Abstract
Objective
To examine the willingness to accept new Medicaid patients among certified rural health clinics (RHCs) and other nonsafety net rural providers.
Data Sources
Experimental (audit) data from a 10‐state study of primary care practices, county‐level information from the Area Health Resource File, and RHC information from the Center for Medicare and Medicaid Services.
Study Design
We generate appointment rates for rural and nonrural areas by patient‐payer type (private, Medicaid, self‐pay) to then motivate our focus on within‐rural variation by clinic type (RHC vs. non‐RHC). Multivariate linear models test for statistical differences and assess the estimates’ sensitivity to the inclusion of control variables.
Data Collection
The primary data are from a large field study.
Principal Findings
Approximately 80 percent of Medicaid callers receive an appointment in rural areas—a rate more than 20 percentage points greater than nonrural areas. Importantly, within rural areas, RHCs offer appointments to prospective Medicaid patients nearly 95 percent of the time, while the rural (nonsafety net) non‐RHC Medicaid rate is less than 75 percent. Measured differences are robust to covariate adjustment.
Conclusions
Our study suggests that RHC status, with its alternative payment model, is strongly associated with new Medicaid patient acceptance. Altering RHC financial incentives may have consequences for rural Medicaid enrollees.
Keywords: Medicaid, rural health care, rural health clinics, primary care, audit methodology
Ensuring a sufficient supply of health care providers in rural areas has been a long‐standing health policy issue at the local and national levels (Newhouse 1990; Ricketts 2000; Rabinowitz et al. 2001; Brooks et al. 2002; Gamm et al. 2002; Gamm and Hutchison 2003; Pepper, Sandefer, and Gray 2010). Numerous studies and commentaries purport a lack of primary care providers in rural areas and inadequate access for local consumers (Ricketts 2000, 2005; Larson and Fleishman 2003)—although some evidence suggests gains in access over time (Rosenthal, Zaslavsky, and Newhouse 2005). Other work simultaneously claims that rural providers are burdened with heavier workloads as they attempt to address excess demand (Colwill and Cultice 2003; Weeks and Wallace 2008). With these concerns in mind, substantial resources and legislative efforts have been devoted to bolster the supply of providers in more remote places (Hart et al. 2002; Krist et al. 2005; Ricketts 2005; Rosenthal, Zaslavsky, and Newhouse 2005).
One specific policy response has been the rural health clinic (RHC) certification program, which began in 1977 and aims to boost rural provider availability for Medicare and Medicaid beneficiaries. Certified providers are given clinic‐specific cost‐based reimbursement for all services rendered to public payer patients, rather than having to accept a flat state (Medicaid) or federal (Medicare) payment rate.1 Receiving the Center for Medicare and Medicaid Services (CMS) RHC designation requires compliance with several mandates, such as some use of nonphysician clinicians, no federally qualified health center (FQHC) classification, and presence in an underserved nonurban area—with some flexibility and variance in this latter characteristic.2 Certification does not require the practice to accept patients irrespective of ability to pay—differentiating it from other safety net initiatives. Instead, the program is primarily an alternative payment model intended to improve access for rural patients relying on public insurance (Office of Inspector General 2005; Medicare Learning Network 2013).
As of 2003, the RHC certification program had expanded from a few hundred practices during its early years to more than 3,000 qualifying clinics and over $600 million in associated CMS spending in that year alone (Office of Inspector General 2005). The RHC population has continued to grow and now numbers close to 4,000 practices in total (Medicare Learning Network 2013). Despite the RHC program's rise in popularity with providers, there is sparse academic research on this topic. In one of the few examples, Kirkbride and Wallace (2009) also comment on the RHC program's long tenure but conspicuous absence of a robust literature evaluating its effects.
Within this work, we investigate the relationship between RHCs and their willingness to accept new Medicaid primary care patients. While the availability of new patient appointments is only one aspect of the much broader and more complex concept of “access,” this information can be used to partially track developments within the health care system as well as discuss policy priorities. Our study in turn relies on an audit methodology to measure the influence of insurance status on providers’ real‐time appointment granting behavior in a way that isolates differentials through a randomized study design; however, we first describe our assumptions and hypotheses regarding the RHC program and how it might influence the supply of appointments.
Conceptual Framework
Our underlying framework considers providers as economic actors responding to relevant prices and market conditions. The U.S. health care market can then be characterized as an amalgamation of privately negotiated and publicly set prices. Providers have some control over reimbursement rates for their privately insured patients, but they are “price takers” for publicly insured patients—prices that are often lower than those for private patients. Because providers cannot easily or sufficiently alter the cost of production for appointments to match payment variation across patients, theory predicts a profit‐maximizing practice will sell the marginal visit to the patient associated with the higher reimbursement (Sloan, Mitchell, and Cromwell 1978; Cromwell and Mitchell 1984)—and hence discriminate between customers based on price.
Sloan, Mitchell, and Cromwell (1978), and later Cromwell and Mitchell (1984), illustrate this point by describing physician practices as selling services to both a high‐paying (private) market and a low‐paying (Medicaid) market. The extent of providers’ participation in the former is driven by patients’ downward sloping demand curve. Involvement in the latter market is determined by a set Medicaid reimbursement—with higher fees generally corresponding to more Medicaid services supplied. Importantly, each of these insights has applications to urban–rural access differences as well as the implications of RHCs within rural markets.
Regarding urban–rural differences, it is generally accepted that the demand for medical care moves inversely with the patient's distance to the point of access (Newhouse et al. 1982; Newhouse 1990), and rural customers tend to travel more for care (Gamm et al. 2002; Hart et al. 2002; Hart, Larson, and Lishner 2005; Chan, Hart, and Goodman 2006). Rural health care consumers are also known to be poorer, less likely to have insurance, and less intense users of medical services overall (Newhouse 1990; Bronstein and Adams 2002; Gamm et al. 2002; Hart et al. 2002; Larson and Fleishman 2003; Hart, Larson, and Lishner 2005; Reschovsky and Staiti 2005; Chan, Hart, and Goodman 2006). Evidence even suggests that urban and rural residents diverge in beliefs about health and medical needs (Ricketts 2000; Mayer, Slifkin, and Cockrell Skinner 2005). Thus, the demand curve facing rural providers may differ from nonrural markets, and in particular, be shifted inward and/or more elastic.
