Abstract
Heparin-induced thrombocytopaenia (HIT) is a life-threatening complication of exposure to heparin. It is mediated by autoantibodies to platelet factor-4 causing platelet activation, destruction and thrombosis. Given their rich arterial supply and a single central vein, the adrenal glands are particularly susceptible to congestive haemorrhage following venous thrombosis. We report a case of bilateral adrenal haemorrhage (BAH) associated with HIT following prophylactic use of unfractionated heparin for venous thromboembolism causing adrenal insufficiency. BAH is a life-threatening paradoxical complication associated with HIT, a prothrombotic state. The resulting adrenal insufficiency can lead to haemodynamic collapse if unrecognised. Early diagnosis, in the wake of vague symptoms, and prompt treatment primarily aimed at repletion of glucocorticoids and close monitoring of enlarging haemorrhage is of utmost importance. Likewise, early identification of HIT is important to prevent potential complications including adrenal haemorrhage.
Background
Heparin-induced thrombocytopaenia (HIT) occurs in ∼0.5–5% of patients treated with heparin, depending on various factors, including the patient population and heparin type used.1 While heparin was discovered in the 1930s, HIT was not reported until the 1960s and 1970s.2 It is mediated by autoantibodies to platelet factor-4 complexed with heparins that initiate antibody-induced platelet activation leading to the development of thrombocytopaenia with thrombosis or disseminated intravascular coagulation.3–5 Once HIT is recognised, an alternative anticoagulant should be initiated to prevent further complications.6
The adrenal glands are unique in that they have a rich arterial supply and a single central vein, making them particularly susceptible to congestive haemorrhage following venous thrombosis.7 HIT associated adrenal haemorrhage tends to be bilateral, causing severe clinical manifestations including haemodynamic collapse.8 9 Early diagnosis and prompt treatment is crucial, as undiagnosed cases tend to be fatal.
Case presentation
A 76-year-old woman with a medical history of rheumatoid arthritis (RA) and hypothyroidism presented initially to the emergency department with fatigue, abdominal pain, nausea, diarrhoea and generalised weakness for 4 days. She had been taken off chronic prednisone therapy recently, tapered over a 2-month period after being on a maintenance dose of 30 mg daily for the preceding 8 months. She was admitted to the hospital for further work up including a CT of the abdomen, which showed normal adrenal glands. Over the next 2 days, her condition improved and she was discharged home on oral prednisone 30 mg daily. She received prophylactic unfractionated heparin subcutaneously at a dose of 5000 units every 8 h during this hospitalisation.
She presented again to the ED 10 days later with extreme weakness and listlessness. Vital signs included a heart rate of 101 bpm and blood pressure of 102/54 mm Hg. Physical examination was unremarkable, and her abdomen was soft and non-tender. Basic blood tests revealed mild hyponatraemia (Na: 124 mmol/L), with normal potassium (4.7 mmol/L) and glucose (6.2 mmol/L) levels. Her platelet count had dropped from 187 to 62 k/mm3, raising suspicion for HIT. Heparin-induced platelet aggregation studies were borderline positive; however, serotonin release assay was positive confirming a diagnosis of HIT. The patient was started on argatroban, a direct thrombin inhibitor, infusion with partial thromboplastin time monitoring and dose adjustment per protocol.
Given her persistent sinus tachycardia and her procoagulable state, CT angiogram of the lungs was ordered to rule out a pulmonary embolism. Although no embolus was detected, the CT scan incidentally revealed bilateral adrenal masses suspicious of haemorrhage (figure 1). These masses were not seen on the CT scan during the previous admission. A subsequent MRI confirmed bilateral adrenal haemorrhage (BAH) (figure 2). Adrenocorticotropic hormone (ACTH) stimulation revealed low serum cortisol at 44 nmol/L and the patient was started on intravenous hydrocortisone. Given her stable haemoglobin and no evidence of ongoing bleeding, the argatroban infusion was maintained. This was later discontinued after adequate bridging to warfarin for 3 days with a target international normalised ratio of 2–3. A repeat MRI carried out at the time of discharge showed no progression in the size of the adrenal haemorrhages. The patient was discharged on oral hydrocortisone 20 mg daily in two divided doses and advised to avoid all forms of heparin products in the future.
Figure 1.

CT of the chest with contrast showing large bilateral adrenal masses (arrows).
Figure 2.
