Abstract
Background. We examined the influenza vaccine effectiveness (VE) during the 2013–2014 influenza season, in which 2009 pandemic influenza A(H1N1) virus (influenza A[H1N1]pdm09) predominated. In 2 previous years when influenza A(H3N2) virus predominated, the VE was low and negatively affected by prior year vaccination.
Methods. We enrolled and followed 232 households with 1049 members, including 618 children; specimens were collected from subjects with acute respiratory illnesses. The VE in preventing laboratory-confirmed influenza A(H1N1)pdm09 infection was estimated in adjusted models. Preseason hemagglutination-inhibition and neuraminidase-inhibition antibody titers were determined to assess susceptibility.
Results. Influenza A(H1N1)pdm09 was identified in 25 households (10.8%) and 47 individuals (4.5%). Adjusted VE against infection with influenza A(H1N1)pdm09 was 66% (95% confidence interval [CI], 23%–85%), with similar point estimates in children and adults, and against both community-acquired and household-acquired infections. VE did not appear to be different for live-attenuated and inactivated vaccines among children aged 2–8 years, although numbers were small. VE was similar for subjects vaccinated in both current and prior seasons and for those vaccinated in the current season only; susceptibility titers were consistent with this observation.
Conclusions. Findings, including substantial significant VE and a lack of a negative effect of repeated vaccination on VE, were in contrast to those seen in prior seasons in which influenza A(H3N2) virus predominated.
Keywords: influenza, vaccine effectiveness, households with children, serologic susceptibility
Annual assessments of influenza vaccine effectiveness (VE) are now regularly conducted in part to recognize and explain patterns in year-to-year variation. Evaluations are typically observational and estimate the VE in preventing medically attended, laboratory-confirmed influenza. In the United States, members of the US Influenza Vaccine Effectiveness Network have collaborated annually to estimate VE in the healthcare setting, with enrollment of patients seeking care for acute respiratory illnesses at ambulatory care facilities [1–4]. These and other similar studies use the case test-negative design to estimate VE, comparing vaccination frequencies in those with and those without laboratory-confirmed influenza [5, 6].
It is recognized that any observational assessment of VE could be affected by a variety of factors, especially recognition of only medically attended illnesses [7, 8]. Alternative approaches to effectiveness estimation are valuable in supplying additional information. Since the 2010–2011 influenza season, we have conducted a complementary study of respiratory virus transmission and influenza VE in households with children [9–12]. Each study year, the cohort of households is defined in advance of the respiratory illness season and followed through the fall and winter. This strategy allows examination of symptomatic respiratory illnesses of any severity, using an alternative design and statistical approach. The VEs in preventing community-acquired influenza and, separately, household-acquired influenza among subjects known to have been exposed, are assessed. Results from our household study in the 2010–2011 and 2012–2013 seasons indicated a lower VE than demonstrated in studies performed in healthcare settings during the same seasons and lower effectiveness point estimates with repeated annual vaccination [9, 10]. The latter finding, novel at the time, was confirmed subsequently [3, 4]. Serologic susceptibility assessments, added to our household study in the 2012–2013 season, indicated that prior vaccination appeared to modify VE by both residual protection and reduced response to vaccination [10].
In both of these study years, influenza A(H3N2) virus predominated, and the focus of VE estimates and serologic studies was limited to that influenza virus subtype, with less emphasis on influenza B virus [9, 10]. Circulation of 2009 pandemic influenza A(H1N1) virus (influenza A[H1N1]pdm09) was limited in both study years, and estimating VE against this subtype was not possible. In fact, until the 2013–2014 season, when circulation of influenza A(H1N1)pdm09 predominated, this subtype had circulated only minimally in the United States since 2009 [13]. In addition, based on little evidence of antigenic drift among circulating influenza A(H1N1)pdm09 strains during those years and continuing through at least the 2015–2016 season, the influenza A(H1N1)pdm09 component of the licensed vaccines has not changed from the strain (A/California/7/2009[H1N1]pdm09-like virus) selected for the monovalent vaccine during the pandemic [13, 14]. Here, we extend our evaluations of VE in households with children during the 2013–2014 season with estimates focused on prevention of influenza A(H1N1)pdm09 infection outcomes. Included are serologic assessments of vaccine response and preseason susceptibility, based on measurement of antibody to both the viral hemagglutinin (HA) and neuraminidase (NA) surface antigens [15, 16].
METHODS
Recruitment and Enrollment
Households were derived from persons who had selected a primary healthcare provider from the University of Michigan Health System in Ann Arbor. Eligible households (shared residence) were composed of at least 4 participating members, of whom at least 2 were children (ie, aged <18 years). At enrollment visits performed from June through September 2013, adult household members provided written informed consent for participation for themselves and their children, and children aged 7–17 years provided their oral assent. Demographic data were reported, and study access to health system medical records was granted. All study contacts, including enrollment, blood collection, and illness visits, were performed at the research study site at the University of Michigan School of Public Health (UM-SPH). The study was reviewed and approved by the institutional review board at the University of Michigan Medical School.
Respiratory Illness Surveillance and Laboratory Testing
Surveillance was performed from October 2013 through early May 2014. Households were instructed at enrollment and via weekly email reminders to report all acute respiratory illnesses in which ≥2 of the following symptoms were present: cough, fever or feverishness, nasal congestion, chills, headache, body aches, and/or sore throat. Subjects with eligible illnesses had combined throat and nasal swab specimens (or, for children aged <3 years, a nasal swab specimen only) collected at an illness visit within 7 days of illness onset. Illnesses were followed for collection of data on whether the subject sought medical attention; healthcare contact for illness treatment was also documented based on medical record review.