With less demand from private patients, a Medicaid patient is more likely to be the marginal customer, and hence, the conceptual model predicts that the probability of receiving an appointment would be relatively higher for a prospective rural Medicaid patient. Consistent with this intuition, existing literature shows rural providers have a larger fraction of their payer mix occupied by Medicaid enrollees, and some even label rural providers “dependent” on Medicaid customers (Bronstein and Adams 2002; Long, King, and Coughlin 2006). However, less private demand does not necessarily imply an absence of an access gap for Medicaid patients in rural markets—only a reduction in its magnitude.3
The presence of RHC practices suggests potential heterogeneity to be found within rural markets. Specifically, the program's reliance on a separate payment model may alter the financial incentives relevant to a given rural provider. Under the assumption that cost‐based reimbursement is more favorable, RHC‐certified providers may show a greater willingness to supply more visits to the Medicaid market—even when facing an identical payer mix and flow of patients as their non‐RHC (nonsafety net) peers.
While the relative pay differences between traditional Medicaid and the RHC cost‐based mechanism likely vary across markets (e.g., due to state Medicaid generosity differences and local provider negotiations), RHCs should generally receive higher fees given that entering into the program requires opting out of normal Medicaid and Medicare reimbursement channels. Their voluntary program participation implicitly suggests that the financial incentives are more appealing than prevailing fees from either traditional public payer model—and historically, Medicare payments for primary care have been more generous than Medicaid (Zuckerman, Williams, and Stockley 2009).
Methods
Data
The primary data for our measure of new patient appointment rates come from a simulated patient (audit) study conducted between November 2012 and April 2013. The simulated patient study used trained field staff posing as adults seeking primary care with a consistent script across calls except for a randomized characteristic: insurance status (privately insured, Medicaid insurance, and a self‐pay group lacking coverage). This design facilitates measuring differences by insurance status in the rate which primary care physician offices grant new patient appointments. The study's scope includes primary care offices across 10 states, which were selected for diversity along a number of dimensions (Arkansas, Georgia, Illinois, Iowa, Massachusetts, Montana, New Jersey, Oregon, Pennsylvania, and Texas). The development and testing of the sample frame and specifics of the research design are fully described elsewhere, along with the state‐level estimates (Rhodes et al. 2014).
Briefly, a current commercial database of practicing physicians and a preaudit (nonexperimental) survey identified all offices with at least one physician in primary care practice—creating the study's sample frame. The audit sample was then drawn, independently within patient insurance type (private, Medicaid, or self‐pay), from the pool of eligible offices based on the proportion of the population with that insurance type in the county. During the experimental portion of the study, callers were randomly assigned an insurance status and reason for contacting the office (i.e., requesting a routine checkup or told to follow up with a primary care provider following a recent high blood pressure screening). For private insurance, the plan with the highest market share in each office's county was used, and the self‐pay group was also independent of individual ability to pay (i.e., the self‐pay callers would accept an appointment irrespective of the required out‐of‐pocket amount, which could be large—see Rhodes et al. 2014 for related analyses and discussion). For Medicaid, the specific Medicaid managed care (MMC) insurance plan (or primary care case management [PCCM] plan when applicable) was identified primarily from the preaudit survey, supplemented with state insurer lists of Medicaid providers. MMC is also not foreign to many rural health care providers, despite much controversy and conflicting views on its potential costs and benefits (Ricketts 2000; Bronstein and Adams 2002; Silberman et al. 2002; Waitzkin et al. 2002; Hurley and Somers 2003).
Callers then contacted eligible practices to request the earliest possible appointment with a randomly chosen physician within the practice or any other available provider when the chosen provider was unavailable. Appointments were canceled before ending the call or immediately thereafter. We were unable to ascertain whether an appointment would be available for 12 percent of calls, mainly due to electronic scheduling systems. These administrative barriers were encountered at roughly the same rate for each insurance type within each state (12 percent for private and 13 percent for Medicaid across all states) and were subsequently dropped, yielding a sample of 11,347 completed cases for the three insurance types.
For this study, we also use county‐level information on the poverty rate, unemployment rate, primary care physician density, and health professional shortage areas (HPSAs) from the Area Health Resource File. We rely on the National Center for Health Statistics (NCHS) urban–rural classification system for counties. It is composed of six categories in total, with the final category (NCHS 6) capturing areas considered to be the most rural. We restrict our definition of rural to NCHS 6 areas, which are nonmetropolitan and have no town/city with 10,000 or more people (Ingram and Franco 2012).
We then use the CMS current list of RHC practices to determine which of our audit study rural clinics possess the necessary RHC certification.4 Note, due to the scope and intent of this study, we are deliberately restricting our attention to rural practices within the experimental data and not attempting to identify and compare RHCs in more populated counties where some may exist—see the Office of Inspector General (2005) report.
All 11,347 completed audit cases from the 10 states are eligible for inclusion in the analyses so long as the clinic is not an FQHC or FQHC “look‐alike” facility—although NJ has no calls to rural counties and MA has no calls to RHCs. In other work, we have demonstrated the importance of FQHCs and how their structure and conduct can significantly depart from non‐FQHC facilities (Richards et al. 2014). As RHCs are explicitly not safety net institutions, we compare them directly to other nonsafety net providers, excluding FQHC observations (570 calls in total—458 nonrural and 112 rural calls). Exactly, 394 additional caller‐practice observations are omitted due to incomplete information on provider mix (regression output that includes these observations is available in the Appendix). The missing information rate for rural RHCs and non‐RHCs is identical—approximately 1.5 percent. Our final analytical sample is 10,383 (4,947 private, 3,965 Medicaid, and 1,471 self‐pay). A total of 941 calls belong to rural areas (393 private, 380 Medicaid, and 168 self‐pay).
Rural to Nonrural Comparisons
Our key outcome throughout is a binary indicator for whether the practice schedules an appointment with the caller. We begin with a simple descriptive exercise comparing appointment rates at nonsafety net clinics to then setup our within‐rural area analytic focus.
