Abstract
Background:
Uncuffed endotracheal tubes are commonly used in children but due to several decade preferred in paediatric oral surgery. Due to lack of conclusive evidences in this regard, we have conducted this study to compare post-operative morbidity following use of cuffed and uncuffed endotracheal tubes in paediatric patients undergoing cleft lip-palate surgery.
Methods:
This randomised controlled trial was conducted on children aged 2 to 12 years.110 patients were allocated in two parallel groups using computer generated list of random numbers. Post operative extubation stridor, sore throat, time to first oral intake and regaining of normal voice were compared between two groups.
Results:
The incidence of sore throat was significantly more (P value > 0.005) in patients of uncuffed group compared to cuffed group. The time to first oral intake and time to regain normal voice were significantly earlier in cuffed group compared to the other.
Conclusion:
With standard care, preformed cuffed ET tube has shown reduced incidence of post operative sore throat. Cuffed group has earlier oral intake and normal voice regain compared to uncuffed group.
Keywords: Cleft palate, cuffed, postoperative morbidity, preformed tracheal, uncuffed
Introduction
The use of cuffed or uncuffed endotracheal tube (UETT) in children <8 years is a matter of debate for years. Several studies stated multiple disadvantages of UETT like inappropriate size selection, increased tube exchange rate, chance of aspiration of oral secretions, blood and tissue debris, gas leakage, operation theatre pollution, difficult low flow anesthesia, improper monitoring of end-tidal CO2 (EtCO2), other ventilatory parameter and lung function, tube tip dislodgement, and accidental extubation during manipulation of head.[1,2] Throat pack given to prevent these complications again increases pack related postoperative sore throat (POST).[3,4,5,6] These problems can be solved by the use of cuffed tube. In spite of these advantages, cuffed tube is not widely accepted in pediatric practice because of the ideas against cuffed ET tube that, it would produce airway mucosal injury. Recent imaging study report suggests that with low cuff pressure (≤15 cm H2O), cuffed tube can efficiently seal the airway without increase in complications.[7] Hence, the use of cuffed endotracheal tubes (CETTs) in children can be suggested in the pediatric population with monitoring of cuff pressure.
According to Sathyamoorthy et al., all types of ETTs have the potential to cause airway damage. The factors like previous intubation, coexisting morbidity, patient movement etc., may have a role in producing airway edema and scarring. The rigid cricoid ring and vocal folds are particularly susceptible to damage due to lack of any substantial submucosal layer.[8] Weiss et al. 2009 have found a significantly low rate of tube exchange in cuffed tube compared to uncuffed tube in patients below 5 years of age. The postextubation stridor was comparable in both groups.[9] The importance of CETT can be best appreciated in oral surgical procedures, e.g., Cleft lip-palate surgery where the chance of aspiration is more than another surgery.[10,11,12,13,14,15,16] Due to the paucity of studies from India, we conducted a study in the pediatric population.
Hence, in this randomized controlled trial, we intended to compare the postoperative morbidity due to cuffed versus uncuffed tube in cleft lip-palate surgery in pediatric patients.
Materials and Methods
After approval from the Institutional Ethics Committee and informed written consent from the parents, this randomized controlled trial was carried out on children undergoing cleft lip-palate surgery under general anesthesia from April 2014 to March 2015. All children were hospitalized at least 1 day before surgery. The preoperative anesthetic fitness assessment was conducted on each patient. Patients with American Society of Anesthesiologists physical status 1 and 2 were selected. Patient with other congenital anomalies and patients with high risk of postoperative infection and aspiration were excluded from the study. After written consent from the legally acceptable representative, the patients were allocated into either of two groups guided by computer-generated list of random numbers.
The sample size was calculated based on the reported incidence of POST of 15% and 45% in cuffed and UETT.[6,15] Totally, 47 evaluable subjects were required in each group to achieve a power of the study of 90% and 5% type I error. Assuming a drop-out of 15%, approximately 56 patients were required in each arm. Sample size calculation was done using nMaster version 2.0 software (Deptt. of Biostatistics, CMC Vellore, India). One patient from each group was excluded from the analysis as they required a prolonged postoperative ventilatory support. Two patients of cuffed group were assigned uncuffed tube group due to unavailability of the appropriate tube. Hence, as per “intention to treat” analysis, 57 patients of uncuffed group were compared with 53 patients of cuffed tube group [Figure 1].
