Abstract
Anthropometry involves the external measurement of morphologic traits of human beings. High quality anthropometric measurements are fundamental to clinical and epidemiological research. The measurements for each method have inherent variations, either due to biologic variation or due to error in measurement. Errors in measurement cannot be avoided completely but they can be minimized to a large extent. We define methods to estimate measurement error in anthropometry, offer guidelines for acceptable error, and suggest ways to minimize measurement error; thereby improving anthropometry quality in health assessments. We propose that special attention be paid to the following six key parameters for quality assurance of anthropometric measurements: (i) Identification of certified lead anthropometrist and trainer, (ii) manual of standard operating procedures, (iii) choice of robust equipment, (iv) equipment calibration, (v) standardization training and certification, and (vi) measurements resampling.
Keywords: Anthropometry, accuracy, epidemiologic studies, quality control
High quality anthropometric measurements are fundamental to clinical and epidemiological research. With the ‘epidemiologic transition’ from communicable to noncommunicable diseases (NCDs) underway in India as in several other ‘late-industrializing’ countries,(1,2) there has been a rollout of a National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular Disease, and Stroke (NPCDCS) initially across a selected subset of 620 districts spread over almost all states by the Indian government,(3) and also concomitant interest in national surveillance(4,5,6) as well as research(7) on NCDs and their risk factors over the last decade;(8,9,10,11,12) all of which involve anthropometric measurements.
Anthropometry involves the external measurement of morphologic traits of human beings(13) and may include height, weight, circumferences, skin fold thickness, and several other measurements.(14) These anthropometric measurements have an important place in management of both communicable and NCDs.
The measurements for each method have inherent variations, either due to biologic variation or due to error in measurement.(15,16) The extent to which measurement error can affect measurement or the interpretation of health status is less emphasized.(13) Further, differential measurement errors may also affect computed indices using more than one measurement, for example, body mass index, waist-hip ratio, etc. So while there are standard tools such as World Health Organization STEP wise approach to Surveillance (WHO-STEPS) for use of anthropometry in research studies, there is insufficient easily available guidance literature on measurement errors and ways to assure quality in measurements. In this communication, we define methods to estimate measurement error in anthropometry, offer guidelines for acceptable error, and suggest ways to minimize measurement error; thereby improving anthropometry quality in health assessments.
Types of Errors
There are potentially two types of errors in anthropometry; those linked to:
Repeated measures giving the same value (reliability) and
Measurements departing from true values (accuracy or bias).(13)
Reliability has two components: Precision and dependability.(17) Precision is the consistency between repeated measurements over time, while dependability refers to the physiological fluctuation within the individual. Accuracy is the extent to which the ‘true’ value of a measurement is attained. While random errors affect the reliability of measurements, inaccuracy is due to systematic bias. Reliability is influenced by observer-related issues (e.g., inconsistency in locating landmarks or applying pressure to the instrument) as well as subject-related issues (e.g., due to respiration or change of posture). Inaccuracy may be due to instrument error or to errors of measurement technique.
Measurement of Error and Acceptable Levels of Measurement Error
Attention to quality control involves the measurement of the magnitude of these errors. Imprecision may be estimated by carrying out repeated measures on the same subjects and calculating one or more of the following: Technical error of measurement (TEM), % TEM, reliability coefficient (R), or intraclass correlation coefficient (ICC).(13,14,16,18)
When a measurement is taken on the same individual more than once, the value obtained each time will not be the same; this produces what is called the ‘technical error of measurement’. This most commonly used measure is essentially the standard deviation between repeated measures. Ulijaszek and Kerr show that the calculations for intra- and interobserver error are the same.(13) Intraobserver TEM between two measurements and interobserver TEM between two measurers is obtained by:
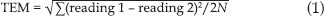
where N is the number of participants measured. When more than two measurers are involved,

where N is the number of participants, K is the number of measurers, and M is the measurement. The units of TEM are the same as the units of the measurement under consideration.(13) An example calculation of TEM from measurements of hip circumference made by four observers is shown in Table 1 with the step-wise calculations for ∑1KM2, (∑1KM)2/K, the difference between the two, the sum of these differences, and then the TEM. In this example, the TEM is 2.71 cm.
Table 1.
Sample calculation of technical error of measurement (TEM) for hip circumference measurements taken by four measurers on a set of 10 volunteers
However, the size of the TEM is positively associated with the size of the measurement. Hence, this is sometimes converted into a relative TEM (%TEM) = (TEM/mean)*00. This is a measure of coefficient of variation (CV), which has no units and allows direct comparison of all types of anthropometric measures.
