Abstract
Background
In palliative care patients, fatigue can be severely debilitating and is often not counteracted with rest, thereby impacting daily activity and quality of life. Further complicating issues are the multidimensionality, subjective nature and lack of a consensus definition of fatigue. The review aimed to evaluate the efficacy of pharmacological treatments for fatigue in palliative care, with a focus on patients at an advanced stage of disease, including patients with cancer and other chronic diseases.
Methods
We considered randomized controlled trials concerning adult palliative care with a focus on pharmacological treatment of fatigue compared with placebo, application of two drugs, usual care or a non‐pharmacological intervention. The primary outcome had to be non‐specific fatigue (or related terms such as asthenia). We searched the CENTRAL, MEDLINE, PsycINFO and EMBASE, and a selection of cancer journals up to 28 April 2014. Two review authors independently assessed trial quality and extracted the data.
Results
We screened 1645 publications of which 45 met the inclusion criteria. In total, we analysed data from 18 drugs and 4696 participants. There was a very high degree of statistical and clinical heterogeneity in the trials. Meta‐analysis of data was possible for modafinil, pemoline, and methylphenidate.
Conclusions
Due to the limited evidence, we cannot recommend a specific drug for the treatment of fatigue in palliative care patients. Some drugs, which may be beneficial for the treatment of fatigue associated with palliative care such as amantadine, methylphenidate, and modafinil, should be further researched.
Keywords: Pharmacological treatments, Fatigue, Palliative care, Advanced disease, Systematic review
Introduction
Fatigue is a common symptom in palliative care patients, and virtually, every intervention used to treat cancer, as well as the primary disease itself, may cause or contribute to fatigue. In a study of 1000 patients in an American palliative care programme, fatigue, weakness, and lack of energy were three of the five most frequently reported symptoms with a prevalence of 84%, 66%, and 61%, respectively.1 Fatigue is also commonly reported in non‐cancer patients with progressive life‐threatening diseases, such as multiple sclerosis and .amyotrophic lateral sclerosis,2 chronic obstructive pulmonary disease,3 heart failure,4 HIV,5 as well as chronic heart, kidney, or lung diseases.6, 7 Several drugs, such as the new anti‐neoplastic therapies, or drugs regularly used in palliative care have sedative properties, for example, opioid analgesics, benzodiazepines, antidepressants, or anticonvulsants can cause fatigue.8
The pathophysiology of fatigue in palliative care patients is not fully understood. ‘Primary fatigue’ has been said to be related to the high cytokine load. Disease‐related symptoms, such as sleep disturbances, may also account for fatigue and may be termed ‘secondary fatigue’. There are several definitions of fatigue. For this Cochrane review, we selected the definition of the European Association of Palliative Care: ‘Fatigue is a subjective feeling of tiredness, weakness, or lack of energy’.8
Assessment of fatigue will depend on subjective self‐assessment by the patient, substituted by caregiver or medical staff estimations only where self assessment is not possible. Single‐item scales have been proposed, and a multitude of checklists and questionnaires with multiple dimensions have been validated.9 It is possible that a number of hindrances such as lack of consensus on the definition of fatigue or on significant cut‐off levels of evaluation instruments limited structured approach with assessment and treatment steps have led to underestimation and undertreatment fatigue.
If possible, a causative treatment approach should be addressed. Most patients will require symptomatic treatment of fatigue with pharmacological and non‐pharmacological therapies. Some studies10, 11 have examined the role of non‐drug treatments for cancer‐related fatigue, such as patient education with provision of information on fatigue and its treatment, keeping a diary, energy expenditure planning, and physical exercise. On the other hand, there is a growing body of evidence that gives examples of effective pharmacological treatments for fatigue.12, 13, 14 Several recent systematic reviews15, 16, 17 have covered some drugs used to treat fatigue in cancer patients.
