Abstract
Background:
Knowledge of community medicine is essential for health care professionals to function as efficient primary health care physicians. Medical students learning Community Medicine as a subject are expected to be competent in critical thinking and generic skills so as to analyze community health problems better. However, current teaching by didactic lectures fails to develop these essential skills. Problem-based learning (PBL) could be an effective strategy in this respect. This study was hence done to compare the academic performance of students who were taught Community Medicine by the PBL method with that of students taught by traditional methods, to assess the generic skills of students taught in a PBL environment and to assess the perception of students toward PBL methodology.
Materials and Methods:
This study was conducted among seventh-semester final-year medical students between June and November 2014. PBL was introduced to a randomly chosen group of students, and their performance in an assessment exam at the end of postings was compared with that of the remaining students. Generic skills and perception toward PBL were also assessed using standardized questionnaires.
Results:
A total of 77 students took part in the brainstorming session of PBL. The correlation between self-assigned scores of the participants and those assigned by the tutor in the brainstorming session of PBL was significant (r = 0.266, P = 0.05). Out of 54 students who took part in the presentation session, almost all 53 (98.1%) had good perception toward PBL. Demotivational scores were found to be significantly higher among males (P = 0.024). The academic performance of students (P < 0.001) and success rates (P = 0.05) in the examination were higher among students who took part in PBL compared to controls.
Conclusion:
PBL helped improve knowledge of students in comparison to those exposed only to didactic lectures. As PBL enabled students to identify the gaps in their knowledge and enhanced their group functioning and generic skills, we recommend PBL sessions: They would help optimize the training in Community Medicine at medical schools. Good correlation of tutor and self-assessment scores of participants in the brainstorming session suggests that the role of tutors could be restricted to assessment in presentation sessions alone. Demotivation, which hinders group performance in PBL, needs to be corrected by counselling and timely feedback by the tutors.
Keywords: Community medicine, generic skills, medical students, perception, performance, problem-based learning (PBL)
Introduction
Community medicine plays a pivotal role in the delivery of health care. For efficiency in health care delivery, community health care professionals need to be successful primary health care physicians. This involves meticulous identification of common health problems in the community and the creation of effective interventional strategies to address these issues. Medical graduates today have to be critical thinkers and self-directed learners. They should have generic skills such as being able to effectively communicate and work in groups, in addition to problem-solving, while working in the community in activities including community diagnosis and investigation of epidemics. However, training for the same is lacking. Teaching is limited essentially to didactic lectures where students fail to develop these essential generic skills.(1)
World Health Organization (WHO) consultations on public heath teaching and training recommend utilization of 40% time for skill-building in all public health courses by innovative learning methods. These methods should make training student-centered, inquiry-driven, problem-oriented, and evidence-based, with the role of the teacher as a facilitator to help students to acquire these competencies.(2) The Medical Council of India also recommends the teaching of concepts in Community Medicine in a small group, teaching by student-centric and problem-based approaches.(3) The medical schools must therefore identify and define the curriculum models and instructional methods accordingly to meet these requirements among students.(2)
Problem-based learning (PBL) is a student-centered pedagogy in which students themselves determine what and how they learn.(4) PBL also encourages critical thinking skills, independent responsibility for learning, knowledge acquisition, sharing information, time management skills, better retention of information, and problem-solving abilities. It thus stimulates higher-order learning in students, leading to the achievement of high professional competency.(5,6) In the process, the student is inculcated with capabilities such as the ability to work productively as a team member, to master his/her communication skills, to develop better clinical reasoning skills and presentation skills, the ability to make decisions in unfamiliar situations, and respect for others, which are all key areas of a student's education in community medicine.(6,7) Studies have found that students in PBL classes have higher attendance and academic performance than students who have had experienced a mostly lectured-based curriculum.(8,9)
This was the first time that the Department of Community Medicine, Kasturba Medical College, Mangalore, Karnataka introduced PBL in their teaching curriculum. As PBL is not a common learning methodology in this setting, it was necessary to prove its effectiveness over the traditional teacher-led method of education.