Respiratory tract specimens were tested for influenza virus by real-time reverse transcription polymerase chain reaction (RT-PCR) in the investigators' laboratory at the UM-SPH. The RT-PCR primers, probes, and testing protocol were developed and provided by the Influenza Division of the Centers of Disease Control and Prevention and designed for universal detection of influenza A and B viruses, plus subtypes of influenza A virus and lineage determination of influenza B viruses.
Blood Specimen Collection and Serologic Processing
Blood specimens were collected from participants aged ≥13 years who volunteered to have a single tube of blood collected at summer enrollment visits and again at scheduled visits before the influenza season (ie, during late fall). Sera from collected specimens were tested with the hemagglutination-inhibition (HAI) assay, using as a target the influenza A(H1N1)pdm09 strain (A/California/7/2009 pdm09-like virus) present in the 2013–2014 North American influenza vaccine [15]. Sera were also tested with the neuraminidase (NA)–inhibition (NAI) assay, using as the target a reassortant influenza virus (kindly provided by M. Eichelberger, Food and Drug Administration) with the NA representing the A(H1N1)pdm09 vaccine strain and a mismatched hemagglutinin (HA; H6 subtype), to avoid interference by HA-specific antibodies [16]. Serologic testing was performed in the investigators' laboratory at the UM-SPH.
Statistical Analyses
Households were characterized by size and composition, and subjects were characterized by demographic factors, high-risk health status, and influenza vaccination status. Health system medical records were reviewed to document the presence of health conditions considered to confer a high risk for complications of influenza [17]. Household members made their own decisions regarding vaccination; documentation of influenza vaccine receipt (for both the current and prior seasons) was based on evidence in medical records or the Michigan Care Improvement immunization registry. Associations of subject characteristics with vaccination status and influenza outcomes were examined and compared using χ2 or Fisher exact tests.
Cox proportional hazard models were used to estimate the effectiveness of receipt of at least 1 dose of influenza vaccine in preventing RT-PCR–confirmed influenza. Vaccination status was modeled as a time-varying covariate, with subjects considered vaccinated 14 days after vaccine receipt. VE was calculated as 100 × [1 – hazard ratio] and estimated in unadjusted and adjusted models; adjusted models included values for subject age and high-risk health status and accounted for clustering within households by computing robust variances, using sandwich estimators [9, 10, 18]. VE was also estimated for each combination of current-season and prior-season vaccine exposure (ie, current only, both current and prior, and prior only), with subjects unvaccinated in both seasons as the reference group. We also estimated and compared the effectiveness of the live-attenuated (LAIV) and inactivated (IIV) influenza vaccines among children 2–17 years of age.
Because of the predominance of infection with influenza A(H1N1)pdm09 among household members this season (47 of 50 infected subjects [94%]; 47 of 52 total influenza illnesses [90%]), analyses are focused on influenza A(H1N1)pdm09 infection outcomes. In analyses, the single influenza A(H3N2) virus and 4 influenza B virus (Yamagata lineage) infections were censored at the time of onset. Analyses estimated VE in preventing all influenza A(H1N1)pdm09 infections and, separately, community-acquired influenza A(H1N1)pdm09 infections (household index cases) and household-acquired influenza A(H1N1)pdm09 infections (secondary cases resulting from exposure to household index cases). A secondary (household-acquired) case was defined by transmission link to an index case if both cases were due to influenza A(H1N1)pdm09 and if illness onset in the secondary case occurred 1–7 days after illness onset in the index case. Overall and community VEs were estimated by comparing the hazard of influenza A(H1N1)pdm09 infection among vaccinated and unvaccinated subjects; cases that were household acquired were censored at the time of illness onset for community estimates. Household VE was estimated by comparing the hazard of influenza A(H1N1)pdm09 infection among vaccinated and unvaccinated subjects exposed to a household index case.
Preseason susceptibility to influenza A(H1N1)pdm09 infection was estimated using antibody titers determined by the HAI and NAI assays in sera collected at late fall preseason visits (or at summer enrollment visits, for those subjects without late fall preseason specimens and no evidence of influenza vaccine receipt). For vaccinated subjects, these susceptibility measures represented postvaccination titers. HAI and NAI antibody titers, representing preseason susceptibility, were calculated for each subject as the reciprocal (eg, 160) of the highest dilution of sera (eg, 1:160) that inhibited HA or NA activity. HAI and NAI titers were log transformed, and the mean and standard deviation (SD) of the transformed values were calculated and then exponentiated to obtain the geometric mean and SD. Geometric mean titers (GMTs) were estimated for each combination of current-season and prior-season vaccine exposure (ie, current only, both current and prior, prior only, and neither current nor prior) and by joint vaccination and case status. GMTs were compared across categories, using Wilcoxon rank sum tests. Serologic response to vaccination was estimated by measuring fold increases in antibody titers, determined by the HAI and NAI assays, between summer enrollment (prevaccination) specimens and late fall preseason (postvaccination) specimens. The proportions of vaccinated subjects tested with ≥4-fold increases in titers of antibody to the HA and NA targets were determined. All statistical analyses were performed using SAS software (release 9.3; SAS Institute); all figures were prepared using R software (version 3.1.0). A P value of <.05 or a positive lower bound of a confidence interval (CI) indicated statistical significance.