This paper provides an executive summary of a recent Cochrane Collaboration systematic review,18 which synthesizes evidence for the evaluation of the efficacy of pharmacological treatments for fatigue in palliative care, with a focus on patients at an advanced stage of disease, including patients with cancer and other chronic diseases. The review updated the original review,19 ‘Pharmacological treatments for fatigue associated with palliative care’ and also incorporated the review ‘Drug therapy for the management of cancer‐related fatigue’.16
Materials and methods
Eligibility criteria
Criteria for review entry were randomized controlled trials with focus on pharmacological treatment involving adults (≥18 years, both sexes), suffering fatigue in palliative care or in terminal illness. Participants could receive anti‐cancer treatment.
Outcome measures
Patient‐reported fatigue and the improvement of fatigue were the primary outcomes of this review, while the secondary outcomes included asthenia, weakness, tiredness, exhaustion, and treatment‐related burden.
Search strategy
We re‐engineered the search strategy (filter) of the previous review by Peuckmann‐Post et al. 19 to facilitate the combination with another review by Minton et al.16 To identify studies for inclusion in this updated review, we developed a detailed search strategy for each electronic database and other resources. To validate the search strategy, we selected sentinel studies.20, 21 The following electronic databases were searched from their inception until 28 April 2014 CENTRAL, MEDLINE (Ovid), PsycINFO (Ovid), and EMBASE. Additional information was obtained from standard textbooks on palliative medicine, unpublished literature through searches of conference proceedings and also from experts in the field of palliative care.
Data collection and analysis
Two review authors extracted the data (M. M. and M. C.) using a standard data extraction form and reviewed the data from the included studies. Two other authors (L. R. and H. C.) cross‐checked and sub‐sampled the data. We contacted the original investigators when dealing with the missing data. Two authors (M. M. and M. C.) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions and adapted from those used by the Cochrane Pregnancy and Childbirth Group, with any disagreements resolved by discussion or by involving other review authors (L. R. and H. C.). Subgroup analysis was performed for dealing with following different criteria; type of drug, type of disease, and type of assessment tools.
Results
We identified 1645 publications in the search. After we removed 186 duplicate studies, we retrieved articles against the inclusion criteria and found 45 studies, which met the inclusion criteria (Figure 1). In total, we analysed data from 18 drugs, nine type of disease, and 4696 participants. Only two21, 22 of the treatment groups in this review were large enough to give a low risk of bias (200 participants or more per treatment arm). Most studies reported some benefit of the active treatment. In general, adverse reactions were mild and had little or no impact.
Figure 1.
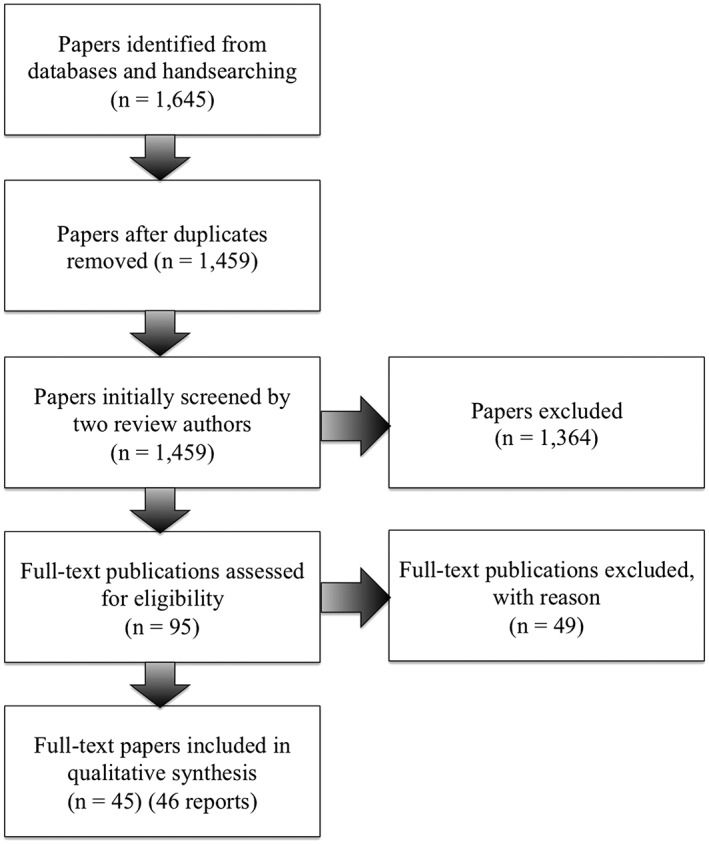
Study flow diagram.18
We used studies investigating pemoline and modafinil in participants with multiple sclerosis‐associated fatigue and methylphenidate in participants suffering from cancer and fatigue for meta‐analysis. However, the US Food and Drug Administration (FDA) has decided to withdraw pemoline products (marketed as Cylert) because of the risk of liver toxicity, which outweighs the benefits of the drug.