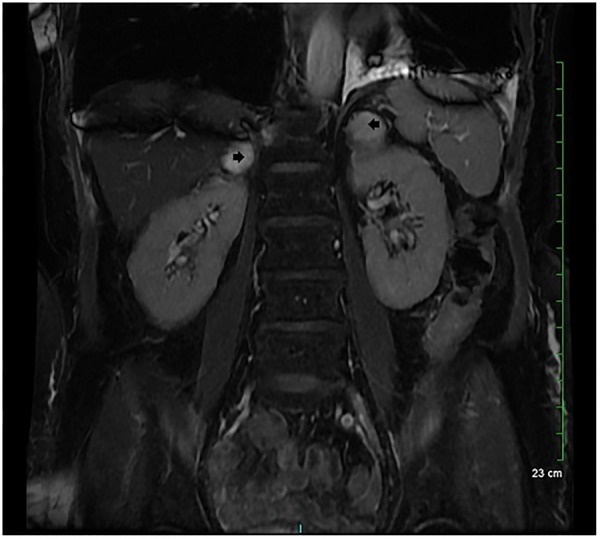
MRI of the abdomen confirming bilateral adrenal haemorrhage (arrows).
Discussion
BAH is a life-threatening complication associated with a prothrombotic state of HIT, which can result in adrenal insufficiency and haemodynamic collapse.10 A high index of clinical suspicion is required for diagnosing BAH as initial presentation can often be non-specific and patients may exhibit a wide array of symptoms ranging from fatigue, nausea, vomiting and abdominal pain, to overt haemodynamic instability.7
BAH associated with HIT was first described by Findling et al11 in 1987, in two case reports; since then, it has become increasingly well-documented. A literature search conducted in 2011 at the University of Virginia found 17 case reports of HIT associated BAH, all presenting with complete haemodynamic collapse.9 The majority of these cases occurred in association with unfractionated heparin (16 of 18 cases), while one case was associated with enoxaparin and one was associated with dalteparin. Fever and abdominal pain were the most common manifestations. Adrenal insufficiency was confirmed by corticotropin-stimulation test in 12 cases and adrenal haemorrhage was seen on CT imaging in 14 cases. There were five deaths resulting in an overall mortality rate of 27%, however, the mortality rate was 100% in the three cases where adrenal insufficiency went unrecognised.12–15
Formation of HIT antibodies typically requires 4 or more days of exposure to heparins and presents with a dropping platelet count within 5–14 days. In addition to a high index of clinical suspicion, a variety of assays are available for the diagnosis of HIT, including the platelet aggregation test, serotonin release assay and enzyme immunoassay.16 Once a diagnosis of HIT is suspected, all heparin products, including low molecular weight heparin, should be discontinued immediately and an alternative anticoagulant such as argatroban should be started.6 The diagnosis of BAH should be confirmed anatomically and hormonally with CT or MRI and serum cortisol, in conjunction with a corticotropin-stimulation test, respectively. 17 Repletion of glucocorticoids and close monitoring of adrenal haemorrhage are parts of the mainstay of treatment. In cases with a high clinical suspicion for adrenal crisis, an initial dose of 50 mg of hydrocortisone should be administered immediately. This should be followed by repeat dosing of 50 mg of hydrocortisone every 6 h until there is clinical improvement.18
It is important to identify cases of HIT early to prevent potential complications including adrenal haemorrhage. The rapid clinical deterioration and potential for complete haemodynamic collapse from acute adrenal crisis requires a high degree of clinical suspicion, regardless of confounding factors and the complexity of the case. Our patient was on maintenance oral steroids for RA and this may have prevented her from developing severe haemodynamic collapse. Our case report aims to highlight the risk of BAH associated with HIT in patients receiving any form of heparin, a drug widely used for prevention of venous thromboembolism in the in-patient setting.
Learning points.
Heparin-induced thrombocytopaenia, a prothrombotic state, is commonly encountered in hospitalised patients, with the widespread use of heparin for venous thromboembolism prophylaxis.
Bilateral adrenal haemorrhage is a paradoxical complication of heparin-induced thrombocytopaenia that can lead to adrenal insufficiency and haemodynamic collapse.