RESULTS
Characteristics of Households and Participants
A total of 1049 participants, including 618 children (59%), from 232 households were enrolled in the 2013–2014 study year. Most households (96%) had participated the prior year (during the 2012–2013 season). Household size ranged from 4 to 10 members (median, 4 members); all households had at least 2 participating children, and 68% had ≥1 child aged <9 years.
Participant characteristics, plus distributions of vaccination status and influenza A(H1N1)pdm09 infection outcomes, are presented in Table 1. Overall, 126 subjects (12%) had high-risk health condition, and 661 (63%) had documented evidence of receipt of at least 1 dose of 2013–2014 influenza vaccine; vaccine coverage significantly varied by age and race. Among vaccinated subjects, 559 (85%) received IIV, and 102 (15%) received LAIV; 96% of LAIV recipients were children aged 2–17 years. Based on national immunization guidelines, 217 vaccinated children (96%) <9 years old were considered fully vaccinated [17].
Table 1.
Characteristics of Participating Household Members During the 2013–2014 Influenza Season, by Documented Influenza Vaccine Receipt and 2009 Pandemic Influenza A(H1N1) Virus (Influenza A[H1N1]pdm09) Infection Status: Household Influenza Vaccine Effectiveness Study, Ann Arbor, Michigan
| Participant Characteristics | All Subjects, No. (%) (n = 1049) | Documented Influenza Vaccination, No. (%)a | Influenza A(H1N1)pdm09 Infection, No. (%)b |
|---|---|---|---|
| Age, y | |||
| <9 | 314 (29.9) | 225 (71.7)c,d | 22 (7.0)e |
| 9–17 | 304 (29.0) | 191 (62.8) | 5 (1.6) |
| 18–49 | 380 (36.2) | 215 (56.6) | 20 (5.3) |
| ≥50 | 51 (4.9) | 30 (58.8) | 0 (0.0) |
| Race | |||
| White | 823 (78.5) | 534 (64.9)d | 34 (4.1)e |
| Asian | 83 (7.9) | 57 (68.7) | 6 (7.2) |
| Black | 61 (5.8) | 35 (57.4) | 0 (0.0) |
| Other/unknown | 82 (7.8) | 35 (42.7) | 7 (8.5) |
| Sex | |||
| Female | 529 (50.4) | 339 (64.1) | 24 (4.5) |
| Male | 520 (49.6) | 322 (61.9) | 23 (4.4) |
| High-risk health condition | |||
| Any | 126 (12.0) | 88 (69.8) | 10 (7.9)e |
| None | 923 (88.0) | 573 (62.1) | 37 (4.0) |
| Documented influenza vaccinationa | |||
| Yes | 661 (63.0) | … | 16 (2.4)d |
| No | 388 (37.0) | … | 31 (8.0) |
| Overall | 1049 (100) | 661 (63.0) | 47f (4.5) |
a Vaccination was defined as at least 1 dose influenza vaccine received during the 2013–2014 vaccination period, as documented in the medical record or state immunization registry; subjects with laboratory-confirmed influenza A(H1N1)pdm09 virus infection were considered vaccinated if vaccine was administered ≥14 days prior to illness onset. The denominator for percentages is all subjects (vaccinated or unvaccinated) with the specified characteristic.
b The denominator for percentages is all subjects (with or without influenza A[H1N1]pdm09 infection) with the specified characteristic.
c A total of 217 of 225 vaccinated children (96.4%) <9 years of age were considered fully vaccinated, as defined by Advisory Committee on Immunization Practices recommendations.
d P<.001, by the Pearson χ2 or Fisher exact tests, comparing vaccinated and unvaccinated subjects or subjects with and those without laboratory-confirmed influenza.
e P<.05, by the Pearson χ2 or Fisher exact tests, comparing vaccinated and unvaccinated subjects or subjects with and those without laboratory-confirmed influenza.
f This value denotes the 47 cases of influenza A(H1N1)pdm09 infection identified in 47 individuals.
Illness Surveillance and Influenza Outcomes
During surveillance, 425 participants (41%) from 157 households (68%) reported 706 acute respiratory illnesses, and specimens from 676 (86%) were collected. All illness specimens were tested for influenza virus by RT-PCR. Influenza A(H1N1)pdm09 was identified in 47 individuals (4.5%) and 25 households (10.8%). Infection risks were significantly higher in young children (7.0% among those aged <9 years) and in participants with ≥1 high-risk health condition and were significantly lower in vaccinated subjects, compared with unvaccinated subjects (2.4% vs 8.0%; P < .001). Seventeen influenza A(H1N1)pdm09 cases (36%) were considered household acquired, based on exposure to 30 index or co-index community-acquired infections; 8 cases (17%) were medically attended.
Estimates of Influenza VE
Influenza A(H1N1)pdm09 infection risks for vaccinated and unvaccinated subjects and results from unadjusted and adjusted VE models are presented in Table 2. Infection risks for overall, community-acquired, and household-acquired illnesses were 4.5%, 2.9%, and 18.5%, respectively. Overall, adjusted VE against infection with influenza A(H1N1)pdm09 was 66% (95% CI, 23%–85%), with nearly identical point estimates in all 3 age categories. Vaccine was 54% effective (95% CI, −4% to 80%) in preventing community-acquired influenza A(H1N1)pdm09 infection and 65% effective (95% CI, 10%–87%) in preventing household-acquired infection. Among children aged 2–8 years, influenza A(H1N1)pdm09 infection risks were lower in recipients of LAIV, compared with those who received IIV (1.6% vs 4.3%), resulting in slightly higher VE point estimates for LAIV; both estimates indicated lower risk in vaccinated children, but neither estimate was statistically significant. Among children aged 9–17 years, influenza A(H1N1)pdm09 infection risks were slightly higher in recipients of LAIV, compared with IIV recipients (2.8% vs 0.7%), and VE points estimates favored IIV; however, because of the low overall infection risk (1.6%) in this age group, CIs were wide, and neither estimate was statistically significant.