Figure 1.
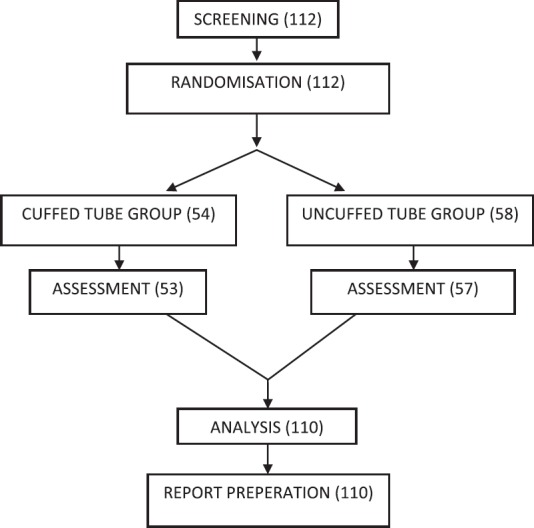
Flowchart as per CONSORT Guideline
We followed the standard practice of inducing anesthesia by inhalation of sevoflurane in 100% oxygen. Intravenous access was secured with 22-gauge intravenous cannula. The precordial stethoscope was used in every case to monitor the ventilation and heart rate (HR). Continuous perioperative monitoring (HR, SpO2, noninvasive blood pressure, electrocardiogram, EtCO2, and core temperature) was performed. Once a suitable depth of anesthesia was reached, face mask ventilation was confirmed, paralysis achieved with injection atracurium. Then, tracheal intubation was done under direct laryngoscopy by oral route without the use of bougies or stylets.
Preformed CETT, south facing (Mallinckrodt Medical, Athlone, Ireland) with high volume, low-pressure cuffs and preformed UETT were used in our study. Tube size selections were based on Motoyama formula (ID [mm] = [age in year/4] + 3.5)[1,7,10] for CETT in children aged 2 years or older. UETT sizes were selected according to Modified Cole's formula (ID [mm] = [age in year/4] + 4.0).[7,17] Tube insertion depths were managed according to standard guidelines. Lungs were checked for bilateral equal breath sounds.
Appropriate sizes of tracheal tubes were judged according to the presence of air leak. Air leak pressures after intubation were tested with the patient supine and the head in neutral position. An audible air leak at the patient's mouth had to be present at ≤20 cm H2O positive inflation pressure in UETTs and in CETTs with the cuff fully deflated in accordance with the recommendations of Motoyama et al.[9,17] Tracheal tube size was judged as adequate if the leak pressure (airway pressure needed to establish an air leak around the tracheal tube with the cuff not inflated) was ≤20 cm H2O and if the sealing pressure (cuff pressure to seal the trachea) was ≤20 cm H2O. The UETT was exchanged to the next smaller size of UETT or CETT variety if the leak pressure was too high (>20 cm H2O) and CETT was changed to similar size UETT or 0.5 mm smaller CETT. CETT changed to next larger size if a sealing pressure more than 20 cm H2O was necessary to prevent a leak. When changing an UETT to next smaller size which resulted in excessive air leak, a sterile water-soaked gauze throat pack or CETT was used. In three patient of either group, the tube has to be changed due to discrepancy of size and high leak pressure.
After assuring that no oversized tube was inserted in either group, adequacy of sealing was tested by mechanical ventilation of the patients. For CETTs, the cuff was inflated with the cuff pressure manometer (Portex). Cuff pressure was limited to 20 cm H2O with a pressure release valve. The Minimal sealing pressure was assessed under steady-state ventilation conditions and maintained during the procedure. This was performed by slowly reducing the cuff pressure until an audible leak appeared at the patient's mouth and then the pressure was increased until leak disappearance. Minimal cuff pressure required to seal the airway and quality of sealing was recorded. Further intubation time, anesthetic technique, course of intubation, leak pressure, and use of throat pack were noted.