Treatment is primarily aimed at repletion of deficient glucocorticoids and close monitoring for expanding adrenal haemorrhage.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Jang IK, Hursting MJ. When heparins promote thrombosis: review of heparin-induced thrombocytopenia. Circulation 2005;111:2671–83. 10.1161/CIRCULATIONAHA.104.518563 [DOI] [PubMed] [Google Scholar]
- 2.Kelton JG, Warkentin TE. Heparin-induced thrombocytopenia: a historical perspective. Blood 2008;112:2607–16. 10.1182/blood-2008-02-078014 [DOI] [PubMed] [Google Scholar]
- 3.Visentin GP, Ford SE, Scott JP et al. Antibodies from patients with heparin-induced thrombocytopenia/thrombosis are specific for platelet factor 4 complexed with heparin or bound to endothelial cells. J Clin Invest 1994;93:81–8. 10.1172/JCI116987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kelton JG, Smith JW, Warkentin TE et al. Immunoglobulin G from patients with heparin-induced thrombocytopenia binds to a complex of heparin and platelet factor 4. Blood 1994;83:3232–9. [PubMed] [Google Scholar]
- 5.Rauova L, Poncz M, McKenzie SE et al. Ultralarge complexes of PF4 and heparin are central to the pathogenesis of heparin-induced thrombocytopenia. Blood 2005;105:131–8. 10.1182/blood-2004-04-1544 [DOI] [PubMed] [Google Scholar]
- 6.Lubenow N, Eichler P, Lietz T et al. Lepirudin for prophylaxis of thrombosis in patients with acute isolated heparin-induced thrombocytopenia: an analysis of 3 prospective studies. Blood 2004;104:3072–7. 10.1182/blood-2004-02-0621 [DOI] [PubMed] [Google Scholar]
- 7.Arthur CK, Grant SJ, Murray WK et al. Heparin-associated acute adrenal insufficiency. Aust N Z J Med 1985;15:454–5. 10.1111/j.1445-5994.1985.tb02776.x [DOI] [PubMed] [Google Scholar]
- 8.Winter AG, Ramasamy R. Bilateral adrenal hemorrhage due to heparin-induced thrombocytopenia following partial nephrectomy—a case report. F1000Res 2014;3:24 10.12688/f1000research.3-24.v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenberger LH, Smith PW, Sawyer RG et al. Bilateral adrenal hemorrhage: the unrecognized cause of hemodynamic collapse associated with heparin-induced thrombocytopenia. Crit Care Med 2011;39:833–8. 10.1097/CCM.0b013e318206d0eb [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Warkentin TE, Safyan EL, Linkins LA. Heparin-induced thrombocytopenia presenting as bilateral adrenal hemorrhages. N Engl J Med 2015;372:492–4. 10.1056/NEJMc1414161 [DOI] [PubMed] [Google Scholar]
- 11.Findling JW, Korducki JM, Lahiri PK et al. Bilateral adrenal hemorrhage associated with heparin-induced thrombocytopenia. Wis Med J 1987; 86:27–9. [PubMed] [Google Scholar]
- 12.Rowland CH, Woodford PA, De Lisle-Hammond J et al. Heparin-induced thrombocytopenia-thrombosis syndrome and bilateral adrenal haemorrhage after prophylactic heparin use. Aust N Z J Med 1999;29:741–2. 10.1111/j.1445-5994.1999.tb01626.x [DOI] [PubMed] [Google Scholar]
- 13.[No authors listed] Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 49–1989. A 71-year-old man with thrombocytopenia and hypotension after resection of a colonic carcinoma. N Engl J Med 1989;321:1595–603. 10.1056/NEJM198912073212308 [DOI] [PubMed] [Google Scholar]
- 14.Souied F, Pourriat JL, Le Roux G et al. Adrenal hemorrhagic necrosis related to heparin-associated thrombocytopenia. Crit Care Med 1991;19:297–9. 10.1097/00003246-199102000-00033 [DOI] [PubMed] [Google Scholar]
- 15.Weyrich P, Balletshofer B, Hoeft S et al. Acute adrenocortical insufficiency due to heparin-induced thrombocytopenia with subsequent bilateral haemorrhagic infarction of the adrenal glands. Vasa 2001;30:285–8. 10.1024/0301-1526.30.4.285 [DOI] [PubMed] [Google Scholar]
- 16.Lee GM, Arepally GM. Diagnosis and management of heparin-induced thrombocytopenia. Hematol Oncol Clin North Am 2013;27:541–63. 10.1016/j.hoc.2013.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rao RH, Vagnucci AH, Amico JA. Bilateral massive adrenal hemorrhage: early recognition and treatment. Ann Intern Med 1989;110:227–35. 10.7326/0003-4819-110-3-227 [DOI] [PubMed] [Google Scholar]
- 18.Cooper MS, Stewart PM. Corticosteroid insufficiency in acutely ill patients. N Engl J Med 2003;348:727–34. 10.1056/NEJMra020529 [DOI] [PubMed] [Google Scholar]