Table 2.
Estimates of Vaccine Effectiveness (VE) in Preventing Outcomes of 2009 Pandemic Influenza A(H1N1) Virus (Influenza A[H1N1]pdm09) Infection, by Age, Influenza A[H1N1]pdm09 Source, and Vaccine Received, During the 2013–2014 Influenza Season: Household Influenza Vaccine Effectiveness (HIVE) Study, Ann Arbor, Michigan
| Variable | No. Positive/No. Evaluated (%) |
VE, % (95% CI)a |
||
|---|---|---|---|---|
| Vaccinated | Unvaccinated | Unadjusted | Adjustedb | |
| All influenza A(H1N1)pdm09 | ||||
| All Ages | 16/661 (2.4) | 31/388 (8.0) | 58 (5–82) | 66 (23–85) |
| <9 y | 8/225 (3.6) | 14/89 (15.7) | 65 (0–88) | 68 (10–88) |
| 9–17 y | 2/191 (1.1) | 3/113 (2.7) | 50 (−269 to 93) | 65 (−143 to 95) |
| ≥18 y | 6/245 (2.5) | 14/186 (7.5) | 59 (−4 to 83) | 66 (15–86) |
| Community-acquired influenza A(H1N1)pdm09c | ||||
| All Ages | 12/661 (1.8) | 18/388 (4.6) | 47 (−24 to 77) | 54 (−4 to 80) |
| Household-acquired influenza A(H1N1)pdm09d | ||||
| All Ages | 4/38 (10.5) | 13/54 (24.1) | 58 (−1 to 83) | 65 (10–87) |
| All influenza A(H1N1)pdm09 | ||||
| Age 2–8 y | ||||
| LAIV | 1/62 (1.6) | 13/83 (15.7) | 85 (−31 to 98) | 82 (−65 to 98) |
| IIV | 6/141 (4.3) | 13/83 (15.7) | 58 (−34 to 87) | 65 (−3 to 88) |
| Age 9–17 y | ||||
| LAIV | 1/36 (2.8) | 3/113 (2.7) | −27 (−1249 to 88) | 11 (−658 to 90) |
| IIV | 1/155 (0.7) | 3/113 (2.7) | 69 (−265 to 97) | 78 (−150 to 98) |
Abbreviations: CI, confidence interval; IIV, inactivated influenza vaccine; LAIV, live attenuated influenza vaccine.
a VE was calculated as 100 × [1 − hazard ratio] and denotes the effectiveness of at least 1 dose of influenza vaccine in preventing laboratory-confirmed influenza A(H1N1)pdm09 infection. Vaccination status was modeled as time-varying covariate, with subjects considered vaccinated 14 days after vaccine receipt. To adjust for correlation of exposures and outcomes among subjects in the same household, robust variances for model parameter estimates were computed using sandwich estimators [18].
b Models were adjusted for age in months (natural cubic spline) and medical record–documented high-risk health status (present/absent).
c Thirty cases of influenza A(H1N1)pdm09 infection were defined as community acquired.
d Seventeen cases of influenza A(H1N1)pdm09 infection were defined as household acquired.
Estimates of VE by 2-year vaccination history for subjects aged ≥9 years and, separately, those aged <9 years are presented in Table 3. Results indicated substantial protection for subjects in both age groups who were vaccinated in both the current (2013–2014) and prior (2012–2013) seasons as compared to those unvaccinated in both seasons. Results also indicated similar but nonsignificant protection for the relatively fewer subjects vaccinated in just the current season, plus evidence of residual protection for subjects vaccinated in just the prior season.
Table 3.
Estimates of Vaccine Effectiveness (VE) in Preventing Laboratory-Confirmed Infection Due to 2009 Pandemic Influenza A(H1N1) Virus, by 2-Year Vaccination Status, Among Subjects ≥9 Years of Age, and Separately, Among Subjects <9 Years
| 2-Year Vaccination Status | No. Positive/No. Evaluated (%) | VE, % (95% CI)a |
|
|---|---|---|---|
| Unadjusted | Adjustedb | ||
| Subjects ≥9 y of age | |||
| 2013–2014 only | 1/65 (1.5) | 59 (−221 to 95) | 63 (−204 to 96) |
| Both 2012–2013 and 2013–2014 | 7/371 (1.9) | 59 (−1 to 84) | 67 (20–86) |
| 2012–2013 only | 4/59 (6.8) | 17 (−225 to 79) | 34 (−144 to 82) |
| Neither year | 13/240 (5.4) | Reference | Reference |
| Subjects <9 y of age | |||
| 2013–2014 only | 1/23 (4.4) | 55 (−212 to 94) | 66 (−92 to 94) |
| Both 2012–2013 and 2013–2014 | 7/202 (3.5) | 76 (26–93) | 77 (32–92) |
| 2012–2013 only | 1/16 (6.3) | 85 (−29 to 98) | 85 (−31 to 98) |
| Neither year | 13/73 (17.8) | Reference | Reference |
Abbreviation: CI, confidence interval.
a VE was calculated as 100 × [1 − hazard ratio] and denotes the effectiveness of receipt of influenza vaccine in the current year (2013–2014) only, the prior year (2012–2013) only, or both years, compared with no vaccination in both years, in preventing laboratory-confirmed influenza.
b Models were adjusted for age in months (natural cubic spline) and medical record–documented high-risk health status (present/absent).
