Abstract
Segmental arterial mediolysis (SAM) is a non-arteriosclerotic, non-inflammatory arteriopathy characterised by dissecting aneurysms and most commonly found in abdominal arteries. A rupture of a visceral artery aneurysm is generally associated with high mortality. We present the case of a 57-year-old woman with a rupture of an intrahepatic aneurysm that led to intra-abdominal haemorrhage. The patient was surgically treated by evacuating the abdominal haematoma and ligature of the right hepatic artery. Histology of the right hepatic artery revealed the diagnosis of SAM. Six months postoperatively, the patient was in excellent physical condition with normal liver function and arterial blood flow of the right hepatic sections over collateral circulation.
Background
Segmental arterial mediolysis (SAM) is a non-atherosclerotic, non-inflammatory arteriopathy that typically affects medium-sized abdominal arteries. The medial layer undergoes a vacuolisation and lysis of unknown aetiology, which leads to dissection and aneurysm of the arterial wall.1
Patients with symptomatic SAM may present with non-specific, often self-limiting abdominal pain or severe pain with intra-abdominal haemorrhage.1 A rupture of the aneurysm is commonly compounded with life-threatening abdominal haemorrhage, resulting in mortality rates up to 50%.2 Successful treatment depends on the clinical findings and ranges from conservative medical therapy involving control of hypertension to an endovascular procedure or surgical intervention.2
We report on the rare incident of a patient with a large liver haematoma due to a ruptured aneurysm of the intrahepatic, right hepatic artery branches and discuss the different treatment options.
Case presentation
A 57-year-old woman presented with an acute onset of right upper abdominal pain and was admitted to a peripheral hospital, with a suspected symptomatic cholelithiasis. Shortly after admission, the patient was suddenly found unresponsive and in hypovolaemic shock.
Investigations
After successful resuscitation, a CT angiography (CTA) of the abdomen was performed, which revealed a large intrahepatic haematoma in segments 5 and 8, with perforation of the liver capsule (figure 1). The patient was transferred to our hospital immediately. The cause of the bleeding was a ruptured aneurysm of the right posterior intrahepatic artery branches. Additionally, several aneurysms of the right hepatic artery branches and an aneurysm of the coeliac trunk were identified (figure 2). The morphological pattern of the CTA was indicative of a SAM.
Figure 1.

CT angiography of the liver with a large intrahepatic haematoma in segments V and VIII.
Figure 2.
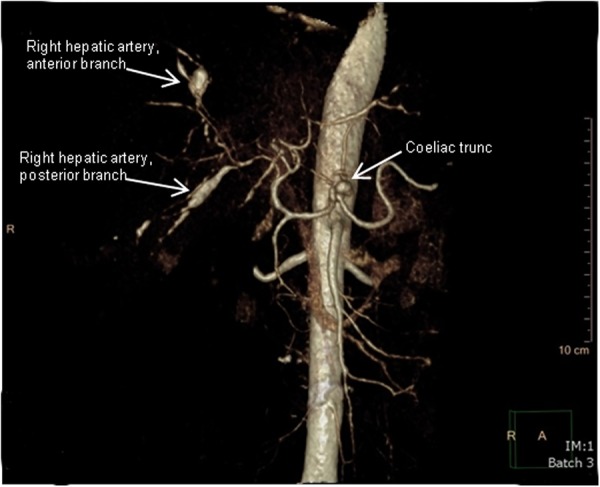
The CT angiography showed multiple aneurysms of the right hepatic artery and coeliac trunk.
Treatment
A catheter embolisation was considered to be too risky due to the possible arterial dissection of the aneurysm of the coeliac trunk. The patient developed an intra-abdominal compartment syndrome and an immediate transverse laparotomy was performed. Three litres of blood were evacuated and the right hepatic artery was ligated to prevent recurrent haemorrhage. A sample of the artery was taken for histological analysis. A cholecystectomy was performed during the same intervention.
The patient recovered quickly and was discharged 6 days after surgery. Histological findings of a right hepatic artery specimen confirmed the diagnosis of SAM showing a lysis of the arterial media with no signs of inflammation.
Outcome and follow-up
Six months postoperatively, the patient presented in good physical condition with normal blood test results and normal liver function. The CTA showed an almost complete resorption of the haematoma, with arterial blood flow in the right liver over collateral circulation (figure 3).
Figure 3.

