Abstract
Introduction and Aim:
Epidural analgesia is an effective technique for postoperative pain relief following thoracoabdominal surgeries. Lower limb motor weakness is a well-known complication of epidural analgesia with local anesthetics and delays postoperative rehabilitation. Our aim in conducting this observational study was to assess the frequency of lower limb motor weakness in patients receiving epidural analgesia following upper abdominal surgery and the factors associated with it.
Materials and Methods:
All adult patients, aged 20-70 years, who underwent upper abdominal surgery and received postoperative analgesia with an epidural infusion of bupivacaine with fentanyl, were included. Data were collected over 4 months from notes entered by acute pain service after each round. Data collected included level of epidural placement, drug solution and volume, degree of lower limb motor weakness and measures taken to relieve it. Bromage scale was used to assess motor weakness.
Results:
Data were collected on 123 patients. Bupivacaine 0.1% with fentanyl 2 μg/mL was used in 113 (92%) patients. Lower limb motor weakness developed in 45 patients (36.5%). The highest frequency was seen in patients with epidural at L2-L3 level. The common management steps were a change of patient's position or decrease in concentration of local anesthetic. These measures produced improvement in 39 (87%) patients whereas the local anesthetic was stopped temporarily in the remaining six patients.
Conclusion:
Lower limb motor weakness occurred in 36.5% patients. It was more common with a lumbar epidural. It was successfully managed in all patients. Lower thoracic epidurals are recommended for abdominal surgeries.
Keywords: Complications of epidural, epidural analgesia, lower limb motor weakness
Introduction
Continuous epidural infusion following major abdominal surgeries is a popular and effective technique for postoperative pain relief.[1] Epidural analgesia has shown to decrease the stress response to surgery and reduce the incidence of postoperative cardiovascular and respiratory complications, intestinal paralysis, and deep vein thrombosis and thus promote earlier mobilization and rehabilitation.[2,3] However, continuous epidural analgesia may be associated with side effects and requires close postoperative monitoring to ensure its effectiveness and safety.
Lower limb motor weakness is a well-known complication of epidural analgesia with local anesthetics. It leads to delays in the postoperative rehabilitation process and may necessitate temporary or permanent discontinuation of the epidural infusion causing pain, patient discomfort, and dissatisfaction. Königsrainer et al.[1] identified that postoperative lower limb motor weakness was the most frequent side effect managed by acute pain service (APS) team. Assessment of the prevalence of a problem and its associated factors is useful in making preventive strategies and maintaining standards of care.[1,4] We, therefore, conducted an observational study to assess the frequency of lower limb motor weakness in patients receiving continuous epidural infusion for postoperative analgesia following upper abdominal surgery at our hospital. We also collected data on the level of epidural insertion, concentration and volume of the local anesthetic used, degree of motor weakness and the measures taken to relieve the motor weakness.
Materials and Methods
Approval was obtained from the Anesthesia Research Committee and exemption was granted by the University Ethics Review Committee.
The standard practice for the conduct of epidural analgesia for major abdominal surgeries at the authors’ hospital involves identification of the epidural space with the patient in the sitting position before the induction of general anesthesia. A mid-line approach is used with the loss of resistance to air or saline. Depending on individual practice, a lumbar or lower thoracic interspace is used for epidural catheter placement for abdominal surgeries. The catheter is fixed at the insertion site with “lock it plus” catheter securing device (Smiths Medical ASC, Inc. Keene NH, USA). The remaining catheter is taped along the left side of patient's back up to the shoulder. A test dose of 3 mL of 2% lignocaine is routinely given after insertion. Bupivacaine 0.25% is used for loading dose in a volume of 12-15 mL, followed after 60-90 min by a continuous epidural infusion of bupivacaine 0.125%, 0.1% or 0.0625% with fentanyl 2 μg/mL, depending on individual practice. The preferred concentration of bupivacaine at the authors’ department is 0.1%. The infusion is continued for at least 48 h postoperatively. Paracetamol 1 g.6/h is usually prescribed as co-analgesic and intravenous tramadol 50 mg is prescribed on as required basis for rescue analgesia.