Serologic Assessments of Preseason Susceptibility and Response to Vaccination
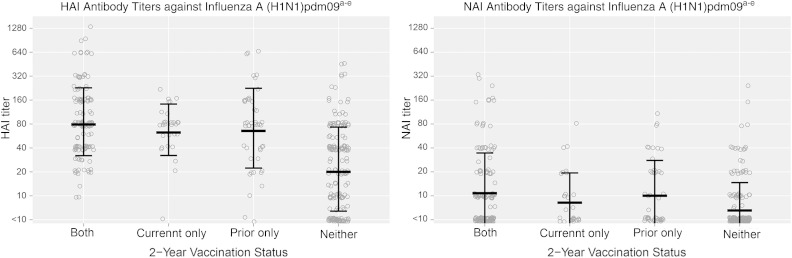
HAI and NAI antibody titers measured in sera collected from 383 subjects (66% of 578 subjects aged ≥13 years) were used to estimate preseason susceptibility to influenza A(H1N1)pdm09 infection; these titers were associated with antibody produced in response to vaccination and/or past infection. Figure 1 presents the distributions of titers of antibody against influenza A(H1N1)pdm09, based on each combination of current-season and prior-season vaccine exposure, with GMTs and SDs denoted by linked lines. Results indicated significantly higher HAI (P < .001) and NAI (P < .05) GMTs for subjects with each vaccination history, compared with GMTs for subjects unvaccinated both years, with no significant differences in HAI and NAI GMTs for subjects vaccinated one or both years.
Figure 1.
Distributions of pre-season susceptibility titers of hemagglutination-inhibition (HAI) and neuraminidase-inhibition (NAI) antibody against 2009 pandemic influenza A(H1N1) virus, based on each combination of current-season and prior-season vaccine exposure. aAntibody titers measured by hemagglutination-inhibition (HAI) and neuraminidase-inhibition (NAI) assays in sera collected from a subset of subjects aged ≥13 years at pre-season visits (or at enrollment for those subjects without pre-season specimens and no evidence of influenza vaccine receipt) were used to estimate pre-season susceptibility to influenza; bSera were tested with the HAI assay using as the antigen the influenza A (pH1N1)pdm09 virus strain present in the 2013–2014 North American influenza vaccine (A/California/07/2009); cSera were tested with the NAI assay using as the target, a reassortant influenza virus with the NA representing the A (pH1N1)pdm09 virus strain present in the 2013–2014 North American influenza vaccine (A/California/07/2009) and a mismatched HA (H6 subtype); dEach circle indicates the titer of an individual observation; Linked lines indicate the geometric mean titer ± the geometric standard deviation; eAll vaccination groups (both years, current only, and prior only) had significantly higher geometric mean titers (P < .001) than those unvaccinated both years for all antigens.
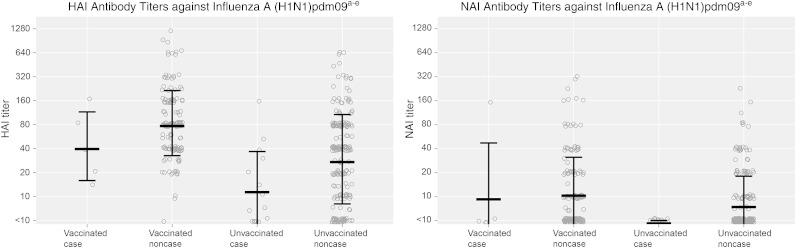
Figure 2 presents HAI and NAI susceptibility titers for current-season vaccinated and unvaccinated subjects who ultimately were cases or noncases, based on influenza A(H1N1)pdm09 identification by RT-PCR. Twenty influenza A(H1N1)pdm09 cases (95% of 21 cases among subjects aged >13 years; 43% of all 47 cases) had susceptibility assessments. Overall, influenza A(H1N1)pdm09 cases had significantly lower HAI and NAI GMTs than noncases (P < .01 for both comparisons), indicating greater susceptibility. When stratified by vaccination status, HAI and NAI GMTs were not significantly different for vaccinated cases and noncases but differed significantly for unvaccinated cases and noncases (P = .01).
Figure 2.
Preseason susceptibility hemagglutination-inhibition (HAI) and neuraminidase-inhibition (NAI) antibody titers against 2009 pandemic influenza A(H1N1) virus for current-season vaccinated and unvaccinated subjects who ultimately were cases or noncases. aAntibody titers measured by hemagglutination-inhibition (HAI) and neuraminidase-inhibition (NAI) assays in sera collected from a subset of subjects aged ≥13 years at pre-season visits (or at enrollment for those subjects without pre-season specimens and no evidence of influenza vaccine receipt) were used to estimate pre-season susceptibility to influenza; bSera were tested with the HAI assay using as the antigen the influenza A (pH1N1)pdm09 virus strain present in the 2013–2014 North American influenza vaccine (A/California/07/2009); cSera were tested with the NAI assay using as the target, a reassortant influenza virus with the NA representing the A (pH1N1)pdm09 virus strain present in the 2013–2014 North American influenza vaccine (A/California/07/2009) and a mismatched HA (H6 subtype); dEach circle indicates the titer of an individual observation; Linked lines indicate the geometric mean titer ± the geometric standard deviation; eInfluenza A (pH1N1)pdm09 cases had significantly lower geometric mean HAI and NAI titers than non-cases overall (P < .001, P = .003); this pattern was more pronounced for unvaccinated (P = .01, P = .01) subjects compared to vaccinated (P = .15, P = .32) subjects.