R has not been used widely and so values to which measurers must strive to attain are largely unknown unlike the other parameters.
Acceptable levels of measurement error
Lower the TEM, better the reliability. For trainee anthropometrists, the acceptable intraobserver range of TEM is <1 mm (for skinfolds) and <1 cm for circumferences; the acceptable interobserver range of TEM is 1-2 mm for skinfolds, <1 cm for arm and waist circumferences, and 1-2 cm for hip and thigh circumferences. In terms of % TEM, the acceptable intraobserver range of TEM is <1.5%, while interobserver is <2%.(16) Absolute values of acceptable TEM listed absolute are used both as training targets and in dissemination of study results.
Requirements For High Quality Measurements
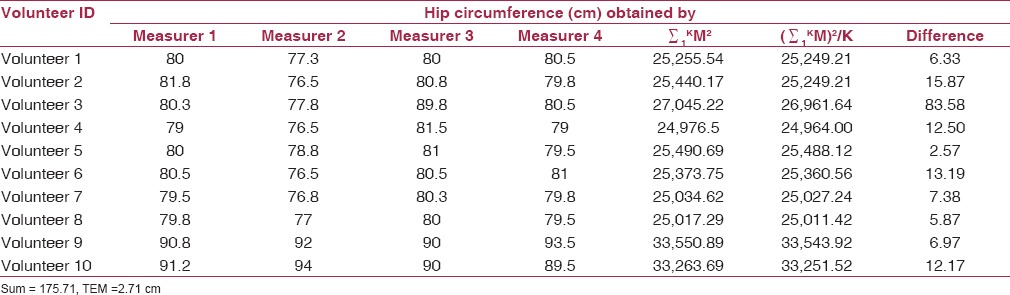
Errors in measurement cannot be avoided completely, but they can be minimized to a large extent. We propose that investigators pay special attention to following a quality assurance protocol comprising of six key steps for anthropometric measurements as depicted in the conceptual framework in Figure 1.
Figure 1.
Conceptual framework for a quality assurance protocol in anthropometric measurements
Certified lead anthropometrist andtrainer
Manual of standard operating procedures
Robust equipment
Equipment calibration
Standardization training andcertification
Resampling (about 5-10%)
Certified Lead Anthropometrist and Trainer
The first step is to have a lead certified anthropometrist-cum-trainer on the team. This trainer can be certified against an existing lead anthropometrist from the same or another institution. If there is no access against another lead anthropometrist, an individual with practice of anthropometric and/or physiologic measurements can be identified and certified by attaining a reproducibility (= repeatability around the mean value) of ± 2% for circumference measurements and ± 10% for skin fold thickness measurements.(19) Skilled anthropometrists can obtain almost similar values even if the individual is obese.(20)
Manual of Standard Operating Procedures
Next step is to standardize the training for all identified trainees using a measurements training manual. This may be adapted from an existing standard training manual(21,22,23) to serve as standard operating procedures for several critical steps before, during, and after measurement. Sometimes a study-specific manual may be prepared by collating points from several of these manuals. Critical issues include: Site selection in the clinic/household, preparation/positioning of the instrument, instructions to the participant and positioning/maneuvering of participant, identification of body landmarks, application and reading of the instrument, and recording of the measurements. Several decisions also need to be taken regarding options such as:
Precision up to decimal, or rounding-off of digits;
Taking two or three readings and calculating average of two, three, or last two readings;
Site of measurement, that is, left/right or dominant/nondominant side of the body. Avoidance of common errors such as measuring waist circumference at the level of the umbilicus which underestimates the measurement is also critical.(17,24,25)
Robust equipment
The right decisions need to be made prior to the start of the project regarding choice of robust instruments that would have the precision required for the project objectives and that would be appropriate for facility- or community-based use as required. For example, the precision of the Holtain calipers is 0.2 mm, while that of the Lange calipers is 0.5 mm. Further, these equipment need to be well-maintained and stored appropriately when not in use.
