Abstract
Objective: The purpose of this study was to examine similarities and differences between disruptive mood dysregulation disorder (DMDD) and bipolar disorder not otherwise specified (BP-NOS) in baseline sociodemographic and clinical characteristics and 36 month course of irritability in children 6–12.9 years of age.
Methods: A total of 140 children with DMDD and 77 children with BP-NOS from the Longitudinal Assessment of Manic Symptoms cohort were assessed at baseline, then reassessed every 6 months for 36 months.
Results: Groups were similar on most sociodemographic and baseline clinical variables other than most unfiltered (i.e., interviewer-rated regardless of occurrence during a mood episode) Young Mania Rating Scale (YMRS) and parent-reported General Behavior Inventory-10 Item Mania (PGBI-10M) items. Children with DMDD received lower scores on every item (including irritability) except impaired insight; differences were significant except for sexual interest and disruptive-aggressive behavior. Children with DMDD received lower scores on eight of 10 PGBI-10M items, the other two items rated irritability. Youth with DMDD were significantly less likely to have a biological parent with a bipolar diagnosis than were youth with BP-NOS. Children with DMDD were more likely to be male and older than children with BP-NOS, both small effect sizes, but had nearly double the rate of disruptive behavior disorders (large effect). Caregiver ratings of irritability based on the Child and Adolescent Symptom Inventory-4R (CASI-4R) were comparable at baseline; the DMDD group had a small but significantly steeper decline in scores over 36 months relative to the BP-NOS group (b = −0.24, SE = 0.12, 95% CI −0.48 to −0.0004). Trajectories for both groups were fairly stable, in the midrange of possible scores.
Conclusions: In a sample selected for elevated symptoms of mania, twice as many children were diagnosed with DMDD than with BP-NOS. Children with DMDD and BP-NOS are similar on most characteristics other than manic symptoms, per se, and parental history of bipolar disorder. Chronic irritability is common in both groups. Comprehensive evaluations are needed to diagnose appropriately. Clinicians should not assume that chronic irritability leads exclusively to a DMDD diagnosis.
Introduction
Disruptive mood dysregulation disorder (DMDD) was added to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) in large part to decrease the overdiagnosis of bipolar spectrum disorders (BPSD), including bipolar disorder not otherwise specified (BP-NOS) (in DSM-5, this diagnosis is incorporated into Other Specified Bipolar and Related Disorders, or OSBARD) (American Psychiatric Association 2013). Although temper outbursts and irritability are common symptoms in youth presenting to outpatient clinics, by definition, DMDD is characterized by persistent, nonepisodic irritability and/or anger that go far beyond the severity and frequency of typical temper tantrums, with symptoms occurring persistently over at least 1 year (American Psychiatric Association 2013). Additionally, by definition, youth with DMDD maintain an irritable and/or angry mood between outbursts, whereas youth with BP-NOS may return to a euthymic state and are more likely to show spontaneous fluctuations or episodes (Findling et al. 2003; Youngstrom et al. 2008a; Leibenluft 2011).
Previous studies examined a precursor to DMDD called severe mood dysregulation (SMD) (Leibenluft 2011). Towbin and colleagues (2013) summarized the similarities and differences between SMD and BP-NOS based on their respective definitions. Chronic irritability is required for SMD and allowable, but not required, for BP-NOS. A history of distinct, recurrent manic or hypomanic episodes that are too brief in duration (typically 2–3 days) to meet criteria for bipolar disorder type I or II are exclusionary for SMD but required for BP-NOS. A family history of bipolar disorder and the likelihood of converting to bipolar disorder type I or II within 7 years is unlikely for SMD but is true for BP-NOS in approximately half of the cases. A history of a full-duration manic episode is exclusionary for both SMD and BP-NOS, as is a history of hypomania. (For the BP-NOS group, this is only true if there is also a history of major depressive disorder [MDD], which would lead to a diagnosis of bipolar disorder type II.) However, empirical comparison of these two diagnoses is quite limited.
The majority of research conducted on SMD has used data collected from a highly selected sample from the National Institute of Mental Health (NIMH) Intramural Program. Within a sample of 146 youth who met the SMD phenotype, the majority were male (66%) and had elevated rates of attention-deficit/hyperactivity disorder (ADHD) (86%), oppositional defiant disorder (ODD) (85%), and anxiety disorders (58%) (Leibenluft 2011). Although SMD includes the main criteria of DMDD, it also requires symptoms of hyperarousal similar to those of ADHD (Leibenluft et al. 2003). Although some research suggests similarities between SMD/DMDD and bipolar disorder, such as deficits in facial emotion labeling (Guyer et al. 2007), differences are more common. In an epidemiologic examination of parental psychiatric history, parents of youth with SMD were significantly less likely to be diagnosed with a BPSD than parents of youth with a BPSD (2.7% vs. 33.3%) (Brotman et al. 2007). Stringaris and colleagues (2010) examined the longitudinal course of this cohort and reported the children with SMD were 50 times less likely to develop a (hypo-)manic or mixed episode than were youth with bipolar disorder.
According to a community-based follow-up study, SMD has a lifetime prevalence of 3.3% in youth 9–19 years of age; at an 8 year follow-up, youth diagnosed with SMD at an average age of 10 were significantly more likely than those not diagnosed with SMD to have a depressive disorder by age 18 (odds ratio 7.2, confidence interval 1.3–38.8, p = 0.02) but not bipolar disorder (Brotman et al. 2006). It is of note that of those participants without SMD, one quarter had other diagnoses, including any emotional disorder (6.1%), any behavioral disorder (19.6%), any anxiety disorder (4.5%), or substance abuse/dependence (8.8%) (Brotman et al. 2006). Copeland and colleagues (2014) followed this cohort into adulthood. Those with SMD (using retrofitted criteria to meet DMDD criteria by these authors) were significantly more likely than those without SMD/DMDD to have an adult depressive or anxiety disorder, and they had a 10.3 greater odds of having multiple adult disorders than those without SMD/DMDD (Copeland et al. 2014). The authors did not report on presence/absence of bipolar disorder; therefore, it is unknown if rates differed in adulthood between participants who did versus those who did not meet criteria for SMD/DMDD as children.