CT angiography after 6 months showed a small residual haematoma in the liver. Note peripheral arterial blood flow in the right liver most probably due to intra- or extrahepatic collaterals.
Discussion
SAM is a rare but increasingly recognised vascular disease occurring in middle-aged patients and typically involving the coeliac artery and its branches, especially the splenic artery.2 The hepatic artery and in particular its intrahepatic branches are less commonly affected.2 3 The incidence of the disease is unclear, but most likely underestimated since an angiography is not a routine examination for patients presenting with abdominal pain.3 Only three cases of intra-abdominal haemorrhage related to SAM of the hepatic artery are reported in literature. One patient could be treated conservatively.4 In contrast, the two other patients underwent right hemihepatectomies. This major intervention was necessary to control either ongoing bleeding or to extract the ischaemic section of the liver after intra-arterial embolisation.5
The gold standard for the diagnosis of SAM is histopathological examination.6–8 Nonetheless, not all patients undergo surgery. Clinical criteria such as advanced age, no pre-existing inflammatory or arteriosclerotic vascular disease, sudden onset of intra-abdominal haemorrhage and ‘string-of-beads’ appearance of abdominal visceral arteries in the diagnostic imaging should raise suspicion for SAM.2 9 The patient presented in this report met all of the above-mentioned criteria and the histology of the right hepatic artery revealed pathognomonic lesions. Gaps in the arterial wall and fibrosis without inflammatory reaction are criteria that differentiate SAM from true vasculitis.7 10
Endovascular management with catheter angiography and embolisation have become important procedures in the treatment of arterial aneurysms, even in emergency settings.11 Successful endovascular management of SAM-associated aneurysms has been reported in a series of 21 patients, most commonly using coil embolisation techniques.12 However, considering potential complications of endovascular interventions, we refrained from coil embolisation in this patient. The aneurysm of the coeliac trunk was considered a potential risk factor for progressive arterial dissection after catheter manipulation.12–14 A selective embolisation of the right posterior branch may not have prevented further bleeding, because of multiple intrahepatic aneurysms in the entire right liver. Additionally, the patient developed an abdominal compartment syndrome, which was treated by decompressive laparotomy.
The closure of a hepatic artery is intricate. Major complications, which have been reported to be less than 5%, include liver abscess or bile duct injuries.15 The most serious is ischaemic liver failure, which may occur in 1% of patients after hepatic embolisation.16 Therefore, selective embolisation is mandatory in patients with underlying liver disease. A non-diseased liver usually tolerates an occlusion of one hepatic artery. The arterial blood flow of the liver contributes to only 25% of the total liver blood flow and the formation of extrahepatic and intrahepatic collateral circulation after arterial occlusion is well described.17 18 Typically, collaterals can arise from inferior phrenic arteries or gastroduodenal arteries, and supply the liver via the triangular ligaments and peribiliary arterial plexus, respectively.19 The CTA of the presented patient showed arterial vascularisation of the entire liver 6 months after closure of the right hepatic artery.
Learning points.
Patients with segmental arterial mediolysis of hepatic arteries can present with life-threatening intra-abdominal haemorrhage.
A CT angiography can supply appropriate imaging for early diagnosis in an emergency setting.
Surgery and endovascular intervention are the main treatment options.
Treatment options should remain interdisciplinary and tailored to each distinct clinical presentation.