Equipment Calibration
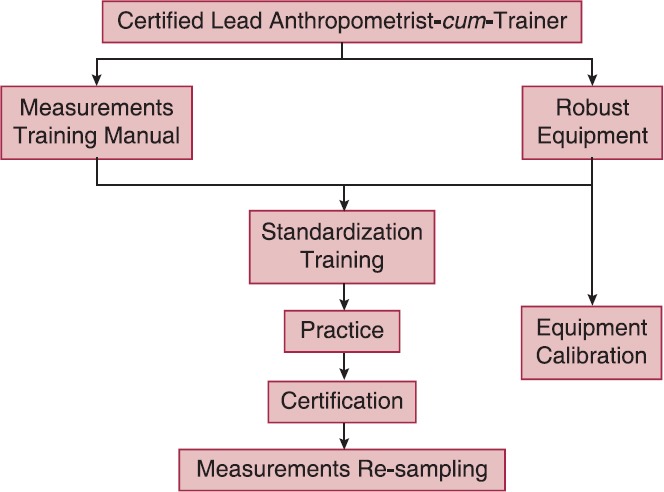
Routine calibration of instruments ensures accurate results by the equipment. Weighing scales, stadiometers, and skin fold calipers should be calibrated. For example, adult weighing scales are calibrated using standard International Organization for Standardization (ISO) certified weights starting from 10 kg. In addition, we also recommend calibration at multiple (at least three to determine linearity) points across the range of expected measurements; if linear, single point calibrations may be sufficient subsequently (for instance, for a health survey of middle-aged adults with expected weights across the range of 30-80 kg, calibration may need to be done at three different points −30, 50, and 80 kg weights). Table 2 illustrates an example for 10 and 20 kg standard weights as measured by two different scales; it is apparent that scale 1 has a systematic bias of +0.2 kg across the range tested; it needs to be noted that this can be corrected for.
Table 2.
Sample equipment calibration sheet for adult weighing scale
Calibration is done as soon as the equipment is purchased and then routinely at weekly intervals. Measurements are recorded and checked for accuracy each time. This also ensures that faulty equipment are quickly identified and replaced.
Standardized Measurement Training, Practice, and Certification
All field personnel who take the anthropometric measurements have to undergo standardization training. A standard manual(21) must be used in the training and certification of workers; it includes test forms, recording sheet, exercises, and criteria for evaluation.
Following standardization training, all trainees must be given opportunity to practice measurements on a set of volunteers (preferably a few dozen over a few days), in both classroom setting and in the field/real-life setting. Practice measurements may initially be under direct supervision by the trainer.
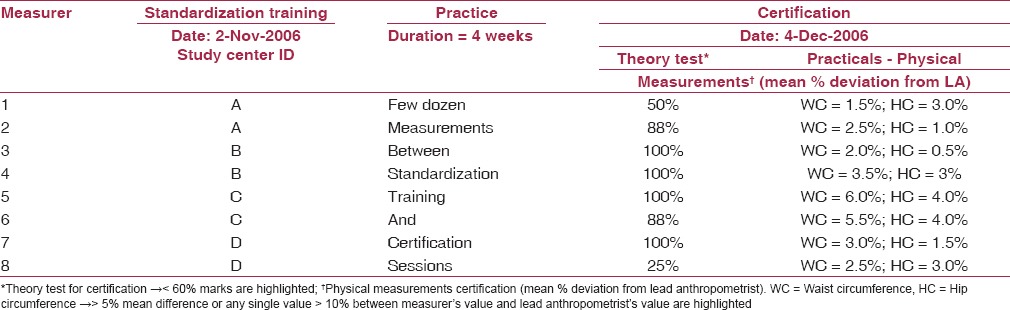
This should be followed by a certification session with the arrangement of volunteers (at least 10), requisite number of equipment and time allocation for measurement, grading, and feedback. For this testing, all measurements are conducted on the same set of subjects by all field personnel and certified against the lead anthropometrist. A CV of <5% is acceptable to be certified.(21) Additionally, TEM as explained above are also used for certification of fieldworkers.(13) A sample report of the certification program is shown in Table 3 for feedback and refresher training. Only certified personnel should be authorized to conduct measurements on field. Periodic retraining and certification (at 12-monthly intervals) is also an important requirement to optimize quality control. Advanced data management includes the identification of the measurer by a unique identifier code on the database so that analyses of interobserver variations can be done post-hoc once the data has been collected.
Table 3.
Sample report of certification of measurers against lead anthropometrist (LA)
Resampling of individuals
Resampling in anthropometric measurements involves subsampling from the original sample for repeat testing of some or all of the anthropometric measurements by a different measurer. The basic mechanism by which this is accomplished is for the investigator to allot a subsample of individuals to be remeasured (e.g., weight/circumference) by a second measurer from another area and who is blinded to these values. For instance, if there are three measurers A, B, and C; then on one specified day of the week, measurer A would go to measurer B's area, measurer B would go to measurer C's area, and measurer C would go to measurer A's area. The objective of this strategy is to ensure quality control for managerial purpose rather than for any statistical purpose (such as regression to the mean). A few points to bear in mind are:
That the original sample must preferably be representative,
Resampling should be a rare event (~5%), and
It should be performed by the same set of qualified staff using the same calibrated equipment and the same validated methods as used for the initial sample.
