Abstract
Background:
The Serratus anterior muscle plane (SAP) block has recently been described for the purpose of perioperative pain management following cases of trauma and breast surgery. It might prove a safer alternative to the other regional thoracic paravertebral and central neuraxial blockade techniques. There are no descriptive cadaveric studies in the pre-existing literature to delineate the anatomical plane for this novel technique. The main objectives for our study were to examine the location of the Serratus anterior muscle belly, assess the efficacy of achieving adequate delineation of the muscle plane utilising ultrasound imaging with agitated water as the contrast agent, and finally, to observe the extent of the cepahlo-caudal spread of the injectate in the SAP.
Materials and Methods:
Seven cadavers were studied. 20 mls of saline was injected into posterior axillary line (PAL) at the level of the 4-5th rib under ultrasound guidance. This was followed by injection of 10 mls of water with air (8 mls water and 2 mls of air). The presence of hyperechoic air bubbles in the fluid distended SAP (hypoechoic) area demonstrated the spread of water and air.
Results:
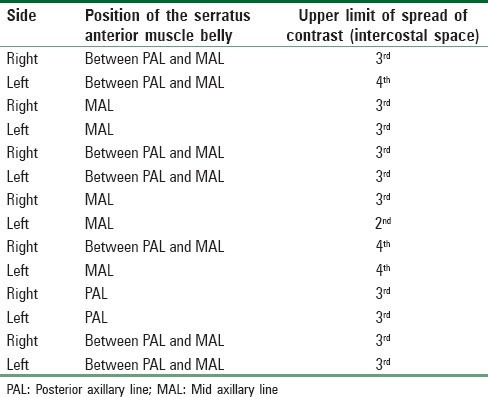
In 36% of cadavers, fully formed Serratus Anterior muscle belly was identified at the midaxillary line (MAL), 14% in PAL, and remaining 50% between PAL and MAL. The lower most limit of air-water spread was identified at the subcostal margin. Cephalad spread of contrast was noted in 2nd intercostal space ICS (7%), 3rd ICS (71%), and 4th ICS (22%).
Conclusion:
This study describes that the serratus anterior muscle is well-formed near the PAL and the injectate spread can be determined with the help of agitated water contrast on ultrasound. Furthermore, there was variability in the cephalad spread of the injectate.
Keywords: Cadaver, serratus anterior plane, ultrasound
Introduction
Cadaver based anatomic studies assessing the spread of injectate involve either injection of colored dyes and dissection or radiologic contrast medium.[1,2,3] To delineate the spread of injectate, a transfer to the radiology suite for computerized axial tomography or magnetic resonance imaging (MRI) is needed. As the cadaver is damaged while dissecting, it cannot be used subsequently for other studies or training related purposes. The search for an entirely non-invasive and inexpensive method of assessing the spread of injectate continues.
Ultrasound is a non-invasive, highly portable, reliable, and in-expensive method of assessment which could circumvent the disadvantages of both the dissection and radiological methods. The spread of injectate can be identified with ultrasound as a hypoechoic layer of fluid in fascial planes or around the areas of interest such as nerves. Micro-bubbles created either by agitated water or saline and air act as an excellent contrast medium for an ultrasound, which has been used for a number of years in cardiology for outlining cardiac chambers and identification of shunts.[4]
We hypothesized that agitated air-water can serve as a contrast media and can be used to identify the spread of injectate in ultrasound guided fascial plane blocks. Serratus anterior plane (SAP) block has recently been described and suggested as an alternative to paravertebral block for breast surgery and trauma.[5] Until now, there has been only one radiological study assessing the spread in the serratus interfascial plane.[6] As breast surgeries are fairly common and it falls into the area of clinical expertise of two of the authors, we aimed to evaluate the ultrasound spread of injectate in the SAP with the intention to follow-up with the clinical trials.
Materials and Methods
Ethical approval for this study (project reference hc27-61682) was provided by the Ethical Committee University of Leicester, UK on April 10, 2014.
Seven embalmed cadavers, fixed with Vickers embalming fluid number 4 were utilized in this study. All procedures were performed by a senior anesthetic consultant experienced in ultrasound guided SAP blocks. Of the seven cadavers studied, there were four males and three females, and were aged between 50 and 91 years. Fourteen SAP were identified in total, by using the both sides of the cadaver. The sequence of the study was as follows. First, an ultrasound scout scan in two planes was performed to identify the serratus anterior muscle, to define the SAP and to rule out preexisting air artifacts. Second, agitated air and water was injected in the SAP. Finally, the post injections scan to assess the cranio-caudal spread of ultrasound contrast were performed in the SAP.