We first calculate and display unadjusted mean appointment rates for each of the six county size (NCHS) categories and by patient‐payer type (private, Medicaid, and self‐pay). We then implement regression analyses, which provide statistical tests for any relative differences in appointment probabilities (by insurance type) revealed by the unadjusted rates. We use indicator variables for our Medicaid and self‐pay callers and compare them against privately insured callers along the urban–rural classification. Our linear probability models (LPMs) place nonrural counties as the geographic base category and then interact the Medicaid caller indicator with an indicator variable for the rural county location group—likewise for the self‐pay indicator (making privately insured the base insurance group). The interaction terms tell us if willingness to accept a new Medicaid or self‐pay patient is appreciably higher or lower inside rural areas when compared to private patients. For our main results, we estimated two specifications. The initial specification includes no other covariates, but the second model controls for caller demographics (including the reason for contacting the practice), clinic provider mix, county‐level poverty and unemployment rates, density of primary care physicians at the county level, and state fixed effects. Clinic provider mix is important as rural practices may be structured differently in terms of staff and total providers—which could also influence their appointment availability. The county controls can help net out any appointment variation due to environmental factors that may differ between rural and nonrural places. In this way, our first regression model provides statistical tests for any appointment rate gaps evident in the unadjusted data, while our second model assesses the sensitivity of the estimated gap to covariate inclusion.
Table SA2 provides alternative specifications with rural counties as the geographic omitted category and also uses a step‐wise introduction of covariates for comparison.
Within Rural Areas and RHCs
To more closely examine rural areas, we first construct unadjusted appointment rates for rural (nonsafety net) non‐RHCs (also partitioned by HPSA location) and RHCs for each of the three insurance groups. We then implement regression analyses to formally test any rate differentials observed in the unadjusted data as well as explore their robustness when control variables are added. The analytic approach closely follows the previous layout; however, the key variable is now an indicator for RHC status as opposed to rural location. Interacting the RHC indicator with the Medicaid indicator gives us a difference‐in‐differences (DD) estimate of its influence on Medicaid appointment availability within rural areas while controlling for its influence on private insurance appointment rates—similarly so for the self‐pay group. This design removes fixed provider differences between RHC and non‐RHC providers; however, it cannot account for any unobserved selection into RHC status that may favor Medicaid acceptance—we consider this more in our discussion and limitations section. The two LPMs for this subsample of calls proceed identically to the aforementioned specifications involving all urban–rural counties. In addition, the provider mix controls may be equally or more important as RHC program participants have certain requirements in relation to nonphysician clinician staffing (estimates from a step‐wise inclusion of covariates can be found in Table SA5).
There is also some latitude in what qualifies as an underserved area when applying for and receiving RHC certification. To assess the sensitivity of our results to clinic location, we impose a stricter definition of underserved on our data and estimate identical models that exclude any rural practices located outside of Health Resources and Services Administration (HRSA) designated underserved areas (i.e., partial and full HPSA rural counties). The intent is to compare clinics in similar contexts (e.g., payer mix and local socioeconomic status) and to ascertain that the findings within the first set of rural‐specific models are not driven by an atypical subset of non‐RHCs. In our data, 7 percent of RHCs are located outside of HPSAs compared to 21 percent of non‐RHC rural clinics.
Throughout the empirical analyses, the standard errors are clustered at the county level, and linear regression models are used due to ease of interpretation, the presence of interaction terms, and our intent to compare coefficients across models (Allison 1999; Ai and Norton 2003; Mood 2010). Observations are weighted based on the proportion of the population with the same insurance type within the county where the call was made.
Results
Table 1 provides summary statistics for practices by county size and then clinic type within rural areas. The proportion of practices with a small to moderate number of physicians is similar across all six county size columns, but rural areas have relatively few large practices. Rural practices also staff nonphysician clinicians (NPs and PAs) more frequently—nearly 70 percent of these practices have at least one nonphysician provider. At the county level, the average economic conditions are similar across groups, but the physician density sharply declines when moving from the most to least populated counties. Within rural counties, the RHC provider mix departs from their non‐RHC (nonsafety net) peers, with RHCs somewhat less likely to be solo‐physician practices and almost no RHCs lack nonphysician staff.5
Table 1.
Sample Characteristics for Each NCHS County Size Classification and Rural Clinic Group
| Clinic Characteristics | Large Central Metro (NCHS 1) | Large Fringe Metro (NCHS 2) | Medium Metro (NCHS 3) | Small Metro (NCHS 4) | Micropolitan (NCHS 5) | Rural (NCHS 6) | Within Rural Areas | ||
|---|---|---|---|---|---|---|---|---|---|
| Non‐RHC | RHC | ||||||||
| Not Underserved Area | Underserved Area | ||||||||
| Total calls | 1,997 | 3,587 | 1,893 | 1,021 | 944 | 941 | 138 | 454 | 349 |
| No. physicians | |||||||||
| 1 | 56.6 | 56.6 | 48.3 | 51.1 | 57.1 | 53.1 | 56.6 | 60.5 | 41.8 |
| 2–3 | 25.1 | 28.8 | 29.9 | 25.0 | 26.0 | 30.4 | 26.3 | 27.0 | 36.6 |
| 4–9 | 13.2 | 12.4 | 18.2 | 18.7 | 13.7 | 14.8 | 15.8 | 10.6 | 20.1 |
| 10 or more | 5.0 | 2.1 | 3.6 | 5.3 | 3.1 | 1.7 | 1.3 | 1.9 | 1.5 |
| No. nonphysician clinicians | |||||||||
| 0 | 66.8 | 59.8 | 51.6 | 46.9 | 46.0 | 31.7 | 43.4 | 46.0 | 7.7 |
| 1 | 18.0 | 22.2 | 26.1 | 26.9 | 25.7 | 34.3 | 31.6 | 28.1 | 43.8 |
| 2 | 6.7 | 9.8 | 12.8 | 13.7 | 15.5 | 21.2 | 15.8 | 15.2 | 31.4 |
| 3 | 3.0 | 3.9 | 4.8 | 5.1 | 6.1 | 7.1 | 5.3 | 6.1 | 9.3 |
| 4 or more | 5.5 | 4.2 | 4.7 | 7.3 | 6.8 | 5.6 | 3.9 | 4.6 | 7.7 |
| Poverty rate (%) | 16.7 | 9.3 | 14.3 | 16.1 | 17.6 | 16.9 | 15.3 | 17.0 | 17.4 |
| Unemployment rate (%) | 8.5 | 7.9 | 7.8 | 7.7 | 8.7 | 7.6 | 6.9 | 7.8 | 7.7 |
| Physician density (per 100K) | 83.5 | 64.6 | 65.8 | 64.3 | 48.0 | 39.9 | 45.5 | 40.3 | 37.4 |
Values are expressed in %. Sample restricted to non‐federally qualified health center (FQHC) clinics with no missing information. Nonphysician providers include full‐time nurse practitioners and physician assistants. Poverty, unemployment, and physician density rates correspond to clinic's county. Underserved areas are rural counties that are HRSA classified as full or partial health professional shortage area (HPSA) counties. RHC, rural health clinic.