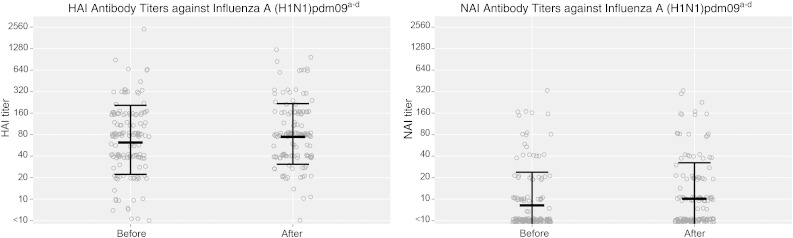
Figure 3 presents HAI and NAI GMTs measured in specimens collected during summer enrollment (before vaccination) and late fall (≥30 days after vaccination) visits; paired sera were available from 141 vaccinated subjects (43% of all 325 vaccinated subjects aged ≥13 years; 21% of all 661 vaccinated subjects). Results indicated only minor differences in HAI and NAI GMTs between time points for vaccinated subjects. Only 15 subjects (11%) had a ≥4-fold increase in titer of antibody to the HA target of influenza A(H1N1)pdm09, and 9 (6%) had a ≥4-fold increase in the titer of antibody to the NA target; a single subject (<1%) had a ≥4-fold increase in the titer of antibody to both targets. Approximately 85% of vaccinated subjects who failed to demonstrate ≥4-fold titer increases in antibody titer for the HA and NA targets, and 67% of those with appropriate titer increases had been vaccinated in both the current and prior seasons (P > .05, by the Fisher exact test); the single subject with ≥4-fold increases in antibody titer to both targets had been vaccinated both seasons.
Figure 3.
Hemagglutination-inhibition (HAI) and neuraminidase-inhibition (NAI) antibody titers against 2009 pandemic influenza A(H1N1) virus in specimens collected during summer enrollment (before vaccination) and late fall (≥30 days after vaccination) visits. aAntibody titers measured by hemagglutination-inhibition (HAI) and neuraminidase-inhibition (NAI) assays in sera collected from a subset of vaccinated subjects aged ≥13 years prior to vaccination (May–September 2013) and ≥30 days post-vaccination (November–December 2013) were used to evaluate response to influenza vaccination; bSera were tested with the HAI assay using as the antigen the influenza A (pH1N1)pdm09 virus strain present in the 2013–2014 North American influenza vaccine (A/California/07/2009); cSera were tested with the NAI assay using as the target, a reassortant influenza virus with the NA representing the A (pH1N1)pdm09 virus strain present in the 2013–2014 North American influenza vaccine (A/California/07/2009) and a mismatched HA (H6 subtype); dEach circle indicates the titer of an individual observation; Linked lines indicate the geometric mean titer ± the geometric standard deviation.
DISCUSSION
We observed substantial vaccine protection (66%; 95% CI, 23%–85%) in the 2013–2014 season against infection with influenza A(H1N1)pdm09, which predominated during this season, with similar VE point estimates by age category and against both community-acquired and household-acquired infection. Our overall VE estimates were very similar to estimates from the US Influenza Vaccine Effectiveness Network in the same season and somewhat higher than those from the European I-MOVE Network; these networks examine VE in healthcare settings, using alternative designs to that used in the household study [19, 20]. We also examined and compared VE estimates in children aged 2–17 years, based on vaccine type. Both the LAIV and IIV appeared to reduce the risk of influenza A(H1N1)pdm09 infection in children, but none of the estimates were statistically significant, at least in part because of limited sample sizes, and CIs were wide. LAIV had been thought to provide better protection than IIV in children [21] and a preferential recommendation was initiated by the Advisory Committee on Immunization Practices (ACIP) prior to the 2014–2015 season [22]. We found evidence of a slight but not significant advantage for LAIV in children aged 2–8 years, but IIV appeared to be more effective in older children. These results neither support nor refute the preferential recommendation, which the ACIP elected not to renew in February 2015, based on additional comparative analyses [23], but are in keeping with the concept that any potential advantage of LAIV is limited to the youngest children.
With the exceptions of the influenza pandemic in 2009 and now the 2013–2014 influenza season, recent seasons have seen wide circulation of influenza A(H3N2) virus and, to a lesser extent, influenza B virus strains, with only minimal circulation of influenza A(H1N1)pdm09. In seasons when it was possible to estimate VE by virus strain, VE estimates against influenza A(H1N1)pdm09 have been consistently higher than estimates against influenza A(H3N2) viruses [2–4]. The influenza A(H3N2) virus strain selected for inclusion as a component of the annual vaccines has been updated 3 times in the past 6 seasons (since 2009–2010). These updates are due to changes in the antigenic/genetic characteristics of circulating strains that could potentially lower vaccine induced protection [17, 24]. In contrast, the influenza A(H1N1)pdm09 strain appears more antigenically stable, and similar vaccine component updates have not been necessary; 99% of tested influenza A(H1N1)pdm09 viruses collected during the 2013–2014 season were found to be antigenically similar to the A/California/7/2009(H1N1)pdm09-like virus selected for the monovalent vaccine during the 2009 pandemic [13, 14].
