Abstract
Background:
Monitoring where people die is key to ensure that palliative care is provided in a responsive and integrated way.
Aim:
To examine trends of place of death and project hospital deaths until 2030 in an ageing country without integrated palliative care.
Design:
Population-based observational study of mortality with past trends analysis of place of death by gender, age and cause of death. Hospital deaths were projected until 2030, applying three scenarios modelled on 5-year trends (2006–2010).
Setting/participants:
All adult deaths (⩾18 years old) that occurred in Portuguese territory from 1988 to 2010.
Results:
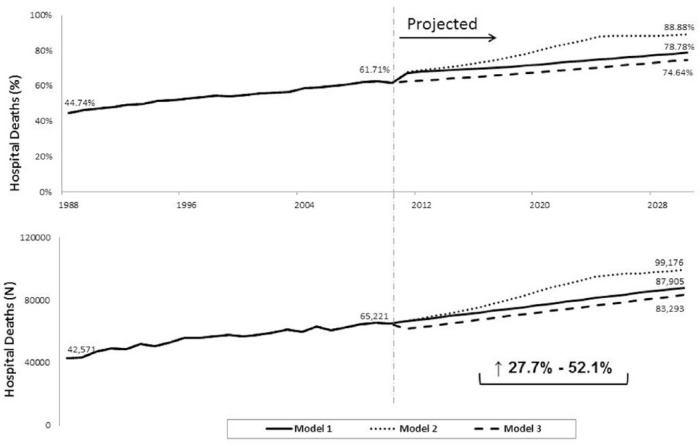
There were 2,364,932 deceased adults in Portugal from 1988 to 2010. Annual numbers of deaths increased 11.1%, from 95,154 in 1988 to 105,691, mainly due to more than doubling deaths from people aged 85+ years. Hospital deaths increased by a mean of 0.8% per year, from 44.7% (n = 42,571) in 1988 to 61.7% (n = 65,221) in 2010. This rise was largest for those aged 85+ years (27.8% to 54.0%). Regardless of the scenario considered, and if current trends continue, hospital deaths will increase by more than a quarter until 2030 (minimum 27.7%, maximum 52.1% rise) to at least 83,293 annual hospital deaths, mainly due to the increase in hospital deaths in those aged 85+ years.
Conclusion:
In one of the most ageing countries in the world, there is a long standing trend towards hospitalised dying, more pronounced among the oldest old. To meet people’s preferences for dying at home, the development of integrated specialist home palliative care teams is needed.
Keywords: Palliative care, terminal care, death certificates, health planning, home care services, aged
What is already known about the topic?
The majority of people would prefer to die at home.
Monitoring where people die is key to ensure that palliative care is provided in a responsive and integrated way.
What this paper adds?
Hospital death proportions have increased steadily from 44.7% to 61.7% in one of the most ageing countries in the world (Portugal, 1988–2010).
Hospital deaths are projected to increase further by at least a quarter until 2030, to 74.6% of all deaths.
The past and future increase in hospital deaths in such an ageing country is mainly due to the rise of hospital deaths in the older people (85+ years).
Implications for practice, theory or policy
To meet people’s preferences for dying at home, the development of integrated specialist home palliative care teams is needed.
Introduction
Worldwide, people are increasingly living and dying with ageing due to better life expectancy.1 Many countries face increasing mortality caused by chronic illness and large cohorts of baby-boomers reaching later life, coupled with rising numbers of deaths in hospital.2
However, when eliciting preferences for where to die in the context of advanced illness, 31%–87% of patients, 25%–64% of caregivers and 49%–70% of the general population state home is their preferred place,3 hospital being one of the least preferred places.4
With a population of 10 million and around 100,000 deaths per year, Portugal has the seventh most ageing population in the world, alongside countries such as Denmark, Germany and France, with 24% of people aged 60+ years.1 As this proportion is expected to rise to 40% by 2050, Portugal will become the second most ageing country in the world, only behind Japan.1 It is known that ageing is associated with higher levels of dependency, comorbidities and complex needs.2
In light of the current and future socio-demographic scenario in Portugal, which resonates with many other developed and ageing nations, the provision of appropriate physical, psychological, social and spiritual support to older people facing incurable illnesses is a public health priority.5 Nonetheless, there are major barriers to the integration of palliative care into the wider health system as a treatment component within the continuum of care for patients: scarcity of palliative care services, lack of recognition of palliative care needs by professionals, late referrals, medical and nursing education without basic training on palliative care.7 A recent World Health Organization (WHO) resolution8 urges countries to develop integrated models of palliative care, mainly focused in primary care, community and home care services.
Monitoring where people die is, therefore, key to ensure that care in later life towards death is provided in a responsive and integrated way. This study aimed to examine trends of place of death by age, gender and cause of death and to project future hospital deaths until 2030 in an ageing country without integrated palliative care (Portugal 1988–2030).7
Methods
Study design
Epidemiological population-based analysis of Portuguese mortality data from 1988 to 2010 by gender, age and cause of death, and projections of hospital deaths until 2030. This study followed the STrengthening the Reporting of OBservational Studies in Epidemiology (STROBE) guidelines.