A small number of studies have characterized DMDD. Within a large community sample of 6-year-old children, 8% met criteria for DMDD when criteria were retrospectively applied. Of these, 61% demonstrated comorbidity with an emotional or behavioral disorder (Dougherty et al. 2014). Participants with DMDD had significantly higher rates of ODD and depression than participants without DMDD (55% vs. 5%, 13% vs. 5%, respectively) (Dougherty et al. 2014). Both ODD and ADHD at 3 years of age predicted DMDD at age 6 (Dougherty et al. 2014). Familial and environmental predictors included low parental support, lower levels of marital satisfaction, and parental lifetime substance use disorders. However, parental internalizing disorders were not associated with a DMDD diagnosis at age 6 (Dougherty et al. 2014).
Axelson et al. (2012) utilized the Longitudinal Assessment of Manic Symptoms (LAMS) sample to characterize children who met all DSM-5 DMDD criteria, with the exception being that participants with BPSD were allowed in the DMDD group. Just over one fourth (26%) of the LAMS sample met DMDD criteria at baseline. Results indicated significantly higher rates of ADHD (79%), disruptive behavior disorders (96%; ODD 78%, conduct disorder 18%) in children who met DMDD than in those who did not meet criteria for DMDD. In addition, youth with DMDD had significantly elevated scores on dimensional measures of mania and depression, and were more impaired than those without DMDD.
Sparks and colleagues (2014) examined offspring of parents who had bipolar disorder. They reported that these offspring were more likely than offspring of community control parents to meet DMDD criteria (odds ratio 8.3, 6.7% vs. 0.8%) and to have higher rates of chronic irritability (12.5% versus 2.5%, p < .005). Chronic irritability was noted in offspring who had diagnoses of bipolar disorder, depression, ADHD, and disruptive behavior disorders.
Margulies and colleagues (2012) examined rates of DMDD in 82 consecutive psychiatrically hospitalized c,hildren. They reported that nearly one third (31%) of children met DMDD criteria by parental report; however, only half of these (16%) did when diagnosis was based on inpatient observation. Over half (56%) of the 82 children had parent-reported manic symptoms (scores ≥20 on the Child Mania Rating Scale-Parent form). Of these 46, nearly half (n = 21, 46%) met DMDD by parental report but only one third (17.4%) did based on inpatient observation. The authors concluded “The overall utility of the DMDD diagnosis and whether it would prevent children from receiving other and better-defined diagnoses remains to be seen.” (p. 495).
To date, no one has compared DMDD directly with BP-NOS to determine the similarities and differences between these two diagnoses over time. Cross-sectionally, the two diagnoses are expected to exhibit similarities (and, therefore, the new diagnosis of DMDD is intended to decrease the misdiagnosis of bipolar disorder), but their longitudinal courses are expected to differ. This is important as treatment, particularly pharmacologic interventions, likely will differ for these two diagnoses. If DMDD develops into depressive and/or anxiety disorders, antidepressant treatment would be a logical first pharmacologic treatment of choice. Alternately, if DMDD continues to show a more externalizing behavior trajectory – consistent with the overlap in symptoms with ODD (Axelson et al. 2011) and the cross-sectional comorbidities with disruptive behavior disorders noted – then a different treatment package of psychosocial (Eyberg et al. 2008) and pharmacological interventions would be indicated (Jensen et al. 2007). In contrast, if BP-NOS continues to express itself as part of the bipolar continuum, atypical antipsychotics and/or mood stabilizers likely would be the first pharmacologic treatment of choice (McClellan et al. 2007). Therefore, it is crucial to develop clear templates for clinicians so that they can precisely differentiate youth with DMDD from youth with BP-NOS.
This study used a longitudinal cohort to compare children who met diagnostic criteria for DMDD or BP-NOS at entry into the study. First, we determined whether the two groups differed on a variety of sociodemographic and clinical variables. Second, we evaluated group differences in participants' parent-rated irritability over a 36 month follow-up period. We hypothesized that youth with DMDD and BP-NOS would have many similarities on symptoms common in outpatient clinics (e.g., irritability, aggression, impulsivity) but that children with DMDD versus BP-NOS would differ, by definition, in their expression of classically manic symptoms (e.g., euphoric mood, decreased sleep). Further, given the diagnostic criteria for DMDD, the two groups should exhibit distinct irritability trajectories, with DMDD participants maintaining consistently higher levels of irritability than youth with BP-NOS, whose irritability should be largely confined to episodes.
Method
Ascertainment of this sample has been described in detail elsewhere (Findling et al. 2010; Horwitz et al. 2010). In summary, institutional review boards at each university-affiliated LAMS site (Case Western Reserve University, Cincinnati Children's Medical Center, the Ohio State University, and the University of Pittsburgh Medical Center) approved all procedures. Parents/guardians at outpatient clinics provided written informed consent before completing the screening procedure, which consisted of a brief demographic form and the Parent General Behavior Inventory 10-Item Mania Scale (PGBI-10M) (Youngstrom et al. 2008b) to screen for elevated symptoms of mania (ESM). Results from this screening were used to invite a group of children with ESM and a smaller, demographically matched sample of children without ESM to enroll into the longitudinal portion of the study, for which parents provided consent and the children, assent, prior to their participation.
Sample
A subsample of 217 children 6–12.9 years of age from the LAMS cohort (n = 685) were included in the current study on the basis of a BP-NOS (n = 77) or DMDD (n = 140) diagnosis (defined subsequently) at baseline. In youth from the original cohort, the diagnoses most commonly assigned at baseline were: ADHD (76.1%), other disruptive behavior disorders (51.1%), BPSD (22.9%), depressive disorders (17.5%). and anxiety disorders (31.3%) (Findling et al. 2010).
Measures
Demographics
Parents/guardians provided information including age, sex, race, ethnicity, and health insurance status.
Family history
The Family History Screen (Weissman et al. 2000) was completed to collect information on parental psychiatric disorders. In addition to presence or absence of manic symptoms, parents were considered to have a probable bipolar disorder if they had elated mood plus three additional symptoms of mania or irritable mood plus four additional symptoms of mania.