Figure 1 displays the unadjusted appointment rates for the three experimental groups, stratified by county size. Across all rural and nonrural areas, privately insured callers receive an appointment roughly 85–90 percent of the time, with the self‐pay appointment rate slightly below. However, nonrural practices offer Medicaid patients an appointment less than 60 percent of the time, which contrasts with rural areas where the average Medicaid appointment rate is 80 percent. The descriptive patterns in Figure 1 are also insensitive to the inclusion of FQHC practices and those with missing information on provider mix (Table SA1). Broadly, our data patterns seem consistent with the notion that rural providers are more receptive to new Medicaid patients—as detailed in the existing literature.
Figure 1.
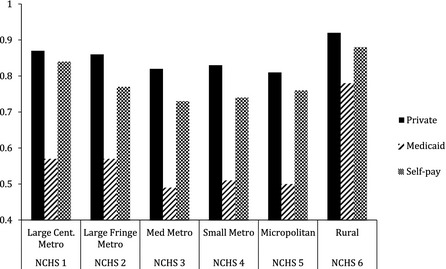
Unadjusted New Patient Primary Care Appointment Rates by Payer and NCHS Urban–Rural Classification
- Note. NCHS 6 represents rural areas. Audit sample restricted to non‐FQHC clinics without missing information on model covariates. Self‐pay appointment rates are independent of ability to pay the requested visit fee.
Within Table 2, we model the relationships seen in Figure 1 and test for differences in new patient acceptance rates by county size as well as differences in rates between the insurance groups. Even after covariate adjustment, Medicaid callers in rural counties are 13 percentage points less likely to receive an appointment (“Medicaid” noninteracted term added with the “Medicaid × Rural” interaction coefficient) compared to those with private insurance. However, there is a larger 30 percentage point appointment rate gap among the nonrural counties (“Medicaid” noninteracted coefficient). The rural interaction estimate is statistically significant at the 1 percent level and robust to the inclusion of covariates (column 2). The rural noninteracted term (“Rural” in Table 2) captures the urban–rural difference in the probability of receiving an appointment for privately insured callers. Column 1 suggests a 7 percentage point increase in the likelihood of acceptance for privately insured patients contacting rural clinics; however, after controlling for basic clinic and location characteristics (column 2), there is no clear evidence of a rural advantage for these patients. The self‐pay coefficients likewise offer no compelling indication of a rural differential, and Table SA3 provides estimates from alternative analytic samples, which incorporate the cases excluded from our main analyses. Overall, the regression estimates reinforce the Medicaid‐related patterns revealed in Figure 1 and help motivate our within‐rural empirical component.
Table 2.
Appointment Rate Differentials by Insurance Type with Rural Area Interactions (N = 10,383)
| (1) | (2) | |
|---|---|---|
| Medicaid | −0.307*** (0.017) | −0.309*** (0.017) |
| Self‐pay | −0.070*** (0.012) | −0.067*** (0.013) |
| Rural | 0.074*** (0.022) | 0.028 (0.025) |
| Medicaid × Rural | 0.173*** (0.033) | 0.175*** (0.032) |
| Self‐pay × Rural | 0.036 (0.028) | 0.037 (0.028) |
| Caller char. | Yes | |
| State FE | Yes | |
| Provider mix | Yes | |
| County‐level char. | Yes |
Sample restricted to calls to non‐FQHC clinics with no missing information on model covariates.
Omitted categories are nonrural (NCHS 1–5) counties and private insurance callers.
Caller controls include demographics and acute care scenario. Provider controls include number of physicians and nonphysician clinicians. County controls include the poverty rate, unemployment rate, and number of primary care physicians per 100,000 people.
Observation weights used; standard errors clustered at county level.
***p ≤ .01.
Figure 2 displays new patient appointment rate variation by rural clinic type. While the rates for privately insured and self‐pay patients are generally indistinguishable between clinic types, a large difference emerges for Medicaid patients. The unadjusted appointment rate for Medicaid callers falls by 20 percentage points or more (down to less than 75 percent) when seeking care at a non‐RHC facility. The consistency in the appointment rates for privately insured and self‐pay patients between RHC and non‐RHC providers also suggests that public payer patients are not crowding‐out other new patients for RHC providers.
Figure 2.
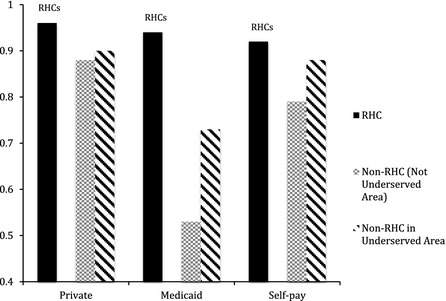
Unadjusted New Patient Appointment Rates by Rural Clinic Type
- Note. Sample restricted to non‐FQHC clinics without missing information on model covariates and located in NCHS classified rural areas. Note the sample sizes are much smaller and hence confidence intervals much larger for the second group (non‐RHC not in Underserved Areas). Self‐pay rates are independent of ability to pay the requested visit fee.
We formally assess the association between RHCs and rural Medicaid rates with our DD results in Table 3. RHCs have no detectable relationship with privately insured probabilities of appointment (“RHC Status” coefficient in column 2) but are associated with a 19 percentage point increase in the likelihood of a Medicaid caller receiving a new patient visit (“RHC Status” coefficient added to the “Medicaid × RHC” coefficient in column 2)—paralleling the gaps seen in the unadjusted data (Figure 2). Introducing controls for provider mix and county characteristics leave the estimates unchanged. No clear differential emerges for self‐pay patients.