This study was hence done to compare the academic performance of students who were taught by PBL methodology with that of students taught by traditional methods, to assess the generic skills of students taught in a PBL environment, and to assess the perception of students toward PBL.
Materials and Methods
This experimental study was done among seventh-semester final-year MBBS students of Kasturba Medical College, Mangalore. Ethical approval for conducting this study was obtained from the institutional Ethics Committee. The tutor underwent training in PBL facilitation skills through workshops conducted by experts in the Medical Education Unit of this institution and at Melaka-Manipal Medical College, Manipal Campus, India. Content validation of the study tools was done by experts in Internal Medicine and from Medical Education Unit of this institution. The study was then conducted between June and November 2014. It is during this period that students in their seventh semester have clinical postings in Community Medicine, in batches of 50 students every month. Each batch is further divided into five subgroups of 10 students each. Each subgroup has to present a medicosocial/bedside case in communicable disease, noncommunicable disease, pediatrics, antenatal care, or postnatal care every day, followed by lectures by the tutors in the hospital wards. A subgroup of students chosen by simple random method formed the study group in PBL intervention and were given an exercise on malaria. Similarly, another subgroup was chosen to participate in a PBL exercise on tuberculosis. The remaining 40 students in each round of PBL sessions constituted the control groups. The study groups were briefed about the objective of the study, and written informed consent was taken individually for their participation. These students were given 30 minutes orientation on PBL methodology using PowerPoint slides self-prepared by the tutor based on PBL literature available online. This was followed by 10 minutes question/answer session and discussion in rounds among participants on PBL methodology using validated multiple-choice questions (MCQs) shown on PowerPoint slides. The entire PBL session was modelled on the Maastricht “seven jump” process using validated PBL exercises.(5)
The generic skills of the students during the brainstorming and presentation sessions were assessed by the tutor using a separate, validated, modified version of standard checklists developed by Elizondo-Montemayor.(10) The students also self-assessed their performance using the same checklist at the end of each session. Each parameter in the checklist was scored between 1 and 10 points. Various parameters in the checklists of the brainstorming and presentation sessions were categorized into those to assess knowledge-building and inquiry skills, group skills, problem-solving skills, and attitude during discussion and professionalism. The cumulative score for each category was further classified as poor, average, or good performance. Individual feedback on their performance was given to all participants by the tutor at the end of each session. After the presentation session, students were given a validated, modified version of the standardized feedback form(10) to enable them to share their PBL tutorial experience. It contained 49 statements to assess perception under areas such as application of knowledge base, clinical reasoning and decision-making, self-directed learning, and collaborative work in PBL sessions. It also included statements on perceptions toward peer performance (inclusive of a question on perception towards self-contribution in PBL sessions) and tutor's performance, and on PBL exercise given in the sessions. This form was designed as a five-point Likert scale. Five points were assigned to “strongly agree” responses and one point was assigned to “strongly disagree” responses. Reverse scoring was done for negative statements. Cumulative scores ranging 53-115 were considered as poor, 116-178 as average, and 179-241 as good perception toward PBL. The statements in this perception assessment form were also categorized as those related to cognition, motivation, and demotivation. The motivation domain dealt with the extent to which students express concern, motivate, and help each other learn.(11) The cognition domain dealt with the extent of learning and understanding the topic, and the demotivation domain dealt with adverse influence on learning due to the extent of nonparticipation among a few students.(11)
Demographic information on the age, gender and nationality of the participants and their previous experience in case-based learning (CBL) or PBL was also collected in this form. On the final day of the 1-month postings, students of both the study and the control group took part in two written examinations, one on malaria and the other on tuberculosis, each of 30 minutes duration. Each paper contained 10 MCQs to assess content knowledge, 4 clinical reasoning MCQs to assess problem-solving and critical-thinking skills, and 1 short-answer question to assess the understanding of basic concepts and in-depth knowledge about the related disease. Out of the 10 direct MCQs, the first 5 were based on Bloom's taxonomy levels 1 and 2 (knowledge and comprehension) and the second 5 were based on levels 3-6 (application, analysis, synthesis, and evaluation).(12) The clinical reasoning MCQs were long case vignettes consisting of patient history, physical findings, and laboratory data; students would be required to study them and synthesize important findings to reach an accurate conclusion.