Psychiatric diagnoses
Trained interviewers administered to children and their parent or legal guardian the Schedule for Affective Disorders and Schizophrenia for School-Age Children- Present and Lifetime Version (K-SADS-PL), with additional items about depressive and manic symptoms from the Washington University St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS-PL-W) (Kaufman et al. 1997; Geller et al. 2001). Additional questions were added to screen for pervasive developmental disorders. Study interviewers completed this semistructured interview to assess current and lifetime psychiatric diagnoses and the duration of each illness. Mood disorder diagnoses were evaluated at the baseline assessment and every 6 months afterwards.
DMDD diagnosis
DMDD in the LAMS sample was originally operationalized by Axelson et al. (2012) using K-SADS-PL-W items. For this study, we excluded 44 participants with bipolar diagnoses (n = 27 who met criteria for DMDD and BP-NOS; these participants were included in the BP-NOS group; n = 16, bipolar type 1; n = 1, cyclothymic disorder) from the DMDD group to more closely mirror DSM-5 criteria (American Psychiatric Association 2013).
• Severe recurrent temper outbursts. This criterion was derived from the “loses temper” item (at threshold, frequency is 2–5 times per week).
• Chronic irritability. This criterion was derived from the ODD section of the behavioral disorders supplement: “easily annoyed or angered” and “angry or resentful” items (both at threshold).
• Duration. Participants administered the K-SADS-PL-W ODD supplement were assessed for the presence of symptoms for a least 6 months, regardless of if they met full criteria for ODD. DMDD criterion states that symptoms must have been present for at least 12 months, with no more than 3 consecutive months when the person was without the preceding diagnostic criteria.
• Impairment in more than one setting. The ODD section of the behavioral disorders supplement evaluated impairment in at least two settings.
• No presence of a BPSD diagnosis. Youth with any bipolar spectrum disorder (i.e., bipolar I or II disorder, BP-NOS, or cyclothymia) were excluded.
BP-NOS diagnosis
The LAMS study uses previously developed criteria from the Course and Outcomes of Bipolar Youth (COBY) study to diagnose BP-NOS (Birmaher et al. 2009). These are:
• Child does not meet the Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV) criteria for bipolar disorder type I or II (American Psychiatric Association 1994)
-
• A distinct period of abnormally elevated, expansive, or irritable mood plus the following
∘ Two Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) B-criterion manic symptoms (three if the mood is irritability only) that are clearly associated with onset of abnormal mood (American Psychiatric Association 2000)
∘ A clear change in functioning
∘ Presence of elated and/or irritable mood and manic symptoms for a significant part of the day (4 hours, although this does not necessarily need to be expressed consecutively)
∘ 4 days (not necessarily consecutive) meeting criteria B.1eB.3 over patient's lifetime
∘ C. Mood and affective symptoms must be abnormal for child's level of development and environment
• Symptoms or mood changes that occur during substance use or antidepressant treatment do not count toward a bipolar diagnosis
-
• Exclusion criteria
∘ Current or lifetime DSM-IV diagnosis of schizophrenia, mental retardation, autism, or severe autism spectrum disorders
∘ Mood disorders caused by substance abuse, a medical condition, or secondary to use of medications (e.g., corticosteroids)
• If onset occurs prior to onset of comorbid substance use disorders, cases are included
• Children with mild comorbid Asperger disorder or pervasive developmental disorder not otherwise specified are included if their mood symptomatology was clearly episodic and best accounted for by the bipolar diagnosis
Medication history
Parents/guardians provided a comprehensive history of the child's past and current psychotropic medication usage.
Functional assessment
Study interviewers assigned ratings on the Children's Global Assessment Scale (CGAS) following completion of their comprehensive evaluation to assess the severity of current and lifetime impairment (Shaffer et al. 1983). The CGAS captures children's functionality at home, at school, and with peers.
Mood ratings
Unfiltered (meaning that severity of the symptom was rated regardless of whether it occurred in the context of a mood episode) (Yee et al. 2014) ratings of manic and depressive symptoms that occurred in the previous 2 weeks were obtained via interview of the child and parent/guardian using the Young Mania Rating Scale (YMRS) and the Children's Depression Rating Scale- Revised (CDRS-R) (Young et al. 1978; Poznanski et al. 1984). In contrast to methodology used by Axelson et al. (2012), the current study included total scores of irritability items so that scores from the two diagnostic groups in this study could be compared with results from other studies.
Questionnaires
Several self-report measures were completed by caregivers to characterize children's symptoms. Elevated symptoms of mania were assessed using the PGBI-10M (Youngstrom et al. 2008b). Anxiety symptoms during the past 6 months were obtained from the Screen for Child Anxiety Related Emotional Disorders (SCARED-P) (Birmaher et al. 1997).
Irritability scale
An irritability scale was derived from items found in the Child and Adolescent Symptom Inventory-4R (CASI-4R) ADHD, ODD, and conduct disorder subscales (Gadow and Sprafkin 2005). This was done to generate a continuous irritability variable based on caregiver report of the child's symptoms. To secure content validity with a previous well-validated irritability scale, Affective Reactivity Index (ARI) items (Stringaris et al. 2012), were considered in the selection of CASI-4R items. Six items were identified from the CASI-4R that mapped onto the ARI items: 1) Loses temper, 2) irritable for most of the day, 3) touchy or easily annoyed, 4) angry or resentful, 5) extremely tense or unable to relax, 6) deliberately annoys others. Principal axis factor analysis confirmed a single factor solution that showed an excellent level of reliability (Cronbach's α = 0.87).
Analyses
Statistical analyses used IBM SPSS version 22.0 (IBM Corp. 2013) and R (R Core Team 2014). Unweighted means, standard deviations, and frequency counts were calculated for descriptive statistics. Between-group differences were assessed with χ2 analyses for binary variables and independent t tests for continuous variables. Cohen's d effect size using the pooled standard deviation and φ's for χ2 were computed.
To compare caregiver-reported irritability level at baseline and during the 36 month follow-up observation between diagnostic groups, a hierarchical linear model, with a random intercept and slope, with repeated measures nested within subject (level 1), and time and diagnostic group as fixed covariates (level 2), was used. The diagnostic group × time interaction was the key outcome, with the coding using DMDD as the target and BP-NOS as the comparison. A model-based (semi) parametric bootstrap method was used to generate 95% confidence intervals based on 10,000 bootstrap replicates.
