Abstract
Background:
The understanding of youth mental health needs and development of service delivery models is a national public health challenge.
Objectives:
The rates and predictors of emotional and behavioral problems among 1087 youth were assessed in a pre-university college in Bangalore, India. Variations in rates of disturbance, identified by using different cut-off points, were also examined.
Materials and Methods:
The Strengths and Difficulties Questionnaire was used as a self-report screening tool.
Results:
Results indicated that 10.1% of adolescents had total difficulty levels in the abnormal range, with 9% at risk for emotional symptoms, 13% for conduct problems, 12.6% for hyperactivity/inattention and 9.4% for peer problems. Select gender differences were present. Cut-off scores derived from the sample yielded lower estimates of disturbance than the published cut-offs. Regression analysis identified predictors of total difficulty levels.
Conclusions:
Implications for assessment of youth mental health and planning targeted services in educational institutions are discussed.
Keywords: Adolescents, emotional and behavioral difficulties, India, strengths and difficulties questionnaire, youth mental health
Introduction
Youth mental health needs are a growing concern in both developed and developing nations. Resource-poor countries, like India, have additional challenges of low awareness about mental disorders, stigma and scarcity of mental health professionals.(1) There are few studies on the prevalence and patterns of emotional and behavioral disturbances among Indian adolescents,(2,3,4,5,6,7,8) with the largest knowledge gaps for middle and late adolescence.
Although this developmental stage is marked by a range of potential stressors, help seeking rates in traditional mental health services tend to be low. Parents, teachers, school or college counsellors and other supportive adults need to be empowered to recognise and respond to emotional and behavioral difficulties among youth.
Brief, low-cost screening instruments, like the Strengths and Difficulties questionnaire, may help build a national database of youth mental health needs, beyond diagnosable psychiatric conditions.(9) However, there are some concerns about inaccurate estimates, particularly concerning cross-cultural variations in rating and in caseness indicators of the SDQ.(10) While some studies have used the original cut-off scores, others(11,12,13) have reported discrepancies in rates while using alternate cut-off points derived from their sample percentile distributions.
The present study was planned in the initial phase of a two-year Adolescent Mental Health and Suicide Prevention Teacher Training programme in an educational institution in Bangalore, India. It assessed the rates of vulnerable adolescents at risk for a range of emotional and behavioral difficulties in order to plan targeted training objectives and processes. Additionally, it examined the utility of a brief screening tool and compared the rates of adolescent problems using varied cut-off points.
Materials and Methods
Sample
Informed assent and consent for participation was sought from all 1336 students enrolled in a pre-university college, and their parents. The sample included 1087 male and female students enrolled in the first and second year of a pre-university college in Bangalore (81.4% participation rate). The the mean age was 16.4 years (SD = 0.83). There were more males than females (57.5% vs 42.5%). The sample was almost equally divided between the first and second year of pre-university college, with a slightly higher proportion of students from the Commerce stream (53.6% vs 46.4%). About 3/4th lived in nuclear families and the majority (63.2%) lived in an urban area. Paternal education levels tended to be higher than maternal education levels.
Tools
Sociodemographic data sheet
Relevant socio-demographic details were recorded. Perceptions of difficulties in the family domain; e.g. physical punishment, parental marital discord, death of a parent, excessive alcohol/drug use by a family member, financial difficulties in the family; were assessed in a yes/no format.
Strengths and Difficulties Questionnaire (SDQ)(14)
This 25 item behavioral screening questionnaire has a three point rating (not true, somewhat true, certainly true). Four problem scales; emotional symptoms, conduct problems, hyperactivity/inattention, peer relationship problems add to generate a total difficulties score (0-40). A fifth scale assesses positive aspects of prosocial behavior.