There was every chance of tube occlusion and inadvertent extubation at any stage due to shared airway. Intraoperatively, any untoward effects like decreased oxygenation, accidental endobronchial intubation, or extubation were recorded. A head ring and a roll under the shoulders were frequently used to extend the neck. General anesthesia was maintained according to standard protocol using N 2 O:O2 = 2:1, sevoflurane (3-4%), injection atracurium, injection glycopyrrolate, injection dexamethasone, and injection ondansetron were used before intubation after securing the intravenous access. Intraoperative analgesia was provided with injection fentanyl, paracetamol infusion. Postoperative analgesia was maintained by regular doses of paracetamol and diclofenac suppository according to body weight.
On completion of surgery, the oropharynx was thoroughly inspected, and the throat pack (where used) with blood clots were removed and hemostasis assessed. The child was extubated after antagonism of residual neuromuscular block and when fully awake. Supplementary oxygen was given postoperatively. All patients were sent to the post anesthesia care unit after extubation. The occurrence of laryngospasm, postextubation stridor, sore throat, time to first oral intake, regaining of normal voice in next 24 h and any other complications were recorded by an anesthesiologist blinded to group allocation. Postoperative morbidities were assessed clinically at regular interval.
The summary statistics was presented with appropriate measure of central tendency (mean and median) and dispersion (standard deviation and interquartile range for numerical variable and frequency for categorical variables). Independent groups were compared using appropriate test of significance. P < 0.05 was considered as statistically significant. Statistical calculation was performed using SPSS© version 20 (IBM Inc., New York, USA) and sample size was calculated using software nMaster© version 2.0 (Department of Biostatistics, CMC, Vellore, Tamil Nadu, India).
Results
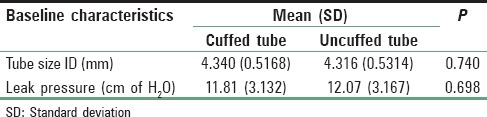
Of 110 patients of cleft lip-palate surgery satisfying the selection criteria, we have used preformed CETT in 53 patients (48.2%) and UETT among the rest. About 55.5% of the sample were male. Patients’ demographic variables are presented in Table 1. Baseline characteristics are presented in Tables 2 and 3. Patient's outcome measures are presented in Bar Graphs 1 and 2.
Table 1.
Demographic variables
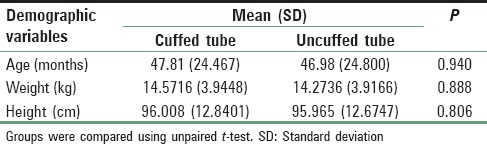
Table 2.
Baseline characteristics (types of surgery and ASA)
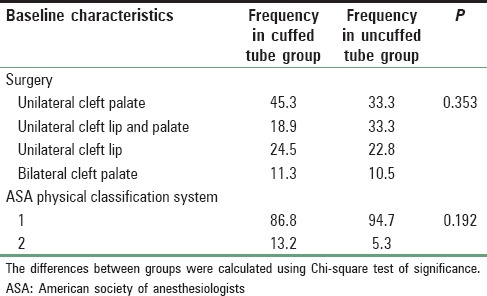
Table 3.
Baseline characteristics (tube size and leak pressure)
Bar Graph 1.
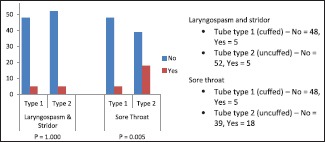
Laryngospasm and stridor, sore throat
Bar Graph 2.
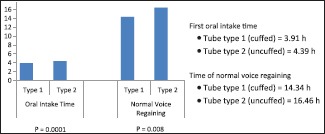
First oral intake time, time of normal voice regaining
Postextubation laryngospasm and stridor were noted 9.4% and 8.8% in cuffed and uncuffed groups, respectively with no statistically significant difference between the groups (P = 0.15). But, the incidence of sore throat was significantly higher in uncuffed (31.6%) in comparison to cuffed (9.4%) variety (P = 0.005). Mean oral intake time was significantly more (4.39 h) in uncuffed compared to the other (3.91 h) (P = 0.0001). Similarly, mean time of regaining normal voice was also significantly late in uncuffed (16.46 h) than cuffed (14.34 h) (P = 0.008).