Results
Baseline comparisons
First, demographic variables were compared between the 140 children who met criteria for DMDD and the 77 who met criteria for BP-NOS. Significant age and sex differences between diagnostic groups were observed (Table 1). Children with DMDD were more likely to be male and younger than children with BP-NOS, with small effect sizes for both factors. There were no significant differences between groups in clinical treatment history. When baseline clinical characteristics were compared, children with DMDD had lower levels of manic symptoms, but nearly double the rate of disruptive behavior disorders, with large effect sizes for both factors.
Table 1.
Baseline Sociodemographic and Clinical Characteristics of Children with DMDD and BP-NOS
| Variable | DMDD (n = 140) | BP-NOS (n = 77) | t test or χ2 | Cohen's d or φ |
|---|---|---|---|---|
| Age, mean ± SD | 9.11 ± 1.83 | 9.87 ± 2.07 | 2.79** | 0.39 |
| Gender, male n (%) | 97 (69) | 42 (55) | 4.69* | 0.15 |
| Race, white n (%) | 82 (59) | 45 (58) | 0.00 | |
| Medicaid, yes n (%) | 80 (57) | 39 (51) | 0.85 | |
| No. of meds at baseline, mean ± SD | 0.95 ± .98 | 1.04 ± 1.16 | 0.60 | |
| No. of diagnoses at baseline, mean ± SD | 2.91 ± 1.19 | 3.04 ± 1.26 | 0.77 | |
| Hospitalization, yes n (%) | 10 (7) | 5 (7) | 0.03 | |
| ESM+ n (%) | 127 (91) | 75 (97) | 2.94 | |
| CGAS, mean ± SD | 51.33 ± 8.99 | 51.57 ± 8.58 | 0.19 | |
| YMRS, mean ± SD | 17.31 ± 7.62 | 25.09 ± 7.71 | 7.16*** | 1.01 |
| CDRS, mean ± SD | 36.64 ± 9.56 | 39.27 ± 10.60 | 1.87 | |
| PGBI-10M, mean ± SD | 14.01 ± 6.68 | 15.39 ± 6.06 | 1.5 | |
| SCARED-P, mean ± SD | 17.32 ± 12.90 | 17.44 ± 10.78 | 0.07 | |
| Irritability Scale, mean ± SD | 11.62 ± 3.78 | 12.39 ± 3.60 | −1.46 | |
| ADHD, yes n (%) | 118 (84) | 59 (77) | 1.94 | |
| Disruptive disorder, yes n (%) | 137 (98) | 41 (53) | 67.06*** | 0.56 |
| Anxiety, yes n (%) | 42 (30) | 26 (34) | 0.33 | |
| Elimination disorder, yes n (%) | 31 (22) | 17 (22) | 0.00 | |
| PDD, yes n (%) | 4 (3) | 0 (0) | 2.24 | |
| Psychosis, yes n (%) | 3 (2) | 2 (3) | 0.05 | |
| Maternal history of probable bipolar disorder, yes n (%) | 14 (10) | 15 (20) | 3.86* | |
| Paternal history of probable bipolar disorder, yes n (%) | 12 (9) | 9 (12) | 0.52 | |
| Probable diagnosis of either parent bipolar spectrum, yes n | 26 (19) | 24 (31) | 4.45* | 0.14 |
p < .05, **p < 0.01, ***p < 0.001.
DMDD, disruptive mood dysregulation disorder; BP-NOS, bipolar disorder, not otherwise specified; ESM, elevated symptoms of mania; CGAS, Children's Global Assessment Scale; YMRS, Young Mania Rating Scale; CDRS, Children's Depression Rating Scale; PGBI-10M, Parent General Behavior Inventory 10-Item Mania Scale; SCARED-P, Screen for Child Anxiety Related Emotional Disorders; ADHD, attention-deficit/hyperactivity disorder; PDD, pervasive developmental disorder.
When specific items on the unfiltered (i.e., rated regardless of occurrence within a mood episode) interviewer-rated YMRS were compared, children with DMDD averaged equal or lower scores on every item except impaired insight; all differences were significant except for sexual interest and disruptive-aggressive behavior (Table 2). It is of note that children with DMDD had lower YMRS irritability scores than children with BP-NOS. On the PBGI-10M, children with DMDD received lower scores on eight of ten items (only two of the eight reached a significant difference) (Table 2). The two items for which children with DMDD received an identical or higher score both assessed irritability/rage. Participants with DMDD did not significantly differ from those with BP-NOS in presence or absence of any manic symptoms in biological parents. However, participants with DMDD were significantly less likely than those with BP-NOS to have a biological parent with a probable bipolar spectrum diagnosis (19% vs. 31%, p < 0.05).
Table 2.