The original British cut-off points were derived by classifying approximately 10% of the normative sample with the most extreme scores in the “abnormal” banding, the next 10% in the “borderline” banding and the remaining 80% in the “normal” banding categories. Some studies in Europe, Asia and Africa have used scores above the 90th percentile of their samples to define the ‘abnormal’ group.(11,12,15,16) In the present study, it was planned to contrast rates calculated from using both the original cut-offs and the percentile scores derived from the study sample.
The SDQ has good psychometric properties in varied cultures and languages and demonstrated use in Indian studies.(7,17,18,19)
Procedure
Institutional ethical clearance was obtained and classroom administration was done after obtaining written parental consent and student assent.
Analysis
Individuals were considered to be in the abnormal range if the SDQ total difficulties score was above the 90th percentile for this data. Separate cut-off levels were estimated for males and females. Individuals scoring over the 92.5 percentile, on each of the SDQ subscales, were placed in the abnormal range for that domain.(12) Number (%) of individuals falling in the abnormal range using the UK cutoff(20) and the cut offs derived in this study are presented.
Analyses using t-tests and one-way ANOVAs identified independent variables to be considered in the multiple regression analyses (at P < 0.1), to identify predictors of total difficulties, from among twelve variables; gender, education and stream, type of family, residence of family, paternal and maternal education levels, presence of physical punishment by parent/s, parental marital discord, parental death, excessive alcohol/drug use by a family member, family financial difficulties.
Results
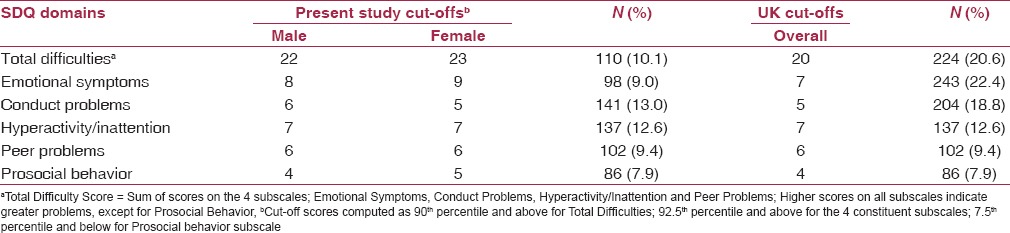
The cut-off scores derived from the percentile distribution of this study differed from that of the original UK cut-offs in select SDQ domains [Table 1]. The difference in the overall difficulties score cutoff was mainly due to the differences observed in domains of emotional symptoms (rate lowered from 22.4% to 9%) and conduct problems (rate lowered from 18.8% to 13%). The rates of hyperactivity/inattention, peer problems and prosocial behavior in the abnormal range were the same using the original cut-offs and the cut-off points derived from the study sample.
Table 1.
Percentage of abnormal scores on SDQ based on sample percentile cut-offs and UK percentile cut-offs
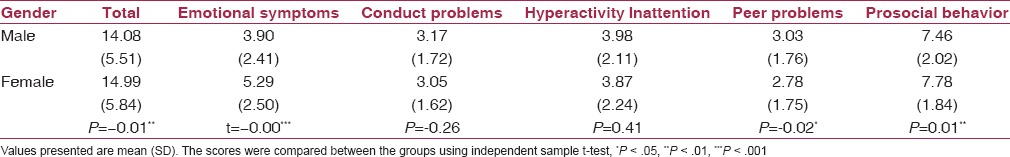
Findings related to gender differences indicated significantly higher levels of emotional symptoms and total problems among females [Table 2]. Males had significantly higher levels of peer problems and lower levels of prosocial behavior. There were no significant gender differences in the levels of self-reported conduct problems and hyperactivity/inattention.
Table 2.
Gender differences in SDQ total and subscale mean scores
Multiple regression analysis examined if the following nine variables significantly predicted the level of total problems on SDQ [Table 3]; gender, education level, education stream, maternal education level, presence of physical punishment by parent/s, parental marital discord, death of a parent, excessive alcohol/drug use by a family member, financial difficulties in the family.
Table 3.