One mark was awarded for a correct answer to each MCQ, and a maximum of 6 marks were awarded for the short-answer question. Participants obtaining 50% marks in the examination were considered successful.
A total of three sets of question papers were used on rotation every month throughout the study.
The Cronbach's alpha values of internal consistency for the assessment questionnaire, namely, Set 1, 2, and 3 on tuberculosis were 0.723, 0.711, and 0.891, respectively. Similarly, the values for Set 1, 2, and 3 for the assessment questionnaire on malaria were 0.848, 0.794, and 0.799, respectively, indicating good reliability.
Data entry and analysis were done using the software package Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, USA) version 16. Karl Pearson's coefficient of correlation, unpaired t-test, one-way analysis of variance, and chi-square test were used to test association. P ≤ 0.05 was taken as a statistically significant association.
Results
The total of number of students who took part in the brainstorming session of PBL was 77. The numbers of participants aged 20, 21, 22, and ≥23 years were 13 (16.9%), 36 (46.7%), 14 (18.2%), and 14 (18.2%) respectively. The majority of participants [46 (59.7%)] were females; the majority were Indian nationals [61 (79.2%)]. No students had prior exposure to PBL in other subjects. However, 30 (39%) participants reported prior exposure to CBL in other subjects.
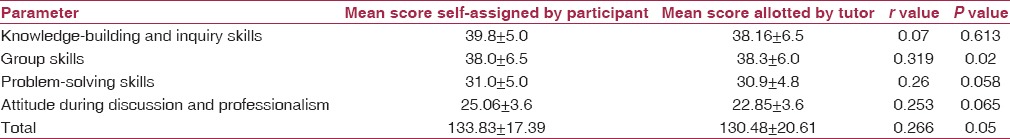
In the brainstorming session, the correlations between self-assigned scores of the participants and those given by the tutor in knowledge-building and inquiry skills (P = 0.613), problem-solving skills (P = 0.058), and attitude during discussion and professionalism (P = 0.065) were not significant. Only the scores assigned for group skills showed significant correlation (r = 0.319, P = 0.02). The overall performance scores in the brainstorming session also showed significant correlation (r = 0.266, P = 0.05) [Table 1].
Table 1.
Correlation between self-assigned scores by participants and scores allotted by the tutor in the brainstorming session (N = 77)
Student performance in knowledge-building and inquiry skills, group skills, problem-solving skills, and attitude during discussion in the brainstorming session was rated average for 16 (20.8%) and good for 61 (79.2%) participants by the tutor.
Out of the 77 participants who took part in the brainstorming session, 54 students took part in the presentation session of PBL.
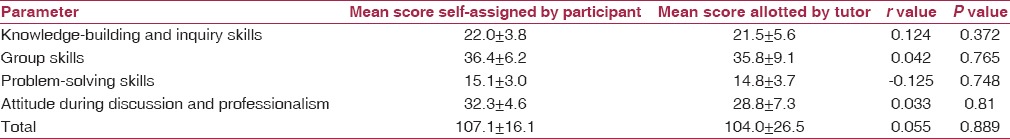
There was no significant correlation between self-assigned scores of the participants with those given by the tutor in the presentation session [Table 2].
Table 2.
Correlation between self-assigned scores by participants and scores allotted by the tutor in the presentation session (N = 54)
The assessment by the tutor of the performance of students in knowledge-building and inquiry skills in presentation session was poor for 3 (5.6%), average for 15 (27.8%), and good for 36 (66.6%) participants. The ratings of students as poor, average, and good in the group skills section were 3 (5.6%), 16 (29.6%), and 35 (64.8%); in the problem-solving skills section were 3 (5.6%), 14 (25.9%), and 37 (68.5%); and in the section for attitude during discussion were 3 (5.6%), 12 (22.2%), and 39 (72.2%). Attitude during discussion, including accepting feedback with openness, reacting positively to feedback, standing up for one's own point of view, and the ability to change point of view in light of new information gained from peers, varied significantly with nationality (P = 0.042).