Methylphenidate in cancer
Meta‐analysis was performed for two studies,23, 24 which used the Functional Assessment for Chronic Illness Therapy ‐ Fatigue as the assessment tool in fatigue, comparing methylphenidate with placebo. The studies showed a slightly superior effect of methylphenidate compared with placebo (standardized mean difference 0.49, 95% confidence interval 0.15 to 0.83; Figure 2).
Figure 2.
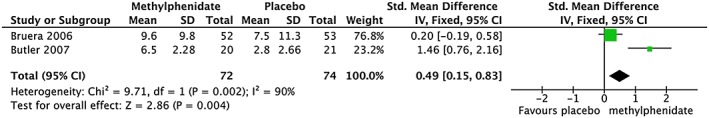
Forest plot of comparison of methylphenidate vs. placebo in cancer: Functional Assessment for Chronic Illness Therapy ‐ Fatigue score change.18
Modafinil in multiple sclerosis
Modafinil was tested in 115 patients with multiple sclerosis,25 but failed to demonstrate the superiority of modafinil vs. placebo. Another recent study of 21 patients with multiple sclerosis showed positive effect of modafinil.2 However, this result must be interpreted with caution because of the small participant numbers. Meta‐analysis of these two studies also failed to demonstrate a significant effect, with a standardized mean difference of −0.14 (Figure 3).
Figure 3.
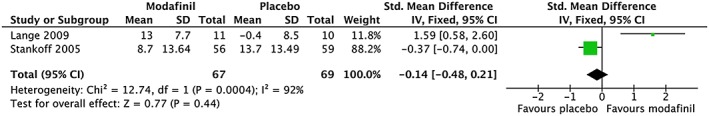
Forest plot of comparison of modafinil in cancer.18
Discussion
The aim of the Cochrane review18 was to evaluate the efficacy of pharmacological treatments for fatigue in palliative care, with a focus on patients at an advanced stage of disease, including patients with cancer and other chronic diseases.
Our search strategy allowed us to identify all relevant studies. We identified 45 studies for inclusion, with a wide range of underlying diseases and drug interventions. Treatment results pointed to weak and inconclusive evidence for the efficacy of amantadine, pemoline, and modafinil in multiple sclerosis and for carnitine and donepezil in cancer‐related fatigue. Meta‐analysis shows an estimated superior effect for methylphenidate in cancer‐related fatigue, but not for modafinil in multiple sclerosis. Further studies about the efficacy and safety of potential medicines for fatigue treatment such as acetylsalicylic acid, mistletoe extract, megestrol acetate, and medroxyprogesterone acetate are needed.
Many of the included studies involved only a small number of participants and did not follow a consistent research methodology. In some cases, the investigated population was very heterogeneous, and any outcome may have been associated with depression, making it difficult to distinguish from primary fatigue. These limitations made it difficult to compare the methodological quality across the studies.
There are many possible causes of secondary fatigue. Unfortunately, little evidence from randomized trials is available on the efficacy of these treatments. In clinical practice, any potential cause for secondary fatigue should be treated.
The results of the literature search indicate that recent research interest focuses on modafinil, which seems a promising agent to diminish fatigue for palliative care patients. This may be an interesting perspective for the future.