Data sources
Data for all deaths that occurred in Portuguese territory (mainland, Azores and Madeira) from 1988 to 2010 were provided by the Portuguese Statistics Institute (INE) free of charge, under a protocol established between the INE, the researchers’ host organisation and the Portuguese Ministry of Science, Technology and Higher Education. The dataset included data derived from death certificates, which are originally completed by the physician who was primarily responsible for the care of the person or the one who first attends the place of death.9
The requested dataset contained individual anonymised data for all deaths by place of death, gender, age, date of death and cause of death. Date of death was coded into three variables: day of the week, month and year of death.
Projections of gender- and age-specific mortality rates and population estimates were provided by the Eurostat with no costs associated, for the years 2011–2060. The methodological details of these forecasts are described in detail elsewhere.10 They rely on several assumptions of fertility, mortality and migration, in which the ‘what-if’ scenarios are based in.
Classification of place of death and primary outcome
In the Portuguese death certificate, place of death is classified into three categories since 1996: ‘domicile’, ‘hospital/clinic’ and ‘other place’. The first category includes deaths occurring at home, care homes, nursing homes or any non-public/non-clinical place. Deaths at ‘hospital/clinic’ are those occurring in clinical facilities, such as public or private hospitals (this category is from now on named ‘hospital’). Finally, a person is categorised as having died at ‘other place’ when this occurred in a public space (e.g. street, transports). Before 1996, there was one additional category: ‘public way’. It was deemed sensible to aggregate this with the category ‘other place’.
Our primary outcome was defined as death in hospital (i.e. occurring at ‘hospital/clinic’) versus others, as deaths occurring at home and care homes/nursing homes are not separately coded in Portuguese death certificates, which prevented us from examining past trends and projecting for these different places.
Analysis
Past trends
We analysed place of death for all adults (⩾18 years old) who have died in Portuguese territory during a 23-year period (1988–2010). We tabulated frequencies for the different places in each year by gender, age and cause of death. Six age groups were defined taking into account Portuguese preferences data6 and to enable international comparisons.11–14 We calculated gender- and age-standardised proportions of hospital deaths (direct method) to control for the influence of differences in the gender and age distribution of deaths in changes of place of death over time. The gender and age distribution of 1988 was taken as standard. Place of death was also analysed by cause of death from 2002 onwards (year when the International Classification of Diseases, 10th revision (ICD-10) was implemented in Portugal), divided into three major groups: cancer, non-cancer and external/unknown causes. All but the latter analysis were performed in Microsoft Excel® (cause of death was analysed in SPSS® version 18).
Projections
From the Eurostat projections (gender- and age-specific mortality rates and resident numbers), we calculated projected gender- and age-specific numbers of deaths. Projections of hospital deaths assumed that the last 5-year trends (2006–2010) will be maintained and were performed in three steps: (1) calculation of gender- and age-specific mean of the slopes of deaths by place of death in the last 5 years (2006–2010), (2) the slopes’ means were applied consecutively from 2010 onwards to obtain gender- and age-specific place of death numbers or proportions and (3) gender- and age-specific place of death numbers or proportions were applied to the projections of total deaths to obtain the respective proportions or numbers of hospital deaths.
We modelled three scenarios based on different assumptions: in model 1, we assumed that trends in absolute changes in numbers of hospital deaths will be maintained; in model 2, we assumed that future hospital deaths will be determined by proportional changes in numbers of hospital deaths; and in model 3, proportions of non-hospital deaths of recent years were assumed to be the main driver of future hospital trends. These models are explained in more detail in Appendix 1 (further details design of the models are available from the authors on request).
Approvals
To access the mortality data, a protocol with the INE, the researchers’ host organisation and the Portuguese Ministry of Science, Technology and Higher Education was established. This protocol included a biding code of conduct, and all researchers signed a declaration of confidentiality. The ethics committee of the researchers’ host organisation advised that ethical approval was not needed, as the data were anonymised and referred to deceased people.
Results
Past trends
There were 2,364,932 adults (⩾18 years old) who died in Portugal in the 23 study years, 52.2% men. Annual numbers of deaths increased 11.1%, from 95,154 in 1988 to 105,691 in 2010 (Table 1), and have overtaken the number of births in 3 recent years (2007, 2009 and 2010; Figure 1). This increase in the number of deaths is mainly due to the sharp increase in the number and proportion of deaths from people aged 85+ years (from 17,241 or 18.1% to 35,175 or 33.3% of all deaths; Table 1; Figure 1). Deaths from people in other age groups have generally decreased or remained similar over time. Therefore, death in Portugal is occurring at later ages, following from the continuous population ageing observed over the last years (Figure 1). The increases in the yearly median death age (75 to 80 years old) and interquartile ranges (65–82 to 71–87 years old) further confirm this trend (Table 1). Men accounted for 52.2% of all deaths in 1988 and 51.2% in 2010 (Figure 1; Appendix 2). Despite trends for both men and women to die later in life, men are dying 6 years earlier than women (at median ages of 77 and 83 years, respectively, in 2010).
Table 1.