Almost all participants [53 (98.1%)] had an overall good perception toward PBL [Table 3]. In this study, 49 (90.7%) participants felt PBL to be more interesting than traditional teaching methods.
Table 3.
Perception towards PBL among study group participants
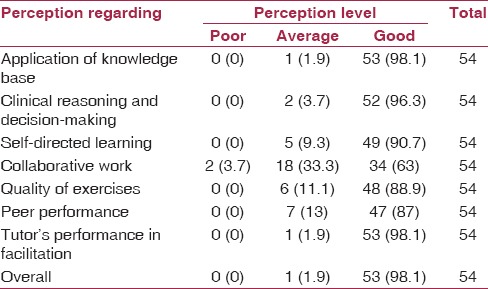
Perception toward PBL was not associated with age (P = 0.145), gender (P = 0.611), nationality (P = 0.167), or previous experience in CBL (P = 0.37).
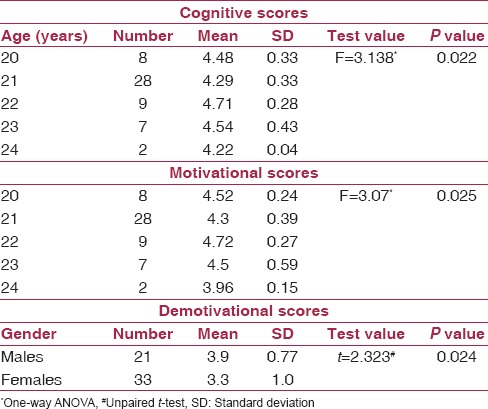
The mean cognitive score was 4.42 ± 0.36, the mean motivational score was 4.41 ± 0.41, and the mean demotivational score was 3.54 ± 0.97 among the students. The median cognitive score was 4.38, the median motivational score 4.43, and the median demotivational score was 4. Cognitive (P = 0.022) and motivational scores (P = 0.025) were found to significantly vary with the age of participants. Demotivational scores were found to be significantly higher among males (P = 0.024) [Table 4]. No association of these scores with nationality or previous exposure to CBL was seen in this study.
Table 4.
Association between sociodemographic variables and motivational, demotivational, and cognitive perception scores among students (N = 54)
Out of the 54 students who took part in the presentation session, 49 appeared for the assessment examination. Among the controls, 369 took part in the assessment examination. To obtain a ratio of 1:4 between study group and control group participants, controls as many as four times the number of PBL participants were selected every month. The selection was by simple random method using a random number table. Therefore, the final control group number came up to 196.
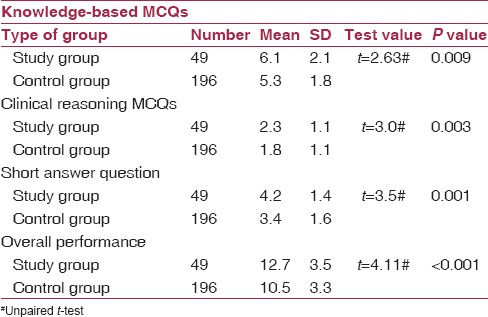
The performance of students who took part in PBL was found to be significantly better than others in various sections and on overall assessment in the examination [Table 5]. The mean performance score for short-answer questions among females (4.5 ± 1.5) was significantly higher than among males (3.7 ± 1.1), P = 0.036. The mean performance score for short-answer questions among the Indian nationals was 4.5 ± 1.36, which was better than that of the foreign students 3.0 ± 1.0 (P = 0.003). The overall performance score was 13.2 ± 3.3 among the Indian nationals, and this was better than that of the foreign students (10.2 ± 3.7) (P = 0.018). Performance scores did not differ significantly on other sections of assessment exam with respect to gender or nationality. Similarly, performance score did not vary with age (P = 0.164) or with previous exposure to CBL among participants (P = 0.921) in the examination.
Table 5.