Discussion
Airway management in cleft lip and cleft palate surgery is very crucial as airway is shared between surgeon and anesthesiologists. There is an increased possibility of inadvertent extubation, tube occlusion by mouth gag used for this surgery and the chance of aspiration, especially in palate surgery where pharyngeal pack is not given. Preformed RAE ETT is considered ideal as it is better fitted in mouth gag and fixation of the tube is easy[1] uncuffed preformed tracheal tubes were more at risk for inadvertent endobronchial intubation than cuffed preformed tracheal tubes.[10]
In our study, we have compared cuffed and uncuffed RAE tube in cleft lip-palate surgery. The trend regarding pediatric ETT in near past was to use uncuffed variety below 8 years of age as the traditional belief was that cuff would produce airway injury and postoperative respiratory complications. Several study stated number of advantages of cuffed tube., including greater ease of intubation, reduced tube exchange rate (from 30.8% to 2.1%)[9] cost and time saving, less trauma and intubation stress, reduced consumption of expensive volatile anesthetics, making low flow anesthesia possible. There is also reduced levels of gases and volatile anesthetics in the operating room, and therefore, a decreased level of environmental pollutants.[11] CETT helps in reliable lung function monitoring and capnography. The risk of aspiration and infection is also decreased.[12,13]
The overall incidence of postextubation stridor in pediatric patients has been reported around 14.9%.[14] we found no significant difference in incidence of postoperative stridor between cuffed and uncuffed tube In this study. However, no study has demonstrated that a CETT compared to UETT causes an increased risk of airway complications provided an appropriate size is chosen, and the cuff pressure is monitored. Our result does not differ with that of Khine et al. Murat et al.[18,19] and Weiss et al. showed that cuffed TTs are not associated with higher airway morbidity in small children.[9] In another study, they mentioned that the use of cuffed TTs in small children provides a reliably sealed airway at cuff pressures of ≤20 cm H2O, reduces the need for TT exchanges, and does not increase the risk for postextubation stridor compared with uncuffed TTs.[1,9]
Tracheal intubation is a leading cause of POST producing trauma to the airway mucosa that contributes to postoperative morbidity and patient dissatisfaction. Patients’ age, sex, large tracheal tube, throat pack, and intracuff pressure are contributing factors for POST. The incidence of sore throat after tracheal intubation, varies from 14.4% to 50%.[3] In our study, the incidence of sore throat was higher in the uncuffed group (31.6%) in comparison to cuffed (9.4%) variety and the P value was statistically significant. By comparing the age, sex, tracheal tube size, the cause of sore throat related to pharyngeal pack might be a consequence of localized trauma, leading to aseptic inflammation of pharyngeal mucosa.[6,20] Our results corroborates with that of Calder et al., who found that children are more likely to have POST with UETTs.[21] They also suggested to measure cuff pressure routinely in case of CETT as there is positively correlation of CP with the incidence of POST. Loeser et al. also found significantly higher incidence of sore throat with uncuffed tubes than of cuffed tubes, even when the patients breathed warmed and humidified gases.[15]
Time to first oral intake and regaining of normal voice after surgery was significantly delayed in uncuffed group compared to the cuffed group in our study. This may be related to increased incidence of sore throat in this group.