Table 3.
Appointment Rate Differentials by Insurance Type and with RHC Interactions—All Rural Areas and Underserved Rural Areas
| Including All Rural Clinics (N = 941) | Rural Clinics in Underserved Areas (N = 781) | |||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Medicaid | −0.200*** (0.039) | −0.198*** (0.036) | −0.165*** (0.044) | −0.166*** (0.043) |
| Self‐pay | −0.030 (0.031) | −0.028 (0.030) | −0.013 (0.035) | −0.016 (0.035) |
| RHC status | 0.070*** (0.028) | 0.018 (0.029) | 0.065** (0.030) | 0.018 (0.031) |
| Medicaid × RHC | 0.176*** (0.044) | 0.174*** (0.041) | 0.147*** (0.049) | 0.147*** (0.047) |
| Self‐pay × RHC | −0.009 (0.052) | 0.002 (0.049) | −0.029 (0.056) | −0.008 (0.053) |
| Caller char. | Yes | Yes | ||
| State FE | Yes | Yes | ||
| Provider mix | Yes | Yes | ||
| County‐level char. | Yes | Yes | ||
Sample restricted to non‐FQHC clinics in rural areas (NCHS 6) with no missing information on model covariates.
Omitted categories are: privately insured group and the non‐RHC provider group.
Columns 1 and 2 include all rural areas in the sample.
Columns 3 and 4 restrict to counties that are full or partial HPSAs.
Caller controls include demographics and acute care scenario. Provider controls include number of physicians and nonphysician clinicians. County controls include the poverty rate, unemployment rate, and number of primary care physicians per 100,000 people.
Observation weights used, standard errors clustered at county level. ***p ≤ .01.
There is also no meaningful difference in new patient acceptance by insurance type among RHCs. The positive and precisely estimated interaction coefficient (“Medicaid × RHC” in Table 3) offsets the negative noninteracted Medicaid coefficient. Conversely, we find a 20 percentage point appointment rate difference between privately insured and Medicaid patients among the non‐RHC practices (“Medicaid” noninteracted coefficient in columns 1 and 2). In comparison to the previously reported findings from Table 2, these (nonsafety net) non‐RHCs are associated with a Medicaid‐to‐private appointment rate differential that is approximately two‐thirds of the measured gap found in more urban counties. Columns 3 and 4 exclude rural practices that are perhaps less comparable by restricting to HPSA‐located clinics. The statistical relationships mirror those in columns 1 and 2, and are likewise robust to the inclusion of practice‐level and county‐level confounders. Table SA7 provides results for modeling disparate appointment granting within clinics that received both private and Medicaid experimental calls (i.e., a paired analysis). The data patterns are consistent with our main findings; however, the much smaller sample sizes encourage cautious interpretation. In addition, Figure SA1 shows that both types of rural practices are highly likely to have Medicaid as part of their payer mix (>90 percent of contacted offices report this among RHCs and non‐RHCs)—suggesting that the RHC differential is primarily related to new patient acceptance, rather than Medicaid program participation.
Beyond appointment granting, we also note that the median number of calendar days (under a week) until the time of the scheduled visit is virtually the same across nonrural and rural practices as well as non‐RHCs and RHCs (these and other descriptive statistics can be found in Table SA8). Thus, higher willingness to accept new Medicaid patients does not appear to lead to longer waits for patients to actually be seen.
Discussion
Prior to the 2014 insurance expansions, our data from 10 states suggest that rural practices are equally likely to offer new patient appointments to privately insured callers when compared to more urban practices, and congruent with prior work, rural providers seem more willing to accept new Medicaid patients. However, our study's key finding is the heterogeneity revealed within rural areas. The supply of new patient appointments in rural areas appears influenced by the presence of RHCs, and RHCs grant appointments for Medicaid callers at rates on par with the privately insured. The RHC to non‐RHC differential in Medicaid rates also emerges despite almost all rural practices having Medicaid in their payer mix at baseline (Figure SA1). Thus, RHC status seems most correlated with practices’ intensive margin decisions (i.e., the willingness to expand their Medicaid patient panel further)—as opposed to the extensive margin (i.e., participating in Medicaid at all). One interpretation is that RHCs’ cost‐based reimbursement—and plausibly more favorable Medicaid prices—eliminates any supply‐side preference for the privately insured. In earlier work, Reschovsky and Staiti (2005) attribute rural providers’ greater affinity toward public payer patients to potential differences in social capital and norms between rural and urban places. Although our study does not encompass these less tangible phenomena, our findings appear more in line with economic actors responding to financial incentives.
Admittedly, our data cannot reveal what induces a practice to become an RHC or control for all possible differences across rural clinics. This cautions against causal interpretations, but it is worth repeating that our estimates are insensitive to two important mandates for RHCs—staffing requirements and underserved practice location. Moreover, arguing that RHCs are the practices that would still cater toward Medicaid customers absent their RHC status requires one to argue that the program is designed backward (i.e., rewarding practices for what they would have done anyway). If this is the case, then the RHC program functions only as an income transfer from taxpayers to RHC certified providers and leaves Medicaid beneficiary welfare unchanged. So while we can only claim that our results are consistent with RHC practices responding to more attractive Medicaid reimbursement policies, we also contend that this is a more likely explanation.
Other RHC‐centered work has been sparse and more confined in terms of geography or patient population. For example, there exists some limited evidence that RHCs decrease ambulatory sensitive conditions within a few states—though only for certain patient groups (Zhang et al. 2006; Probst, Laditka, and Laditka 2009); likewise, another study found RHCs deliver better preventive care for the diabetic subpopulation of Medicaid patients (Kirkbride and Wallace 2009). While this existing literature is valuable, our work provides a novel contribution that captures RHCs’ greater willingness to absorb new Medicaid patients relative to other nonsafety net practices in rural areas.