Item-Level Differences on Baseline Young Mania Rating Scale (YMRS) and Parent Reported General Behavior Inventory-10 Item Mania Scale (PGBI-10M) Scores Between the DMDD and BP-NOS Groups
| Variable | DMDD | BP-NOS | t test | p Value |
|---|---|---|---|---|
| YMRS | (n = 140) | (n = 77) | ||
| Elevated mood | 0.79 ± 0.99 | 2.12 ± 1.31 | 8.41 | <0.001 |
| Increased motor activity energy | 1.46 ± 1.46 | 2.51 ± 1.42 | 5.12 | <0.001 |
| Sexual interest | 0.47 ± 0.91 | 0.73 ± 1.14 | 1.81 | 0.72 |
| Sleep | 0.54 ± 0.98 | 1.08 ± 1.29 | 3.428 | 0.001 |
| Irritability | 3.64 ± 1.95 | 4.27 ± 1.88 | 2.31 | 0.02 |
| Speech (rate & amount) | 1.88 ± 1.97 | 3.58 ± 2.11 | 5.94 | <0.001 |
| Language thought disorder | 1.15 ± 0.98 | 1.91 ± 0.99 | 5.44 | <0.001 |
| Content | 0.70 ± 1.46 | 1.57 ± 2.03 | 3.65 | <0.001 |
| Disruptive-aggressive behavior | 4.13 ± 1.85 | 4.30 ± 1.87 | 0.65 | 0.52 |
| Appearance | 0.55 ± 0.76 | 1.12 ± 1.05 | 4.57 | <0.001 |
| Impaired insight | 2.01 ± 1.53 | 1.91 ± 1.48 | −0.46 | 0.65 |
| PGBI-10M | (n = 137; *n = 136) | (n = 77) | ||
| Happy/energetic/restless | 1.64 ± 1.14 | 1.69 ± 0.92 | 0.32 | 0.76 |
| Others said too high* | 0.90 ± 0.93 | 1.08 ± 0.86 | 1.40 | 0.16 |
| Labile mood | 1.77 ± 0.97 | 1.96 ± 0.91 | 1.44 | 0.15 |
| Intense mood/anxious* | 0.99 ± 0.97 | 1.16 ± 0.93 | 1.25 | 0.21 |
| Happy/energetic/feelings of rage | 1.52 ± 1.10 | 1.32 ± 1.04 | −1.26 | 0.21 |
| Delayed sleep onset* | 1.23 ± 1.08 | 1.35 ± 1.07 | 0.76 | 0.45 |
| Labile/rarely euthymic | 1.72 ± 0.98 | 1.92 ± 0.89 | 1.48 | 0.14 |
| Dysphoric/irritable then elated | 1.20 ± 1.05 | 1.57 ± 0.95 | 2.58 | 0.01 |
| Euphoric/energetic then irritable | 1.79 ± 0.99 | 1.79 ± 0.98 | 0.03 | 0.98 |
| Racing thoughts | 1.26 ± 0.98 | 1.55 ± 0.97 | 2.04 | 0.04 |
DMDD, disruptive mood dysregulation disorder; BP-NOS, bipolar disorder, not otherwise specified.
Longitudinal comparison
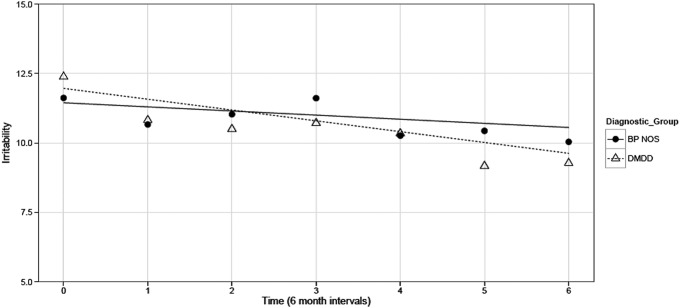
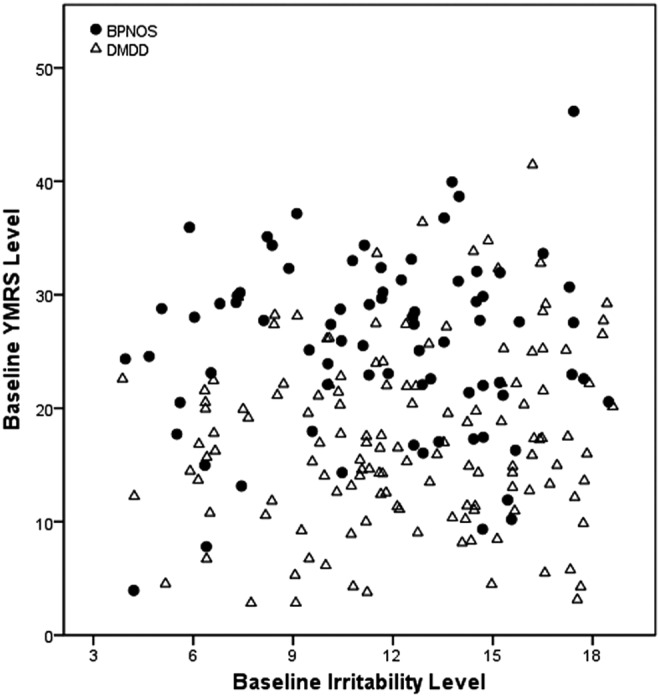
The distribution of scores on the Irritability Scale, which is based on caregiver report of the child's behavior, was approximately normal for the two groups combined, with no outliers (Fig. 1). At baseline, although caregivers of children with DMDD rated them higher on irritability than caregivers of children with BP-NOS, this did not reach statistical significance (b = 0.51, SE = 0.48, t test = 1.07, p > 0.05) (Table 3). Irritability decreased slightly faster for the DMDD group over the 36 month-follow up period (b = −0.24, SE = 0.12, t test = −1.96, p = 0.0499). Trajectories for both groups were fairly stable, in the mid-range of possible scores (Fig. 2).
FIG. 1.
Baseline Young Mania Rating Scale (YMRS) and irritability levels by groups. The correlation observed between irritability and YMRS total score at baseline was r = 0.07, p > 0.05.
Table 3.
Differences in Irritability Level at Baseline and Over Time Between the DMDD and BP-NOS Groups
| Variable | b estimate | SE | t test | 95% CIa |
|---|---|---|---|---|
| Intercept | 11.45 | 0.38 | 29.66 | (10.69, 12.20) |
| Time | −0.14 | 0.10 | −1.52 | (−0.34, 0.05) |
| Diagnostic group (DMDD = 1) | 0.51 | 0.48 | 1.07 | (−0.42, 1.47) |
| Time × diagnostic group (DMDD = 1) | −0.24 | 0.12 | −1.96 | (−0.48, −0.0004) |
95% confidence intervals based on 10,000 bootstrap replicates.
DMDD, disruptive mood dysregulation disorder; BP-NOS, bipolar disorder, not otherwise specified.
FIG. 2.
Irritability trajectories over 36 months in children with disruptive mood dysregulation disorder (DMDD) and bipolar disorder not otherwise specified (BP-NOS).
As there were 27 children who fulfilled criteria for DMDD (other than the bipolar symptom exclusion) and BP-NOS, we completed one additional post-hoc comparison, comparing rates of irritability among three groups, DMDD plus BP-NOS (n = 27), DMDD only (n = 140) and BP-NOS only (n = 50). The DMDD plus BP-NOS and DMDD groups had higher levels of caregiver-reported irritability at baseline than the BP-NOS only group. The only significant difference in slopes was between the DMDD only and DMDD plus BP-NOS groups, with the latter group showing the slowest decline in irritability (b = 0.38, 95% confidence interval [0.02–0.74]).