Performance of students in study and control groups in various sections of the assessment examination (N = 245)
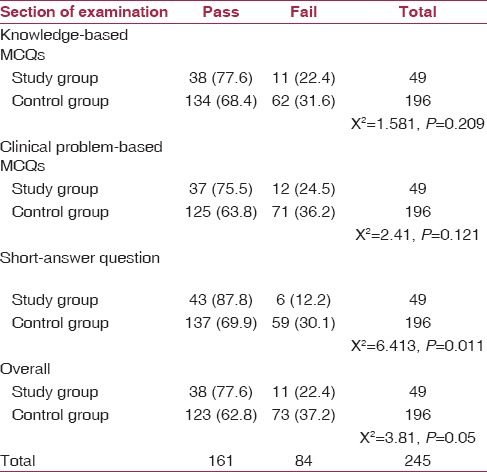
The pass percentage in the study group was significantly higher for short-answer questions (P = 0.011) and in overall assessment (P = 0.05) in the examination in comparison to the control group [Table 6].
Table 6.
Outcome of students of study and control groups in different sections of the assessment examination
Discussion
PBL discussions occurring within a small group of participants are known to facilitate the learning process.(11) Self-assessment of group performance in the discussion process was perceived to be good by most participants in this study, similar to findings in the Shankar et al. study.(13)
Previous researchers have observed that students learning by the PBL approach had better retention of medical knowledge,(14) were better at applying basic science knowledge to a clinical case,(15) had enhanced problem-solving abilities,(16) had marked improvement in higher-order thinking skills,(17) and had better profession-specific skills, communication skills, and teamwork.(18,19) In this study, too, the majority of students in the study group strongly agreed that PBL methodology enhances the above mentioned abilities among participants.
More than half of participants in this study [29 (53.7%)] strongly agreed that PBL exercises paved the way for reading diverse and recent bibliographic sources. In other studies, students following PBL curricula were also found to make greater use of the library, self-selected learning resources, and were more confident in their independent information-seeking skills.(20,21) Previous studies have also reported better ability among students experiencing PBL to identify their own learning issues,(22) a collaborative learning environment due to interaction with other participants,(23) and a tendency to explore and learn new concepts that made learning interesting,(24) which were benefits most participants in this study also strongly agreed to have gained.
A majority of students (66.3%) in a study done in Malaysia reported that PBL developed their confidence in self-directed learning, which was higher than the reporting number of 31 (57.4%) students in this study.(25) Half of the students in this study [27 (50%)] strongly agreed that the PBL experience enhanced their clinical approach. In addition, 38 (70.4%) strongly agreed that it enhanced problem-solving abilities, which was higher than the 53.1% students reporting the same in the Malaysian study.(25) This substantiates the fact that PBL helps in improving practical application of concepts learned. Most participants [53 (98.1%)] in this study felt that the tutor played a good role as a facilitator in PBL exercise, which was similar to the high ratings given to tutors by students in a study done in the UK.(26) More than half of the students (53.4%) in the study done in Malaysia also agreed that the role of the facilitator in the process was helpful to them.(25) A few recent studies have also proved that tutor/facilitator-related behaviors influence student learning during PBL.(27,28)
In the study by Shankar et al., the mean cognitive score of student performance was 3.8 and the mean motivation score was 3.7, which were lower than our observations, where the mean scores in these aspects were both 4.4. However, the demotivation score in the former study was 2.5, indicating better performance than from our participants (mean score 3.5). In another study conducted in KwaZulu-Natal, South Africa the mean cognitive, motivational, and demotivational scores were 3.12, 3.32, and 3.17 respectively.(29)
In this study, demotivation scores were found to be significantly higher among males. Attention should be focused on students who respond negatively to group work in PBL as it leads to group dysfunction.(30) Male participants in particular have to be counselled and motivated more before PBL sessions to improve group performance.