Past trends of place of death by gender, age and cause of death (Portugal – 1988, 2000, 2010).
| All places |
Hospital |
Domicile |
Other place |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1988 | 2000 | 2010 | 1988 | 2000 | 2010 | 1988 | 2000 | 2010 | 1988 | 2000 | 2010 | ||
| All deaths | |||||||||||||
| N | 95,154 | 104,498 | 105,691 | 42,571 | 57,066 | 65,221 | 47,810 | 37,042 | 31,277 | 4773 | 10,390 | 9193 | |
| % | 100 | 100 | 100 | 44.7 | 54.6 | 61.7 | 50.2 | 35.4 | 29.6 | 5.0 | 9.9 | 8.70 | |
| Stand. % | – | – | – | 44.7 | 56.2 | 63.4 | 50.2 | 33.8 | 27.6 | 5.0 | 10.1 | 9.0 | |
| Age (years) | |||||||||||||
| Med, IQR | 75, 65–82 | 77, 68–85 | 80, 71–87 | 72, 61–80 | 75, 65–83 | 79, 69–86 | 78, 70–85 | 81, 73–87 | 83, 74–88 | 61, 39–77 | 75, 57–84 | 80, 66–87 | |
| 18–34 | N | 3325 | 3067 | 1370 | 1751 | 1629 | 679 | 567 | 428 | 252 | 1007 | 1010 | 439 |
| % | 3.5 | 2.9 | 1.3 | 52.7 | 53.1 | 49.6 | 17.1 | 14.0 | 18.4 | 30.3 | 32.9 | 32.0 | |
| 35–44 | N | 2677 | 3147 | 2474 | 1521 | 1940 | 1545 | 741 | 567 | 531 | 415 | 640 | 398 |
| % | 2.8 | 3.0 | 2.3 | 56.8 | 61.6 | 62.4 | 27.7 | 18.0 | 21.5 | 15.5 | 20.3 | 16.1 | |
| 45–54 | N | 5493 | 5299 | 5210 | 3265 | 3500 | 3536 | 1714 | 1076 | 1073 | 514 | 723 | 601 |
| % | 5.8 | 5.1 | 4.9 | 59.4 | 66.1 | 67.9 | 31.2 | 20.3 | 20.6 | 9.4 | 13.6 | 11.5 | |
| 55–64 | N | 11,879 | 9449 | 8881 | 6742 | 6293 | 6265 | 4465 | 2211 | 1927 | 672 | 945 | 689 |
| % | 12.5 | 9.0 | 8.4 | 56.8 | 66.6 | 70.5 | 37.6 | 23.4 | 21.7 | 5.7 | 10.0 | 7.8 | |
| 65–74 | N | 21,215 | 21,791 | 16,861 | 10,906 | 13,705 | 11,637 | 9575 | 6396 | 4092 | 734 | 1690 | 1132 |
| % | 22.3 | 20.9 | 16.0 | 51.4 | 62.9 | 69.0 | 45.1 | 29.4 | 24.3 | 3.5 | 7.8 | 6.7 | |
| 75–84 | N | 33,324 | 34,438 | 35,686 | 13,587 | 18,639 | 22,548 | 18,768 | 12,976 | 10,505 | 969 | 2823 | 2633 |
| % | 35.0 | 33.0 | 33.8 | 40.8 | 54.1 | 63.2 | 56.3 | 37.7 | 29.4 | 2.9 | 8.2 | 7.4 | |
| 85+ | N | 17,241 | 27,307 | 35,175 | 4799 | 11,360 | 18,998 | 11,980 | 13,388 | 12,891 | 462 | 2559 | 3286 |
| % | 18.1 | 26.1 | 33.3 | 27.8 | 41.6 | 54.0 | 69.5 | 49.0 | 36.6 | 2.7 | 9.4 | 9.3 | |
| Gender | |||||||||||||
| Men | N | 49,654 | 54,559 | 54,112 | 24,121 | 31,447 | 34,839 | 22,354 | 17,335 | 14,463 | 3179 | 5777 | 4810 |
| % | 52.2 | 52.2 | 51.2 | 48.6 | 57.6 | 64.4 | 45.0 | 31.8 | 26.7 | 6.4 | 10.6 | 8.9 | |
| Stand. % | – | – | – | 48.6 | 58.7 | 64.8 | 45.0 | 30.4 | 25.2 | 6.4 | 10.9 | 10.0 | |
| Med, IQR | 72, 61–80 | 74, 64–82 | 77, 66–84 | 69, 59–78 | 73, 63–80 | 76, 66–84 | 76, 67–82 | 78, 69–84 | 79, 69–86 | 54, 33–69 | 67, 45–79 | 73, 55–83 | |
| Women | N | 45,500 | 49,939 | 51,579 | 18,450 | 25,619 | 30,382 | 25,456 | 19,707 | 16,814 | 1594 | 4613 | 4383 |
| % real | 47.8 | 47.8 | 48.8 | 40.5 | 51.3 | 58.9 | 55.9 | 39.5 | 32.6 | 3.5 | 9.2 | 8.5 | |
| Stand. % | – | – | – | 40.5 | 53.4 | 61.9 | 55.9 | 37.5 | 30.2 | 3.5 | 9.1 | 7.9 | |
| Med, IQR | 79,70–85 | 81, 72–87 | 83, 76–88 | 75, 65–82 | 78, 69–85 | 82, 73–87 | 81, 74–86 | 84, 77–89 | 85, 79–90 | 76, 59–83 | 82, 73–88 | 85, 78–90 | |
%: non-standardised proportion; stand. %: age- and gender-standardised proportion; Med: median; IQR: interquartile range.
All medians and IQR relative to age; median reported instead of mean due to non-normal age distribution. ‘Domicile’ includes deaths at home and care/nursing homes; ‘Hospital’ includes deaths in clinical facilities; ‘Other place’ includes deaths occurring in public spaces.
Figure 1.
Past trends and future projections of total numbers of births and deaths (Portugal, 1890–2060), deceased and resident population pyramids (Portugal, 1988, 2010, 2030).