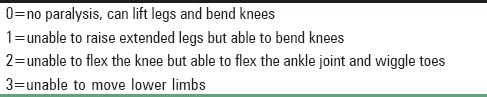
The APS at the authors’ hospital is responsible for following up all patients receiving continuous epidural infusions on the various surgical units of the hospital. APS conducts round twice daily, or more often if required to assess and manage pain and any side effects, if present. The anesthesiologist who inserts the epidural fills an epidural form containing information about patient demographics, the level of epidural placement, length of catheter inserted, epidural drugs administered intraoperatively and a prescription for epidural infusion to be administered postoperatively. The same form is used in the postoperative period by nurses for documentation of patient's hemodynamics, pain scores, sedation scores, motor weakness and other relevant information. The motor block is assessed by using modified Bromage scale of 0-3 [Table 1].
Table 1.
Modified Bromage scale used for assessing lower limb motor weakness
Data collection
All adult patients, aged 20-70 years, who underwent upper abdominal surgery and were receiving postoperative analgesia with epidural infusion of bupivacaine with fentanyl were included, while patients receive other analgesic modalities or epidural infusion following orthopedic procedures or for labor analgesia were excluded. Data were collected on the evening of surgery and then twice daily until the epidural infusion was discontinued. Data were collected from November 01, 2014 to February 28, 2015, by one of the authors from APS notes entered in the dedicated APS register after each round. A predesigned form was filled for data collection, documenting level of epidural placement, drug solution used, volume being infused, pain scores, degree of motor weakness, measures taken to relieve the motor weakness and the improvement in symptoms assessed 1 h after the institution of measures to manage motor weakness. A Bromage score of >0 was labeled as motor weakness. Patient's name or medical record number was not mentioned on the forms to ensure confidentiality.
All statistical analysis was performed using statistical packages for social science version 19 (SPSS Inc., Chicago, IL, USA). Frequencies and percentages were computed for categorical variables such as lower limb motor weakness, the level of epidural placement, etc., and also for the steps taken to manage the motor weakness. The relationship between level of epidural insertion and Bromage scale was evaluated by Chi-square test. P ≤ 0.05 was considered as significant.
Results
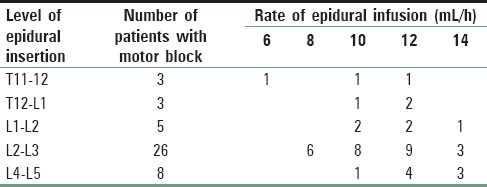
Data were collected on 123 patients during the 4 months of the study period. Patients’ demographic data and type and duration of surgery are provided in Table 2. Bupivacaine 0.1% with fentanyl 2 μg/mL was used in 113 (92%) patients, bupivacaine 0.0625% with fentanyl 2 μg/mL was used in 8 (6.5%) patients and bupivacaine 0.125% with fentanyl 2 μg/mL was used in only 1 (0.8%) patient, while the concentration was not mentioned in one patient. The rate of epidural infusion in the patients with lower limb motor block is shown in Table 3. There was a wide variation in the infusion rate, which depended upon the initial prescription by the primary anesthesiologists and adjustments made by APS after assessment of pain and side effects. Lower limb motor weakness developed at some point during the first 72 h postoperatively in 45 patients (36.5%). Forty-four of the 113 patients (38.9%) receiving bupivacaine 0.1% developed lower limb motor weakness, one of the eight patients receiving bupivacaine 0.0625% developed temporary unilateral motor block of Bromage grade 1, while the only patient receiving 0.125% did not develop motor weakness. The block was Bromage grade 1 in 40 patients and grade 2 in five patients while none of the patients had Bromage grade 3 motor block at any point in time. Pain scores were <3 on a numeric rating scale of 0-10 (0= no pain, 10= worst imaginable pain) at all times of assessment.
Table 2.