Footnotes
Contributors: CB and CS edited, and FG and SB reviewed the report.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Pillai AK, Iqbal SI, Liu RW et al. Segmental arterial mediolysis. Cardiovasc Intervent Radiol 2014;37:604–12. 10.1007/s00270-014-0859-4 [DOI] [PubMed] [Google Scholar]
- 2.Yoshida H, Ukai K, Sugimura M et al. A case report of segmental arterial mediolysis in which computed tomography angiography was useful for diagnosis. Clin J Gastroenterol 2013;6:447–53. 10.1007/s12328-013-0433-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Michael M, Widmer U, Wildermuth S et al. Segmental arterial mediolysis: CTA findings at presentation and follow-up. AJR Am J Roentgenol 2006;187:1463–9. 10.2214/AJR.05.0281 [DOI] [PubMed] [Google Scholar]
- 4.Tomonaga T, Eguchi S, Hidaka M et al. A case of ruptured segmental arterial mediolysis of the hepatic artery: report of a case. Hepatogastroenterology 2011;58:1912–14. 10.5754/hge10177 [DOI] [PubMed] [Google Scholar]
- 5.Marshall L, O'Rourke T, McCann A et al. Spontaneous intrahepatic haemorrhage: two cases of segmental arterial mediolysis. ANZ J Surg 2015;85:49–52. 10.1111/ans.12304 [DOI] [PubMed] [Google Scholar]
- 6.Tameo MN, Dougherty MJ, Calligaro KD. Spontaneous dissection with rupture of the superior mesenteric artery from segmental arterial mediolysis. J Vasc Surg 2011;53:1107–12. 10.1016/j.jvs.2010.11.034 [DOI] [PubMed] [Google Scholar]
- 7.Horsley-Silva JL, Ngamruengphong S, Frey GT et al. Segmental arterial mediolysis: a case of mistaken hemorrhagic pancreatitis and review of the literature. JOP 2014;15:72–7. 10.6092/1590-8577/2036 [DOI] [PubMed] [Google Scholar]
- 8.Slavin RE, Yaeger MJ. Segmental arterial mediolysis--an iatrogenic vascular disorder induced by ractopamine. Cardiovasc Pathol 2012;21:334–8. 10.1016/j.carpath.2011.09.003 [DOI] [PubMed] [Google Scholar]
- 9.Uchiyama D, Koganemaru M, Abe T et al. A case of successful transcatheter arterial embolization for intraabdominal hemorrhage due to suspected segmental mediolytic arteriopathy. Jpn J Intervent Radiol 2005;20:278–81. [Google Scholar]
- 10.Baker-LePain JC, Stone DH, Mattis AN et al. Clinical diagnosis of segmental arterial mediolysis: differentiation from vasculitis and other mimics. Arthritis Care Res (Hoboken) 2010;62:1655–60. 10.1002/acr.20294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yoon T, Kwon T, Kwon H et al. Transcatheter arterial embolization of splenic artery aneurysms: a single-center experience. Vasc Specialist Int 2014;30:120–4. 10.5758/vsi.2014.30.4.120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shenouda M, Riga C, Naji Y et al. Segmental arterial mediolysis: a systematic review of 85 cases. Ann Vasc Surg 2014;28:269–77. 10.1016/j.avsg.2013.03.003 [DOI] [PubMed] [Google Scholar]
- 13.Dzieciuchowicz Ł, Snoch-Ziółkiewicz M, Oszkinis G et al. Superior mesenteric artery dissection as a complication of an endovascular attempt to treat aneurysms of the pancreaticoduodenal arteries. Interact Cardiovasc Thorac Surg 2015. 10.1093/icvts/ivv157 [DOI] [PubMed] [Google Scholar]
- 14.Mammen T, Joseph P, Sitaram V et al. Acute parent artery dissection as a complication of mesenteric endovascular coil embolisation for pancreatic pseudoaneurysm. Br J Radiol 2008;81:e7–10. 10.1259/bjr/33510361 [DOI] [PubMed] [Google Scholar]
- 15.Ramsey DE, Kernagis LY, Soulen MC et al. Chemoembolization of hepatocellular carcinoma. J Vasc Interv Radiol 2002;13(Pt 2):S211–21. 10.1016/S1051-0443(07)61789-8 [DOI] [PubMed] [Google Scholar]
- 16.Chan AO, Yuen MF, Hui CK et al. A prospective study regarding the complications of transcatheter intraarterial lipiodol chemoembolization in patients with hepatocellular carcinoma. Cancer 2002;94:1747–52. 10.1002/cncr.10407 [DOI] [PubMed] [Google Scholar]
- 17.Mine T, Murata S, Ueda T et al. Contribution of extrahepatic collaterals to liver parenchymal circulation after proper hepatic artery embolization. J Gastroenterol Hepatol 2014;29:1515–21. 10.1111/jgh.12571 [DOI] [PubMed] [Google Scholar]
- 18.Charnsangavej C, Chuang VP, Wallace S et al. Angiographic classification of hepatic arterial collaterals. Radiology 1982;144:485–94. 10.1148/radiology.144.3.6285413 [DOI] [PubMed] [Google Scholar]
- 19.Rappaport AM, Schneiderman JH. The function of the hepatic artery. Rev Physiol Biochem Pharmacol 1976;76:129–75. [DOI] [PubMed] [Google Scholar]