Data source for past deaths, births and resident numbers (1890–2010) – INE; data source for future deaths, births and resident numbers (2011–2060) – Eurostat; deceased age pyramids only include deaths at ages of 18+ years. Left bars (blue) in the age pyramids refer to men and right bars (red) refer to women.
The proportions and absolute numbers of deaths due to cancer as the underlying cause have been slowly increasing since 2002, from 21.0% (22,181 deaths) to 23.6% (24,293 deaths) in 2010, while deaths due to non-malignant diseases decreased from 67.6% (71,374 deaths) in 2002 to 64.7% (68,422 deaths) in 2010 (Table 2). Unknown and external causes were responsible for the remaining deaths. Women die more frequently from non-malignant diseases than men (70.9% vs 58.9% in 2010, respectively). Older people also die more often from non-malignant diseases; these accounted for 80.2% of the deaths from people aged 85+ years in 2010. Cancers are responsible for almost half of the deaths (44.5% in 2010) from those aged 55–64 years.
Table 2.
Past trends of place of death by cause of death (Portugal – 2002, 2010).
| Cause of death | All places |
Hospital |
Domicile |
Other place |
|||||
|---|---|---|---|---|---|---|---|---|---|
| 2002 | 2010 | 2002 | 2010 | 2002 | 2010 | 2002 | 2010 | ||
| Cancer | N | 22,181 | 24,923 | 15,252 | 19,058 | 6214 | 5073 | 715 | 792 |
| % | 21.0 | 23.6 | 68.8 | 76.5 | 28.0 | 20.4 | 3.2 | 3.2 | |
| Non-malignant | N | 71,374 | 68,422 | 39,480 | 42,085 | 26,598 | 21,257 | 5296 | 5080 |
| % | 67.6 | 64.7 | 55.3 | 61.5 | 37.3 | 31.1 | 7.4 | 7.4 | |
| External/unknown | N | 11,960 | 12,346 | 4572 | 4078 | 3251 | 4947 | 4137 | 3321 |
| % | 11.3 | 11.7 | 38.2 | 33.0 | 27.2 | 40.1 | 34.6 | 26.9 | |
‘Domicile’ includes deaths at home and care/nursing homes; ‘Hospital’ includes deaths in clinical facilities; ‘Other place’ includes deaths occurring in public spaces. The cause of death was coded according to the International Classification of Diseases, 10th revision (ICD-10) and grouped into three major groups: cancer (including haematological malignancies), non-malignant diseases and external or unknown causes of death.
During the study period, 1,289,266 deaths were recorded as occurring in hospital (54.5% of all deaths). The proportion of hospital deaths increased steadily over time by a mean of 0.8% and 1030 deaths per year, from 44.7% (42,571 deaths) in 1988 to 61.7% (65,221 deaths) in 2010. Differences in the gender and age distribution of the deceased over the years analysed did not alter this trend (Figure 2). The increase in hospital death proportions occurred in all age groups except the youngest (18–34 years), but was largest in the older age groups (75–84 and 85+ years) and more prominent in women than men (Table 1). People dying in hospital were more often men and younger than those dying elsewhere, but these differences have been decreasing over time (Table 1). People dying with cancer died more often in hospital than those dying from non-malignant diseases (76.5% compared to 61.5% in 2010).
Figure 2.
Past trends of deaths by place of death and proportion of hospital deaths by age group (Portugal, 1988–2010).
st: age- and gender-standardised proportion; the age groups presented represent more than 90% of all deaths in the study in recent years.
From 1988 to 2010, 889,021 deaths occurred in the domicile (37.6% of all deaths), including deaths at home and care homes. Despite the increase in total numbers of deaths in the years analysed, domicile deaths have decreased over time, from 47,810 (50.2%) in 1988 to 31,277 (29.6%) in 2010 (Figure 2). This fall was observed in all age groups except the youngest (18–34 years) and was higher in the age groups of 65+ years (mirroring the age differences observed in hospital deaths). The trend is not explained by changes in the gender and age distribution over the years as it maintained when calculated using age- and gender-standardised percentages of hospital deaths (Figure 2).
Deaths in the domicile were more frequent in older ages and among women (Table 1). People dying from cancer die less often in the domicile than those dying from non-malignant diseases (20.4% compared to 31.1% in 2010).
A minority of deaths were registered as taking place in ‘other places’ (186,545 deaths from 1988–2010, accounting for 7.9% of all deaths). Historically, men and younger people died in other places more often than women and older people, but these differences have been decreasing over time. Notably, the proportion of the very old (85+ years) people dying in other places has increased 7 percentage points, from 2.7% to 9.4% in 2010 (Table 1). People aged 18–34 years and those dying from external or unknown causes die more frequently in other places than other age groups (Table 1).
Projections
Annual numbers of deaths are projected to rise further by 5.6% until 2030 to 111,584 deaths. This is mainly due to the projected increase in deaths from people aged 85+ years, which are expected to increase by 42.7%, to 45.0% of all deaths in Portugal in 2030 (Table 3; Figure 1). The projections also show a progressively ageing population. Substantial changes in the age pyramids of residents and deceased populations will occur until 2030, when 30.9% of the residents are expected to be aged 60+ years and 7.0% aged 80+ years, compared to 23.9% and 4.6%, respectively, in 2010 (Figure 1).
Table 3.