The ultrasound scans were performed with a GE Medical Systems Ultrasound Logiq e machine (GE Healthcare, Chalfont St. Giles, Bucks, UK) with a 9-13 MHz 12 L-RS linear array transducer. Cadavers were placed in the prone position. During the scout scanning the correct vertebral levels were identified lateral to the spine in a para-sagittal plane by counting down the ribs. The scanning was performed in the transverse plane starting at anterior axillary line at the level of 4-5th inter-costal space and then moving posteriorly toward the mid and posterior axillary lines (PAL) to identify the belly of serratus anterior muscle (identified as the maximum thickness of the serratus muscle in that rib space) and the latissimus dorsi overlying it [Figure 1a and b]. 20 mls of water was injected through 21 gauge 100 mm Stimuplex® (B. Braun, Melsungen, Germany) needle using an in-plane approach [Figure 1c] into the SAP under the belly of the serratus muscle. Subsequently, 10 mls of agitated air-water contrast (8 mls water and 2 mls of air) was injected through the same needle at the point of injection. Five minutes later, the post injection scan was repeated, as described above, to identify the spread of contrast visible as hyperechoic areas due to the presence of air bubbles [Figure 1d] and to define the extent of the spread in a cranio-caudal direction with the cadaver in the prone position.
Figure 1.
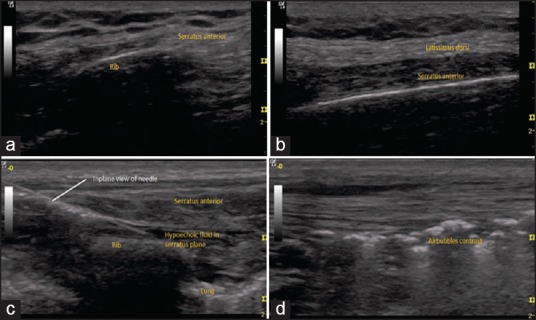
(a) Ultrasound image of incomplete serratus muscle belly in anterior axillary line (b) Ultrasound image of complete belly formation in posterior axillary line (c) Ultrasound image of in-plane view of needle and hypoechoic fluid in-plane (d) Ultrasound image of hyperechoic air bubbles in-plane
Result
The air-water contrast was identified in all cases in the serratus anterior muscle plane. A well-formed serratus anterior muscle belly was identified at the midaxillary line (MAL) in 36% of cadavers, PAL in 14% of cadavers, and between MAL and PAL in 50% of cadavers.
The caudal spread of contrast was observed at the subcostal margin in all the cadavers, but the cephalad spread was variable [Table 1]. In 7 % of cadavers the cephalad spread was seen up to 2nd intercostal space (ICS), 71% of cadavers up to 3rd ICS, and 21% of cadavers at 4th ICS.
Table 1.
Spread of agitated water contrast
Discussion
We were able to identify the contrast air bubbles in 100% of our cadavers on ultrasound imaging under the serratus anterior muscle. Use of agitated air-water serves as a good ultrasound contrast medium in embalmed cadavers for delineation of muscle planes. The technique has number of advantages such as portability of imaging equipment, low cost of contrast media, dynamic and can be repeated as often, ease of handling, and avoidance of defacement of cadaver, thus allowing the use of same cadavers for subsequent anatomical dissection training.
Our study shows that agitated air-water contrast could be used to assess the extent of the spread of injectate in fascial planes on ultrasound. Even though, microbubbles contrast has been in use in contrast echocardiography and joint arthrography for a long-time,[7] it's utility for studying spread of injectate in muscle planes needs validation with dye and dissection or MRI with contrast studies. From the results of our study, the cephalad spread was variable. In majority of cadavers, the cephalad spread was up to the 3rd inter-costal space (other factors which could influence spread, such as injection pressure, length of needle, syringe size, volume of injectate, and position of cadaver, being constant). One is mindful of extrapolating data from cadaveric studies to patients as spread of injectate may not be the same (other factors may influence the spread of injectate in patients, such as differing tissue resistance, respiration, vascular pulsations, movement, and muscle contractions). Further, clinical studies will help us understand how the ultrasound spread correlates with the radiological spread and how this spread correlates with sensory dermatomal blockade with an injection of local anesthetics.