Predictors of total difficulty levels on the SDQ
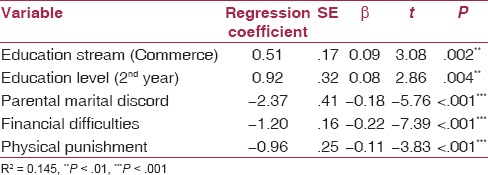
The results indicated that five predictors explained 14.5% of the variance (F = 20.61, P < .001) in total difficulty levels: Education stream (Commerce; β = 0.09; t = 3.08; P < .01); Education level (2nd year Pre-University; β = .08, t = 2.86, P < .01); presence of parental marital discord (β = −0.18, t = −5.76, P < .001), financial difficulties (β = −0.22; t = −7.39, P < .001) and parental physical punishment (β = −0.11; t = −3.83, P < .001).
Discussion
The study provides a snapshot of vulnerability among students from a pre-university college in Bangalore, with 10% of the sample at risk, with both internalizing (emotional) and externalizing (conduct) manifestations as prominent. The rates tended to be lower than those in other Indian studies using the SDQ.(4,7,17) At least partially, this could be due to the use of the original cut-offs in this group of studies. Goodman et al.(10) cautioned that SDQ tended to overestimate prevalence in low and middle-income countries, including India. In the present study, cut-offs derived from the percentile distribution of the sample were higher than the original cut-offs for total, emotional and conduct problems, resulting in lower rates in these domains.
The findings support the call for local and contextual knowledge and population specific norms when using screening tools like SDQ as an indicator for further exploration and follow-up.(14,21)
The present study identified gender differences in patterns of psychopathology among adolescents. Consonant with theoretical models(22) and other studies using the SDQ,(7,23,24,25) emotional symptoms were predominant among girls and peer problems among boys. Interestingly, in contrast to previous research, the present findings did not support the tilt towards higher conduct problems and hyperactivity among males. The reasons could include the subjective interpretations of the SDQ items in these domains and may also reflect the narrowing of the gender gap pertaining to conduct disorder in adolescence.(26) Clearly, college mental health programs must have a gender-informed perspective in early identification and intervention.
Within the sample, students in the Commerce stream and those in the second year, closer to their final examinations, were more at risk. Disturbed home environments can be a potent influence on youth mental health and both parental marital discord and corporal punishment have been linked with adolescent mental health trajectories.(22,27,28) The present study identified the triad of parental marital discord, financial difficulties in the family and physical punishment by parents as predictors of total difficulty levels. Overall, the findings suggest that comprehensive community-based youth mental health interventions must encompass family related vulnerabilities and find ways to engage and involve parents.
The study has inherent limitations in terms of a non-representative sample and the purposive sampling method in a single educational institution. The use of a single stage screening method and the absence of the impact supplement of the SDQ could result in inflated estimates of youth at risk. Future studies focused on identifying ‘caseness’ and planning service delivery could benefit from inclusion of the SDQ impact supplement, a second stage using standardised diagnostic interviews and the analysis of sensitivity and specificity. The importance of specificity would vary depending on the aim; Is the focus on identifying definite psychiatric ‘caseness’ or on exploring the magnitude of potential vulnerability among adolescents to plan a range of promotive and preventive inputs along intervention. Youth mental health initiatives in educational settings need to cover a spectrum of vulnerability and sensitive instruments, like the SDQ, tapping difficulties in the borderline and abnormal range, could help identify varied youth mental health needs.
The present study highlights the need to examine the psychometric properties of the SDQ in a larger, representative community sample of adolescents in India. ROC analysis could clarify the predictive validity of the SDQ, while confirmatory factor analysis could assess the proposed five factor structure of the tool.
Conclusion
The study focused on identifying potential mental health needs in an age band where there is scarce Indian literature and highlighted issues related to assessment methodologies. The findings have implications for understanding gender-specific vulnerabilities, family contextual variables and planning targeted youth mental health services.