Demographic features, ASA physical status and type and duration of surgery performed
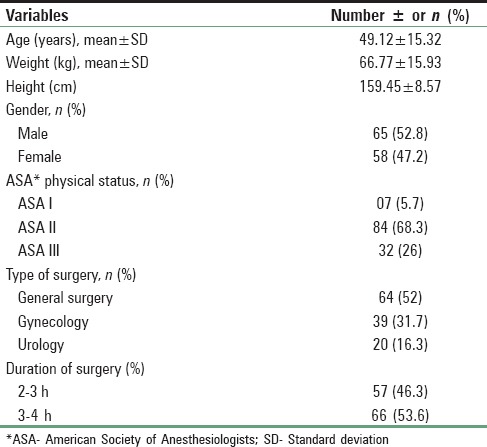
Table 3.
Rate of epidural infusion in patients with motor block according to level of epidural insertion (n = 45)
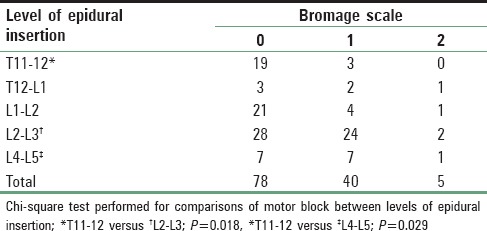
The highest frequency of lower limb weakness was observed on the evening of the day of surgery, that is, 40 of the 113 patients receiving bupivacaine 0.1% were found to have motor block 6 h after the surgical procedure. This number decreased to eight on the 1st postoperative day, while five new patients developed motor block on the 1st postoperative day. The degree of motor weakness in relation to the level of an epidural is provided in Table 4. Motor weakness was significantly higher with epidurals inserted at L2-L3 and L4-L5 levels compared to those inserted at T11-T12 [P < 0.05; Table 4]. Motor block was unilateral in 36 patients (75%). The common step taken for unilateral weakness was change of patient's position with the blocked side up, while for bilateral weakness, a lower concentration of local anesthetic (bupivacaine 0.0625%) with fentanyl 2 μg/mL was administered at the same infusion rate. The patients were revisited by an APS member 1 h after the institution of measures to manage motor weakness to ensure regression of the motor block. Change in patient's position or decreasing local anesthetic concentration produced improvement in 39 (87%) of the 45 patients, including the patient receiving 0.0625% bupivacaine infusion, while local anesthetic was stopped temporarily and restarted with lower concentration after resolution of block in six patients. Two of these six patients required administration of tramadol 50 mg for breakthrough pain during the temporary discontinuation of epidural infusion while the other patients remained pain-free.
Table 4.
Lower limb motor weakness (Bromage scale score) in relation to level of epidural insertion
Discussion
Lower limb motor weakness developed in 45 of the 123 patients (36.5%) included in the study at some point during the first 3 postoperative days, the frequency being higher in epidurals inserted at lumbar compared to lower thoracic levels. The motor weakness resolved in all patients after management was provided by APS. Early mobilization and rapid rehabilitation are important requirements for improving postoperative outcome and effective pain relief after a major surgery without side effects, or complications is a prerequisite to both.[4] Continuous epidural infusion is a popular and effective analgesic strategy for abdominal, thoracic and major lower limb orthopedic surgery.[1,4] Regular monitoring for efficacy of analgesia and any epidural related side effects is essential for patients’ safety and well-being. Lower limb motor weakness caused by epidural infusion of local anesthetic can significantly delay mobilization and rehabilitation process. Thus, monitoring for lower limb motor weakness and its prompt management in patients receiving a continuous epidural infusion of local anesthetics is an important responsibility of APS teams.