Despite our findings, the RHC program is a challenging policy lever to replicate. Cost‐based reimbursement for public payer beneficiaries can be an expensive access equalizer and would likely strain public coffers if extended to many practices or health care domains. At the same time, shrinking or removing the current set of RHC incentives may carry its own negative impact for rural patients. Some state Medicaid administrators recently called into question established RHC payment policies and are seeking potential changes (National Association of Medicaid Directors 2014). Considering our results and other work emphasizing the links between fees and the supply of Medicaid services (Baker and Royalty 2000; Cunningham and Cunningham 2005; Decker 2007, 2009; Buchmueller, Orzol, and Shore‐Sheppard 2013; Polsky et al. 2015), withdrawing enhanced RHC payments could induce RHCs to select new patients in a manner paralleling their non‐RHC peers—perhaps leaving rural Medicaid enrollees with fewer care options and/or greater travel distances between options. In addition, our findings imply that non‐RHCs would be unlikely to fully compensate for any shift away from new Medicaid patients by RHCs. Such consequences could be amplified if rural markets are also disproportionately affected by ongoing Medicaid expansions.
Limitations
Our study has several important limitations. We are only able to assess the rural new patient provider search experience in 10 states—though the states are diverse and improve upon other RHC studies using one or few states. The audit study design also limits experimental Medicaid calls to MMC or PCCM participating providers rather than all PCP practices, which may understate appointment rate differences between Medicaid and other patients. We also acknowledge that the audit data are only capturing one dimension of access (i.e., the supply of new patient appointments among randomly contacted providers) and are unable to speak to other clinic features, such as the quality of care provided or location convenience for patients. Relatedly, our data and analyses cannot reflect the extensive and complex supply‐and‐demand features that more broadly characterize rural health care delivery (e.g., the aggregate supply of providers, proximity of providers to patients, and size and health needs of the local population—which may also vary by insurance type). Other research has appropriately raised and examined these important issues. In addition, some of our first wave observations were collected in early 2013 (when the temporary Medicaid “Fee Bump” was intended to begin), but the enhanced Medicaid payments had yet to be implemented due to several unforeseen challenges (Wilk and Jones 2014). The data are also pre‐2014 Medicaid expansions, which partly highlights the importance of tracking rural patient and provider experiences during the coming years.
Finally, our data do not allow us to adequately assess the impact of becoming an RHC and therefore can only offer what we find to be a compelling interpretation of our results.6 Because the audit study is focused solely on the provision of new patient visits, we also cannot assess overall efficiency and importance of RHCs. Some recent work suggests that there are opportunities to increase efficiency even within the RHC group (Ortiz et al. 2011).
Conclusion
The United States is diverse in its geography and skewed in its accompanying supply of providers. This has been a source of concern, debate, and policy effort for decades and continues to be in the present. While the RHC Services Act of 1977 is a long‐standing program, little has been done to evaluate its effects on patients’ actual health care experiences. Relatedly, others have suggested that improved provider fees could boost rural patient access (Miller and Zuckerman 1991; Weeks and Wallace 2008), but this has rarely been tested directly. The RHC program operates an alternative payment method for providers and therefore offers insights about the importance of reimbursements within rural health care settings.
While our data indicate that rural practices are commonly part of Medicaid provider networks, RHC certification status is associated with substantial variation in the willingness to actually accept a new Medicaid patient. In fact, non‐RHC rural primary care practices exhibit a degree of selection against Medicaid patients in favor of privately insured patients comparable to their nonrural counterparts. As policy makers contemplate the roles of provider payments in the midst of many contemporary shifts in the U.S. health care system, we offer compelling evidence that they are powerful even within markets already accustomed to a sizable Medicaid presence and less demand from privately insured patients. Similarly, any subsequent rural health policy changes involving Medicaid fees will have to consider the tradeoff between budget management and ensuring sufficient appointment availability for new enrollees.
Supporting information
Appendix SA1: Author Matrix.
Figure SA1: Rates of Practices That Report Having Medicaid as Part of Their Insurance Mix by NCHS Urban–Rural Classification and Rural Clinic Type from Preexperimental Call through Screen.
Figure SA2: Unadjusted Medicaid Appointment Rates by Rural Clinic Type and HPSA Designation.
Table SA1: Unadjusted Appointment Rates by County Size and Sensitivity to Excluding FQHCs or Observations with Missing Covariate Information.
Table SA2: Appointment Rate Differentials by Insurance Type with NCHS Classification Interactions Using Rural Areas (NCHS 6) as the Base Category.
Table SA3: Sensitivity to Missing Observation or FQHC Exclusion From Core Models.
Table SA4: Number of Calls in Each State by Rural Clinic Type.
Table SA5: Appointment Rate Differentials and the Impact of RHCs within All Rural Areas (Panel A) and Underserved Rural Areas (Panel B).
Table SA6: Excluding Provider Mix Variables to Recover Fourteen Missing Observations from Core Models.
Table SA7: Probability of Disparate Appointment Granting for Clinics that Received Both Private and Medicaid Experimental Calls.
Table SA8: Additional Unadjusted Summary Statistics by County Location and Rural Clinic Type.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors gratefully acknowledge the Robert Wood Johnson Foundation (grant 70160) for its generous funding of the ongoing audit study project and thank the many excellent team members contributing to this larger research effort, including Ari Friedman, Douglas Wissoker, and David Chearo. Brendan Saloner also thanks the Robert Wood Johnson Foundaton's Health and Society Scholar program for supporting him during part of this work.
Disclosures: None.
Disclaimers: None.
Notes
This also applies to Medicare and Medicaid patients under associated managed care plans.
The Office of Inspector General (2005) report provides a thorough review of the RHC program and also highlights geographic variation in RHC locations.
Remaining differences could be the result of additional transaction costs associated with the Medicaid program or future policy uncertainty.
The updated list (as of summer 2013) can be downloaded via the CMS link (http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/rhclistbyprovidername.zip).
While 7.7 percent of RHCs reported no nonphysician clinicians, our measure does not capture Certified Nurse Midwives—who can fulfill the requirement. Also, our survey did not distinguish between full‐time and part‐time staff, which could lead to respondent confusion. Finally, as our study was not an audit of RHC compliance, no confirmation questions were executed.
Additional RHC to non‐RHC descriptive comparisons, including prices quoted to self‐pay patients receiving appointments, are available in the Appendix.