Projected total deaths and hospital deaths by age and gender according to three models (Portugal – 2010, 2020, 2030).
| All deaths (all places) |
Hospital deaths |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2010 | 2020 | 2030 | Model 1 |
Model 2 |
Model 3 |
||||||
| 2010 | 2020 | 2030 | 2020 | 2030 | 2020 | 2030 | |||||
| Total | |||||||||||
| N | 105,691 | 106,221 | 111,584 | 65,221 | 76,597 | 87,905 | 85,159 | 99,176 | 71,959 | 83,293 | |
| % | 100 | 100 | 100 | 61.7 | 72.1 | 78.8 | 80.2 | 88.9 | 67.7 | 74.6 | |
| Age (years) | |||||||||||
| 18–34 | 1370 | 1003 | 876 | 679 | 245 | 220 | 378 | 271 | 418 | 300 | |
| % | 1.3 | 0.9 | 0.8 | 49.6 | 24.4 | 25.1 | 37.7 | 31.0 | 41.7 | 34.3 | |
| 35–44 | 2474 | 2143 | 1535 | 1545 | 800 | 362 | 1034 | 724 | 1271 | 861 | |
| % | 2.3 | 2.0 | 1.4 | 62.4 | 37.3 | 23.6 | 48.3 | 47.1 | 59.3 | 56.0 | |
| 45–54 | 5210 | 4708 | 4174 | 3536 | 3536 | 3252 | 3613 | 3309 | 3225 | 2885 | |
| % | 4.9 | 4.4 | 3.7 | 67.9 | 75.1 | 77.9 | 76.7 | 79.2 | 68.5 | 69.1 | |
| 55–64 | 8881 | 8064 | 7382 | 6265 | 6593 | 6408 | 6715 | 6541 | 5956 | 5694 | |
| % | 8.4 | 7.6 | 6.6 | 70.5 | 81.8 | 86.8 | 83.3 | 88.6 | 73.9 | 77.1 | |
| 65–74 | 16,861 | 15,138 | 14,710 | 11,637 | 9502 | 7367 | 9760 | 8189 | 11,160 | 11,538 | |
| % | 16.0 | 14.3 | 13.2 | 69.0 | 62.8 | 50.1 | 64.5 | 55.7 | 73.7 | 78.4 | |
| 75–84 | 35,686 | 32,376 | 32,716 | 22,548 | 25,586 | 28,623 | 25,985 | 29,952 | 22,619 | 25,058 | |
| % | 33.8 | 30.5 | 29.3 | 63.2 | 79.0 | 87.5 | 80.3 | 91.6 | 69.9 | 76.6 | |
| 85+ | 35,175 | 42,790 | 50,190 | 18,998 | 30,336 | 41,673 | 37,674 | 50,190 | 27,311 | 36,957 | |
| % | 33.3 | 40.3 | 45.0 | 54.0 | 70.9 | 83.0 | 88.0 | 100.00 | 63.8 | 73.6 | |
| Gender | |||||||||||
| Men | N | 54,112 | 53,332 | 55,870 | 34,839 | 39,043 | 43,458 | 42,852 | 47,167 | 37,301 | 42,608 |
| % | 51.2 | 50.2 | 50.1 | 64.4 | 73.2 | 77.8 | 80.3 | 84.4 | 69.9 | 76.3 | |
| Women | N | 51,579 | 52,889 | 55,718 | 30,382 | 37,554 | 44,447 | 42,307 | 52,009 | 34,658 | 40,685 |
| % | 48.8 | 49.8 | 49.9 | 58.9 | 71.0 | 79.8 | 80.0 | 93.3 | 65.5 | 73.0 | |
%: non-standardised proportion.
Model 1 assumed that last 5 year trends of numbers of hospital deaths will be maintained in the future; model 2 assumed that last 5 year trends of variation of hospital deaths will be maintained; model 3 assumed that last 5 year trends of proportions of non-hospital deaths will be maintained (for more details on how these models were designed, please refer to Appendix 1).
Within this scenario of increasing numbers of deaths occurring at later ages, annual numbers of hospital deaths are projected to increase to more than 80,000 regardless of the scenario considered, ranging from 83,293 deaths (74.6% of all deaths) when assuming trends in non-hospital deaths will continue (model 3) to 99,176 deaths (88.9% of all deaths) when assuming the proportional change in hospital deaths will continue (model 2; Table 3; Figure 3). These numbers correspond to an increase in the annual number of hospital deaths by a minimum of 18,072 deaths (27.7% rise from 2010) to a maximum of 33,955 deaths (52.1% rise) by 2030, when compared to 2010. This is mainly due to the expected sharp increase in hospital deaths from people aged 85+ years, from 18,988 (54.0%) to at least 36,957 (73.6%) deaths in the third model. Model 2 (assuming recent proportional changes in hospital deaths continue) projects 100% of deaths from people aged 85+ years to take place in hospital by 2024 onwards.
Figure 3.
Past trends and future projections of hospital deaths according to three models (Portugal, 1988–2030).
The mean of the last 5-year slopes (2006–2010) was used in all models. The slopes’ variable changed depending on the model: model 1 – slopes of absolute numbers of hospital deaths; model 2 – slopes of proportion of change of hospital deaths; and model 3 – slopes of proportions of non-hospital deaths.
Discussion
Our study shows that regardless of the scenario considered, and if current trends continue, hospital death proportions will increase by more than a quarter until 2030.