Bhardwaj N has mentioned that lower cuff pressure may be safer in children as specific data are unavailable in children regarding perfusion pressure of tracheal mucosa like adults (upper limit of safety of cuff pressure 25-30 cm of H2O).[11] Based on recent studies using magnetic resonance imaging scans, it has been postulated that CETTs with low pressure, high volume cuff will seal the airway at the upper trachea where the posterior membranous wall can stretch and produce a complete seal with low cuff pressure of <15 cm H2O without any increase in airway complications.[16,17,22] In our study, minimal cuff pressure required to seal the trachea was 10.6 (4.3) cm H2O. Our results corresponds with that of Weiss et al., who found cuff inflation or sealing pressure (mean = 14.87 cm of than adults. They concluded CETTs in small children provided a reliably sealed airway at cuff pressures of ≤20 cm H2O, without increasing the risk for postextubation stridor in comparison to uncuffed TTs.[9] But it should be noted Erb and Frei have recommended continuous monitoring of the cuff pressure when using CETTs in this age group.[23] Furthermore, Ramesh et al. have recommended that constant and precise monitoring of cuff pressure is essential as active over-inflation by nitrous oxide diffusion can cause laryngeal complications.[12]
Some limitations of our study might merit discussion. In this monocentric study, we had limited scope of evaluating ethno-racial variations of postoperative morbidity. Children below the age of 2 years were not included in our study. Several possible outcome measures like cuff positions, tube tip dislodgement, tube exchange rate, intubation attempts, ventilator parameters etc., might be considered in future studies. Longer postoperative follow-up was necessary to establish the long-term safety of certain ET tube variety. Hence, a multicentric study with larger sample size and long-term follow-up is needed to conclusively prove the superiority of cuffed ET tube over uncuffed ET tube. There are limitations to use of postextubation stridor as a sign of laryngeal, subglottic or tracheal injury related to ETT use. The diagnoses of postextubation stridor were subjective. Objective methods for evaluation are either impractical or not yet fully evaluated.
Conclusion
The idea against the use of cuffed ETT in pediatric patients has limited justification. With proper selection of tube size, monitoring of cuff pressure and careful postextubation respiratory care, preformed cuffed ETT can be used as safely as uncuffed tube. Cuffed ETTs were better tolerated in terms of airway morbidity measured by less incidence of POST, early oral intake and early regaining of normal voice after the procedure in cleft lip-palate surgery in pediatric age group in our setting.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Weiss M, Dullenkopf A, Böttcher S, Schmitz A, Stutz K, Gysin C, et al. Clinical evaluation of cuff and tube tip position in a newly designed paediatric preformed oral cuffed tracheal tube. Br J Anaesth. 2006;97:695–700. doi: 10.1093/bja/ael247. [DOI] [PubMed] [Google Scholar]
- 2.Litman RS, Maxwell LG. Cuffed versus uncuffed endotracheal tubes in pediatric anesthesia: The debate should finally end. Anesthesiology. 2013;118:500–1. doi: 10.1097/ALN.0b013e318282cc8f. [DOI] [PubMed] [Google Scholar]
- 3.McHardy FE, Chung F. Postoperative sore throat: Cause, prevention and treatment. Anesthesia. 1999;54:444–53. doi: 10.1046/j.1365-2044.1999.00780.x. [DOI] [PubMed] [Google Scholar]
- 4.Tay JY, Tan WK, Chen FG, Koh KF, Ho V. Postoperative sore throat after routine oral surgery: Influence of the presence of a pharyngeal pack. Br J Oral Maxillofac Surg. 2002;40:60–3. doi: 10.1054/bjom.2001.0753. [DOI] [PubMed] [Google Scholar]
- 5.Bosenberg AT. Anesthesia for cleft lip and palate surgery. South Afr J Anaesth Analg. 2007;13:9–14. [Google Scholar]