We used modified Bromage scale to monitor lower limb motor weakness, which is the recommended tool for measurement of lower limb motor weakness during epidural analgesia.[5] An increasing motor block usually indicates administration of an excessive dose of local anesthetic. However, it can be an early indication of more serious complications, including epidural hematoma or abscess, or rarely, it may be due to dural penetration of the catheter.[4] Even in the absence of serious complications, presence of motor weakness impedes the rehabilitation process as ambulation is delayed even with motor weakness of Bromage grade 1.[6] Furthermore, the motor blockade in the postoperative period may lead to the development of pressure lesions on heels and deep vein thrombosis.[7,8] Therefore, protocols must be formulated by every APS team for assessment and management of lower limb motor block in all patients receiving an epidural infusion for postoperative analgesia.[4]
Management of lower limb motor weakness caused by epidural infusion of local anesthetic usually involves reduction of rate of infusion, decreasing the concentration of local anesthetic and making the patient lie on the side with the affected side up. If this does not improve the block within 1 h and the weakness is unilateral, slight withdrawal of the epidural catheter may be considered.[4] If the block is intense, the local anesthetic infusion should be stopped. The motor block must resolve rapidly after decreasing the concentration of local anesthetic or stopping the epidural local anesthetic infusion. If intense block continues 2 h after stopping the infusion, thorough neurological examination and urgent magnetic resonance imaging scan should be done to rule out an epidural hematoma.[4] An APS team member at our hospital re-assesses the patients with motor block 1 h after decreasing the concentration of local anesthetic or stopping the epidural local anesthetic infusion to ensure that improvement has occurred. Adequate analgesia is also ensured if the epidural infusion is temporarily discontinued.
In our patients, lower limb motor weakness developed in 45 patients (36.5%) receiving an epidural infusion during the study period. This frequency is much higher than that found by Königsrainer et al., who found an overall incidence of lower limb motor weakness in 14.7% of the patients.[1] The highest frequency of motor weakness in our study was seen in the first 6 h after surgery, the frequency decreasing markedly on subsequent days, decreasing to 10.5% on the 1st postoperative day. The most probable cause of the high frequency seen in the initial postoperative period could be the 12-15 mL of 0.25% bupivacaine administered to all patients as epidural loading dose in the operating room followed after 60-90 min by a continuous epidural infusion of lower concentrations of bupivacaine, mostly 0.1%, with fentanyl 2 μg/mL. There is a possibility that the motor block caused by the higher concentration of 0.25% bupivacaine had not fully resolved in these patients at the time of the initial assessment. Merson also observed that higher loading doses of bupivacaine increased the chance of postoperative motor block despite the subsequent administration of lower concentrations.[9] In our study, we could not establish the time interval for the development of motor block after epidural bolus or initiation of infusion because these were administered and started by the primary anesthesiologist during the surgery. In order to avoid this high frequency of motor weakness, it would be best to ensure in the recovery room that motor block due to the loading dose of local anesthetic has receded before initiating the continuous infusion of local anesthetic.
We found that patients with epidurals inserted at the lumbar region had a higher frequency of motor weakness compared to epidurals at lower thoracic levels. Königsrainer et al. also observed that incidence of postoperative motor weakness of the legs was seen in 52.4% of patients with epidurals placed in lumbar intervertebral space, compared to only 4.8% of patients with epidural catheters in thoracic intervertebral space.[1] After this finding, they recommended a change of practice to lower thoracic epidurals for abdominal surgeries (T8-T11). In a re-assessment, they found that there was a significant decrease in postoperative lower limb motor weakness after the change of practice, with the overall incidence decreasing from 14.7% to 5.7%. A larger proportion of epidurals being inserted in the lumbar interspaces in our patients could be another reason for the overall higher incidence of motor weakness found in our study compared to Königsrainer et al.'s findings.
Use of lower concentrations of local anesthetic, increasing use of thoracic epidurals and more frequent follow-up in the early postoperative period might prove instrumental in decreasing the incidence of lower limb motor weakness, but these strategies need to be verified further through randomized controlled trials (RCTs). Research has shown that there is less motor blockade with ropivacaine compared to an equianalgesic dose of bupivacaine.[9] However, Buggy et al. found a high incidence of motor block with patient-controlled epidural analgesia using ropivacaine 0.1% in patients who underwent caesarean section under spinal bupivacaine. They concluded that the reported motor-sparing property of ropivacaine might be unreliable.[6] We continue to use bupivacaine in our patients due to the unavailability of ropivacaine in our country. In this situation, our best hope is to use the lowest concentration of bupivacaine that would achieve effective analgesia while avoiding lower limb motor weakness after conducting well-designed, high-powered research to ascertain this concentration.