References
- Ai, C. , and Norton E. C.. 2003. “Interaction Terms in Logit and Probit Models.” Economic Letters 80: 123–9. [Google Scholar]
- Allison, P. D. 1999. “Comparing Logit and Probit Coefficients across Groups.” Sociological Methods & Research 28 (2): 186–208. [Google Scholar]
- Baker, L. C. , and Royalty A. B.. 2000. “Medicaid Policy, Physician Behavior, and Health Care for the Low‐Income Population.” Journal of Human Resources 35 (3): 480–502. [Google Scholar]
- Bronstein, J. M. , and Adams E. K.. 2002. “Rural‐Urban Differences in Health Risks, Resource Use and Expenditures within Three State Medicaid Programs: Implications for Medicaid Managed Care.” Journal of Rural Health 18 (1): 38–48. [DOI] [PubMed] [Google Scholar]
- Brooks, R. G. , Walsh M., Mardon R. E., Lewis M., and Clawson A.. 2002. “The Roles of Nature and Nurture in the Recruitment and Retention of Primary Care Physicians in Rural Areas: A Review of the Literature.” Academic Medicine 77 (8): 790–8. [DOI] [PubMed] [Google Scholar]
- Buchmueller, T. C. , Orzol S., and Shore‐Sheppard L. D.. 2013. “The Effect of Medicaid Payment Rates on Access to Dental Care Among Children.” American Journal of Health Economics 1 (2): 194–223. [Google Scholar]
- Chan, L. , Hart L. G., and Goodman D. C.. 2006. “Geographic Access to Health Care for Rural Medicare Beneficiaries.” Journal of Rural Health 22 (2): 140–6. [DOI] [PubMed] [Google Scholar]
- Colwill, J. M. , and Cultice J. M.. 2003. “The Future Supply of Family Physicians: Implications for Rural America.” Health Affairs 22 (1): 190–8. [DOI] [PubMed] [Google Scholar]
- Cromwell, J. , and Mitchell J. B.. 1984. “An Economic Model of Large Medicaid Practices.” Health Services Research 19 (2): 197–218. [PMC free article] [PubMed] [Google Scholar]
- Cunningham, J. , and Cunningham P. J.. 2005. “The Effects of Medicaid Reimbursement on the Access to Care of Medicaid Enrollees: A Community Perspective.” Medical Care Research and Review 62 (6): 676–96. [DOI] [PubMed] [Google Scholar]
- Decker, S. L. 2007. “Medicaid Physician Fees and the Quality of Medical Care of Medicaid Patients in the USA.” Review of Economics of the Household 5: 95–112. [Google Scholar]
- Decker, S. L. 2009. “Changes in Medicaid Physician Fees and Patterns of Ambulatory Care.” Inquiry 46: 291–304. [DOI] [PubMed] [Google Scholar]
- Gamm, L. , and Hutchison L.. 2003. “Rural Health Priorities in America: Where You Stand Depends on Where You Sit.” Journal of Rural Health 19 (3): 209–13. [DOI] [PubMed] [Google Scholar]
- Gamm, L. , Hutchison L., Bellamy G., and Dabney B. J.. 2002. “Rural Health People 2010: Identifying Rural Health Priorities and Models for Practice.” Journal of Rural Health 18 (1): 9–14. [DOI] [PubMed] [Google Scholar]
- Hart, L. G. , Larson E. H., and Lishner D. M.. 2005. “Rural Definitions for Health Policy and Research.” American Journal of Public Health 95 (7): 1149–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart, L. G. , Salsberg E., Phillips D. M., and Lishner D. M.. 2002. “Rural Health Care Providers in the United States.” Journal of Rural Health 18 (Supplemental): 211–32. [DOI] [PubMed] [Google Scholar]
- Hurley, R. E. , and Somers S. A.. 2003. “Medicaid and Managed Care: A Lasting Relationship?” Health Affairs 22 (1): 77–88. [DOI] [PubMed] [Google Scholar]
- Ingram, D. D. , and Franco S. J.. 2012. “NCHS Urban‐Rural Classification Scheme for Counties.” Vital Health Statistics. Hyattsville, MD: Center for Disease Control and Prevention, National Center for Health Statistics, US Department of Health and Human Services. [Google Scholar]
- Kirkbride, K. , and Wallace N.. 2009. “Rural Health Clinics and Diabetes‐Related Primary Care for Medicaid Beneficiaries in Oregon.” Journal of Rural Health 25 (3): 247–52. [DOI] [PubMed] [Google Scholar]
- Krist, A. H. , Johnson R. E., Callahan D., Woolf S. H., and Marsland D.. 2005. “Title VII Funding and Physician Practice in Rural or Low‐Income Areas.” Journal of Rural Health 21 (1): 3–11. [DOI] [PubMed] [Google Scholar]
- Larson, S. L. , and Fleishman J. A.. 2003. “Rural‐Urban Differences in Usual Source of Care and Ambulatory Service Use: Analyses of National Data Using Urban Influence Codes.” Medical Care 41 (7): 65–74. [DOI] [PubMed] [Google Scholar]
- Long, S. K. , King J., and Coughlin T. A.. 2006. “The Health Care Experiences of Rural Medicaid Beneficiaries.” Journal of Health Care for the Poor and Underserved 17: 575–91. [DOI] [PubMed] [Google Scholar]
- Mayer, M. L. , Slifkin R. T., and Cockrell Skinner A.. 2005. “The Effects of Rural Residence and Other Social Vulnerabilities on Subjective Measures of Unmet Need.” Medical Care Research and Review 62: 617–28. [DOI] [PubMed] [Google Scholar]
- Medicare Learning Network . 2013. Rural Health Clinic: Rural Health Fact Sheet Series. Washington, DC: CMS and DHHS. [Google Scholar]
- Miller, M. E. , and Zuckerman S.. 1991. “Comparing Urban and Rural Physicians.” Health Affairs 10 (4): 243–53. [DOI] [PubMed] [Google Scholar]
- Mood, C. 2010. “Logistic Regression: Why We Cannot Do What We Think We Can Do, and What We Can Do about It.” European Sociological Review 26 (1): 67–82. [Google Scholar]
- National Association of Medicaid Directors . 2014. NAMD Informational Brief: Medicaid and the Federally Qualified Health Center and Rural Health Clinic Programs: Alignment and Modernization Opportunities. Washington, DC: National Association of Medicaid Directors (NAMD). [Google Scholar]
- Newhouse, J. P. 1990. “Geographic Access to Physician Services.” Annual Review of Public Health 11: 207–30. [DOI] [PubMed] [Google Scholar]