In this study, 8 (14.8%) participants strongly agreed that a few group members contributed less to the discussions. The success of any PBL session is dependent on the group members. Only when members help one another by sharing their concepts and viewpoints can stimulation of learning occur among listeners, leading to the solution of the exercise as a team, as observed in a UK-based study.(11) Poor contributions by some group members, on the other hand, may demotivate others from attaining their personal goals.(31) It is here that the facilitator/tutor plays a pivotal role, providing timely feedback and counselling individuals to improve group performance in PBL.(11)
In this study, students in the PBL intervention group performed significantly better than others in the assessment examination in Community Medicine. Similarly, in a Canada-based study, medical students obtained significantly better scores in the overall assessment in Preventive Medicine and Community Health under PBL compared to others.(32)
In a meta-analysis based on 15 studies done in China, it was found that PBL resulted in a significant increase in students’ theoretical examination scores in Preventive Medicine than didactic methods.(24) In a study done in Turkey, medical students in the PBL group scored significantly higher than the traditionally tutored group in a MCQ exam on public health topics.(33)
Experts have also suggested that several concepts covered under public health courses in a traditional curriculum can be effectively taught using PBL. This would result in better appreciation of the social and emotional aspects of health care among students.(4) From the above observations and from our study findings, it is clear that PBL can be used to learn topics in Community Medicine more effectively than through conventional teaching methodologies.
A UK based study observed that medical students in PBL group performed significantly better in MCQ scores when compared with others in the subject of Psychiatry.(34) In a study done in Saudi Arabia, students in a medical college belonging to the PBL curriculum obtained a higher score in the MCQ examination and objective structured practical examination in Respiratory Physiology, compared with students taught by didactic methods.(14) Burford et al. directed a randomized multicenter study in Pharmacology using PBL and traditional curricula, and demonstrated higher scores on knowledge testing from the PBL approach.(35)
However, in another study done among medical students in Lahore, Pakistan for the subjects of Obstetrics and Gynecology (OBG) and Surgery, content knowledge was significantly more among students taught through traditional teaching, involving bedside teaching and lectures in wards, which was different from our observations. But the significant difference in clinical reasoning and problem-solving skills in the PBL intervention group observed in the above mentioned study was similar to our findings.(17)
In this study, the pass percentage in the study group was significantly higher than controls. In other studies done in Canada(32) and United Kingdom,(34) students on a PBL curriculum reported fewer failures, but these observations were not significant.
In the UK based study, female medical students who were assigned the PBL curriculum were significantly more successful in the examinations and clinical viva than their male counterparts.(34) In our study, the only difference between the genders was seen in the performance of short-answer questions, but the overall performance did not differ significantly.
Considering the several benefits of PBL as observed in this study, it is not surprising that several medical schools worldwide are changing their curricula by adopting PBL programs.(35)
Conclusion
The results of the present study show that medical students who participated in a PBL curriculum obtained significantly higher knowledge, better clinical reasoning skills, and deeper understanding of the concepts of Community Medicine when compared with others taught by conventional methods. As PBL enabled students to identify the gaps in their knowledge and enhanced their group functioning and generic skills, we recommend PBL sessions: They would help optimize training in community medicine at medical schools.
The correlation between the tutor-allotted scores and the self-assigned scores of participants about their own performance was significant in the brainstorming session of PBL. Therefore, students’ self-assigned marks can be considered for brainstorming session, while tutors could focus on the assessment of presentation sessions alone. Counselling and timely feedback by tutors are also needed to minimize demotivation of participants, particularly males, during PBL sessions.
Limitations
The students in the control group did not benefit from PBL tutorials. Crossing over would have been ideal to solve this problem, which could not be done due to time restrictions. To explore the issue further, more multicenter studies are required on varied topics in Community Medicine. This will yield more evidence in support of improvement in students’ academic performance in this subject before suggestions can be made to introduce PBL and thus bring about curriculum changes.