There seems to be positive correlation between the spread observed in our study (from T3 to subcostal region) and the findings of Blanco et al. in their volunteer clinical study (below the serratus muscle injections of 0.4 ml/kg local anesthetic gadolinium mixture produced sensory loss in the anterior hemi-thorax between T2 and T6, the lateral hemi- thorax T2-T8, and in the posterior hemi-thorax T2-T9).[6] We, therefore, surmise that the dermatomal spread may be greater than the visualized ultrasound spread. Key methodological differences which could explain Blanco's results are, that it was a clinical study and there was a longer duration from injection to clinical testing (30 minutes).
The serratus anterior muscle originates from the anterolateral surfaces of the first 8 or 9 ribs just anterior to the MAL and inserts on the anterior surface of the medial margin of the scapula from the superior to the inferior angle. The findings of our study showed that most of the cadavers had a well-formed serratus anterior muscle belly just before the PAL in the 4th or 5th ICS which correlates with anatomic studies. The observed spread of ultrasound contrast ranged from T3 to subcostal space in the vast majority in our study. We hypothesize that identifying the belly of the serratus muscle and deposition of injectate below it may play a pivotal role in their spread. Probably our hypothesis could explain why Blanco et al. reported a reduced spread for a below the serratus injection when compared with injection above the serratus (i.e. between latissimus dorsi and serratus anterior) as their injections were too anterior in the MAL. As again, further larger clinical studies are warranted to confirm our suspicion.
Finally, the volume of water we used to delineate the SAP were derived from the previous studies by Blanco et al. (0.4 ml/kg).[6] In our study, we limited the volume of injectate to 30 mls total with which the spread was identified on ultrasound to be from 3rd to subcostal space in the most cases. Again, further clinical trials are warranted to determine the volume of injectate.
Conclusion
This study shows that agitated air-water serves an excellent contrast media, enabling it to be used in cadaveric studies to delineate fascial planes and to demonstrate the spread of injectate. However, it does require validation with dye-dissection or radiological methods. The cephalad spread of injectate in the SAP is variable for the same volumes of injectate and further clinical trials are warranted to corroborate the same.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Tran TM, Ivanusic JJ, Hebbard P, Barrington MJ. Determination of spread of injectate after ultrasound-guided transversus abdominis plane block: A cadaveric study. Br J Anaesth. 2009;102:123–7. doi: 10.1093/bja/aen344. [DOI] [PubMed] [Google Scholar]
- 2.Milan Z, Tabor D, McConnell P, Pickering J, Kocarev M, du Feu F, et al. Three different approaches to transversus abdominis planeblock: A cadaveric study. Med Glas (Zenica) 2011;8:181–4. [PubMed] [Google Scholar]
- 3.Ishiguro S, Yokochi A, Yoshioka K, Asano N, Deguchi A, Iwasaki Y, et al. Technical communication: Anatomy and clinical implications of ultrasound-guided selective femoral nerve block. Anesth Analg. 2012;115:1467–70. doi: 10.1213/ANE.0b013e31826af956. [DOI] [PubMed] [Google Scholar]
- 4.de Jong N, Ten Cate FJ. New ultrasound contrast agents and technological innovations. Ultrasonics. 1996;34:587–90. doi: 10.1016/0041-624x(96)00032-7. [DOI] [PubMed] [Google Scholar]
- 5.Kunhabdulla NP, Agarwal A, Gaur A, Gautam SK, Gupta R, Agarwal A. Serratus anterior plane block for multiple rib fractures. Pain Physician. 2014;17:E553–5. [PubMed] [Google Scholar]
- 6.Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: A novel ultrasound-guided thoracic wall nerve block. Anesthesia. 2013;68:1107–13. doi: 10.1111/anae.12344. [DOI] [PubMed] [Google Scholar]
- 7.Di Tullio M, Sacco RL, Massaro A, Venketasubramanian N, Sherman D, Hoffmann M, et al. Transcranial Doppler with contrast injection for the detection of patent foramen ovale in stroke patients. Int J Card Imaging. 1993;9:1–5. doi: 10.1007/BF01142927. [DOI] [PubMed] [Google Scholar]