This is the first time that mortality is projected by place of death in a country without integrated palliative care (Portugal). Globally, about 39% of countries are in this situation.7 Our projections show a topical upward trend of hospital deaths, in the context of marked ageing and increasing numbers of deaths. This trend goes against what the majority of people prefer, which is to die at home,3,4,6 and raises questions about the future sustainability of hospital inpatient care. The study and its implications substantially strengthen the resolution approved by the WHO Board of Directors in January 2014, calling for countries to integrate palliative care in their healthcare systems.8
Limitations
The limitations of analysing routinely collected mortality data include the possibility of filling and coding errors, and coding changes during the study period. To our knowledge, the accuracy of place of death of this dataset has not been determined. This is a limitation that applies to place of death data for many countries;15,16 in Portugal, the fact that the data are filled in by the doctor who certifies the death may provide added reassurance that the recorded location is correct. In 1996, the coding of place of death in Portuguese death certificates was altered from four to three categories, with the deletion of the category ‘public way’, but the impact of this change on the findings is minimal because the more recent definition of ‘other places’ includes public ways. No further changes have been made in the time period analysed. However, considering recent data showing that the population clearly distinguishes home, care homes and palliative care units in terms of preferences for place of death,6 it is crucial to change the categories for place of death in Portuguese death certificates, in order to distinguish these different places.
Comparing the projected and actual numbers of deaths in Portugal in 2011, we found that the Eurostat projections underestimate the actual numbers of deaths by 4776 deaths (4.6%). This is important to consider when interpreting the results of projected proportions of hospital deaths in models 1 and 2 and projected hospital death numbers in model 3, as they may have been underestimated to the same extent.
Projections rely on assumptions that may or may not confirm in the future, being also dependent on policy decisions that may happen in the meantime. For this study, we assumed that the last 5-year trends (2006–2010) will be maintained. We then modelled three scenarios, based on different assumptions. Despite differences, all three models show a consistent trend of increasing hospital deaths in the future, by at least one quarter until 2030. Importantly, these projections agree with more recent numbers, although it is yet too early to see a consistent trend. Percentages of hospital deaths were 63.4% (64,818) in 2011, 63.6% (68,074) in 2012 and 64.3% (68,223) in 2013; both the percentages and numbers fall between our projected values from models 1 to 3 (INE, personal communication 1/07/2015).
Socio-demographic sustainability
Our findings confirm that people are increasingly dying at older ages in Portugal, with a notable increase in the median age at death of 5 years for men and 4 years for women from 19881,2 to 2010. This is at the forefront of global ageing trends,1,2 showing that Portugal is particularly affected by the complex challenges posed by ageing while having scarce resources to meet people’s palliative care needs.7
In addition, a future reduction in informal and formal care availability is likely, due to the projected fall of birth numbers, which were already outnumbered by deaths in recent years, and decreasing older-age support ratios. Based on the findings, we call for the development of a national public health strategy with two main goals: (1) to increase birth numbers, by providing economic and social conditions for childbearing age people to create families, and (2) to ensure community support for older people, by developing sustainable community services including home care, care homes and day centres supported by public and private sectors and integrated in the health and social care systems.
Projected increase in hospital deaths
Based on the trends observed in the last 5 years (2006–2010), we project hospital deaths to rise by at least 27.7% until 2030, corresponding to an increase of more than 15,000 annual deaths within a projected total number of deaths of approximately 111,000 per year by 2030. This increase will occur mainly due to almost doubling numbers of hospital deaths of those aged 85+ years, irrespective of the model considered. In less than 10 years’ time, by 2024 onwards, and if current trends of proportional changes of hospital deaths continue (model 2), all of those dying at ages of 85 years or beyond will die in hospital. It is important to note that age is one key factor shaping preferences for where to die, with older people having a higher preference for dying at home (66.2% of age 75+ years compared to 51.2% among the 1286 participants in the PRISMA population survey in Portugal).6 The prevailing trend towards hospitalised dying in Portugal is therefore not only difficult to sustain in terms of healthcare resources, but also it is heading in a direction which is against people’s preferences, particularly for those dying at older ages.
Regarding gender differences, we found that men died more frequently in hospital than women, although the difference in proportions has decreased over time. This trend is mirrored in the projections, with models 1 and 2 projecting that if current trends continue, women will die more frequently in hospital than men by 2030. More research is needed to understand these gender trends.
Compared to other countries, the proportion of hospital deaths in Portugal is relatively high −62% compared with 54% in a recent international review of statistics from 45 countries.15 This is unlikely to be explained by the availability of hospital beds, as Portugal had fewer beds (3.4) than EU-27 (5.3) per 1000 population in 2010.17 In the international comparison, Portugal was the eighth country with the highest proportion of hospital deaths, preceded only by Japan, Brazil, Malta, Korea, Botswana, Wales and Sweden.15 We projected this proportion to increase to at least three quarters of all deaths by 2030. In the worst case scenario projected, they can increase up to 89% of all deaths.