- 6.Canbay O, Celebi N, Sahin A, Celiker V, Ozgen S, Aypar U. Ketamine gargle for attenuating postoperative sore throat. Br J Anaesth. 2008;100:490–3. doi: 10.1093/bja/aen023. [DOI] [PubMed] [Google Scholar]
- 7.Taylor C, Subaiya L, Corsino D. Pediatric cuffed endotracheal tubes: An evolution of care. Ochsner J. 2011;11:52–6. [PMC free article] [PubMed] [Google Scholar]
- 8.Sathyamoorthy M, Lerman J, Lakshminrusimha S, Feldman D. Inspiratory stridor after tracheal intubation with a MicroCuff® tracheal tube in three young infants. Anesthesiology. 2013;118:748–50. doi: 10.1097/ALN.0b013e318282cc7a. [DOI] [PubMed] [Google Scholar]
- 9.Weiss M, Dullenkopf A, Fischer JE, Keller C, Gerber AC. European Paediatric Endotracheal Intubation Study Group. Prospective randomized controlled multi-centre trial of cuffed or uncuffed endotracheal tubes in small children. Br J Anaesth. 2009;103:867–73. doi: 10.1093/bja/aep290. [DOI] [PubMed] [Google Scholar]
- 10.Weiss M, Bernet V, Stutz K, Dullenkopf A, Maino P. Comparison of cuffed and uncuffed preformed oral pediatric tracheal tubes. Paediatr Anaesth. 2006;16:734–42. doi: 10.1111/j.1460-9592.2006.01844.x. [DOI] [PubMed] [Google Scholar]
- 11.Bhardwaj N. Pediatric cuffed endotracheal tubes. J Anaesthesiol Clin Pharmacol. 2013;29:13–8. doi: 10.4103/0970-9185.105786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramesh S, Jayanthi R, Archana SR. Paediatric airway management: What is new? Indian J Anaesth. 2012;56:448–53. doi: 10.4103/0019-5049.103959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fine GF, Borland LM. The future of the cuffed endotracheal tube. Paediatr Anaesth. 2004;14:38–42. doi: 10.1046/j.1460-9592.2003.01203.x. [DOI] [PubMed] [Google Scholar]
- 14.Deakers TW, Reynolds G, Stretton M, Newth CJ. Cuffed endotracheal tubes in pediatric intensive care. J Pediatr. 1994;125:57–62. doi: 10.1016/s0022-3476(94)70121-0. [DOI] [PubMed] [Google Scholar]
- 15.Loeser EA, Bennett GM, Orr DL, Stanley TH. Reduction of postoperative sore throat with new endotracheal tube cuffs. Anesthesiology. 1980;52:257–9. doi: 10.1097/00000542-198003000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Litman RS, Weissend EE, Shibata D, Westesson PL. Developmental changes of laryngeal dimensions in unparalyzed, sedated children. Anesthesiology. 2003;98:41–5. doi: 10.1097/00000542-200301000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Motoyama EK. The shape of the pediatric larynx: Cylindrical or funnel shaped? Anesth Analg. 2009;108:1379–81. doi: 10.1213/ane.0b013e31819ed494. [DOI] [PubMed] [Google Scholar]
- 18.Khine HH, Corddry DH, Kettrick RG, Martin TM, McCloskey JJ, Rose JB, et al. Comparison of cuffed and uncuffed endotracheal tubes in young children during general anesthesia. Anesthesiology. 1997;86:627–31. doi: 10.1097/00000542-199703000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Murat I, Constant I, Maud’huy H. Perioperative anaesthetic morbidity in children: A database of 24,165 anaesthetics over a 30-month period. Paediatr Anaesth. 2004;14:158–66. doi: 10.1111/j.1460-9592.2004.01167.x. [DOI] [PubMed] [Google Scholar]
- 20.Weiss M, Dullenkopf A, Gysin C, Dillier CM, Gerber AC. Shortcomings of cuffed paediatric tracheal tubes. Br J Anaesth. 2004;92:78–88. doi: 10.1093/bja/aeh023. [DOI] [PubMed] [Google Scholar]
- 21.Calder A, Hegarty M, Erb TO, von Ungern-Sternberg BS. Predictors of postoperative sore throat in intubated children. Paediatr Anaesth. 2012;22:239–43. doi: 10.1111/j.1460-9592.2011.03727.x. [DOI] [PubMed] [Google Scholar]
- 22.Dalal PG, Murray D, Messner AH, Feng A, McAllister J, Molter D. Pediatric laryngeal dimensions: An age-based analysis. Anesth Analg. 2009;108:1475–9. doi: 10.1213/ane.0b013e31819d1d99. [DOI] [PubMed] [Google Scholar]
- 23.Erb T, Frei FJ. The use of cuffed endotracheal tubes in infants and small children. Anaesthesist. 2001;50:395–400. doi: 10.1007/s001010100158. [DOI] [PubMed] [Google Scholar]