This study was part of an endeavor to improve the quality of epidural analgesia at our hospital. We recommend that there should be more frequent follow-up in the early postoperative period to identify lower limb motor weakness and steps should be taken promptly to avoid its progress, as it is a hindrance to timely initiation of rehabilitation processes. In light of our results and literature review, we further recommend the insertion of epidurals at lower thoracic levels and avoid lumbar epidurals for major abdominal surgery. An audit must be conducted to assess any decrease in incidence of motor weakness at least 1-year after the change in practice.
A limitation of our study is that being an observational study, the epidural technique, and local anesthetic concentration was not standardized in all patients. Another limitation is that we were not able to assess the time of development of motor block after administration of bolus or infusion of local anesthetic because they were initiated by primary anesthesiologists during surgery before the patient was handed over to the APS team. RCTs comparing various concentrations of local anesthetics, different rates of infusion and different local anesthetic agents with standardized techniques are recommended to determine the most suitable drug and the best concentration in terms of satisfactory pain relief without lower limb motor weakness.
Conclusion
Lower limb motor weakness occurred in 45 patients (36.5%) patients receiving the epidural infusion, the frequency being highest on the evening of surgery. Motor weakness was more common with a lumbar epidural. It was successfully managed in all patients by changing patient's position, using a lower concentration of local anesthetic and temporarily stopping the infusion in patients who did not respond to the first two management steps.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Ms. Riffat Aamir for her help during data collection.
References
- 1.Königsrainer I, Bredanger S, Drewel-Frohnmeyer R, Vonthein R, Krueger WA, Königsrainer A, et al. Audit of motor weakness and premature catheter dislodgement after epidural analgesia in major abdominal surgery. Anesthesia. 2009;64:27–31. doi: 10.1111/j.1365-2044.2008.05655.x. [DOI] [PubMed] [Google Scholar]
- 2.Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, et al. Reduction of postoperative mortality and morbidity with epidural or spinal Anesthesia: Results from overview of randomised trials. BMJ. 2000;321:1493. doi: 10.1136/bmj.321.7275.1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beattie WS, Badner NH, Choi P. Epidural analgesia reduces postoperative myocardial infarction: A meta-analysis. Anesth Analg. 2001;93:853–8. doi: 10.1097/00000539-200110000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Faculty of Pain Medicine of Royal College of Anesthetists. Best Practice in Management of Epidural Analgesia in the Hospital Setting; November. 2010. [Last accessed on 2015 Apr 22]. Available from: http://www.aagbi.org/sites/default/files/epidural_analgesia_2011.pdf .
- 5.London: Royal College of Anesthetists; 2009. [Last accessed on 2015 Apr 22]. Description of the Bromage Scale. The 3rd National Audit Project of the Royal College of Anesthetists. Major Complications of Central Neuroaxial Block in the United Kingdom; p. 142. Available from: http://www.rcoa.ac.uk/indexasp?PageID=717 . [Google Scholar]
- 6.Buggy DJ, Hall NA, Shah J, Brown J, Williams J. Motor block during patient-controlled epidural analgesia with ropivacaine or ropivacaine/fentanyl after intrathecal bupivacaine for caesarean section. Br J Anesth. 2000;85:468–70. doi: 10.1093/bja/85.3.468. [DOI] [PubMed] [Google Scholar]
- 7.Smet IG, Vercauteren MP, De Jongh RF, Vundelinckx GJ, Heylen RJ. Pressure sores as a complication of patient-controlled epidural analgesia after cesarean delivery. Case report. Reg Anesth. 1996;21:338–41. [PubMed] [Google Scholar]
- 8.Karnawat R, Chhabra S, Mohammed S, Paliwal B. Comparison of effect of epidural bupivacaine, epidural bupivacaine plus fentanyl and epidural bupivacaine plus clonidine on postoperative analgesia after hip surgery. J Anesth Clin Res. 2013;4:373. doi: 10.4172/2155-6148.1000373. [Google Scholar]
- 9.Merson N. A comparison of motor block between ropivacaine and bupivacaine for continuous labor epidural analgesia. AANA J. 2001;69:54–8. [PubMed] [Google Scholar]