Conclusion
Investing in the time, effort, and personnel needed for the implementation of such a quality assurance protocol is likely to have three intended benefits. Firstly, adherence to the various steps of this protocol constituting ‘good epidemiologic practice’ (GEP) will promote an ‘environment of quality assurance’ among the study personnel within the anthropometric assessment scenario in study settings. Secondly, by minimizing threats to quality at the data collection stage, it is likely to enhance the ‘internal validity’ of the anthropometric assessments, thus assuring investigators that they are indeed measuring what they intend.(26) Lastly, if investigators report the magnitude and direction of measurement error (as coefficient of variation or as TEM) in addition to describing anthropometric measurement details, it would assist in comparability across studies.
In summary, we have defined measurement error, demonstrated key calculations, identified acceptable levels of measurement, and outlined certain critical steps to assuring quality in anthropometric measurements. It is known that there is a clear hierarchy in the precision of anthropometric measurements—with height and weight measurements being most precise, circumference measurements’ precision being intermediate with proneness to inter-observer error, and skinfolds being the most problematic.(13) An understanding of presence of measurement error along with planning for a few critical steps such as rigorous adherence to a standard protocol which includes resampling, choice of robust equipment with frequent calibration, standardized training(17) by a certified anthropometrist, followed by practice and certification of all workers with (i) deviation from lead anthropometrist(21) and (ii) the TEM,(13) being within acceptable limits; should help ensure quality in improving validity of anthropometric measurements in health assessments.
PS: A copy of the equipment calibration sheet, and the simple Excel spreadsheets for certification (using deviation from lead anthropometrist and using TEM) can be obtained by writing to the lead author.
Footnotes
Source of Support: Nil
Conflicts of Interest: None declared.
References
- 1.Ezzati MH, Hoorn SV, Lopez AD, Danaei G, Rodgers A, Mathers CD, et al. Comparative quantification of mortality and burden of disease attributable to selected risk factors. In: Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL, editors. Global Burden of Disease and Risk Factors. Washington: The World Bank; 2006. pp. 241–395. [PubMed] [Google Scholar]
- 2.New Delhi: Office of the Registrar General of India; 2009. RGI-CGHR Collaborators. Report on the Causes of Death in India: 2001-2003; pp. 10–52. [Google Scholar]
- 3.Directorate General of Health Services, Ministry of Health and Family Welfare. National Programme for Prevention and Control of Cancer, Diabetes, CVD and Stroke (NPCDCS): Operational Guidelines. [Last cited on 2011 August 28]. Available from: http://health.bih.nic.in/docs/guidelines-npcdcs.pdf .
- 4.I. Mumbai: IIPS and Macro International; 2007. International Institute for Population Sciences (IIPS). National Family Health Survey (NFHS-3), 2005-06: India. [Google Scholar]
- 5.WHO India-ICMR. NCD RF surveillance 2003-04. Report of the surveillance of risk factors of non-communicable diseases (STEPS 1 and 2) from 5 centres in India. [Last cited on 2010 Sept 8]. Available from: http://www.whoindia.org/linkfiles/ncd_surveillance_ncd_rf_surveillance_report.pdf .