This is not such a common finding in other studies. In Germany, the proportion of hospital deaths is expected to remain stable in future years,12 and in the United Kingdom, Canada and the United States, where home care is more developed, a reversal of trends has already happened.14,18,19 Also, in Belgium, where a policy to support care homes has been developed, a shift in the numbers of deaths from hospital to care homes was observed in recent years.13 Interestingly, in these countries, it was found that patients dying from cancer die more often than others at home. In Portugal, we found the opposite. We know that being supported by home palliative care is a determinant factor to die at home.20 What we see in Portugal is a shortage of these teams and a general lack of integration of palliative care in the mainstream healthcare.6,7 Considering that patients with cancer experience a more predictable trajectory, these patients might be more likely to remain in hospital when deemed to be in the end-of-life stage, so as to access care to relieve their physical suffering in a context of scarce home palliative care. This might be a potential explanation. It would be interesting to compare our results with countries with similar palliative care development levels. For instance, in Botswana, 10% of all cancer deaths occurr at home, while people dying from cardiovascular diseases and other diagnoses died more often in a home setting (14% and 13%, respectively).21 Nonetheless, this comparison is challenging, as in Botswana the proportion of deaths due to unknown causes is very high (33%), and of these, 91% die at home. In Japan, patients with non-malignant diseases also die more often at home than patients with cancer.22 Although palliative care is generally more developed in this country,7 service provision is mainly focused in palliative care units and hospital-support teams. Home palliative care is still under development in Japan. A study of six European countries in 2002/2003 found higher home death proportions in cancer compared to non-cancer deaths in all countries except Norway, where cancer patients were more likely to die in hospital (similar to Portugal). The authors suggested that this could be because palliative care developed mainly in hospitals and access to institutional care remains high in Norway, with primary care playing a relatively weak gate-keeping role.23 Variations are likely to be due to a combination of organisational, societal and cultural factors as well as physicians’ attitudes and training.
Implications for practice, policy and future research
Examining experiences in other countries including the United States and the United Kingdom,14,24 it seems that with targeted national strategies, focused on developing palliative care support in the community, it is possible to influence hospital death trends. This is further supported by evidence from a Cochrane review, which found that specialist home palliative care services double the odds of death at home while significantly decreasing symptom burden when compared to usual care.25
If, by the contrary, nothing is done, our study suggests that countries with ageing populations and scarce palliative care services may face a marked increase in hospital deaths which is not economically sustainable nor desired by the population.
Therefore, in order to meet people’s preferences for dying at home, we call for the development of home palliative care teams integrated in the existent healthcare systems. This is especially needed in ageing countries, where the numbers of deaths and dependency ratios are increasing, so as to avoid unwanted hospitalisations and unsustainable hospital care while increasing the quality of care for the older population.
Further research is needed to determine the impact of such high proportions of older people dying in hospitals in regions where palliative care is not integrated in the healthcare system, both in terms of resources and in relation to the quality of care that people receive at the end of life. We also call for improvements in the way place of death is coded in death certificates, with the inclusion of separate categories which are known to be key in people’s preferences, mainly ‘palliative care unit’, ‘home’ and ‘care/nursing home’, so as to meaningfully monitor such an important outcome.
Acknowledgments
The authors thank the Calouste Gulbenkian Foundation for funding this study in the context of the DINAMO project. DINAMO aims to enhance advanced training and research to optimise home palliative care in Portugal. Principal Investigator: Barbara Gomes; Scientific Director: Irene J Higginson; other members of DINAMO: Pedro L. Ferreira, Vera P. Sarmento, Helder Aguiar, Ana Lacerda, Rita Canario, Duarte Soares and Maja de Brito. Irene J Higginson is an NIHR Senior Investigator and Head of the Department of Palliative Care, Policy and Rehabilitation at King’s College London. Pedro L. Ferreira is Head of the Centre for Health Studies and Research at the University of Coimbra and Professor in this institution. The authors express their gratitude to the Portuguese Statistics Institute (INE), namely to Dr Margarida Rosa and her team for providing the mortality database, access to their safe centre and technical support with no costs associated. They thank the Eurostat for providing population and mortality projections for Portugal, also free of charge. Finally, they are grateful to the Office for Statistics and Education Planning of the Portuguese Ministry of Science, Technology and Higher Education, namely to Dr Pedro Mota, for the invaluable support establishing the protocol with the INE and the Portuguese Ministry of Science, Technology and Higher Education required for this study. The authors thank the charity Cicely Saunders International for their support of the general programme on projections where the methods were developed, Natalia Calanzani for helping with data negotiation and colleagues at the Cicely Saunders Institute for their helpful comments on an earlier draft of this manuscript.
Appendix
Appendix 1.
Three different models for the projections of hospital deaths in Portugal (2011–2030)
| Model | Assumption | Slopes calculation (e.g.: Slope 2009–10) |
|---|---|---|
| Model 1 | Current trends in the number of hospital deaths will be maintained in the future. | Slope 2009–10 = N 2010 hospital deaths − N 2009 hospital deaths |
| Model 2 | Proportional changes of hospital deaths will be maintained in the future. | |
| Model 3 | Differences in proportions of non-hospital deaths will be maintained in the future. | 1. N domicile + N other place = N non-hospital deaths 2. Slope 2009–10 = % Non-hospital deaths 2010 – % Non-hospital deaths 2009 |
Footnotes
Author contributions: B.G. is Principal Investigator, conceived the study and together with I.J.H. and P.L.F. obtained funding. All authors contributed to its design. B.G. and V.P.S. negotiated the acquisition of the mortality data from the Portuguese Statistics Institute; V.P.S. negotiated acquisition of the population projections data from Eurostat. V.P.S. and B.G. decided the projection models, and V.P.S. analysed the data and interpreted the results supervised by B.G. with contributions from I.J.H. and P.L.F. V.P.S. drafted the manuscript; all authors read and approved the final manuscript.