- Newhouse, J. P. , Williams A. P., Bennett B. W., and Schwartz W. B.. 1982. “Does the Geographical Distribution of Physicians Reflect Market Failure?” Bell Journal of Economics 13 (2): 493–505. [Google Scholar]
- Office of Inspector General . 2005. Status of the Rural Health Clinic Program. Washington, DC: DHHS. [Google Scholar]
- Ortiz, J. , Meemon N., Tang C.‐Y., Wan T. T. H., and Chun Paek S.. 2011. “Rural Health Clinic Efficiency and Effectiveness: Insight from a Nationwide Survey.” Journal of Medical Systems 35: 671–81. [DOI] [PubMed] [Google Scholar]
- Pepper, C. M. , Sandefer R. H., and Gray M. J.. 2010. “Recruiting and Retaining Physicians in Very Rural Areas.” Journal of Rural Health 26: 196–200. [DOI] [PubMed] [Google Scholar]
- Polsky, D. , Richards M., Basseyn S., Wissoker D., Kenney G. M., Zuckerman S., and Rhodes K. V.. 2015. “Appointment Availability after Increases in Medicaid Payments for Primary Care.” NEJM 372: 537–45. [DOI] [PubMed] [Google Scholar]
- Probst, J. C. , Laditka J. N., and Laditka S. B.. 2009. “Association Between Community Health Center and Rural Health Clinic Presence and County‐Level Hospitalization Rates for Ambulatory Care Sensitive Conditions: An Analysis across Eight US States.” BMC Health Services Research 9 (134): 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabinowitz, H. K. , Diamond J. J., Markham F. W., and Paynter N. P.. 2001. “Critical Factors for Designing Programs to Increase the Supply and Retention of Rural Primary Care Physicians.” JAMA 286: 1041–8. [DOI] [PubMed] [Google Scholar]
- Reschovsky, J. D. , and Staiti A. B.. 2005. “Access and Quality: Does Rural America Lag Behind?” Health Affairs 24 (4): 1128–39. [DOI] [PubMed] [Google Scholar]
- Rhodes, K. V. , Kenney G. M., Friedman A. B., Saloner B., Lawson C. C., Chearo D., Wissoker D., and Polsky D.. 2014. “Primary Care access for New Patients on the Eve of Health Care Reform.” JAMA — Internal Medicine 174 (6): 861–9. [DOI] [PubMed] [Google Scholar]
- Richards, M. R. , Saloner B., Kenney G. M., Rhodes K. V., and Polsky D.. 2014. “Access Points for the Underserved: Primary Care Appointment Availability at Federally Qualified Health Centers in Ten States.” Medical Care 52 (9): 818–25. [DOI] [PubMed] [Google Scholar]
- Ricketts, T. C. 2000. “The Changing Nature of Rural Health Care.” Annual Review of Public Health 21: 639–57. [DOI] [PubMed] [Google Scholar]
- Ricketts, T. C. 2005. “Workforce Issues in Rural Areas: A Focus on Policy Equity.” American Journal of Public Health 95 (1): 42–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal, M. B. , Zaslavsky A., and Newhouse J. P.. 2005. “The Geographic Distribution of Physicians Revisited.” Health Services Research 40 (6): 1931–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silberman, P. , Poley S., James K., and Slifkin R.. 2002. “Tracking Medicaid Managed Care in Rural Communities: A Fifty‐State Follow‐Up.” Health Affairs 21 (4): 255–63. [DOI] [PubMed] [Google Scholar]
- Sloan, F. A. , Mitchell J. B., and Cromwell J.. 1978. “Physician Participation in State Medicaid Programs.” Journal of Human Resources 13 (NBER Supplemental): 211–45. [PubMed] [Google Scholar]
- Waitzkin, H. , Williams R. L., Bock J. A., McCloskey J., Willging C., and Wagner W.. 2002. “Safety‐Net Institutions Buffer the Impact of Medicaid Managed Care: A Multi‐Method Assessment in a Rural State.” American Journal of Public Health 92 (4): 598–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weeks, W. B. , and Wallace A. E.. 2008. “Rural‐Urban Differences in Primary Care Physicians’ Practice Patterns, Characteristics, and Incomes.” Journal of Rural Health 24 (2): 161–70. [DOI] [PubMed] [Google Scholar]
- Wilk, A. S. , and Jones D. K.. 2014. “To Extend or Not to Extend the Primary Care ‘Fee Bump’ in Medicaid?” Journal of Health Politics, Policy, and Law 39 (6): 1263–75. [DOI] [PubMed] [Google Scholar]
- Zhang, W. , Mueller K. J., Chen L.‐W., and Conway K.. 2006. “The Role of Rural Health Clinics in Hospitalization due to Ambulatory Care Sensitive Conditions: A Study of Nebraska.” Journal of Rural Health 22 (3): 220–3. [DOI] [PubMed] [Google Scholar]
- Zuckerman, S. , Williams A. F., and Stockley K. E.. 2009. “Trends in Medicaid Physician Fees, 2003–2008.” Health Affairs 28 (3): w510–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Figure SA1: Rates of Practices That Report Having Medicaid as Part of Their Insurance Mix by NCHS Urban–Rural Classification and Rural Clinic Type from Preexperimental Call through Screen.
Figure SA2: Unadjusted Medicaid Appointment Rates by Rural Clinic Type and HPSA Designation.
Table SA1: Unadjusted Appointment Rates by County Size and Sensitivity to Excluding FQHCs or Observations with Missing Covariate Information.
Table SA2: Appointment Rate Differentials by Insurance Type with NCHS Classification Interactions Using Rural Areas (NCHS 6) as the Base Category.
Table SA3: Sensitivity to Missing Observation or FQHC Exclusion From Core Models.
Table SA4: Number of Calls in Each State by Rural Clinic Type.
Table SA5: Appointment Rate Differentials and the Impact of RHCs within All Rural Areas (Panel A) and Underserved Rural Areas (Panel B).
Table SA6: Excluding Provider Mix Variables to Recover Fourteen Missing Observations from Core Models.
Table SA7: Probability of Disparate Appointment Granting for Clinics that Received Both Private and Medicaid Experimental Calls.
Table SA8: Additional Unadjusted Summary Statistics by County Location and Rural Clinic Type.