Discussion
We evaluated similarities and differences between DMDD and BP-NOS on sociodemographic and clinical variables at baseline, particularly YMRS items, and tested whether rates of caregiver-reported irritability differed between the two groups over time. DMDD was not clearly distinguished from BP-NOS on most comparison points other than YMRS items and rates of a probable bipolar diagnosis in biological parents. It is of note that the YMRS was administered in an unfiltered manner (i.e., in a “what you see is what you get” manner regardless of whether the symptoms occurred within the context of a mood episode) and was not used to make the diagnosis of DMDD or BP-NOS (for a further discussion of this, see Yee et al. 2014).
Children with DMDD were younger and more likely to be boys. However, these were not striking differences; average ages for both groups were in the 9–10-year-old range and boys were the majority of each group. Youth with DMDD were similar to those with BP-NOS on most clinical factors, including: Number of diagnoses; number of medications; likelihood of prior hospitalization; comorbid ADHD, anxiety disorders, pervasive developmental disorders, elimination disorders, and psychosis; global impairment; PGBI-10M; and depressive and anxiety symptom severity. Only disruptive behavior disorders were more common in children with DMDD, consistent with prior research (Stringaris et al. 2010; Axelson et al. 2012; Towbin et al. 2013). Irritability on the parent-reported Irritability Scale was nominally higher at baseline, but to a nonsignificant degree, for the DMDD group compared with the BP-NOS group, but then decreased more rapidly over time. The difference in slopes was statistically significant, but unlikely to be clinically meaningful. The change of a quarter point is miniscule, given that the scale is only accurate to ± −1.90 points for individual change scores, based on the standard error of the difference score (Jacobson and Truax 1991).
YMRS total scores and all item scores except impaired insight (which was negligibly different between groups) were similar or lower for children with DMDD than for children with BP-NOS. Notably, elevated mood, increased motor activity, decreased sleep, pressured speech, impaired language/thought, thought content, and appearance were all more elevated in children with BP-NOS. Even irritability on the YMRS was more severe for children with BP-NOS. Most PGBI-10M item scores were nominally lower for the children with DMDD compared to children with BP-NOS. One item that measured irritability was identical for the two groups; one item that assessed rage was nominally higher for the DMDD group.
Group comparisons of caregiver-reported irritability revealed three findings of interest. First, the groups did not differ significantly on either the level or change over time in ratings of irritability. Whereas there was a small decrement in irritability scores over time for the DMDD group, irritability remained stable in the BP-NOS group. Second, both groups had midrange irritability scores of 10–12 on a 0–18 scale that remained fairly consistent over the 3 years. Although the presence of both DMDD and BP-NOS is disallowed per DSM-5 rules, when the subgroup who met criteria for both diagnoses (other than the manic symptom exclusion for DMDD) was compared on chronic irritability with those children who had DMDD only or BP-NOS only, the DMDD plus BP-NOS children had significantly less decline in caregiver-reported irritability over time.
Differences in findings regarding irritability, depending upon whether the interviewer rated presence/absence and severity in a “what you see is what you get” unfiltered manner or whether caregivers reported on their children's behavior, are interesting. Children with DMDD appeared less impaired than children with BP-NOS using the former strategy, but the two groups appeared similar when using caregiver report on rating scales. Perhaps the frustration of raising a child with a disruptive behavior disorder, which were ubiquitous in the DMDD group, leads to higher caregiver reports of irritability, whereas interviewer-based questioning that incorporates parent and child input as well as clinical observation during the interview, puts a greater perspective on the severity of the behaviors and affect observed. This is in keeping with previous research showing much lower rates of DMDD when diagnoses are based on clinical observation rather than parental self-report (Margulies et al. 2014).
DMDD was included in the DSM-5 as a way to decrease diagnoses of BPSD in children. Pharmacologic management, in particular, might differ for children with DMDD than those with BP-NOS. Children with DMDD initially display high rates of externalizing symptoms and comorbid disruptive behavior disorders with subsequent risk for development of depressive disorders, which would suggest treatment with antidepressant medications. Those with BP-NOS are likely to be treated with first-line medications for bipolar disorder. Clarifying the differentiating features of DMDD and BP-NOS is, therefore, crucial for the effective management of these disorders. Results from this study point to cross-sectional similarities between these two diagnostic groups on nearly every feature except more classically manic symptoms and family history of probable bipolar disorder in parents. Further, the trajectory of caregiver-reported irritability over a 3 year interval does not meaningfully separate the two groups. Therefore, it will be important for clinicians not to use caregiver-reported chronic irritability in isolation as a reason to consider DMDD the most appropriate diagnosis, but rather to conduct a thorough review of symptoms and course to determine if a child fulfills criteria for DMDD, BP-NOS, or other primary and comorbid diagnoses. In this regard, it is noteworthy that clinicians achieved lower reliability for DMDD than for pediatric bipolar diagnoses in the DSM-5 field trials (Regier et al. 2012). Semistructured approaches (Rettew et al. 2009) or checklists as a way of augmenting the family's description of the presenting problem could be helpful in improving the reproducibility of diagnoses (Croskerry 2003; Gawande 2010; Youngstrom et al. 2014).
Limitations
Several limitations of this study are important to note. The current study utilized retrofitted K-SADS-PL-W responses to determine DMDD diagnoses. Our criteria slightly modified those previously reported in Axelson et al. (2012) to better align with DSM-5 diagnostic criteria. The majority of LAMS study participants were recruited because of their elevated PGBI-10M scores, resulting in a sample with disproportionately elevated symptoms of mania and, therefore, not fully representative of clinical outpatient samples.
Conclusions
Despite these limitations, these findings suggest that children with DMDD and BP-NOS are very similar on most characteristics other than manic symptoms and a probable bipolar family history. Even in a sample enriched with children who have elevated symptoms of mania, DMDD outnumbers a BP-NOS diagnosis almost 2:1.
Clinical Significance
Clinicians will need to complete comprehensive evaluations to appropriately diagnose children and not assume that caregiver-reported chronic irritability leads exclusively to a DMDD diagnosis. Children with DMDD and BP-NOS are fraternal, not identical twins, but they may easily confuse the casual observer.
