1097/CCM.0000000000000193. [DOI] [PubMed] [Google Scholar]
- 9.Goudra BG, Singh PM, Sinha AC. Anesthesia for ERCP: Impact of anesthesiologist's experience on outcome and cost. Anesthesiol Res Pract 2013. 2013:570518. doi: 10.1155/2013/570518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosenthal MB, Frank RG, Li Z, Epstein AM. Early experience with pay-for-performance: From concept to practice. JAMA. 2005;294:1788–93. doi: 10.1001/jama.294.14.1788. [DOI] [PubMed] [Google Scholar]
- 11.Coté GA, Hovis RM, Ansstas MA, Waldbaum L, Azar RR, Early DS, et al. Incidence of sedation-related complications with propofol use during advanced endoscopic procedures. Clin Gastroenterol Hepatol. 2010;8:137–42. doi: 10.1016/j.cgh.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 12.Barnett SR, Berzin T, Sanaka S, Pleskow D, Sawhney M, Chuttani R. Deep sedation without intubation for ERCP is appropriate in healthier, non-obese patients. Dig Dis Sci. 2013;58:3287–92. doi: 10.1007/s10620-013-2783-x. [DOI] [PubMed] [Google Scholar]
- 13.Qadeer MA, Rocio Lopez A, Dumot JA, Vargo JJ. Risk factors for hypoxemia during ambulatory gastrointestinal endoscopy in ASA I-II patients. Dig Dis Sci. 2009;54:1035–40. doi: 10.1007/s10620-008-0452-2. [DOI] [PubMed] [Google Scholar]
- 14.Qadeer MA, Vargo JJ, Khandwala F, Lopez R, Zuccaro G. Propofol versus traditional sedative agents for gastrointestinal endoscopy: A meta-analysis. Clin Gastroenterol Hepatol. 2005;3:1049–56. doi: 10.1016/s1542-3565(05)00742-1. [DOI] [PubMed] [Google Scholar]
- 15.Goudra BG, Singh PM, Sinha AC. Outpatient endoscopic retrograde cholangiopancreatography: Safety and efficacy of anesthetic management with a natural airway in 653 consecutive procedures. Saudi J Anaesth. 2013;7:259–65. doi: 10.4103/1658-354X.115334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rice S. Joan Rivers’ death highlights risks in outpatient surgery for seniors. Mod Healthc. 2014;44:11. [PubMed] [Google Scholar]
- 17.The upside — And downside — Of outpatient surgery: Joan Rivers’ death is a reminder that you should carefully look before you book. Consum Rep. 2015;80:22. [PubMed] [Google Scholar]