Based on previously published evidence of lower influenza VE point estimates with repeated annual vaccination [3, 4, 9, 10], we estimated VE against influenza A(H1N1)pdm09 by 2-year vaccination history. VE estimates were similarly high in 2013–2014 for the large number of subjects vaccinated in both the current and prior seasons and for the far fewer subjects vaccinated in only the current season, with similar findings for older children and adults (subjects aged ≥9 years) and for younger children. This is in contrast to previous seasons (2010–2011 and 2012–2013), when influenza A(H3N2) virus predominated, and VE estimates in the household study indicated substantially lower VE point estimates for subjects vaccinated in both the current and prior seasons, compared with those vaccinated in only the current season [9, 10]. Serologic evidence of preseason susceptibility, based on 2-year vaccination status, to the influenza A(H3N2) strain that predominated in the 2012–2013 season and the influenza A(H1N1)pdm09 strain that predominated in the current 2013–2014 season were consistent with these VE estimates [10]. Specifically, both HAI and NAI antibody titers against influenza A(H3N2) virus in 2012–2013 were higher for those vaccinated in only the current season, compared with those vaccinated in both the current and prior seasons [10]. In contrast, HAI and NAI antibody titers against influenza A(H1N1)pdm09 in 2013–2014 did not substantially differ by 2-year vaccination status. Evidence of some degree of residual protection with vaccination only in the prior year was apparent in both study years [10].
We also examined the response to vaccination with influenza A(H1N1)pdm09 and found little evidence for serologic boosts in antibody titers for vaccinated subjects; a similar lack of response was demonstrated to the influenza A(H3N2) vaccine virus in the 2012–2013 season (unpublished data). For both viruses, history of prior vaccination may impair the subsequent vaccine response [25]. However, because there has been little antigenic drift among circulating influenza A(H1N1)pdm09 viruses, preexisting antibodies are presumably still relevant to protection. In contrast, there has been substantial antigenic drift among circulating influenza A(H3N2) viruses during the same period. It may be that influenza A(H3N2) viruses included in past vaccines were similar enough to current vaccine viruses to impair response, yet dissimilar enough from currently circulating viruses that antibody produced in response to past vaccines does not strongly contribute to protection [25–27].
Influenza VE varies by influenza A virus subtype, with typically higher estimates against influenza A(H1N1) viruses, compared with influenza A(H3N2) viruses [2–4]. Thus, it would be a mistake not to distinguish between influenza A virus subtypes in any VE evaluation. Differences also exist between the influenza A virus subtypes with regard to circulation frequency and likelihood to produce severe disease, with influenza A(H3N2) viruses predominating [28–30]. Some of these differences may be driven, at least in part, by fundamental differences in the degree/speed of relevant antigenic drift of the influenza A(H3N2) and A(H1N1) viruses [31]. The relation of these observations to the effect of prior year vaccination on current VE is even more complex and may be related to vaccination and infection history over multiple influenza seasons. It is only through studies that document infections over time and include serologic evaluations that these complicated issues may be unraveled.
Notes
Disclaimer. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC).
Financial support. This work was supported by the CDC (U01 IP000474) and the National Institute of Allergy and Infectious Diseases (R01 AI097150).
Potential conflicts of interest. S. E. O. has received grant support from Sanofi Pasteur for work unrelated to this report. A. S. M. has received grant support from Sanofi Pasteur and consultancy fees from Sanofi, GSK, and Novavax for work unrelated to this report. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Griffin MR, Monto AS, Belongia EA et al. . Effectiveness of non-adjuvanted pandemic influenza A vaccines for preventing pandemic influenza acute respiratory illness visits in 4 U.S. communities. PLoS One 2011; 6:e23085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Treanor J, Talbot HK, Ohmit SE et al. . Effectiveness of seasonal influenza vaccines in the United States during a season with circulation of all three vaccine strains. Clin Infect Dis 2012; 55:951–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ohmit SE, Thompson MG, Petrie JG et al. . Influenza vaccine effectiveness in the 2011–2012 season: protection against each circulating virus and the effect of prior vaccination on estimates. Clin Infect Dis 2014; 58:319–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McLean HQ, Thompson MG, Sundaram ME et al. . Influenza vaccine effectiveness in the United States during 2012–2013: variable protection by age and virus type. J Infect Dis 2015; 211:1529–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Foppa IM, Haber M, Ferdinands JM et al. . The case test-negative design for studies of the effectiveness of influenza vaccine. Vaccine 2013; 31:3104–9. [DOI] [PubMed] [Google Scholar]
- 6.Jackson ML, Nelson JC. The test-negative design for estimating influenza vaccine effectiveness. Vaccine 2013; 19:2165–8. [DOI] [PubMed] [Google Scholar]