Contributor Information
Collaborators: the LAMS Group
Disclosures
Dr. Fristad receives royalties from American Psychiatric Press, Child & Family Psychological Services, and Guilford Press. Dr. Arnold has received research funding from Curemark, Forest, Lilly, Neuropharm, Novartis, Noven, Shire, and YoungLiving (as well as the National Institutes of Health [NIH] and Autism Speaks) and has consulted with or been on advisory boards for Gowlings, Neuropharm, Novartis, Noven, Organon, Otsuka, Pfizer, Roche, Seaside Therapeutics, Sigma Tau, Shire, and Tris Pharma. Dr. Youngstrom has received grant funding from the National Institute of Mental Health (NIMH) and has consulted with Otsuka and Lundbeck about assessment. Dr. Birmaher receives or has received royalties from NIMH grants and Random House. Dr. Kowatch has acted and/or served as faculty for the Resource for Advancing Children's Health (REACH Institute), been editor for Current Psychiatry and on the Data and Safety Monitoring Board (DSMB) for Forest Pharm, and is employed by The Ohio State University. Dr. Findling receives or has received research support, or acted as a consultant and/or served on a speaker's bureau for Alcobra, American Academy of Child & Adolescent Psychiatry, American Physician Institute, American Psychiatric Press, AstraZeneca, Bracket, Bristol-Myers Squibb, CogCubed, Cognition Group, Coronado Biosciences, Dana Foundation, Elsevier, Forest, GlaxoSmithKline, Guilford Press, Johns Hopkins University Press, Johnson and Johnson, Jubilant Clinsys, KemPharm, Lilly, Lundbeck, Merck, NIH, Neurim, Novartis, Noven, Otsuka, Oxford University Press, Pfizer, Physicians Postgraduate Press, Purdue, Rhodes Pharmaceuticals, Roche, Sage, Shire, Sunovion, Supernus Pharmaceuticals, Transcept Pharmaceuticals, Validus, and WebMD. Dr. Frazier has received federal funding or research support from, acted as a consultant to, received travel support from, and/or received a speaker's honorarium from the Brain and Behavior Research Foundation, Bristol-Myers Squibb, the Cole Family Research Fund, Ecoeos,Forest Laboratories, Ingalls Foundation, IntegraGen, Kugona LLC, NIH, Shire Development, and Simons Foundation. Hannah Wolfson, Dr. Algorta, Dr. Axelson, Dr. Holland, Dr. Horwitz, Dr. Phillips, and Dr. Taylor have no conflicts to declare.
References
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric Association; 1994 [Google Scholar]
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed., Text Revision. Washington, DC: American Psychiatric Association; 2000 [Google Scholar]
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013 [Google Scholar]
- Axelson DA, Birmaher B, Findling RL, Fristad MA, Kowatch RA, Youngstrom EA, Arnold EL, Goldstein BI, Goldstein TR, Chang KD, Delbello MP, Ryan ND, Diler RS: Concerns regarding the inclusion of temper dysregulation disorder with dysphoria in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. J Clin Psychiatry 72:1257–1262, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axelson D, Findling R, Fristad MA, Kowatch RA, Youngstrom EA, Horwitz SM, Arnold E, Frazier TW, Ryan N, Demeter C, Gill MK, Hauser–Harrington JC, Depew J, Kennedy SM, Gron BA, Rowles BM, Birmaher B: Examining the proposed disruptive mood dysregulation disorder diagnosis in children in the Longitudinal Assessment of Manic Symptoms study. J Clin Psychiatry 73:1342–1350, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Goldstein B, Strober M, Gill MK, Hunt J, Houck P, Ha W, Iyengar S, Kim E, Yen S, Hower H, Esposito C, Goldstein T, Ryan N, Keller M: Four-year longitudinal course of children and adolescents with bipolar spectrum disorder: The course and outcome of bipolar youth (COBY) study. Am J Psychiatry 166:795–804, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, Neer SM: The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry 36:545–553, 1997 [DOI] [PubMed] [Google Scholar]
- Brotman MA, Kassem L, Reising MM, Guyer AE, Dickstein DP, Rich BA, Towbin KE, Pine DS, McMahon FJ, Leibenluft E: Parental diagnoses in youth with narrow phenotype bipolar disorder or severe mood dysregulation. Am J Psychiatry, 164:1238–1241, 2007 [DOI] [PubMed] [Google Scholar]
- Brotman MA, Schmajuk M, Rich BA, Dickstein DP, Guyer AE, Costello EJ, Egger HL, Angold A, Pine DS, Leibenluft E: Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biol Psychiatry 60:991–997, 2006 [DOI] [PubMed] [Google Scholar]
- Copeland WE, Shanahan L, Egger H, Angold A, Costello EJ: Adult diagnostic and functional outcomes of DSM-5 disruptive mood dysregulation disorder. Am J Psychiatry, 171:668–674, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croskerry P: The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med 78:775–780, 2003 [DOI] [PubMed] [Google Scholar]
- Dougherty LR, Smith VC, Bufferd SJ, Carlson GA, Stringaris A, Leibenluft E, Klein DN: DSM-5 disruptive mood dysregulation disorder: Correlates and predictors in young children. Psychol Med 44:2339–2350, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyberg SM, Nelson MM, Boggs SR: Evidence-based psychological treatments for children and adolescents with disruptive behavior. J Clin Child Adolesc Psychol 37:215–237, 2008 [DOI] [PubMed] [Google Scholar]
- Findling RL, Kowatch RA, Post RM: Pediatric bipolar disorder: A handbook for clinicians. London: Martin Dunitz; 2003 [Google Scholar]
- Findling RL, Youngstrom EA, Fristad MA, Birmaher B, Kowatch RA, Arnold LE, Frazier TW, Axelson D, Ryan N, Demeter CA, Fields B, Depew J, Kennedy SM, Marsh L, Rowles BM, Horwitz SM: Characteristics of children with elevated symptoms of mania: The Longitudinal Assessment of Manic Symptoms (LAMS) study. J Clin Psychiatry 71:1664–1672, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadow KD, Sprafkin J: Child and Adolescent Symptom Inventory-4R. Stony Brook, NY: Checkmate Plus, 2005 [Google Scholar]