- 6.New Delhi: National Institute of Medical Statistics and Indian Council of Medical Research; 2009. National Institute of Medical Statistics (ICMR). IDSP Non-Communicable Disease Risk Factors Survey, Phase-I States of India, 2007-08; pp. 15–87. [Google Scholar]
- 7.Mony PK, Srinivasan K. A bibliometric analysis of published non-communicable disease research in India. Indian J Med Res. 2011;134:232–4. [PMC free article] [PubMed] [Google Scholar]
- 8.Reddy KS, Prabhakaran D, Chaturvedi V, Jeemon P, Thankappan KR, Ramakrishnan L, et al. Methods for establishing a surveillance system for cardiovascular diseases in Indian industrial populations. Bull World Health Organ. 2006;84:461–9. doi: 10.2471/blt.05.027037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jha P, Gajalakshmi V, Gupta PC, Kumar R, Mony P, Dhingra N, et al. Prospective study of one million deaths in India: Rationale, design, and validation results. PLoS Med. 2006;3:e18. doi: 10.1371/journal.pmed.0030018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Teo K, Chow CK, Vaz M, Rangarajan S, Yusuf S. The Prospective Urban Rural Epidemiology (PURE) study: Examining the impact of societal influences on chronic noncommunicable diseases in low-, middle-, and high-income countries. Am Heart J. 2009;158:1–7. doi: 10.1016/j.ahj.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 11.Ebrahim S, Kinra S, Bowen L, Andersen E, Ben-Shlomo Y, Lyngdoh T, et al. The effect of rural-to-urban migration on obesity and diabetes in India: A cross-sectional study. PLoS Med. 2010;7:e1000268. doi: 10.1371/journal.pmed.1000268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gupta R, Guptha S, Gupta VP, Agrawal A, Gaur K, Deedwania PC. Twenty-year trends in cardiovascular risk factors in India and influence of educational status. Eur J Cardiovasc Prev Rehabil. 2011;26 doi: 10.1177/1741826711424567. [DOI] [PubMed] [Google Scholar]
- 13.Ulijaszek SJ, Kerr DA. Anthropometric measurement error and the assessment of nutritional status. Br J Nutr. 1999;82:165–77. doi: 10.1017/s0007114599001348. [DOI] [PubMed] [Google Scholar]
- 14.Kouchi M, Mochimaru M, Tsuzuki K, Yokoi T. Random errors in anthropometry. J Hum Ergol. 1996;25:155–66. [PubMed] [Google Scholar]
- 15.Guo SS, Siervogel RM, Chumlea WC. Epidemiological applications of body composition. The effects and adjustment of measurement errors. Ann N Y Acad Sci. 2000;904:312–6. doi: 10.1111/j.1749-6632.2000.tb06473.x. [DOI] [PubMed] [Google Scholar]
- 16.Goto R, Mascie-Taylor CG. Precision of measurement as a component of human variation. J Physiol Anthropol. 2007;26:253–6. doi: 10.2114/jpa2.26.253. [DOI] [PubMed] [Google Scholar]
- 17.Mueller WH, Martorell RT, Lohman T, Roche AF, Martorell R. Reliability and accuracy of measurement. In: Lohman T, Roche AF, Martorell R, editors. Anthropometric Standardization Reference Manual. Champaign: Human Kinetics Books; 1988. pp. 83–6. [Google Scholar]
- 18.Marks GC, Habicht JP, Mueller WH. Reliability, dependability, and precision of anthropometric measurements. The Second National Health and Nutrition Examination Survey 1976-1980. Am J Epidemiol. 1989;130:578–7. doi: 10.1093/oxfordjournals.aje.a115372. [DOI] [PubMed] [Google Scholar]
- 19.Wang J, Thornton JC, Kolesnik S, Pierson RN., Jr Anthropometry in body composition. An overview. Ann N Y Acad Sci. 2000;904:317–26. doi: 10.1111/j.1749-6632.2000.tb06474.x. [DOI] [PubMed] [Google Scholar]
- 20.Heyward V, Wagner D. 2nd ed. Champaign: Human Kinetics Publishers Inc; 2004. Applied Human Body Composition Assessment; pp. 90–155. [Google Scholar]
- 21.Zerfas AJ. Los Angeles: Division of Epidemiology, School of Public Health, UCLA; 1985. Checking continuous measures. Manual for Anthropometry; pp. 1a–20b. [Google Scholar]
- 22.Rockville: Westat Inc; 1988. National Health and Nutrition Examination Survey (NHANES) III. Body Measurements (Anthropometry) pp. 1–38. [Google Scholar]
- 23.WHOMONICA Manual. Part III: Population Survey. Section 1: Population Survey Data Component. [Last cited on 2006 May 20]. Available from http://www.ktl.fi/publications/monica/manual/part3/iii-1htm # s4-6 .
- 24.Croft JB, Keenan NL, Sheridan DP, Wheeler FC, Speers MA. Waist-to-hip ratio in a biracial population: measurement, implications, and cautions for using guidelines to define high risk for cardiovascular disease. J Am Diet Assoc. 1995;95:60–4. doi: 10.1016/S0002-8223(95)00014-3. [DOI] [PubMed] [Google Scholar]
- 25.Geneva: WHO; 2011. World Health Organization. Waist circumference and waist-hip ratio: Report of a WHO expert consultation; pp. 5–20. [Google Scholar]
- 26.Rothman KJ, Greenland S, Lash TL. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2008. Modern Epidemiology; pp. 128–47. [Google Scholar]