Conclusions
There is insufficient evidence to support the use of a specific medicine to treat fatigue in palliative care patients. In this regards, amantadine showed the promised benefit in patients with multiple sclerosis with fatigue and methylphenidate in patients with cancer‐related fatigue. Further trials are needed for several medicines, which were used in some studies with positive results such as dexamethasone, methylprednisolone, acetylsalicylic acid, armodafinil, amantadine, and L‐carnitine. To enhance the interpretation and generalization of findings from relevant study populations, randomized controlled trials with larger participant number are required. Consensus is needed regarding fatigue definition and outcome parameters for clinical trials.
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgements
The authors certify that they comply with the ethical guidelines for authorship and publishing of the Journal of Cachexia, Sarcopenia and Muscle.26
Mücke, M. , Mochamat, , Cuhls, H. , Peuckmann‐Post, V. , Minton, O. , Stone, P. , and Radbruch, L. (2016) Pharmacological treatments for fatigue associated with palliative care: executive summary of a Cochrane Collaboration systematic review. Journal of Cachexia, Sarcopenia and Muscle, 7: 23–27. doi: 10.1002/jcsm.12101.
References
- 1. Walsh D, Donnelly S, Rybicki L. The symptoms of advanced cancer: relationship to age, gender, and performance status in 1,000 patients. Support Care Canc 2000;8:175–179. [DOI] [PubMed] [Google Scholar]
- 2. Lange R, Volkmer M, Heesen C, Liepert J. Modafinil effects in multiple sclerosis patients with fatigue. J Neurol 2009;256:645–650. [DOI] [PubMed] [Google Scholar]
- 3. Stridsman C, Lindberg A, Skär L. Fatigue in chronic obstructive pulmonary disease: a qualitative study of people's experiences. Scand J Caring Sci 2014;28:130–138. [DOI] [PubMed] [Google Scholar]
- 4. Goodlin SJ. Palliative care for end‐stage heart failure. Curr Heart Fail Rep 2005;2:155–160. [DOI] [PubMed] [Google Scholar]
- 5. Norval DA. Symptoms and sites of pain experienced by AIDS patients. S Afr Med J 2004;94:450–454. [PubMed] [Google Scholar]
- 6. Jhamb M, Liang K, Yabes J, Steel JL, Dew MA, Shah N, et al. Prevalence and correlates of fatigue in chronic kidney disease and end‐stage renal disease: are sleep disorders a key to understanding fatigue? Am J Nephrol 2013;38:489–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tang W‐R, Yu C‐Y, Yeh S‐J. Fatigue and its related factors in patients with chronic heart failure. J Clin Nurs 2010;19:69–78. [DOI] [PubMed] [Google Scholar]
- 8. Radbruch L, Strasser F, Elsner F, Gonçalves JF, Løge J, Kaasa S, et al. Fatigue in palliative care patients—an EAPC approach. Palliat Med 2008;22:13–32. [DOI] [PubMed] [Google Scholar]
- 9. Dittner AJ, Wessely SC, Brown RG. The assessment of fatigue: a practical guide for clinicians and researchers. J Psychosom Res 2004;56:157–170. [DOI] [PubMed] [Google Scholar]
- 10. Schmitz KH, Holtzman J, Courneya KS, Mâsse LC, Duval S, Kane R. Controlled physical activity trials in cancer survivors: a systematic review and meta‐analysis. Canc Epidemiol Biomarkers Prev 2005;14:1588–1595. [DOI] [PubMed] [Google Scholar]
- 11. Mock V. Evidence‐based treatment for cancer‐related fatigue. J Natl Cancer Inst Monogr. 2004;32:112–118. [DOI] [PubMed] [Google Scholar]
- 12. Barak Y, Magalashvili D, Dolgopiat MD, Ladkani D, Nitzani D, Mazor Z, et al. Effect of alfacalcidol on fatigue in MS patients: a randomized, double‐blind study (S23.004). Neurology 2014;82:S23.004–S23.004. [Google Scholar]