- Gawande A. The Checklist Manifesto. New York, NY: Penguin; 2010 [Google Scholar]
- Geller B, Zimerman B, Williams M, Bolhofner K, Craney J, DelBello MP, Soutullo C: Reliability of the Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS) mania and rapid cycling sections. J Am Acad Child Adolesc Psychiatry 40:450–455, 2001 [DOI] [PubMed] [Google Scholar]
- Guyer AE, McClure EB, Adler AD, Brotman MA, Rich BA, Kime AS, Pine DS, Ermst M, Leibenluft E: Specificity of facial expression labeling deficits in childhood psychopathology. J Child Psychol Psychiatry 48:863–871, 2007 [DOI] [PubMed] [Google Scholar]
- Horwitz SM, Demeter CA, Pagano ME, Youngstrom EA, Fristad MA, Arnold LE, Birmaher B, Gill MK, Axelson D, Kowatch RA, Frazier TW, Findling RL: Longitudinal Assessment of Manic Symptoms (LAMS) study: Background, design, and initial screening results. J Clin Psychiatry 71:1511–1517, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp: IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp; 2013 [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol 59:12–19, 1991 [DOI] [PubMed] [Google Scholar]
- Jensen PS, Youngstrom EA, Steiner H, Findling RL, Meyer RE, Malone RP, Carlson GA, Coccaro EF, Aman MG, Blair J, Dougherty D, Ferris C, Flynn L, Green E, Hoagwood K, Hutchinson J, Laughren T, Leve LD, Novins DK, Vitello B: Consensus report on impulsive aggression as a symptom across diagnostic categories in child psychiatry: Implications for medication studies. J Am Acad Child Adolesc Psychiatry 46:309–322, 2007 [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N: Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36:980–988, 1997 [DOI] [PubMed] [Google Scholar]
- Leibenluft E: Severe mood dysregulation, irritability, and the diagnostic boundaries of bipolar disorder in youths. Am J Psychiatry 168:129–142, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leibenluft E, Dennis CS, Towbin KE, Bhangoo RK, Pine DS: Defining clinical phenotypes of juvenile mania. Am J Psychiatry 160:430–437, 2003 [DOI] [PubMed] [Google Scholar]
- Margulies DM, Weintraub S, Basile J, Grover PJ, Carlson GA: Will disruptive mood dysregulation disorder reduce false diagnosis of bipolar disorder in children? Bipolar Disord 14:488–496, 2012 [DOI] [PubMed] [Google Scholar]
- McClellan J, Kowatch R, & Findling RL: Practice parameter for the assessment and treatment of children and adolescents with bipolar disorder. J Child Adolesc Psychiatry 46:107–125, 2007 [DOI] [PubMed] [Google Scholar]
- Poznanski EO, Grossman JA, Buchsbaum Y, Banegas M, Freeman L, Gibbons R: Preliminary studies of the reliability and validity of the Children's Depression Rating Scale. J Am Acad Child Psychiatry 23:191–197, 1984 [DOI] [PubMed] [Google Scholar]
- R Core Team: R: A language and environment for statistical computing, 2014. Vienna: R Foundation for Statistical Computing Available at http://www.R-project.org/ Accessed November24, 2014
- Rettew DC, Lynch AD, Achenbach TM, Dumenci L, Ivanova MY: Meta-analyses of agreement between diagnoses made from clinical evaluations and standardized diagnostic interviews. Int J Methods Psychiatr Res 18:169–184, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S: A Children's Global Assessment Scale (CGAS). Arch Gen Psychiatry 40:1228–1231, 1983 [DOI] [PubMed] [Google Scholar]
- Sparks GM, Axelson DA, Haifeng Y, Ha W, Ballester J, Diler RS, Goldstein B, Goldstein T, Hickey MB, Ladouceur CD, Monk K, Sakolsky D, Birmaher B: Disruptive mood dysregulation disorder and chronic irritability in youth at familial risk for bipolar disorder. J Am Acad Child Adolesc Psychiatry 53:408–416, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringaris A, Baroni A, Haimm C, Brotman M, Lowe CH, Myers F, Rustgi E, Wheeler W, Kayser R, Towbin K, Leibenluft E: Pediatric bipolar disorder versus severe mood dysregulation: Risk for manic episodes on follow-up. J Am Acad Child Adolesc Psychiatry 49:397–405, 2010 [PMC free article] [PubMed] [Google Scholar]
- Stringaris A, Goodman R, Ferdinando S, Razdan V, Muhrer E, Leibenluft E, Brotman M: The Affective Reactivity Index: A concise irritability scale for clinical and research settings. J Child Psychol Psychiatry 53:1109–1117, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towbin K, Axelson D, Leibenluft E, Birmaher B: Differentiating bipolar disorder-not otherwise specified and severe mood dysregulation. J Am Acad Child Psychiatry 52:466–481, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M: Brief screening for family psychiatric history: The family history screen. Arch Gen Psychiatry 57: 675–682, 2000 [DOI] [PubMed] [Google Scholar]
- Yee AM, Algorta GP, Youngstrom EA, Findling RL, Birmaher B, Fristad MA, The Lams Group: Unfiltered administration of the YMRS and CDRS-R in a clinical sample of children. J Clin Child Adolesc Psychol 2:1–16, 2014. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young RC, Biggs JT, Ziegler VE, Meyer DA: A rating scale for mania: Reliability, validity and sensitivity. Br J Psychiatry 133:429–435, 1978 [DOI] [PubMed] [Google Scholar]
- Youngstrom EA, Birmaher B, Findling RL: Pediatric bipolar disorder: Validity, phenomenology, and recommendations for diagnosis. Bipolar Disord 10:194–214, 2008a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youngstrom EA, Choukas–Bradley S, Calhoun CD, Jensen–Doss A: Clinical guide to the evidence-based assessment approach to diagnosis and treatment. Cogn Behav Pract 22:20–35, 2014 [Google Scholar]
- Youngstrom EA, Fraizer TW, Demeter C, Calabrese JR, Findling RL: Developing a ten item mania scale from the Parent General Behavior Inventory for children and adults. J Clin Psychiatry 69:831–839, 2008b [DOI] [PMC free article] [PubMed] [Google Scholar]