Financial support and sponsorship
St. John's Medical College Research Society grant.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Ms. Rita Pledger for assistance in data entry.
Dr. Uma Devi, Principal. Seshadripuram P.U. College, Yelahanka, Bangalore for facilitating data collection in the college.
Dr. M.V. Ashok. St. John's Medical College and Hospital, Bangalore, for his support.
References
- 1.Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: A global public-health challenge. Lancet. 2007;369:1302–13. doi: 10.1016/S0140-6736(07)60368-7. [DOI] [PubMed] [Google Scholar]
- 2.Bansal V, Goyal S, Srivastava K. Study of prevalence of depression in adolescent students of a public school. Ind Psychiatry J. 2009;18:43–6. doi: 10.4103/0972-6748.57859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhola P, Kapur M. Child and adolescent psychiatric epidemiology in India. Indian J Psychiatry. 2003;45:208–17. [PMC free article] [PubMed] [Google Scholar]
- 4.Dhoundiyal M, Venkatesh R. The psychological world of adolescence: A comparative evaluation between rural and urban girls. Indian J Psychol Med. 2009;31:35–8. doi: 10.4103/0253-7176.53313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Muzammil K, Kishore S, Semwal J. Prevalence of psychosocial problems among adolescents in district Dehradun, Uttarakhand. Indian J Public Health. 2009;53:18–21. [PubMed] [Google Scholar]
- 6.Pillai A, Patel V, Cardozo P, Goodman R, Weiss HA, Andrew G. Non-traditional lifestyles and the prevalence of mental disorders in young adolescents in a community in India. Br J Psychiatry. 2008;192:45–51. doi: 10.1192/bjp.bp.106.034223. [DOI] [PubMed] [Google Scholar]
- 7.Bharath Kumar Reddy KR, Biswas A, Rao H. Assessment of mental health of Indian adolescents studying in urban schools. [Last accessed on 2013 Sep 25];Malaysian J Paediatr Child Health. 2011 17 Retrieved from http://mjpch.com/index.php/mjpch/article/view/276/193 . [Google Scholar]
- 8.Srinath S, Girimaji SC, Gururaj G, Sheshadri S, Subbakrishna DK, Bhola P, et al. Epidemiological study of Child and adolescent psychiatric disorders in urban and rural areas of Bangalore, India. Indian J Med Res. 2005;122:67–79. [PubMed] [Google Scholar]
- 9.Sharan P, Sagar R. The need for national data on epidemiology of child and adolescent mental disorders. J Indian Assoc Child Adolesc Ment Health. 2008;4:22–7. [Google Scholar]
- 10.Goodman A, Heiervang E, Fleitlich-Bilyk B, Alyahri A, Patel V, Mullick MS, et al. Cross-national differences in questionnaires do not necessarily reflect comparable differences in disorder prevalence. Soc Psychiatry Psychiatr Epidemiol. 2012;47:1321–31. doi: 10.1007/s00127-011-0440-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alavi A, Mohammadi MR, Mahmoudi MD, Tehranidost M, Shahrivar Z, Sadaat S. The Farsi version of the Strengths and Difficulties Questionnaire Self-report form. The normative data and psychometric properties. Iran J Child Neurol. 2009;2:27–34. [Google Scholar]
- 12.Du Y, Kou J, Coghill D. The validity, reliability and normative scores of the parent, teacher and self-report versions of the Strengths and Difficulties Questionnaire in China. Child Adolesc Psychiatry Ment Health. 2008;2:8. doi: 10.1186/1753-2000-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Woerner W, Becker A, Rothenberger A. Normative data and scale properties of the German parent SDQ. Eur Child Adolesc Psychiatry. 2004;13(Suppl 2):II3–10. doi: 10.1007/s00787-004-2002-6. [DOI] [PubMed] [Google Scholar]