Declaration of conflicting interests: The funders were not involved in the manuscript production or content, and the views are those of the authors, not any of the funding bodies.
Funding: This study was funded by the Calouste Gulbenkian Foundation in the context of the DINAMO project.
References
- 1. Department of Economic and Social Affairs. Population ageing and development 2012 (Wall Chart). New York: United Nations, 2012. [Google Scholar]
- 2. Gomes B, Cohen J, Deliens L, et al. International trends in circumstances of death and dying among older people. In: Gott M, Ingleton C. (eds) Living with ageing and dying: palliative and end of life care for older people, 1st ed. London: Oxford University Press, 2011, pp. 3–18. [Google Scholar]
- 3. Gomes B, Calanzani N, Gysels M, et al. Heterogeneity and changes in preferences for dying at home: a systematic review. BMC Palliat Care 2013; 12: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gomes B, Higginson IJ, Calanzani N, et al. Preferences for place of death if faced with advanced cancer: a population survey in England, Flanders, Germany, Italy, the Netherlands, Portugal and Spain. Ann Oncol 2012; 23: 2006–2015. [DOI] [PubMed] [Google Scholar]
- 5. Davies E, Higginson IJ. The solid facts: palliative care. Copenhagen: WHO Regional Office for Europe, 2004. [Google Scholar]
- 6. Gomes B, Sarmento VP, Ferreira PL, et al. Epidemiological study of place of death in Portugal in 2010 and comparison with the preferences of the Portuguese population. Acta Med Port 2013; 26: 327–334. [PubMed] [Google Scholar]
- 7. Connor SR, Bermedo MCS. Global atlas of palliative care at the end of life. London: World Palliative Care Alliance and World Health Organization, 2014. [Google Scholar]
- 8. World Health Organization Executive Board. Strengthening of palliative care as a component of integrated treatment within the continuum of care. Resolution EB134.R7, 23 January 2014. Geneva: WHO Executive Board. [Google Scholar]
- 9. Diário da República. Verificação da morte: Lei No. 141/99 de 28 de Agosto. Lisboa: Imprensa Nacional-Casa da Moeda, 1999. [Google Scholar]
- 10. Directorate-General for Economic and Financial Affairs. The 2012 ageing report: underlying assumptions and projections methodologies. Brussels: European Commission, 2011. [Google Scholar]
- 11. Gomes B, Higginson IJ. Where people die (1974–2030): past trends, future projections and implications for care. Palliat Med 2008; 22: 33–41. [DOI] [PubMed] [Google Scholar]
- 12. Simon ST, Gomes B, Koeskeroglu P, et al. Population, mortality and place of death in Germany (1950–2050) – implications for end-of-life care in the future. Public Health 2012; 126: 937–946. [DOI] [PubMed] [Google Scholar]
- 13. Houttekier D, Cohen J, Surkyn J, et al. Study of recent and future trends in place of death in Belgium using death certificate data: a shift from hospitals to care homes. BMC Public Health 2011; 11: 228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Flory J, Yinong YX, Gurol I, et al. Place of death: U.S. trends since 1980. Health Aff 2004; 23: 194–200. [DOI] [PubMed] [Google Scholar]
- 15. Broad JB, Gott M, Kim H, et al. Where do people die? An international comparison of the percentage of deaths occurring in hospital and residential aged care settings in 45 populations, using published and available statistics. Int J Public Health 2012; 58: 257–267. [DOI] [PubMed] [Google Scholar]
- 16. Pivodic L, Higginson IJ, Sarmento VP, et al. Health metrics: standardize records of place of death. Nature 2013; 495: 449. [DOI] [PubMed] [Google Scholar]
- 17. OECD. Health at a glance: Europe 2012. Paris: OECD Publishing, 2012. [Google Scholar]
- 18. Gomes B, Calanzani N, Higginson IJ. Reversal of the British trends in place of death: time series analysis 2004–2010. Palliat Med 2012; 26: 102–107. [DOI] [PubMed] [Google Scholar]
- 19. Wilson DM, Truman CD, Thomas R, et al. The rapidly changing location of death in Canada, 1994–2004. Soc Sci Med 2009; 68: 1752–1758. [DOI] [PubMed] [Google Scholar]
- 20. Gomes B, Higginson IJ. Factors influencing death at home in terminally ill patients with cancer: systematic review. BMJ 2006; 332: 515–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lazenby M, Ma T, Moffat HJ, et al. Influences on place of death in Botswana. Palliat Support Care 2010; 8: 177–185. [DOI] [PubMed] [Google Scholar]
- 22. Yang L, Sakamoto N, Marui E. A study of home deaths in Japan from 1951 to 2002. BMC Palliat Care 2006; 5: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cohen J, Houttekier D, Onwuteaka-Philipsen B, et al. Which patients with cancer die at home? A study of six European countries using death certificate data. J Clin Oncol 2010; 28: 2267–2273. [DOI] [PubMed] [Google Scholar]
- 24. Gao W, Ho YK, Verne J, et al. Changing patterns in place of cancer death in England: a population-based study. PLoS Med 2013; 10: e1001410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gomes B, Calanzani N, Curiale V, et al. Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers. Cochrane Database Syst Rev 2013; 6: CD007760. [DOI] [PMC free article] [PubMed] [Google Scholar]