Acknowledgments
We authors thank the MBBS students and faculty members of the Department of Community Medicine, Kasturba Medical College, Mangalore, India for their support and cooperation throughout this research.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Khoshnevisasl P, Sadeghzadeh M, Mazloomzadeh S, Hashemi Feshareki R, Ahmadiafshar A. Comparison of problem-based learning with lecture-based learning. Iran Red Crescent Med J. 2014;16:e5186. doi: 10.5812/ircmj.5186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katmandu, Nepal: WHO-SEARO Report of a Review Meeting of the Expert Group; 2010. [Last accessed on 2015 Jan 15]. World Health Organization. Improving the Teaching of Public Health at Undergraduate Level in Medical Schools — Suggested Guidelines. Available from: http://www.searo.who.int/entity/primary_health_care/documents/pch_sea_hsd_344.pdf . [Google Scholar]
- 3.New Delhi: MCI; 2012. [Last accessed on 2015 Jan 15]. Medical Council of India. Regulations on Graduate Medical Education. Available from: http://www.mciindia.org/tools/announcement/Revised_GME_2012.pdf . [Google Scholar]
- 4.Tyler I. Toronto: Association of Faculty of Medicine of Canada, Public Health Task Group; 2009. Strengths, Weaknesses and Applicability of Teaching Methods, Report 5. An Environmental Scan of Best Practices in Public Health Undergraduate Medical Education; p. 5. [Google Scholar]
- 5.Wood DF. Problem based learning. BMJ. 2003;326:328–30. doi: 10.1136/bmj.326.7384.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schwartz RW, Burgett JE, Blue AV, Donnelly MB, Sloan DA. Problem-based learning and performance-based testing: Effective alternatives for undergraduate surgical education and assessment of student performance. Med Teach. 1997;19:19–23. [Google Scholar]
- 7.Khan I, Fareed A. Problem based learning variant: Transition phase for a large Institution. J Pak Med Assoc. 2001;51:271–4. [PubMed] [Google Scholar]
- 8.Lieux EM. A comparative study of learning in lecture versus problem-based format. In: Dutch BJ, editor. About Teaching: A Newsletter of the Center for Teaching Effectiveness. Newark: University of Delaware; 1996. pp. 25–7. [Google Scholar]
- 9.Peters AS, Greenberger-Rosovsky R, Crowder C, Block SD, Moore GT. Long-term outcomes of the New Pathway Program at Harvard Medical School: A randomized controlled trial. Acad Med. 2000;75:470–9. doi: 10.1097/00001888-200005000-00018. [DOI] [PubMed] [Google Scholar]
- 10.Elizondo-Montemayor LL. Formative and summative assessment of the problem-based learning tutorial session using a criterion- referenced system. JIAMSE. 2004;14:8–14. [Google Scholar]
- 11.Shankar RP, Nandy A, Balasubramanium R, Chakravarty S. Small group effectiveness in a Caribbean medical school's problem-based learning sessions. J Educ Eval Health Prof. 2014;11:5. doi: 10.3352/jeehp.2014.11.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bloom's taxonomy. Learning Tech. [Last accessed on 2014 Mar 21]. Available from: http://www.learningtech.co.nz/blooms-taxonomy/
- 13.Shankar RP, Nandy A. Student feedback on problem-based learning processes. Australas Med J. 2014;7:522–9. doi: 10.4066/AMJ.2014.2208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meo SA. Evaluating learning among undergraduate medical students in schools with traditional and problem-based curricula. Adv Physiol Educ. 2013;37:249–53. doi: 10.1152/advan.00031.2013. [DOI] [PubMed] [Google Scholar]
- 15.Callis AN, McCann AL, Schneiderman ED, Babler WJ, Lacy ES, Hale DS. Application of basic science to clinical problems: Traditional vs. hybrid problem-based learning. J Dent Educ. 2010;74:1113–24. [PubMed] [Google Scholar]
- 16.Shamsan B, Syed AT. Evaluation of problem based learning course at College of Medicine, Qassim University, Saudi Arabia. Int J Health Sci (Qassim) 2009;3:249–58. [PMC free article] [PubMed] [Google Scholar]
- 17.Tayyeb R. Effectiveness of problem based learning as an instructional tool for acquisition of content knowledge and promotion of critical thinking among medical students. J Coll Physicians Surg Pak. 2013;23:42–6. [PubMed] [Google Scholar]