- 14.Goodman R, Meltzer H, Bailey V. The strengths and difficulties questionnaire: A pilot study on the validity of the self-report version. Eur Child Adolesc Psychiatry. 1998;7:125–30. doi: 10.1007/s007870050057. [DOI] [PubMed] [Google Scholar]
- 15.Kashala E, Elgen I, Sommerfelt K, Tylleskar T. Teacher ratings of mental health among school children in Kinhasa, Democratic Republic of Congo. Eur Child Adolesc Psychiatry. 2005;14:208–15. doi: 10.1007/s00787-005-0446-y. [DOI] [PubMed] [Google Scholar]
- 16.Vaage AB, Thomsen PH, Rousseau C, Wentzel-Larsen T, Ta TV, Hauff E. Paternal predictors of the mental health of children of Vietnamese refugees. Child Adolesc Psychiatry Ment Health. 2011;5:2. doi: 10.1186/1753-2000-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bele SD, Bodhare TN, Valsangkar S, Saraf A. An epidemiological study of emotional and behavioral disorders among children in an urban slum. Psychol Health Med. 2013;18:223–32. doi: 10.1080/13548506.2012.701751. [DOI] [PubMed] [Google Scholar]
- 18.Malhotra S, Kohli A, Kapoor M, Pradhan B. Incidence of child psychiatric disorders in India. Indian J Psychiatry. 2009;51:101–7. doi: 10.4103/0019-5545.49449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Srikala B, Kishore KK. Empowering adolescents with life skills education in schools-School mental health program: Does it work? Indian J Psychiatry. 2010;52:344–9. doi: 10.4103/0019-5545.74310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goodman R. The extended version of the Strengths and Difficulties Questionnaire as a guide to child psychiatric caseness and consequent burden. J Child Psychol Psychiatry. 1999;40:791–9. [PubMed] [Google Scholar]
- 21.Vostanis P. Strengths and difficulties questionnaire: Research and clinical applications. Curr Opin Psychiatry. 2006;19:367–72. doi: 10.1097/01.yco.0000228755.72366.05. [DOI] [PubMed] [Google Scholar]
- 22.Zahn-Waxler C, Shirtcliff EA, Marceau K. Disorders of childhood and adolescence: Gender and psychopathology. Annu Rev Clin Psychol. 2008;4:275–303. doi: 10.1146/annurev.clinpsy.3.022806.091358. [DOI] [PubMed] [Google Scholar]
- 23.Greally P, Kelleher I, Murphy J, Cannon M. Assessment of the mental health of Irish adolescents in the community. RCSI Student Med J. 2010;3:33–5. [Google Scholar]
- 24.Svedin CG, Priebe G. The strengths and difficulties questionnaire as a screening instrument in a community sample of high school seniors in Sweden. Nord J Psychiatry. 2008;62:225–32. doi: 10.1080/08039480801984032. [DOI] [PubMed] [Google Scholar]
- 25.Van Roy B, Grøholt B, Heyerdahl S, Clench-Aas J. Self-reported strengths and difficulties in a large Norwegian population 10-19 years: Age and gender specific results of the extended SDQ-questionnaire. Eur Child Adolesc Psychiatry. 2006;15:189–98. doi: 10.1007/s00787-005-0521-4. [DOI] [PubMed] [Google Scholar]
- 26.4th ed. Washington, DC: American Psychiatric Association; 2008. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 27.Bender HL, Allen JP, McElhaney KB, Antonishak J, Moore CM, Kelly HO, et al. Use of harsh physical discipline and developmental outcomes in adolescence. Dev Psychopathol. 2007;19:227–42. doi: 10.1017/S0954579407070125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Merikangas KR, Nakamura EF, Kessler RC. Epidemiology of mental disorders in children and adolescents. Dialogues Clin Neurosci. 2009;11:7–20. doi: 10.31887/DCNS.2009.11.1/krmerikangas. [DOI] [PMC free article] [PubMed] [Google Scholar]