- 13. Morrow GR, Shelke AR, Roscoe JA, Hickok JT, Mustian K. Management of cancer‐related fatigue. Cancer Invest 2005;23:229–239. [DOI] [PubMed] [Google Scholar]
- 14. Yennurajalingam S, Frisbee‐Hume S, Palmer JL, Delgado‐Guay MO, Bull J, Phan AT, et al. Reduction of cancer‐related fatigue with dexamethasone: a double‐blind, randomized, placebo‐controlled trial in patients with advanced cancer. J Clin Oncol 2013;31:3076–3082. [DOI] [PubMed] [Google Scholar]
- 15. Pucci E, Branãs Tato P, D'Amico R, Giuliani G, Solari A, Taus C. A mantadine for fatigue in multiple sclerosis. Cochrane Database of Systematic Reviews 2007, Issue 1 Art. No.: CD002818. DOI: 10.1002/14651858.CD002818.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Minton O, Richardson A, Sharpe M, Hotopf M, Stone P. Drug therapy for the management of cancer-related fatigue. Cochrane Database of Systematic Reviews 2010, Issue 7 Art. No.: CD006704. DOI:10.1002/14651858.CD006704.pub3. [DOI] [PubMed] [Google Scholar]
- 17. Tejani AM, Wasdell M, Spiwak R, Rowell G, Nathwani S. Carnitine for fatigue in multiple sclerosis. Cochrane Database Syst Rev 2012;5:CD007280:. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mücke M, Mochamat M, Cuhls H, Peuckmann‐Post V, Minton O, Stone P, et al. Pharmacological treatments for fatigue associated with palliative care. Cochrane Database Syst Rev 2015;5:CD006788:. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Peuckmann‐Post V, Elsner F, Krumm N, Trottenberg P, Radbruch L. Pharmacological treatments for fa‐tigue associated with palliative care. Cochrane Database of Systematic Reviews 2010, Issue 11 Art. No.: CD006788. DOI:10.1002/14651858.CD006788.pub2 [DOI] [PubMed] [Google Scholar]
- 20. Rabkin JG, Gordon PH, McElhiney M, Rabkin R, Chew S, Mitsumoto H. Modafinil treatment of fatigue in patients with ALS: a placebo‐controlled study. Muscle Nerve 2009;39:297–303. [DOI] [PubMed] [Google Scholar]
- 21. Jean‐Pierre P, Morrow GR, Roscoe JA, Heckler C, Mohile S, Janelsins M, et al. A phase 3 randomized, placebo‐controlled, double‐blind, clinical trial of the effect of modafinil on cancer‐related fatigue among 631 patients receiving chemotherapy: a University of Rochester Cancer Center Community Clinical Oncology Program Research base study. Cancer 2010;116:3513–3520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Morrow GR, Hickok JT, Roscoe JA, Raubertas RF, Andrews PLR, Flynn PJ, et al. Differential effects of paroxetine on fatigue and depression: a randomized, double‐blind trial from the University of Rochester Cancer Center Community Clinical Oncology Program. J Clin Oncol 2003;21:4635–4641. [DOI] [PubMed] [Google Scholar]
- 23. Bruera E, Valero V, Driver L, Shen L, Willey J, Zhang T, et al. Patient‐controlled methylphenidate for cancer fatigue: a double‐blind, randomized, placebo‐controlled trial. J Clin Oncol 2006;24:2073–2078. [DOI] [PubMed] [Google Scholar]
- 24. Butler JM, Case LD, Atkins J, Frizzell B, Sanders G, Griffin P, et al. A phase III, double‐blind, placebo‐controlled prospective randomized clinical trial of d‐threo‐methylphenidate HCl in brain tumor patients receiving radiation therapy. Int J Radiat Oncol Biol Phys 2007;69:1496–1501. [DOI] [PubMed] [Google Scholar]
- 25. Stankoff B, Waubant E, Confavreux C, Edan G, Debouverie M, Rumbach L, et al. Modafinil for fatigue in MS: a randomized placebo‐controlled double‐blind study. Neurology 2005;64:1139–1143. [DOI] [PubMed] [Google Scholar]
- 26. von Haehling S, Morley JE, Coats AJS, Anker SD. Ethical guidelines for publishing in the Journal of Cachexia, Sarcopenia and Muscle: update 2015. J Cachexia Sarcopenia Muscle 2015;6:315–316. [DOI] [PMC free article] [PubMed] [Google Scholar]