- 18.Prince KJ, van Eijs PW, Boshuizen HP, van der Vleuten CP, Scherpbier AJ. General competencies of problem-based learning (PBL) and non-PBL graduates. Med Educ. 2005;39:394–401. doi: 10.1111/j.1365-2929.2005.02107.x. [DOI] [PubMed] [Google Scholar]
- 19.AlHaqwi AI. Learning outcomes and tutoring in problem based-learning: How do undergraduate medical students perceive them? Int J Health Sci (Qassim) 2014;8:125–32. doi: 10.12816/0006078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Albanese MA, Mitchell S. Problem-based learning: A review of literature on its outcomes and implementation issues. Acad Med. 1993;68:52–81. doi: 10.1097/00001888-199301000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Blumberg P, Michael JA. Development of self-directed learning behaviors in a partially teacher-directed problem-based learning curriculum. Teach Learn Med. 1992;4:3–8. [Google Scholar]
- 22.Kaufman DM, Mann KV. Comparing students’ attitudes in problem-based and conventional curricula. Acad Med. 1996;71:1096–9. doi: 10.1097/00001888-199610000-00018. [DOI] [PubMed] [Google Scholar]
- 23.Yew EH, Schmidt HG. Evidence for constructive, self-regulatory, and collaborative processes in problem-based learning. Adv Health Sci Educ Theory Pract. 2009;14:251–73. doi: 10.1007/s10459-008-9105-7. [DOI] [PubMed] [Google Scholar]
- 24.Ding X, Zhao L, Chu H, Tong N, Ni C, Hu Z, et al. Assessing the effectiveness of problem-based learning of preventive medicine education in China. Sci Rep. 2014;4:5126. doi: 10.1038/srep05126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Al-Naggar RA, Bobryshev YV. Acceptance of problem based learning among medical students. J Community Med Health Educ. 2012;2:146. [Google Scholar]
- 26.Roberts C, Lawson M, Newble D, Self A, Chan P. The introduction of large class problem-based learning into an undergraduate medical curriculum: An evaluation. Med Teach. 2005;27:527–33. doi: 10.1080/01421590500136352. [DOI] [PubMed] [Google Scholar]
- 27.Chng E, Yew EH, Schmidt HG. Effects of tutor-related behaviours on the process of problem-based learning. Adv Health Sci Educ Theory Pract. 2011;16:491–503. doi: 10.1007/s10459-011-9282-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bate E, Hommes J, Duvivier R, Taylor DC. Problem-based learning (PBL): Getting the most out of your students - Their roles and responsibilities: AMEE Guide No. 84. Med Teach. 2014;36:1–12. doi: 10.3109/0142159X.2014.848269. [DOI] [PubMed] [Google Scholar]
- 29.Singaram VS, Van Der Vleuten CP, Van Berkel H, Dolmans DH. Reliability and validity of a Tutorial Group Effectiveness Instrument. Med Teach. 2010;32:e133–7. doi: 10.3109/01421590903480105. [DOI] [PubMed] [Google Scholar]
- 30.Singaram VS, Dolmans DH, Lachman N, van der Vleuten CP. Perceptions of problem-based learning (PBL) group effectiveness in a socially-culturally diverse medical student population. Educ Health (Abingdon) 2008;21:116. [PubMed] [Google Scholar]
- 31.Dolmans DH, Wolfhagen IH, van der Vleuten CP. Motivational and cognitive processes influencing tutorial groups. Acad Med. 1998;73(Suppl):S22–4. doi: 10.1097/00001888-199810000-00034. [DOI] [PubMed] [Google Scholar]
- 32.Kaufman DM, Mann KV. Comparing achievement on the Medical Council of Canada Qualifying Examination Part 1 of students in conventional and problem-based learning curricula. Acad Med. 1998;73:1211–3. doi: 10.1097/00001888-199811000-00022. [DOI] [PubMed] [Google Scholar]
- 33.Gurpinar E, Musal B, Aksakoglu G, Ucku R. Comparison of knowledge scores of medical students in problem-based learning and traditional curriculum on public health topics. BMC Med Educ. 2005;5:7. doi: 10.1186/1472-6920-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McParland M, Noble LM, Livingston G. The effectiveness of problem-based learning compared to traditional teaching in undergraduate psychiatry. Med Educ. 2004;38:859–67. doi: 10.1111/j.1365-2929.2004.01818.x. [DOI] [PubMed] [Google Scholar]
- 35.Azer SA. Introducing a problem-based learning program: 12 tips for success. Med Teach. 2011;33:808–13. doi: 10.3109/0142159X.2011.558137. [DOI] [PubMed] [Google Scholar]