- 7.Jackson ML, Rothman KJ. Effects of imperfect test sensitivity and specificity on observational studies of influenza vaccine effectiveness. Vaccine 2015; 33:1313–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Osterholm MT, Kelley NS, Sommer A, Belongia A. Efficacy and effectiveness of influenza vaccines: a systematic review and meta-analysis. Lancet Infect Dis 2012; 12:36–44. [DOI] [PubMed] [Google Scholar]
- 9.Ohmit SE, Petrie JG, Malosh RE et al. . Influenza vaccine effectiveness in the community and the household. Clin Infect Dis 2013; 56:1363–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ohmit SE, Petrie JG, Malosh RE, Fry AM, Thompson MG, Monto AS. Influenza vaccine effectiveness in households with children during the 2012–2013 season: assessments of prior vaccination and serologic susceptibility. J Infect Dis 2015; 211:1519–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Monto AS, Malosh RE, Petrie JG, Thompson MG, Ohmit SE. Frequency of acute respiratory illnesses and circulation of respiratory viruses in households with children over 3 surveillance seasons. J Infect Dis 2014; 210:1792–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Petrie JG, Ohmit SE, Cowling BJ et al. . Influenza transmission in a cohort of households with children: 2010–2011. PLoS One 2013; 8:e75339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Epperson S, Blanton L, Kniss K et al. . Influenza activity – United States, 2013–14 season and composition of the 2014–15 influenza vaccines. MMWR Morb Mortal Wkly Rep 2014; 63:483–90. [PMC free article] [PubMed] [Google Scholar]
- 14.Appiah GD, Blanton L, D'Mello T et al. . Influenza activity – United States, 2014–15 season and composition of the 2015–16 influenza vaccine. MMWR Morb Mortal Wkly Rep 2015; 64:583–90. [PMC free article] [PubMed] [Google Scholar]
- 15.Ohmit SE, Petrie JG, Cross RT, Johnson E, Monto AS. Influenza hemagglutination-inhibition antibody titer as a correlate of vaccine-induced protection. J Infect Dis 2011; 204:1879–85. [DOI] [PubMed] [Google Scholar]
- 16.Monto AS, Petrie JG, Cross RT et al. . Antibody to influenza virus neuraminidase: an independent correlate of protection. J Infect Dis 2015; 212:1191–9. [DOI] [PubMed] [Google Scholar]
- 17.Grohskopf LA, Shay DK, Shimabukuro TT et al. . Prevention and control of seasonal influenza with vaccines. Recommendations of the Advisory Committee on Immunization Practices (ACIP)—United States, 2013–2014. MMWR Recomm Rep 2013; 62(RR-07):1–43. [PubMed] [Google Scholar]
- 18.Wei LJ, Lin DY, Weissfield L. Regression analysis of multivariate incomplete failure time data by modeling marginal distribution. J Am Statistical Assoc 1989; 84:1065–73. [Google Scholar]
- 19.Flannery B, Thaker SN, Clippard J et al. . Interim estimates of 2013–2014 seasonal influenza vaccine effectiveness—United States, February 2014. MMWR Morb Mortal Wkly Rep 2014; 63:137–42. [PMC free article] [PubMed] [Google Scholar]
- 20.Valenciano M, Kissling E, Reuss A et al. . The European I-Move multicentre 2013–2014 case-control study. Homogeneous moderate influenza vaccine effectiveness against A (H1N1) pdm09 and heterogeneous results by country against A (H3N2). Vaccine 2015; 33:2813–22. [DOI] [PubMed] [Google Scholar]
- 21.Belshe RB, Edwards KM, Vesikari T et al. . Live attenuated versus inactivated influenza vaccine in infants and young children. N Engl J Med 2007; 356:685–96. [DOI] [PubMed] [Google Scholar]
- 22.Grohskopf LA, Olsen SJ, Sokolow LZ et al. . Prevention and control of seasonal influenza with vaccines. Recommendations of the Advisory Committee on Immunization Practices (ACIP), 2014. MMWR Morb Mortal Wkly Rep 2014; 63:691–7. [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Advisory Committee on Immunization Practices (ACIP) reaffirms recommendation for annual influenza vaccination: no stated preference for nasal spray vaccine or flu shot expressed. http://www.cdc.gov/media/releases/2015/s0226-acip.html Accessed 17 August 2015. [Google Scholar]
- 24.Russell CA, Jones TC, Barr IC et al. . Influenza vaccine strain selection and recent studies on the global migration of seasonal influenza vaccines. Vaccine 2008; 26(suppl 4):D31–4. [DOI] [PubMed] [Google Scholar]
- 25.Fonville JM, Wilks SH, James SL et al. . Antibody landscapes after influenza virus infection or vaccination. Science 2014; 346:996–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bedford T, Riley S, Barr IG et al. . Global circulation patterns of seasonal influenza viruses vary with antigenic drift. Nature 2015; 523:217–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Truscott J, Fraser C, Cauchemez S et al. . Essential epidemiological mechanisms underpinning the transmission dynamics of seasonal influenza. J Royal Society Interface 2012; 9:304–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thompson WW, Weintraub E, Dhankhar P et al. . Estimates of US influenza-associated deaths made using four different methods. Influenza Other Respir Viruses 2009; 3:37–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thompson WW, Shay DK, Weintraub E et al. . Influenza-associated hospitalizations in the United States. JAMA 2004; 292:1333–40. [DOI] [PubMed] [Google Scholar]
- 30.Hayward AC, Fragaszy EB, Bermingham A et al. . Comparative community burden and severity of seasonal and pandemic influenza: results of the Flu Watch Cohort study. Lancet Respir Med 2014; 2:445–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith DJ, Lapedes AS, de Jong JC et al. . Mapping the antigenic and genetic evolution of influenza viruses. Science 2004; 305:371–6. [DOI] [PubMed] [Google Scholar]